Abstract
Fixation of subtrochanteric fracture, even for experienced surgeons, is a challenge. This fracture is most difficult to treat, and the incidence of complications in this type of fracture is higher. This study compared surgical results of two methods, proximal femur locking compression plate and intramedullary locking nail. This is an analytic study, performed on all patients with subtrochanteric fracture who were referred to the hospital during 3 years. They were treated with proximal femur locking plate or intramedullary locking nail. The postoperative complications were evaluated and recorded. Finally, the data were analyzed by SPSS software. Complications were studied in both groups. Neither treatment has statistically significant difference in complications, onset of complications incidence, and time of full-weight bearing. Although the Harris Hip Score among patients improved in both methods of treatment, there is no significant difference between the two groups. The results of subtrochanteric fracture fixation by intramedullary or locking plate were similar and had the same outcome.
Keywords: Subtrochanteric fracture, Locking plate, Intramedullary locking nail, Postoperative complications
Introduction
Fixation of subtrochanteric fracture, even for experienced surgeons, is a challenge. This fracture includes about 10–30 % of all hip fractures and can affect all age groups [1] but mostly occurs in older people (as a result of low-energy trauma such as falling) and young people (due to high-energy trauma such as a car accident or falling from a height) [2]. The rate of complications in this type of fracture also is higher [3].
Although there are several surgical procedures for subtrochanteric fracture treatment including 45° condylar blade plate, 135° angled blade plate, and intramedullary nail and various methods of treatment are mentioned in texts in some types of subtrochanteric fractures, no gold standard treatment has been offered for this kind of fracture [4].
In some studies, intramedullary nailing was reported as the best method of subtrochanteric fracture fixation. Authors have reported that most subtrochanteric fractures are treated with intramedullary devices [5], because the rate of treatment failure and varus collapse in extramedullary implants is more than that achieved by intramedullary nails [5] while the need for reoperation in the intramedullary nails is more than that in extramedullary implants [3]. On the other hand, in some studies, the proximal femoral locking plate technique is superior, because of its high union rate and less complications in comminuted subtrochanteric fractures [3]. Given such challenges, in this study, we compared the results of subtrochanteric fracture treatment with these two methods.
Materials and Methods
This is an analytic study, carried on all patients with subtrochanteric fracture who were referred to Poursina hospital from April 2010 to April 2013. They were treated with proximal femur locking plate or intramedullary locking nail. Inclusion criteria included patients older than 18 years with type 2A Russell–Taylor (a stable medial buttress) subtrochanteric fractures caused by trauma and underwent surgery within 3 days after the accident with one of these two methods. Exclusion criteria included pathologic fractures, multiple fractures in the lower extremities, inability to walk before injury (abnormal preoperative hip ROM), proven psychological problems that interfere with the postoperative assessment, not being referred during the follow-up, simultaneously head trauma, open fracture, pregnancy, and any use of materials affecting the union (cigarettes, alcohol, cortisone, etc.).
The intramedullary nail group was treated with closed reduction using a traction table and percutaneous insertion of a proximal femoral nail without anatomic reduction. The locking plate group was treated with open anatomic reduction, minimizing soft-tissue stripping of fracture fragments, and internal fixation using a fixed-angle locking proximal femur plate and interfragmentary screws. Both groups were recommended for physiotherapy and partial weight-bearing postoperation, as soon as possible. The patients were evaluated about variables consisting of age, sex, affected side, postoperative complications (nonunion, malunion, infection, device failure, thromboembolism, pneumonia, compartment syndrome, and deep vein thrombosis (DVT)), range of motion of hip joint, onset of complications' incidence, and time of full-weight bearing. The patients were followed up for 2 weeks and visited at the first, third, and sixth months and 1 year postoperation. Trochanteric region malunion means internal or external rotation and varus or valgus and limb shortening (more than 1 cm). Union of fracture was considered as the disappearance of fracture line between cortices 3 and 4 on anterior–posterior and lateral radiographs, complete bony trabeculae crossing the fracture site, and painless movement in clinical examination. Delayed union was defined as lack of progression of union for more than 3 months after fracture or uncompleted union up to 9 months. Redness and discharge from the surgical site with positive culture indicate infection. Also, patients in both groups were evaluated with Harris hip scoring criteria (to evaluate the function of the hip joint) in the first visit and 6 months later.
Finally, the data were analyzed by SPSS-19 software. Analysis was performed by descriptive statistics, the chi-squared test and independent t-test, and the general linear model. To investigate ROM, as it follows normal distribution, independent t-test was used, and paired t-test was used for other quantitative variables. P-value <0.05 was significant.
