Abstract
Dacron heart patch has been used in decompressive craniectomy, performing the function of septa, mainly to prevent extra adhesion of temporal muscle and decompressive meningeal adhesion in the second-stage cranioplasty, so as to make the operation easier. Then, we made the following modification technology: (1) We used artificial suturing-free dura participate directly in the duraplasty. (2) Dacron patch is not in need of trimming the side holes and can directly cover the decompression window. From March 2012 to October 2013, we applied the technology of artificial dura with Dacron heart patch in 23 patients; after operation, we found that the initial depressive craniectomy cost less time, due to the tension-reduced suture which was not needed, and in the second-stage cranioplasty, the temporal was easy to remove and had no adhesion with the Dacron patch, so as to reach temporal muscle anatomy preservation, and with no obvious postoperative complication.
Keywords: Dacron heart patch, Manual suturing-free dura, Decompressive craniectomy operation, Cranioplasty, Temporal muscle anatomy preservation
Introduction
In cranioplasty, the improper operation may cause a series of problems as follows: (1) Too thick flap may easily lead to rupture of dura, and too thin flap easily leads to poor blood circulation in it and even rupture during stripping; (2) the flap stripping will cause large indirect pull to the brain tissue, leading to cerebral contusion, secondary intracranial hemorrhage, epilepsy, and so on; (3) anatomy and blood supply of temporal muscle can be greatly disturbed in the second operation, which may lead to the increase of bleeding during the operation, and interfere normal morphology of the temporal muscle, and even cause temporal muscle atrophy after operation [1–3]. In fact, the artificial stripping and forming of skin flap and dura are the technique key in cranioplasty. Therefore, we considered whether we could choose a kind of material to be placed between the dura and subcutaneous in the decompressive craniectomy which could be used as artificial isolation layer in the second-stage cranioplasty to make the subcutaneous tissue easy to separate with the decompressive dura, thereby reducing the occurrence of stripping complications. Based on our experiences and previous reports [4–6], we have used Dacron heart patch as temporary patch in craniectomy. This method does not interfere with temporal muscle in the second-stage cranioplasty, so the temporal muscle anatomy level had no any change. We also referred to the work of many peers and chosen the Dacron heart patch as a temporary spacer; in the practice, we found that patch indeed played a good role; the operation time of the second cranioplasty shortened obviously, and the complications after operation decreased. But the following problems were found in the using process: (1) endocranium-enlarged cranioplasty needs to take autologous fascia or periosteum in operation, which can lead to the prolongation of decompression operation time and (2) trimming Dacron side hole for granulation penetrating growth to reduce postoperative effusion, but which could slightly aggravate the stripping difficulty in the second-stage cranioplasty. Therefore, aiming at these problems, we made the improvement, using artificial suturing-free dura and directly covering to reduce tension of dura, without trimming patch side hole, and the surrounding was no longer fixed. The improved technology was applied to 23 patients, and the operation time of decompressive craniectomy and operative complications were observed, for investigating the effect of this technology.
Materials and Methods
Decompressive Craniectomy
Control Group (30 Patients)
Routine frontotemporal tongue-shaped decompressive flap was made, with one-time shaping of myocutaneous flap. After drilling 5–6 holes, the bone flap was removed. Under the decompression window, the decompression should be ensured to reach the bottom of the middle cranial fossa. After treating the brain lesion, the autologous fascial flap was pruned for tension-reduced dura. When necessary, the thigh lata fascia was taken for repair, and Dacron heart patch (Shanghai Chest Medical Technological Co., Ltd., Shanghai, China), slightly larger than the decompressive window, was used to cover the decompression window; paying special attention to at least one edge of the patch should be significantly greater than the decompression window (we generally fixed the position on the forehead part), to be quickly found out in the second stage. Patch was properly pruned, 5–6 fine pores, in favor of granulation inward growth to reduce the incidence of effusion after operation, and which was loosely fixed around with the silk thread, suturing the scalp, paying attention to the para-position suture of the temporal muscle.
