Abstract
Sonography is an important clinical tool in diagnosing appendicitis in children as it can obviate both exposure to potentially harmful ionising radiation from computed tomography scans and the need for unnecessary appendicectomies. This review examines the diagnostic accuracy of ultrasound in the identification of acute appendicitis, with a particular focus on the the utility of secondary sonographic signs as an adjunct or corollary to traditionally examined criteria. These secondary signs can be important in cases where the appendix cannot be identified with ultrasound and a more meaningful finding may be made by incorporating the presence or absence of secondary sonographic signs. There is evidence that integrating these secondary signs into the final ultrasound diagnosis can improve the utility of ultrasound in cases where appendicitis is expected, though there remains some conjecture about whether they play a more important role in negative or positive prediction in the absence of an identifiable appendix.
Keywords: Appendicitis, child, paediatrics, ultrasonography
Introduction
Acute appendicitis is the most common emergency presentation requiring surgical intervention in both adults and children. During 2013–2014 in Australia, almost 29,000 appendicectomies were performed, comprising approximately 10% of all emergency surgery.1 Since the 1980s, ultrasound has been commonly used to diagnose appendicitis with a range of reported sensitivities (71.2–99%) and specificities (91.3–98.2%).2, 3, 4, 5, 6, 7, 8, 9 There is currently some debate about the best imaging modality or combination of modalities to accurately and cost‐effectively diagnose the condition. Studies have variously advocated ultrasound in all presentations,10 as a first‐line modality,11, 12, 13 and even inappropriate as it delays treatment.14 Pershad et al. found that performing ultrasound on all children with suspected appendicitis was the most cost‐effective diagnostic approach.15
Computed tomography (CT) provides a more accurate diagnosis of appendicitis than ultrasound and a high negative predictive value (NPV), however its inherent radiation risks warrant cautionary use in children with suggestion that it be used only as a staged or complementary second‐line modality.16, 17, 18, 19, 20, 21 Children are reported to be 10 times more sensitive to the effects of ionising radiation than adults,22 yet Rice et al.23 have found that clinicians have a limited knowledge of the radiation risk posed by CT. Children in a non‐paediatric hospital are 4–5 times more likely to undergo a CT scan than those in a paediatric hospital.24, 25 Improved accuracy and the development of definitive guidelines for the use of ultrasound in the diagnosis of suspected appendicitis would provide surgeons with improved decision‐making ability and reduce the need to expose children to the potentially harmful effects of CT, particularly in non‐paediatric health facilities.
Magnetic resonance imaging (MRI) has also been used in the assessment of paediatric appendicitis demonstrating similar diagnostic results to CT without the ionising radiation.26 MRI has shown to have a higher positive predictive value (PPV) than sonography but otherwise similar diagnostic accuracy.27 Interestingly, MRI is often unable to visualise the appendix in between 30% and 53% of cases, yet it maintains a very high NPV (99–100%).28, 29, 30 MRI may potentially be used as a first‐line imaging modality in children with suspected appendicitis31 or as a second‐line study after an equivocal ultrasound26 as an ionising radiation‐free alternative to CT, though cost and magnet availability are prohibitive in many clinical settings at present.
While dedicated paediatric sonographers are more likely than their general counterparts to locate the appendix,32, 33 many children do not present to specialist paediatric departments. Definitive sonographic criteria or techniques that improve accuracy and assist diagnosis would be of particular benefit in these cases. Secondary signs of appendicitis are well established with a recent investigation of their predictive value identifying potential diagnostic use in the absence of an identifiable appendix.3, 34, 35 The purpose of this review is to examine appendiceal sonography, established sonographic criteria, paediatric‐specific techniques and the predictive value of secondary signs.
Method
A review of literature was conducted by searching electronic databases for relevant keywords. MEDLINE (PubMed) was searched using Medical Subject Headings (MeSH): Appendicitis and Ultrasound and Children. A search of PubMed, Web of Science, and Scopus using the keywords: paediatric or pediatric; ultrasound or sonography or ultrasonography; and appendicitis, yielded approximately 300 articles. While articles were restricted to relevance to a paediatric population, some articles that were considered significant with respect to technique, criteria, and epidemiology were also included, despite not having a solely paediatric focus. Articles that significantly dealt with secondary sonographic signs (see Table 1) were further interrogated with the Web of Science citation map to include cited works. From these searches, 105 articles were examined, of which 56 have been included in this review. Criteria for exclusion were articles that were adult rather than paediatric focussed unless secondary sonographic signs were specifically mentioned, or if they were not primarily centred on ultrasound as a modality. Articles published within the last 10 years were used, however some seminal works that established current practice guidelines were also included despite being now over several decades old.