Results
One hundred fourteen patients with subtrochanteric fractures were enrolled to the study. Demographic characteristics of the patients are shown in Table 1.
Table 1.
Demographic characteristics of patients, fracture, and surgery features
| Characteristics | Number (%) | |
|---|---|---|
| Sex | Male | 63 (55.3) |
| Female | 51 (44.7) | |
| Age (year) | <40 | 43 (37.7) |
| 41–60 | 49 (43) | |
| 61–70 | 13 (11.4) | |
| 71–80 | 6 (5.3) | |
| ≥81 | 3 (2.6) | |
| Age (year) (mean ± standard deviation) | 47.28 ± 15.94 | |
| Fixation method | Locking plate | 71 (62.3) |
| Intramedullary locking nail | 43 (37.7) | |
| Affected side | Right | 61 (53.5) |
| Left | 53 (46.5) | |
| Time of incidence of complications (day) (mean ± standard deviation) | 45.20 ± 40.32 | |
In this study, there was no significant difference between two surgical methods according to sex, age, and side of fracture. Also, complications in the two groups did not differ in these variables.
Overall, in 26 patients, surgical complications were observed. Of these, 27 % were infected, 15 % were infected with other complications, 12 % had device failure, 11 % had malunion, 8 % had nonunion, 8 % had nonunion combined with infection, 4 % had malunion combined with infection, and 15 % had other complications such as thromboembolism, pneumonia, deep vein thrombosis, and compartment syndrome. No difference existed between the complications of the two groups (Table 2).
Table 2.
Complications according to fixation methods
| Complications | Intramedullary locking nail | Locking plate | Total, n (%) |
|---|---|---|---|
| Infection | 2 | 5 | 7 (27) |
| Pure nonunion | 0 | 2 | 2 (8) |
| Pure malunion | 0 | 3 | 3 (11.5) |
| Device failure | 1 | 2 | 3 (11.5) |
| Complex complications | |||
| Infection with other complications | 1 | 3 | 4 (15) |
| Infection with nonunion | 2 | 0 | 2 (8) |
| Infection with malunion | 1 | 0 | 1 (4) |
| Others | 3 | 1 | 4 (15) |
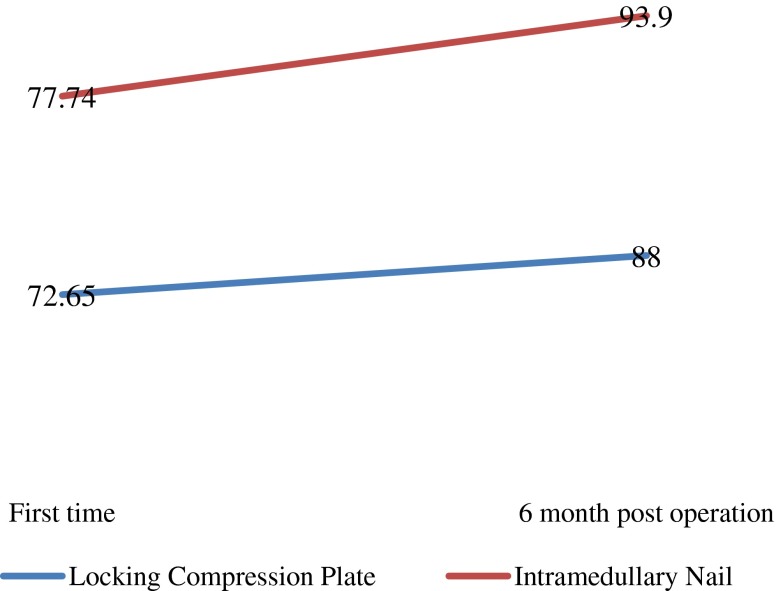
In the present study, the mean of range of motion was 136.84 ± 6.17°. Evaluation of this variable based on sex, age, and type of surgery is shown in Table 3. Assessment of Harris hip score revealed a significant increase in both groups during the first- to sixth-month visit, but this change shows no significant difference between two groups (P = 0/628; Figure 1).
Table 3.
Mean of range of motion based on sex, age, and surgical technique
| Range of motion | P-value | ||
|---|---|---|---|
| Sex | Male | 137.61 ± 6.34 | 0.13 |
| Female | 135.88 ± 5.89 | ||
| Age (year) | <60 | 137.93 ± 5.70 | 0.001 |
| 60-70 | 132.69 ± 6.65 | ||
| 71-80 | 131.66 ± 6.83 | ||
| ≥81 | 131.66 ± 2.88 | ||
| Surgical technique | Locking plate | 135.07 ± 5.63 | <0.0001 |
| Intramedullary locking nail | 139.76 ± 5.97 |
Figure 1.
