Abstract
Bilateral superficial cervical plexus block may help in reduction of postthyroidectomy pain. The aim of this study was to evaluate the influence of bilateral superficial cervical plexus block (BSCB) given either presurgically or postsurgically on analgesia in postthyroidectomy patients. Sixty adult euthyroid patients were randomly allocated to one of the three groups, to receive BSCB either presurgically (group A) or postsurgically (group B). Both of the above groups were compared with parenteral analgesics (group C). Thyroid surgery was performed according to a standardised procedure. Postoperative pain was assessed by visual analog scale (VAS), with 10 being the worst pain and 0 being no pain, when patient was fully awake and extubated (0) and after 1, 2, 4, 8, 12, 18, 24, 36 and 48 h. VAS was assessed at four phases: at rest, neck movements, vocalisation and swallowing. Total use of intraoperative fentanyl was noted. The time for first rescue analgesic was also noted. There was no significant statistical difference amongst three groups as regards demographic data and duration of surgery. Patients given BSCBs (either presurgically or postsurgically) had significant lower VAS at all four phases of pain assessment as compared to group C. The time for first rescue analgesia was the earliest in group C. We concluded that BSCB whether given presurgically or postsurgically significantly reduce pain intensity and opioids requirement in postoperative period after thyroid surgery.
Keywords: Bilateral superficial cervical plexus nerve block, Thyroid surgery, VAS, Analgesia, Presurgical and postsurgical
Introduction
Postthyroidectomy pain, which is significant, is treated traditionally either using NSAIDS which have the risk of increasing postoperative bleeding for a vascular organ like the thyroid without causing adequate analgesia or with narcotics which produce undue sedation with the risk of respiratory depression [1]. Superficial cervical plexus block (SCB), being a purely sensory block, appears to provide an ideal alternative. Moreover, its landmarks are simple and the block is technically easy to learn and master being a subcutaneous injection, avoiding risk of life-threatening complications associated with deep cervical block [2, 3].
A scientific basis for preemptive analgesia has demonstrated that changes occur in the spinal cord and brain in response to painful stimulation that results in enhanced pain transmission and ultimately enhanced pain perception [4]. Intraoperative and postoperative analgesia cannot be considered separately, and planning for postoperative analgesia should begin prior to surgery.
Thus, we decided to compare the analgesic efficacy of bilateral superficial cervical plexus block (BSCB) in thyroid surgery, one given preoperatively to assess the preemptive analgesia with a postsurgical/postoperative block and to compare the two with parenteral analgesia.
Material and Methods
After the ethical committee approval, 60 adult euthyroid patients of ASA grades I and II of either sex, undergoing elective thyroid surgeries were taken up. The patients were randomly divided into three groups of 30 each: group A, patients received BSCB preoperatively (after induction of general anaesthesia and before skin incision); group B, patients received BSCB postoperatively (after skin closure and before reversal) and group C, patients received only parenteral analgesics.
Patients with contraindication to regional anaesthesia or allergy to local anaesthetics were excluded from the study. Written informed consent was taken separately for the block explaining the involved risks/benefits. All the patients were familiarised with use of the visual analog score (VAS) preoperatively.
Patients were premedicated with tablet alprazolam 0.25 mg PO night before surgery. After establishing a standard monitoring, anaesthesia was induced with fentanyl 1–2 μg/kg i.v., propofol 2–3 mg/kg i.v. Orotracheal intubation was facilitated by the administration of vecuronium 1 mg/kg i.v. Anaesthesia was maintained with isoflurane (0.8–1.2 %) in N2O and O2 mixture. Thyroid surgery was performed according to a standardised procedure. Supplemental fentanyl was given in incremental doses of 1 μg/kg i.v. as and when required (rise in MAP or pulse rate by 20 % from the baseline value).
BSCBs were performed by the anaesthetist on both sides of neck in the following way: after placing an extension under the shoulders, the head was turned to one side and part preparation was done. A 12-ml 0.25 % bupivacaine solution was loaded, and a 22-gauge (B level) needle was inserted on the midpoint of the posterior border of sternocleidomastoid muscle. Four milliliters each was injected superiorly and inferiorly along the posterior border of sternocleidomastoid (Erbs point), while 4 ml was injected under the belly of the muscle after repeated negative aspirations. The head was turned to the opposite side and same procedure was repeated. The duration of surgery and total intraoperative fentanyl required were also noted. At the end of surgery, neuromuscular blockade was reversed, and patients were extubated after ensuring normal movements of the vocal cords by laryngoscopy.