Table 1.
Summary of publications with emphasis on secondary sonographic signs of appendicitis
| Author | Year | Comments |
|---|---|---|
| Kessler et al.36 | 2004 | Prospective study of 125 patients, not limited to children. There is examination of the diagnostic qualities of some secondary signs: inflammatory fat changes (SN 91%, SP 76%), caecal wall thickening (SN 25%, SP 88%), lymph nodes (SN 32%, SP 62%) and peritoneal fluid (SN 51%, SP 71%). |
| Lee et al.34 | 2009 | Prospective study of 317 adult patients. Found that an increased intra‐abdominal fat echo was seen in patients with appendicitis (SN 73%, SP 98%). |
| Rodriguez et al.37 | 2006 | Retrospective study of 769 children that underwent appendicectomy. Increased echogenic fat was seen more in children under 5 years (15%) compared to older children (4%). |
| Wiersma et al.3 | 2009 | Prospective study of 212 children. Integrated secondary sonographic signs into their findings and found their absence to be a safe negative predictor without a visible appendix and a strong positive predictor of appendicitis when present (SN 99%, SP 97%, PPV 93%, NPV 99%). |
| Jaremko et al.38 | 2011 | Retrospective study of 189 children integrating secondary sonographic signs into their findings and also identified that inconclusive ultrasounds were more likely in children older than 12 years (SN 88%, SP 89%, PPV 80%, NPV 93%). |
| van Atta et al.39 | 2014 | Prospective study of 512 children using CT for equivocal cases and integrating secondary signs into their findings (SN 96%, SP 97%, PPV 94%, NPV 98%). |
SN, sensitivity; SP, specificity; PPV, positive predictive value; NPV, negative predictive value; CT, computed tomography.
Pathogenesis and potential risks
Appendicitis typically develops over a period of 24–36 h, and potentially in half that time period in young children.40 After the appendiceal lumen is obstructed by an appendicolith or foreign body, it distends and initially presents as peri‐umbilical pain when the T8–T10 visceral nerves are stimulated.41 Intra‐luminal pressure continues to increase, mucosal perfusion is reduced and bacteria begin invading the wall with inflammation eventually spreading into the adjacent mesentery causing localised right lower quadrant (RLQ) pain as the nerves of the peritoneum become stimulated.42 If left untreated, the reduction in perfusion to the appendiceal wall and loss of mucosal integrity can lead to gangrene and perforation resulting in longer, more complicated admissions and higher morbidity.37, 43 Rodriguez et al.37 found that the risk of perforation is inversely proportional to a child's age. Negative appendectomies, the surgical removal of a normal appendix due to a false positive diagnosis, are reported to result in a longer hospital stay, higher mortality rate and are consequently more expensive to treat than for patients with appendicitis, highlighting the need for more accurate pre‐surgical diagnoses.43
Sonographic technique
The use of ultrasonography in the diagnosis of appendicitis in children is well‐established but remains a challenging examination for sonographers not comfortable or confident with paediatrics. Children have unique attributes that must be considered during the examination. They are already experiencing pain‐induced discomfort, have usually been subjected to clinical examinations and often cannulation. This can predispose them to fear further medical procedures such as an ultrasound examination, potentially reducing their compliance and limiting the success of the procedure. Parents/carers should be present and have the procedure explained to them so that they remain calm for their child and have reasonable expectations of the diagnostic findings. Obtaining a clinical history from paediatric patients is often difficult as verbal development may be limited and so the parent/carer's observations of the child preceding the examination are invaluable. The scan of the RLQ is an extension of the physical examination and while an indication of a broad region of pain may not be of great assistance, specific localisation can expedite the search for an inflamed appendix.44, 45