Harris hip score in two groups
The average time of complication incidence and postoperative full-weight bearing were evaluated. There was no significant difference between treatment groups for these two variables. The mean time of full-weight bearing on the lower limb was estimated at 125.14 ± 35.66 days for the locking plate group and 129.30 ± 30.60 days for the intramedullary nail group. The mean time of incidence of postoperative complications was 50.66 ± 41.48 days for the locking plate group and 37.00 ± 29.17 days for the intramedullary nail group.
Discussion
Until now, no gold standard method of fixation for some subtypes of subtrochanteric fracture has been demonstrated [5]. The high rate of mechanical failure of the fixation of unstable proximal femoral fractures with proximal locking plate is expected [6]. Also, tilting of rotational order following the intramedullary nail is a fundamental problem [7]. The aim of this study was to determine the effects of these two methods. Accordingly, 114 patients were enrolled in this study.
Postoperative complications including infection, nonunion, malunion, and device failure were observed in 26 patients of the study population which did not differ between the sexes. Although the incidence of complications in our study was not statistically different between the two groups, the complications such as malunion or nonunion were observed only in the locking plate technique, and more complex complications were seen only in the way of intramedullary nail. Haefeli and colleagues studied 17 patients who were treated by locking plate. In their study, one person has been infected, and one person needed reoperation [8]. In Berkes and colleagues' study, the use of locking plates in proximal femoral fractures leads to 36.8 % device failure. It is attributed to the stiffness of this tool that prevents any fracture site micromotion, placing the mechanical burden on the implant, which can result in failure at the bone–screw interface or fatigue failure of the implant itself [9]. In Glassner's study, seven treatment failures with the locking plate were due to nonunion, implant fracture, and loss of fixation [10]. Generally, different causes for this issue are intended. The accuracy of the technique used and the skill and precision of the surgeon can be effective for incandescing surgical complications [11]. However, in this study, it was shown that the use of a locking plate or intramedullary nail may not be a factor for the occurrence of complications.
Glassner in his study stated that five of the seven cases treated with locking plate developed complications and device failure after 12.7 days, in average [10]. Our study is also partly consistent with Glassner's results; as 44 % of the patients experienced complications during the first 10 days. It seems that complications such as infection occur in the first 10 days, but other complications including device failure, nonunion, and malunion need more time to appear.
In this study, the range of motion of the intramedullary nail group was 4° more than that of the locking plate group. Although this difference was statistically significant, it did not make a critical difference in the clinical appearance. Studies have shown that between the range of motion and gender, there was no significant difference which was consistent with our study [12–14]. Haefeli suggested that full-weight bearing on the lower extremity is achieved faster in the locking plate technique than in other methods [8]. Although the difference was not significant in our study, the mean of full-weight bearing in the locking plate was less than that in intramedullary nail.
According to our results, these two methods of treatment had almost identical outcome, while other studies on the effectiveness of each method are discussed, for example, it is expressed that a fixed-angle device (locking plate) prevents toggling between the size of the plate and screws, and as a result, rigidity and the pullout force increase. This feature has led to the locking plate being considered as a premier implant for the treatment of unstable fractures such as subtrochanteric fracture [15]. However, Saini and his colleagues found in their study that the locking plate led to stable fixation with a high union rate and fewer complications [3], while Parker and his colleagues in their clinical trial showed there is more improvement in mobility with intramedullary implant fixation [16].
In Yong's study, in the follow-up at 6–10 months after surgery using the locking plate and intramedullary nail, no significant differences were found between the Harris hip score of the two groups [17]. Although our study showed that in all cases the Harris hip score of the locking plate technique is better than that of intramedullary nail technique, both methods showed the same changes when they were compared during the 6-month period, which is consistent with the Yong study. Of course, factors such as the individual experience, even the type of fractures and surrounding tissue injuries, can have an effect on the Harris hip score [11].
Conclusion
Although some studies distinguished between the two methods, in this study, according to complications studied, no advantage was found for the locking plate and intramedullary nail techniques.
Contributor Information
Ahmadreza Mirbolook, Phone: +98-9112310025, Email: ahmadreza_mirbolook@yahoo.com.
Babak Siavashi, Email: dr.babak.siavashi@gmail.com.