The following parameters were observed in postoperative period: (a) Degree of analgesia, patients were assessed for analgesia at 0, 1, 2, 4, 8, 12, 18, 24, 36 and 48 h subjectively by the VAS. The VAS was assessed during four phases: at rest, on lateral rotation of the neck, during swallowing and while vocalisation. Rescue analgesics were given if the VAS ≥3 at rest or ≥5 on swallowing. If VAS ≤2 on rest and ≤4 on swallowing, no further analgesics were given. If the VAS was 3–5 on rest and 5–7 on swallowing, an injection of diclofenac 1–1.5 mg/kg i.m. was given. If the VAS was ≥6 on rest and ≥8 on swallowing, an injection of pethidine 1 mg/kg i.m. was given to patients. (b) Duration of analgesia was assessed from the time of reversal till such point when patient required first rescue analgesia. (c) Nausea and vomiting were treated with an injection of ondansetron 0.08 mg/kg i.v., and any complications due to block or surgery itself were looked for, such as respiratory distress, respiratory obstruction, Horner’s syndrome and hoarseness of voice.
Results
The study was conducted as double-blind randomised control trial by sealed envelope system. The prevention of postoperative pain after thyroid surgery by bilateral superficial cervical plexus blocks performed by Dieudonne found that morphine required in PACU in saline group was 6/40 (15 %) and in bupivacaine group was 4/40 (45 %). Taking these values as reference, the minimum required sample size with 80 % power of study and 5 % level of significance was 33 patients in each study group. Due to time constraint and dropouts, the sample size was taken as 30 per group.
Categorical variables were presented in numbers and percentages (%) and continuous variables as mean ± SD. Statistical tests were applied as ANOVA/Kruskal-Wallis test for quantitative data (when the data sets were not normally distributed) between the three groups, paired T test/Mann-Whitney test for quantitative variables (when the data sets were not normally distributed) within the groups and chi-square/Fisher’s exact test for qualitative data between and within the three groups. P value <0.05 was considered statistically significant.