The seminal work on appendix sonography by Puylaert9 described the graded compression technique that remains in use today. A linear transducer is used to gradually apply pressure to the RLQ to compress and displace the bowel and its contents, ideally permitting identification of the appendix that lies beneath. The ascending colon is identified in the transverse plane by its gassy signature and the probe is then moved inferiorly towards the caecum while applying compression. Adequate compression is achieved when the psoas and iliac vessels can be identified, as the appendix will be anterior to these structures, though the ability to apply sufficient compression can be limited by inability of the child to tolerate any associated discomfort. There is considerable variation in the ability to sonographically locate the normal appendix with success ranging from as high as 82% to as few as 2% identified.37, 46
The development of complementary techniques such as posterior manual compression, where the sonographer's left hand provides anterior force to the patient's right lower back above the ileum in order to reduce the distance to a high frequency transducer allow better identification of deeper appendices.12 When utilising the bladder as an acoustic window or a right posterior approach for retro‐caecal appendices, a lower frequency curvilinear transducer can be useful without using compression.5 This lower frequency transducer may be helpful when dealing with obese children where a body mass index greater than 85th percentile has been shown to result in significantly lower diagnostic accuracy with sonography.47
Sonographic criteria
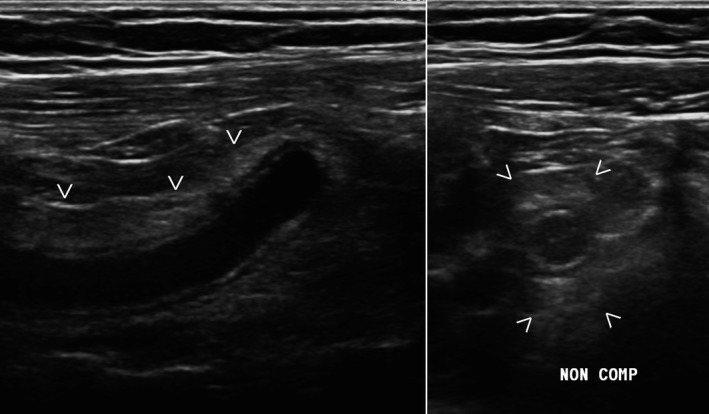
There are a wide variety of documented sonographic criteria for diagnosing appendicitis, with some more commonly accepted than others. The maximum outside diameter (MOD) is commonly used and is determined by measuring the outer borders of the hypoechoic tunica muscularis (Fig. 1). It is important to note that the measurement is performed when the appendix is compressed using the graded compression technique to prevent false positives and ensure a degree of repeatability. A normal appendix will compress and be less than 6 mm, while an inflamed appendix is usually both enlarged and importantly, non‐compressible.36 There are conflicting views regarding the significance of the appendiceal diameter, with Kessler et al.'s36 finding that it is the most accurate predictor. In contrast, Rettenbacher et al.48 stated that it should not be used as the sole predictor of appendicitis because the diameter can increase in response to other RLQ inflammation. Of particular note are children with cystic fibrosis who have a lower incidence of appendicitis than the general population, yet the specificity of sonography can be compromised by dilation of the normal appendiceal lumen with mucoid material increasing the likelihood of a false positive diagnosis based on MOD.49, 50
Figure 1.
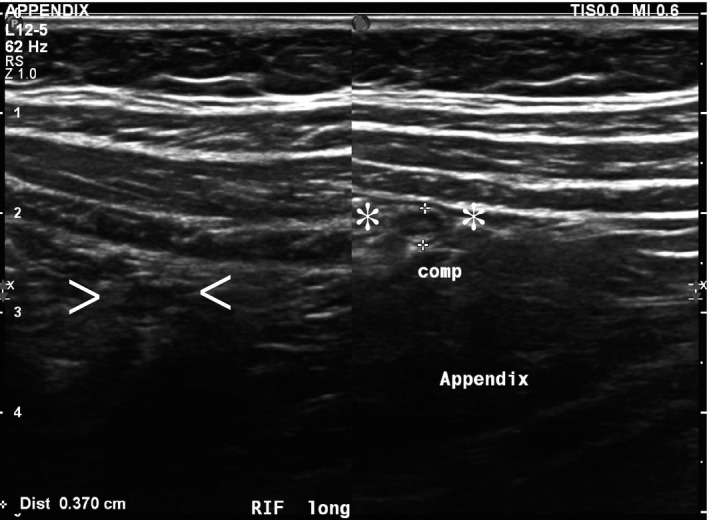
The outside diameter of the compressed appendix (asterisks) of 4 mm and uncompressed (arrowheads) on the left.