Improvement Group (23 Patients)
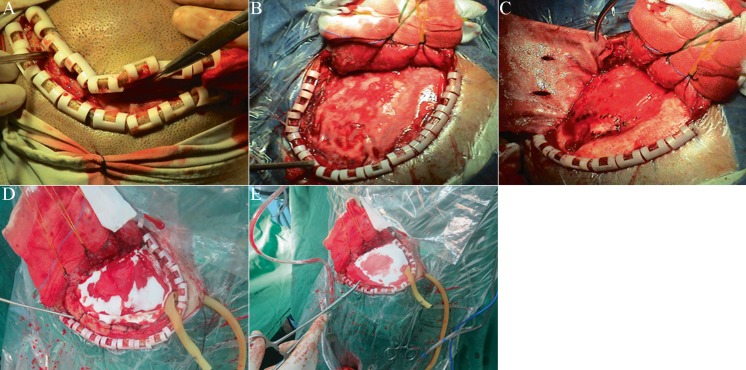
The decompressive craniectomy was performed with improvements mainly as follows: (1) The artificial suturing-free dura patch participated directly in dura cranioplasy. After the dura was removed along the original direction, the same size of artificial suturing-free dura patch (DuraMsx, Beijing Tianyifu Company) covered the decompression window (Fig. 1d). (2) Dacron patch was not pruned at the side hole and covered directly over the decompression window (Fig. 1e). (3) Dacron patch was no longer in need of fixation.
Fig. 1.
a After cutting the skin, finding out the edge of the spacer, expanding the incision along the edges of septa was continued. b Dissecting the flap, the spacer surface was visibly smooth, and the corresponding temporal muscle flap was relatively free of adhesions. c The spacer was stripped out, and it was not visible adhesion with the subcutaneous. d After the technology improvement, the suturing-free artificial dura patch was used to cover, to reduce the tension of dura. e Placement of the spacer: paying attention to at least one edge should exceed the bone window, no longer pruning the pores, and the surrounding was no longer fixed
Cranioplasty
Along the original incision, the incision was first cut in the front (Fig. 1a), paying attention first to finding out the patch edge; then, along the patch, the flap was further expanded and cut, and due to good isolation effect of the patch, thus, stripping was very smooth and quick. Then, the patch was removed (Fig. 1b), which was almost found having no adhesion beneath the meningeals (Fig. 1c); after putting back the bone flap, the skin was sutured.
Results
Operation Time of Decompressive Craniectomy
In the initial decompressive craniectomy in the improvement group, the artificial suturing-free dura patch was used to cover the decompression window, without tension-reduced suturing using periosteum or fascia lata. The average operation time in the improvement group was 90.43 ± 7.45 min, which was significantly shorter than 130.13 ± 13.64 min in the control group (P < 0.01).
Operative Complications
After the second-stage cranioplasty, both the control group and improvement group obtained good recovery, without infection, subcutaneous effusion, or rejection reaction. No secondary intracranial hemorrhage or secondary epilepsy was found in the two groups. There was no statistical significance of the above complication between the two groups.
Discussion
Severe craniocerebral injury, cerebral edema, and acute cerebral hernia often had to be underwent during the decompression craniectomy operation [7, 8], and along with which, the second-stage cranioplasty will be faced. Although the cranioplasty belongs to the basic level operation, there are still some complications, such as cerebrospinal fluid leakage, infection, hemorrhage, dropsy, epilepsy, and others [1, 9, 10]; key comprehensive points of the second-stage cranioplasty is “artificial meningeal” stripping and forming; if the striping is smooth, it will contribute to short operation time, less bleeding, meningeal integrity, the suitable thickness flap, and small stretch to the brain tissue, which is followed by reduced postoperative complications. Therefore, in turn, some of the work in the first decompression craniectomy appears very important, for example, whether we can choose a material to be arranged between the meningeal and subcutaneous, to be used as artificial isolation spacer, to make the subcutaneous tissue easy to separate with the decompressive meningeal, thereby reducing stripping complications, and using this way in the second-stage operation does not interfere with temporal muscle, so that the temporal muscle anatomy level had no any change. Therefore, the domestic and foreign counterparts have done a lot of work on this problem. Alessandro Di Rienzo et al. [11] inverted the incised decompressive dura to package the temporal muscle, and another dura patch was sutured with the meningeal, so that the temporal muscle can be easily isolated in the second-stage cranioplasty; Paolo Missori et al. [12] used double dual patch (bovine pericardial technology), which also can relieve adhesions of muscle flap; Bulters D and Belli A [13] used silicon as the isolation material; Tetsuro Kawaguchi et al. [4] used the similar repair spacer, but the patch only covered the temporal and not large range covering the whole decompressive window; therefore, when the flap was separated, there was a part of flap adhesion; Shigeru Miyake et al. [5] used ePTFE patch, which was placed under decompressive meningeal, and was not removed later; Setsuko Nakagawa [10] reported that infection rate after using ePTFE patch increased significantly; Antonis Vakis [6] used the patch and removed later, but we had made some improvements on their basis, and combined with the use of suturing-free artificial dura, greatly saved the time of primary decompression operation, at the same time did not increase the adhesion probability.