There was no significant statistical difference between the three groups as regards demographic data and duration of surgery. The mean age was 31.80 ± 9.48, 32.45 ± 9.91 and 34.25 ± 10.01 years in groups A, B and C, respectively. Eight males and 12 females were included in group A, seven males and 13 females in group B and five males and 15 females were included in group C. The duration of surgery was 2.925 ± 0.06 h in group A, 3.100 ± 0.07 h in group B and 2.975 ± 0.05 h in group C.
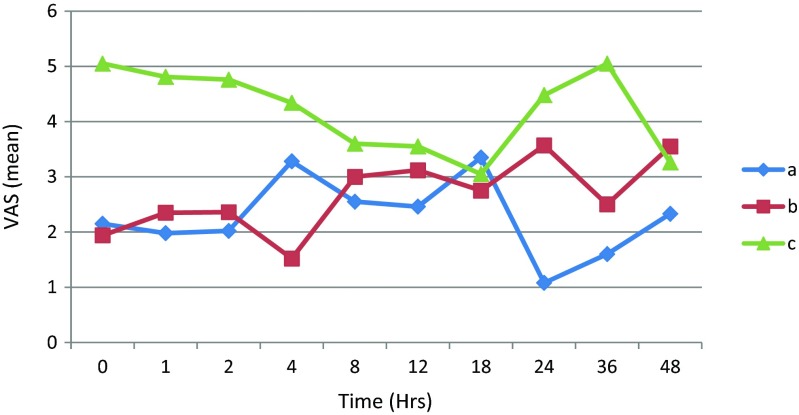
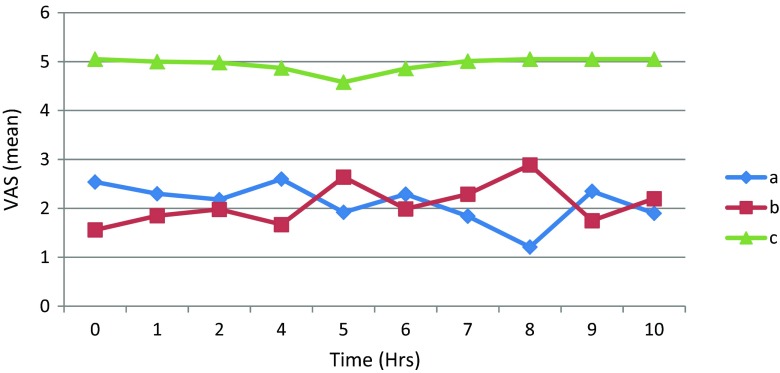
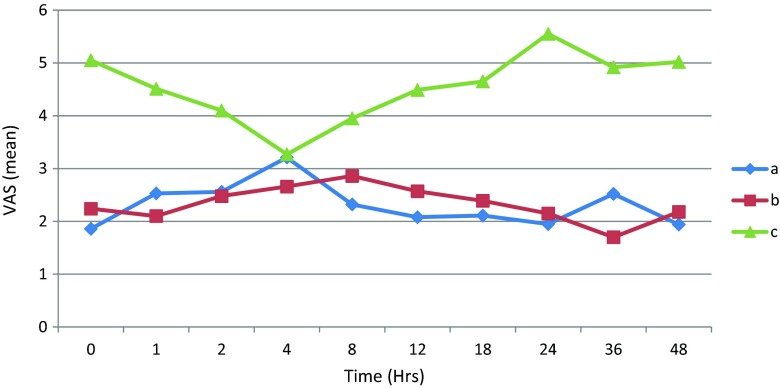
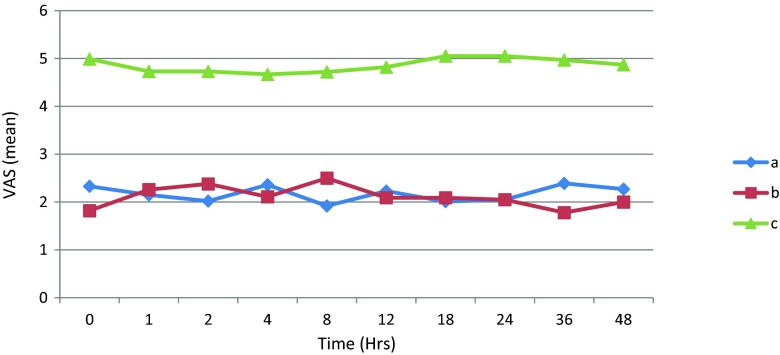
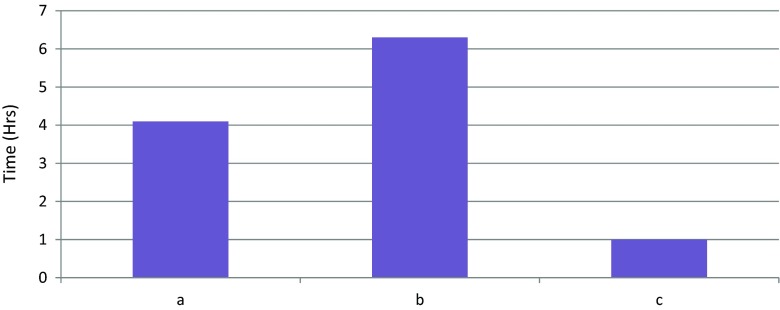
On comparing the mean VAS at rest, scores were significantly lower in group A (2.27) and group B (2.66) compared to group C (4.19) during the first 48 h (Fig. 1). At neck movements, there was a highly significant difference between groups A (2.11) and C (4.95) (p < 0.001) and groups B (2.08) and C (4.95) (p < 0.001; Fig. 2). At swallowing, there was a significant difference in overall mean VAS scores in group A (2.30) and group B (2.33) compared to group C (4.55) (p < 0.001; Fig. 3). While at vocalisation, a significant statistical difference was observed between groups A (2.17) and C (4.86) and groups B (2.10) and C (4.86) (p < 0.001; Fig. 4). The mean intraoperative fentanyl requirement was significantly higher in group B (143.5 ± 10 μg) and group C (138.25 ± 11 μg) as compared to group A (103.00 ± 08 μg) (p < 0.05). The need for first rescue analgesic was the earliest in group C patients (1.00 h), followed by group A (4 h), and last in group B (6.3 h) which was statistically significant (p < 0.001) as shown in Fig. 5. The total number of postoperative doses of rescue analgesics required was the highest in group C (7.25) followed by group A (5.40) and last in group B (4.65). Nausea and vomiting were reported minimally (<2 %) in groups A and B and incidence being around 30 % in group C. There were no major complications reported in any of the three groups related either to the surgery or the block.
Fig. 1.
Trends in postoperative VAS at rest
Fig. 2.
Trends in postoperative VAS at neck movements
Fig. 3.
Trends in postoperative VAS at vocalisation
Fig. 4.