Other traditional signs are the presence of an appendicolith and the colour Doppler characteristics of the appendix wall. An appendicolith is highly reflective and casts a posterior acoustic shadow, yet are only seen in 50% of paediatric cases (Fig. 2).40 Increased colour Doppler flow within the appendiceal wall is a useful sonographic sign for confirmation of appendicitis with a specificity of 96%, but a low sensitivity of only 52% renders it a poor criterion (Fig. 3).36 Similarly, intra‐luminal air is not a reliable indicator of acute appendicitis as it is found in both normal and inflamed appendices and can be easily confused with dirty shadowing from normal faeces or a small appendicolith.36, 46 Measurement of the appendiceal wall has also been used as a potential indicator of appendicitis, but is technically difficult to reliably perform as the inflammation of the mucosa may have a similar hypoechoic appearance to intra‐luminal pus (Fig. 4).36
Figure 2.
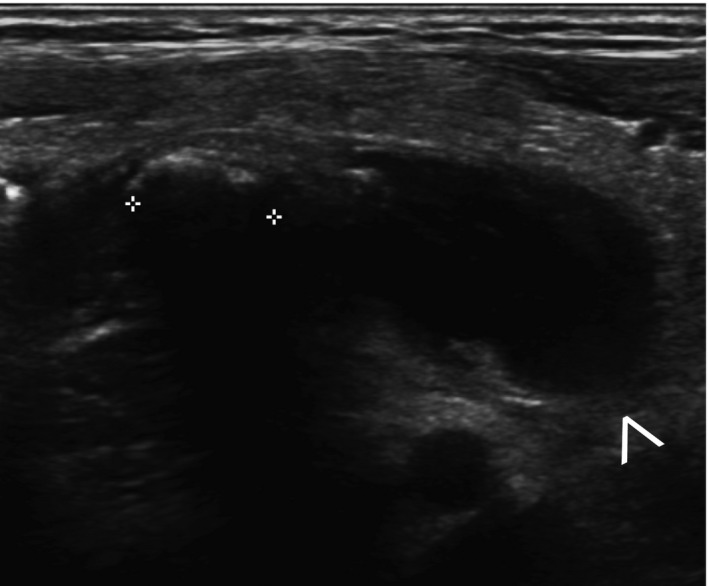
An appendicolith (between electronic calipers) is seen demonstrating acoustic shadowing within the appendiceal lumen, proximal to the distended tip (arrowhead).
Figure 3.
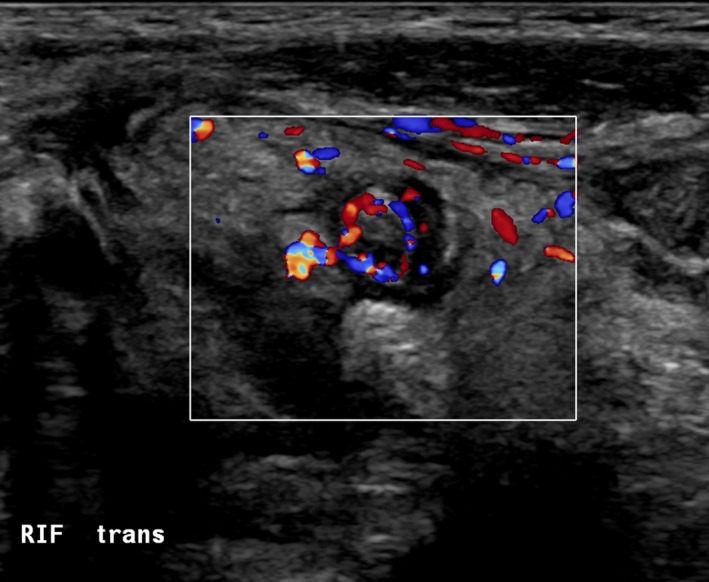
A transverse image of an inflamed appendix with colour Doppler indicating increased blood flow to the appendiceal wall.
Figure 4.