It was seen from the results that the Docan heart patch reached the effect that we needed. First, the spacer had very good tissue compatibility, and there was no patient who had rejection; second, the spacer had no adhesion with the brain tissue and subcutaneous tissue, easy to be stripped, which can make the operation bleeding volume decrease and save the operation time.
In the decompressive craniectomy operation, the tension-reduced suture of dura has been accepted by everyone, because it can keep the stability of cerebrospinal fluid circulation and prevent the spilling over. The current tension material generally has four kinds: (1) the autogenous fascia [14–16] such as autogenous periosteum, fascia lata, and galea, etc.; we initially used autologous periosteum or fascia for repair, and its advantage is obtaining raw material locally, which does not need disinfection and with no rejection; (2) Allogeneic dura mater repair materials [17]: this material rejection is light and suitable for a long time preservation, but may have viral infections; (3) xenogeneic dural repair materials [18]: mainly is animal pericardium, which has the advantages of rich source, good tissue compatibility, and which has the disadvantage of the possibility of aseptic inflammation, in addition to longer absorption time; (4) artificial dura mater repairing material [19, 20] is updated faster, for example, the Dacron heart patch that we used is actually such materials. In the usage process, we gradually select the Dacron heart patch as a temporary spacer; sometimes or occasionally, it was no longer removed, as long-term repair, with no rejection and cerebrospinal fluid leakage. Artificial suture-free dura can directly cover tension-reduced incision, in effect, which can save the meningeal suturing time and does not increase the risk of late adhesion.
In summary, in the second-stage cranioplasty, Dacron heart patch can be used as a good medium, with function of septum. It makes the flap stripping easier. The combination of artificial suturing-free dura and Dacron heart patch technology can shorten the operation time of decompressive craniectomy, without increasing the complications of the second-stage cranioplasty.
Footnotes
Fei Wang and Yan Xue contributed equally to this work.
References
- 1.Jaberi J, Gambrell K, Tiwana P, Madden C, Finn R. Long-term clinical outcome analysis of poly-methyl-methacrylate cranioplasty for large skull defects. J Oral Maxillofac Surg. 2013;71:81–88. doi: 10.1016/j.joms.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 2.Rocque BG, Amancherla K, Lew SM, Lam S. Outcomes of cranioplasty following decompressive craniectomy in the pediatric population. J Neurosurg Pediatr. 2013;12:120–125. doi: 10.3171/2013.4.PEDS12605. [DOI] [PubMed] [Google Scholar]
- 3.Walcott BP, Kwon CS, Sheth SA, Fehnel CR, Koffie RM, Asaad WF, Nahed BV, Coumans JV. Predictors of cranioplasty complications in stroke and trauma patients. J Neurosurg. 2013;118:757–762. doi: 10.3171/2013.1.JNS121626. [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi T, Hosoda K, Shibata Y, Koyama J. Expanded polytetrafluoroethylene membrane for prevention of adhesions in patients undergoing external decompression and subsequent cranioplasty. Neurol Med Chir (Tokyo) 2003;43:320–323. doi: 10.2176/nmc.43.320. [DOI] [PubMed] [Google Scholar]
- 5.Miyake S, Fujita A, Aihara H, Kohmura E. New technique for decompressive duraplasty using expanded polytetrafluoroethylene dura substitute. Neurol Med Chir (Tokyo) 2006;46:104–106. doi: 10.2176/nmc.46.104. [DOI] [PubMed] [Google Scholar]