Trends in postoperative VAS at swallowing
Fig. 5.
Time for first rescue analgesia
Discussion
The concept of multimodal analgesia has led to the use of cervical plexus block along with general anaesthesia for the perioperative pain relief during thyroidectomy [3]. Postthyroidectomy pain perception includes many components linked to deep and superficial layers of the wound and intraoperative neck position [5]. In our study, a comparison of presurgical with postsurgical BSCB was done for postoperative analgesia with parenteral analgesics. For pain assessment, VAS was chosen because it was more sensitive and was easy to follow in our group of patients [6]. VAS was assessed at four phases: rest, neck movements, swallowing and vocalisation.
On comparing the mean VAS at rest, we found that the mean scores were significantly lower in group A (2.27) and group B (2.66) during most of postoperative period as compared to group C (4.19) (Fig. 1). A similar trend was also noted in VAS scores during the other three phases of observation (swallowing, neck movements and vocalisation) (Figs. 2, 3 and 4).
This implies that patients receiving BSCB have superior quality of analgesia than those receiving only parenteral analgesic. It also implies that postthyroidectomy pain has primarily a superficial component.
Reviewing the literature, we found that both superficial and deep cervical plexus blocks have been used for analgesia during thyroidectomy. The superficial plexus block is a purely sensory block, covers the entire surgical area and has been found to be easy to learn and practise by most researchers [7–9]. We also found the block to be effective in all cases despite of a short learning curve [10]. Guay concluded that superficial cervical plexus block is easy to master, is effective and carries low risk of serious complications [10]. Pandit et al. found the superficial block to be comparable to combined approach with an equal degree of patient satisfaction [7]. Moreover, a systematic review of 69 studies comparing superficial, deep and combined approach found that superficial block provided an equal or better analgesia and was also safer than deep technique with lesser risk of complications [11]. Suh et al. also found SCB to be more effective than either combined and deep blocks in reducing incisional pain, headache and posterior neck pain following thyroidectomy [8].
We advocate both presurgical and postsurgical BSCB for analgesia in a patient planned for thyroid surgery as both techniques have their own advantages. Comparing analgesia, we found that patient receiving presurgical block required lesser intraoperative analgesia (103.00 ± 0.8 μg) but required early postoperative rescue analgesia (4 h). Patients with postsurgical block on other hand required higher intraoperative analgesia (143.5 ± 10 μg) but had better postoperative analgesia in terms of delayed rescue analgesia (6.3 h) and least number of total rescue analgesics (4.65). However, the total duration of analgesia (time of block to first rescue analgesia) was comparable in group A (4 + 2.9 h (duration of surgery)) and group B (6.3 h) ruling out any pre emptive advantage (Fig. 5).
Technically, presurgical block is easier to perform with clear cut landmarks except in patients with large thyroid swellings where preoperative anatomy may be distorted. While in postoperative blocks surgery may change the landmarks and dissection may cause local anaesthetic to leak into other facial planes. Herbland et al. comparing the presurgical with postsurgical block found the two to be comparable but contrarily not highly efficacious in postthyroidectomy pain control [12]. Messner et al. advised the use of presurgical block keeping in mind its preemptive effect [13].
The efficacy of BSCB has been further enhanced with additives to local anaesthetics. Addition of adrenaline can not only prolong the effect of the block but also reduce the peak plasma levels of local anaesthetics [10, 12]. Clonidine is also known to enhance the efficacy and duration of the block [14] and has been found to decrease postoperative nausea and vomiting [15]. BSCB alone and in combination with ketamine infusion has been successfully used as a sole anaesthetic for thyroid surgery [16].
To conclude, BSCB given presurgically or postsurgically is safe, simple and highly efficacious for perioperative analgesia for thyroid surgery and can be easily administered under a general anaesthesia without any serious complications. We advocate its routine use for all thyroid surgeries.
Acknowledgments
Conflict of Interest
None.