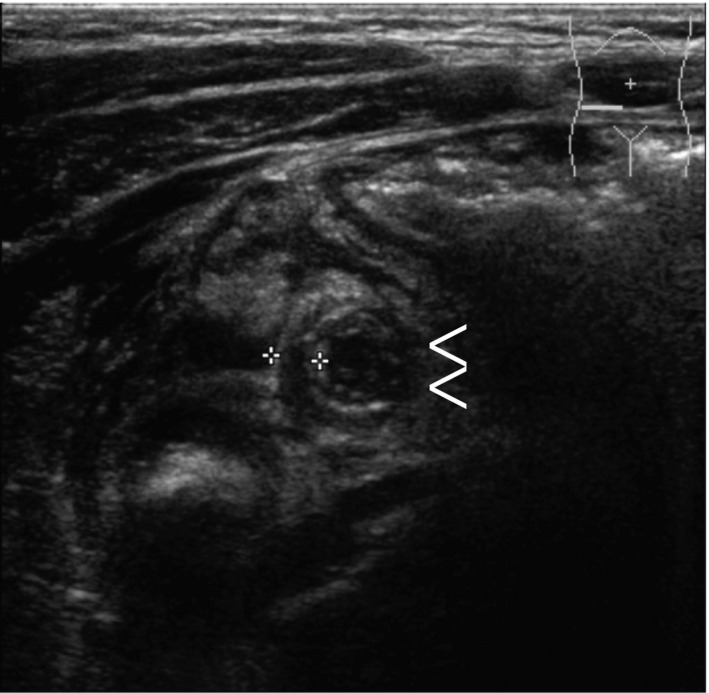
A transverse image of an inflamed appendix with the lateral wall of the appendix measured (between electronic calipers), while the medial wall is difficult to differentiate from the luminal contents and surrounding tissue (arrowheads).
Potential pitfalls in the sonographic diagnosis of appendicitis include an incomplete investigation of the appendix resulting in failure to identify segmental or tip appendicitis44 and overestimation of an increased appendiceal diameter leading to a false positive diagnosis.49 Anatomical variation can also complicate diagnosis. The appendix is most commonly retro‐ileal, but a retro‐caecal location has been reported in 5–28% of cases, making identification by ultrasound technically difficult due to artefact from overlying bowel gas/faeces (Fig. 5).12, 46, 51 The lack of a visible appendix makes determining diameter and other previously mentioned criteria impossible to assess, highlighting the potential diagnostic use of more readily visible secondary signs of appendicitis.
Figure 5.

The retro‐caecal appendix: an inflamed appendix (A) is seen posterior to the caecum (C).
Secondary sonographic signs
There are several secondary sonographic signs of appendicitis that can be useful diagnostic indicators, and potential positive or negative predictors in the absence of a visible appendix or an otherwise equivocal study. One such sign is echogenic mesenteric fat, which has been proven to have a PPV for appendicitis of 99% (Fig. 6).34 The mesentery can provide both a path for disease spread and barrier for infection as it potentially walls off inflamed areas such as an acute appendix. A useful method for determining if there is an increase in mesenteric echogenicity is to compare the contralateral side of the patient as a baseline.34 Free intra‐peritoneal fluid in the RLQ can also be an indication of appendicitis, as can the presence of enlarged intra‐peritoneal lymph nodes (Fig. 7). Mesenteric lymphadenitis is a common differential finding in the context of RLQ pain and can be identified with ultrasound. There is usually no echogenic mesenteric fat in this condition as unlike appendicitis, the inflammation is contained within the nodes.34, 52 In addition, potential secondary signs of a perforated appendix are thickening of adjacent bowel wall and echogenic sludge in the urinary bladder (Fig 8).35
Figure 6.
Echogenic mesentery (arrowheads) is seen surrounding an inflamed appendix in longitudinal (left) and transverse planes (right), note has also been made that this appendix was non‐compressible.
Figure 7.