- 6.Vakis A, Koutentakis D, Karabetsos D, Kalostos G. Use of polytetrafluoroethylene dural substitute as adhesion preventive material during craniectomies. Clin Neurol Neurosurg. 2006;108:798–802. doi: 10.1016/j.clineuro.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 7.Bender A, Heulin S, Röhrer S, Mehrkens JH, Heidecke V, Straube A, Pfefferkorn T. Early cranioplasty may improve outcome in neurological patients with decompressive craniectomy. Brain Inj. 2013;27:1073–1079. doi: 10.3109/02699052.2013.794972. [DOI] [PubMed] [Google Scholar]
- 8.Bobinski L, Koskinen LO, Lindvall P. Complications following cranioplasty using autologous bone or polymethylmethacrylate-retrospective experience from a single center. Clin Neurol Neurosurg. 2013;115:1788–1791. doi: 10.1016/j.clineuro.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 9.de Monaco BA, Fonoff ET, Teixeira MJ. Early resorption of an artificial bone graft made of calcium phosphate for cranioplasty: case report. Neuropsychiatr Dis Treat. 2013;9:1801–1802. doi: 10.2147/NDT.S43806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nakagawa S, Hayashi T, Anegawa S, Nakashima S, Shimokawa S, Furukawa Y. Postoperative infection after duraplasty with expanded polytetrafluoroethylene sheet. Neurol Med Chir (Tokyo) 2003;43:120–124. doi: 10.2176/nmc.43.120. [DOI] [PubMed] [Google Scholar]
- 11.Di Rienzo A, Iacoangeli M, Alvaro L, Colasanti R, Nocchi N, Di Somma LG, Scerrati M. Autologous vascularized dural wrapping for temporalis muscle preservation and reconstruction after decompressive craniectomy: report of twenty-five cases. Neurol Med Chir (Tokyo) 2013;53:590–595. doi: 10.2176/nmc.oa2013-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Missori P, Polli FM, Peschillo S, D’Avella E, Paolini S, Miscusi M. Double dural patch in decompressive craniectomy to preserve the temporal muscle: technical note. Surg Neurol. 2008;70:437–439. doi: 10.1016/j.surneu.2007.03.029. [DOI] [PubMed] [Google Scholar]
- 13.Bulters D, Belli A. Placement of silicone sheeting at decompressive craniectomy to prevent adhesions at cranioplasty. Br J Neurosurg. 2010;24:75–76. doi: 10.3109/02688690903506135. [DOI] [PubMed] [Google Scholar]
- 14.Li CC, Chang SC, Fu JP, Tzeng YS, Wang CH, Chen TM, Chen SG. Comparison of hatchet-shaped tensor fascia lata flap and pedicle anterior lateral thigh flap for treatment of trochanteric sores: a retrospective analysis of 48 patients. Ann Plast Surg. 2013;71:659–663. doi: 10.1097/SAP.0b013e3182586fac. [DOI] [PubMed] [Google Scholar]
- 15.Matros E, Disa JJ. Discussion: Fascia lata allografts as biological mesh in abdominal wall repair: preliminary outcomes from a retrospective case series. Plast Reconstr Surg. 2013;132:640–641. doi: 10.1097/PRS.0b013e31829fe14e. [DOI] [PubMed] [Google Scholar]
- 16.Shimada K, Ishikura N, Heshiki T, Kawakami S. Treatment for chronic abscess after cranioplasty: reconstruction of dura maters using the anterolateral thigh flap with fascia lata. J Craniofac Surg. 2007;18:1305–1308. doi: 10.1097/scs.0b013e31811ec238. [DOI] [PubMed] [Google Scholar]
- 17.Laun A, Tonn JC, Jerusalem C. Comparative study of lyophilized human dura mater and lyophilized bovine pericardium as dural substitutes in neurosurgery. Acta Neurochir (Wien) 1990;107:16–21. doi: 10.1007/BF01402607. [DOI] [PubMed] [Google Scholar]
- 18.Vanaclocha V, Saiz-Sapena N. Duraplasty with freeze-dried cadaveric dura versus occipital pericranium for Chiari type I malformation: comparative study. Acta Neurochir (Wien) 1997;139:112–119. doi: 10.1007/BF02747190. [DOI] [PubMed] [Google Scholar]
- 19.Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006;104:469–479. doi: 10.3171/jns.2006.104.4.469. [DOI] [PubMed] [Google Scholar]
- 20.Knopp U, Christmann F, Reusche E, Sepehrnia A. A new collagen biomatrix of equine origin versus a cadaveric dura graft for the repair of dural defects—a comparative animal experimental study. Acta Neurochir (Wien) 2005;147:877–877. doi: 10.1007/s00701-005-0552-0. [DOI] [PubMed] [Google Scholar]