References
- 1.Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, Cosman F. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21(3):399–408. doi: 10.1007/s00198-009-0962-6. [DOI] [PubMed] [Google Scholar]
- 2.Ekstrom W, Nemeth G, Samnegard E, Dalen N, Tidermark J. Quality of life after a subtrochanteric fracture: a prospective cohort study on 87 elderly patients. Injury. 2009;40(4):371–376. doi: 10.1016/j.injury.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Saini P, Kumar R, Shekhawat V, Joshi N, Bansal M, Kumar S. Biological fixation of comminuted subtrochanteric fractures with proximal femur locking compression plate. Injury. 2013;44(2):226–231. doi: 10.1016/j.injury.2012.10.037. [DOI] [PubMed] [Google Scholar]
- 4.Rockwood CA, Green DP, Bucholz RW. Rockwood and Green's fractures in adults. 7. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 5.Luo Q, Fang C, Shen WY, Lau TW, Leung F. A lesson from the failure of intramedullary fixation of atypical subtrochanteric fractures: a report of two cases. JBJS Case Connect. 2013;3(1):1–4. doi: 10.2106/JBJS.CC.L.00098. [DOI] [PubMed] [Google Scholar]
- 6.Streubel PN, Moustoukas MJ, Obremskey WT. Mechanical failure after locking plate fixation of unstable intertrochanteric femur fractures. J Orthop Trauma. 2013;27(1):22–28. doi: 10.1097/BOT.0b013e318251930d. [DOI] [PubMed] [Google Scholar]
- 7.French BG, Tornetta P., 3rd Use of an interlocked cephalomedullary nail for subtrochanteric fracture stabilization. Clin Orthop Relat Res. 1998;348:95–100. doi: 10.1097/00003086-199803000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Haefeli M, Huber H, Dierauer S, Ramseier LE. Fixation of subtrochanteric extending/derotational femoral osteotomies with the Locking Compression Plate in ambulatory neuro-orthopaedic patients. J Child Orthop. 2010;4(5):423–428. doi: 10.1007/s11832-010-0281-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berkes MB, Little MT, Lazaro LE, Cymerman RM, Helfet DL, Lorich DG. Catastrophic failure after open reduction internal fixation of femoral neck fractures with a novel locking plate implant. J Orthop Trauma. 2012 doi: 10.1097/BOT.0b013e31823b4cd1. [DOI] [PubMed] [Google Scholar]
- 10.Glassner PJ, Tejwani NC. Failure of proximal femoral locking compression plate: a case series. J Orthop Trauma. 2011;25(2):76–83. doi: 10.1097/BOT.0b013e3181e31ccc. [DOI] [PubMed] [Google Scholar]
- 11.Kanthimathi B, Narayanan V. Early complications in proximal femoral nailing done for treatment of subtrochanteric fractures. Malays Orthop J. 2012;6(1):25–29. doi: 10.5704/MOJ.1203.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan N, Askar Z, Ahmed I, Durrani Z, Khan M, Hakeem A. Intertrochanteric fracture of femur; outcome of dynamic hip screw in elderly patients. Professional Med J. 2010;17(2):328–333. [Google Scholar]
- 13.Rahme DM, Harris IA. Intramedullary nailing versus fixed angle blade plating for subtrochanteric femoral fractures: a prospective randomised controlled trial. J Orthop Surg (Hong Kong) 2007;15(3):278–281. doi: 10.1177/230949900701500306. [DOI] [PubMed] [Google Scholar]
- 14.Song HR, Oh CW, Mattoo R, Park BC, Kim SJ, Park IH, Jeon IH, Ihn JC. Femoral lengthening over an intramedullary nail using the external fixator: risk of infection and knee problems in 22 patients with a follow-up of 2 years or more. Acta Orthop. 2005;76(2):245–252. doi: 10.1080/00016470510030652. [DOI] [PubMed] [Google Scholar]
- 15.Latifi MH, Ganthel K, Rukmanikanthan S, Mansor A, Kamarul T, Bilgen M. Prospects of implant with locking plate in fixation of subtrochanteric fracture: experimental demonstration of its potential benefits on synthetic femur model with supportive hierarchical nonlinear hyperelastic finite element analysis. Biomed Eng Online. 2012;11:23. doi: 10.1186/1475-925X-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parker MJ, Bowers TR, Pryor GA. Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: a randomised trial of 600 fractures. J Bone Joint Surg Br. 2012;94(3):391–397. doi: 10.1302/0301-620X.94B3.28406. [DOI] [PubMed] [Google Scholar]
- 17.Yong C, Tan C, Penafort R. Dynamic hip screw compared to condylar blade plate in the treatment of unstable fragility intertrochanteric fractures. Malays Orthop J. 2009;3(1):1–5. doi: 10.3928/01477447-20090301-30. [DOI] [Google Scholar]