References
- 1.Lacoste L, Thomas D, Kraimps JL, Chabin M, Ingrand, Barbier J, et al. Post thyroidectomy analgesia: morphine, buprenorphine, or bupivacaine? J Clin Anesth. 1997;9:189–193. doi: 10.1016/S0952-8180(97)00038-X. [DOI] [PubMed] [Google Scholar]
- 2.Negmi H, Moustafa A, Rabie M, Kamal A, Sobhi S. The influence of bilateral superficial cervical plexuses block (BSCBs) as pre-emptive analgesia on patient satisfaction after thyroid surgery. Alex J Anesth Intensive Care. 2005;8:11–16. [Google Scholar]
- 3.Shih ML, Duh QY, Hsieh CB, Liu YC, Lu CH, Wong CS, et al. Bilateral superficial cervical plexus block combined with general anesthesia administered in thyroid operations. World J Surg. 2010;34(10):2338–2343. doi: 10.1007/s00268-010-0698-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woolf CJ, Chong MS. Pre-emptive analgesia: treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362–379. doi: 10.1213/00000539-199377020-00026. [DOI] [PubMed] [Google Scholar]
- 5.Dieudonne NMD, Gomola AMD, Bonnichon PMD, et al. Prevention of postoperative pain after thyroid surgery. A double blind randomised study of bilateral superficial cervical plexus blocks. Anesth Analg. 2001;92:1538–1542. doi: 10.1097/00000539-200106000-00038. [DOI] [PubMed] [Google Scholar]
- 6.Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anesthesia and surgery. Br J Anaesth. 2000;84:6–10. doi: 10.1093/oxfordjournals.bja.a013383. [DOI] [PubMed] [Google Scholar]
- 7.Pandit JJ, Bree S, Dillon P, Elcock D, McLaren ID, Crider B. A comparison of superficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: a prospective, randomised study. Anesth Analg. 2000;91(4):781–786. doi: 10.1097/00000539-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Suh YJ, Kim YS, In JH, Joo JD, Jeon YS, Kim HK. Comparison of analgesic efficacy between bilateral superficial and combined (superficial and deep) cervical plexus block administered before thyroid surgery. Eur J Anaesthesiol. 2009;26(12):1043–1047. doi: 10.1097/EJA.0b013e32832d6913. [DOI] [PubMed] [Google Scholar]
- 9.Weiss A, Isserhorst C, Gahlen J, Freudenberg S, Roth H, Hammerschmitt N. Acute respiratory failure after deep cervical plexus block for carotid endarterectomy as a result of bilateral recurrent laryngeal nerve paralysis. Acta Anesthesiol Scand. 2005;49(5):715–719. doi: 10.1111/j.1399-6576.2005.00694.x. [DOI] [PubMed] [Google Scholar]
- 10.Guay J. Regional anesthesia for carotid surgery. Curr Opin Anaesthesiol. 2008;21(5):638. doi: 10.1097/ACO.0b013e328308bb70. [DOI] [PubMed] [Google Scholar]
- 11.Pandit JJ, Satya Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth. 2007;99(2):159–169. doi: 10.1093/bja/aem160. [DOI] [PubMed] [Google Scholar]
- 12.Herbland A, Cantini O, Reynier P, Valat P, Jougon J, Arimone Y, Janvier G. The bilateral superficial cervical plexus block with 0.75% ropivacaine administered before or after surgery does not prevent postoperative pain after total thyroidectomy. Reg Anesth Pain Med. 2006;31(1):34–39. doi: 10.1097/00115550-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Messner M, Albrecht S, Lang W, Sittl R, Dinkel M. The superficial cervical plexus block for postoperative pain therapy in carotid surgery. A prospective randomised controlled trial. Eur J Vasc Endovasc Surg. 2007;33(1):50–54. doi: 10.1016/j.ejvs.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 14.Andrieu G, Amrouni H, Robin E, Carnaille B, Wattier JM, Pattou F, et al. Analgesic efficacy of bilateral superficial cervical plexus block administered before thyroid surgery under general anesthesia. Br J Anaesth. 2007;99(4):561–566. doi: 10.1093/bja/aem230. [DOI] [PubMed] [Google Scholar]
- 15.Karthikeyan VS, Sistla SC, Badhe AS, Mahalakshmy T, Rajkumar N, Manwar S, Gopalkrishnan S. Randomized controlled trial on the efficacy of bilateral superficial cervical plexus block in thyroidectomy. Pain Pract. 2013;13(7):539–546. doi: 10.1111/papr.12022. [DOI] [PubMed] [Google Scholar]
- 16.Mukhopadhyay S, Niyogi M, Dutta M, Ray R, Gayen GC, Mukherjee M, et al. Bilateral superficial cervical plexus block with or without low dose intravenous ketamine analgesia: effective, simple, safe, and cheap alternative to conventional general anesthesia for selected neck surgeries. Local Reg Anesth. 2012;5:1–7. doi: 10.2147/LRA.S28360. [DOI] [PMC free article] [PubMed] [Google Scholar]