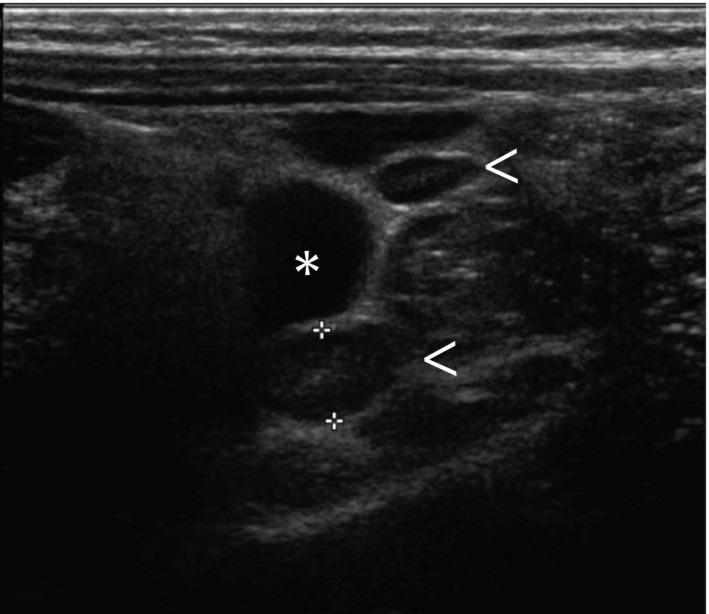
Peritoneal free fluid (asterisk) and lymph nodes (arrowheads) can be secondary signs of appendicitis.
Figure 8.
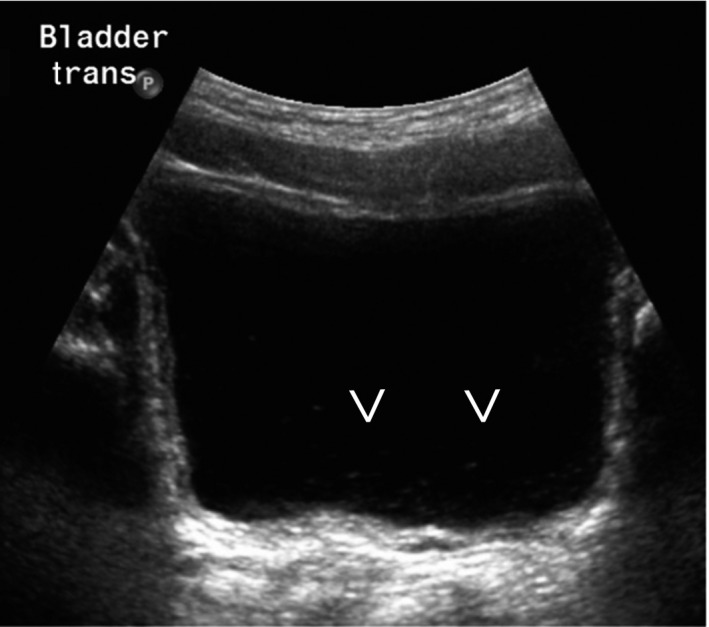
Echogenic debris can be seen in the urinary bladder (arrowheads) in this patient with a perforated appendix.
In a study of 146 children, Wiersma et al.46 reported that the presence of secondary signs may be affected by the location of the appendix so that a retro‐caecal appendix has a different sonographically visible mesenteric reaction in comparison to an inflamed retro‐ileal appendix. They also reported that the absence of secondary signs and non‐visualisation of the appendix had a high NPV, and conversely that the presence of secondary signs alone was a strong positive predictor of appendicitis. Reliance on secondary signs however has also been associated with a high number of false positives.4 Estey et al.53 and more recently Ross et al.54 confirmed the PPV of secondary signs, yet their absence did not permit reliable exclusion of appendicitis. These contradictory findings warrant further investigation to determine the diagnostic potential of individual or certain combinations of secondary signs to obtain the most comprehensive and meaningful sonographic conclusion.
Conclusion
Ultrasound diagnosis of appendicitis traditionally yielded one of the following conclusions: a positive finding where an inflamed appendix that meets the sonographic criteria described above, a normal appendix or an equivocal finding where the appendix is not seen at all. Some studies have included the presence or combination of secondary signs into their criteria to give a more accurate and meaningful diagnosis and creating four possible findings: unequivocally positive (appendix is seen and inflamed), probably positive (appendix was poorly seen or not visualised and secondary signs are present), probably negative (appendix was poorly seen or not seen and no secondary signs) and unequivocally negative (appendix seen and normal).3, 38, 39, 55 With recent studies demonstrating that up to 46% of ultrasound studies do not visualise the appendix, the value of sonographers recognising that secondary signs are reliable diagnostic corollaries could facilitate better clinical outcomes and decrease the need for potential harm in the form of radiation exposure from CT and or unnecessary surgical procedures from negative appendicectomies.47, 53, 56
Conflict of Interest
The authors declare that they have no conflicts of interest in relation to this article.
J Med Radiat Sci 63 (2016) 59–66
References
- 1. Australian Institute of Health and Welfare . Admitted Patient Care 2013–14: Australian Hospital Statistics. Health services series no. 60. Cat. no. HSE 156. AIHW, Canberra, Australia, 2015. [Google Scholar]
- 2. Sivit CJ, Applegate KE, Stallion A, et al. Imaging evaluation of suspected appendicitis in a pediatric population. Am J Roentgenol 2000; 175: 977–80. [DOI] [PubMed] [Google Scholar]
- 3. Wiersma F, Toorenvliet BRB, Bloem JJL, Allema JH, Holscher HC. US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol 2009; 19: 455–61. [DOI] [PubMed] [Google Scholar]
- 4. Gracey D, McClure MJ. The impact of ultrasound in suspected acute appendicitis. Clin Radiol 2007; 62: 573–8. [DOI] [PubMed] [Google Scholar]
- 5. Baldisserotto M, Marchiori E. Accuracy of noncompressive sonography of children with appendicitis according to the potential positions of the appendix. AJR Am J Roentgenol 2000; 175: 1387–92. [DOI] [PubMed] [Google Scholar]
- 6. Dilley A, Wesson D, Munden M, et al. The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3‐year analysis. J Pediatr Surg 2001; 36: 303–8. [DOI] [PubMed] [Google Scholar]
- 7. Limchareon S, Wongsuttilert A, Boonyarit A. Efficacy of ultrasonography in evaluation of suspected appendicitis in pediatric population. J Med Ultrasound 2014; 22: 213–7. [Google Scholar]
- 8. Mittal MK, Dayan PS, Macias CG, et al. Performance of ultrasound in the diagnosis of appendicitis in children in a multicenter cohort. Acad Emerg Med 2013; 20: 697–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology 1986; 158: 355–60. [DOI] [PubMed] [Google Scholar]
- 10. Puylaert JBCM. Ultrasonography for diagnosing appendicitis. BMJ 1988; 297: 740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reed MH. Imaging utilization commentary: a radiology perspective. Pediatr Radiol 2008; 38: 660–3. [DOI] [PubMed] [Google Scholar]
- 12. Lee JH. Sonography of acute appendicitis. Semin Ultrasound CT MRI 2003; 24: 83–90. [DOI] [PubMed] [Google Scholar]
- 13. Rice HE, Arbesman M, Martin DJ, et al. Does early ultrasonography affect management of pediatric appendicitis? A prospective analysis. J Pediatr Surg 1999;34:754–8; discussion 758–9. [DOI] [PubMed] [Google Scholar]
- 14. York D, Smith A, Phillips JD, von Allmen D. The influence of advanced radiographic imaging on the treatment of pediatric appendicitis. J Pediatr Surg 2005; 40: 1908–11. [DOI] [PubMed] [Google Scholar]
- 15. Pershad J, Waters TM, Langham MR, Li T, Huang EY. Cost‐effectiveness of diagnostic approaches to suspected appendicitis in children. J Am Coll Surg 2015; 220: 738–46. [DOI] [PubMed] [Google Scholar]
- 16. Garcia K, Hernanz‐Schulman M, Bennett DL, Morrow SE, Yu C, Kan JH. Suspected appendicitis in children: diagnostic importance of normal abdominopelvic CT findings with nonvisualized appendix. Radiology 2009; 250: 531–7. [DOI] [PubMed] [Google Scholar]
- 17. Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta‐analysis Radiology 2006; 241: 83–94. [DOI] [PubMed] [Google Scholar]
- 18. Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rosendahl K, Aukland SM, Fosse K. Imaging strategies in children with suspected appendicitis. Eur Radiol Suppl 2004; 14: L138–45. [DOI] [PubMed] [Google Scholar]
- 20. Thirumoorthi AS, Fefferman NR, Ginsburg HB, Kuenzler KA, Tomita SS. Managing radiation exposure in children – reexamining the role of ultrasound in the diagnosis of appendicitis. J Pediatr Surg 2012; 47: 2268–72. [DOI] [PubMed] [Google Scholar]
- 21. Krishnamoorthi R, Ramarajan N, Wang NE, et al. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA. Radiology 2011; 259: 231–9. [DOI] [PubMed] [Google Scholar]
- 22. Jacobs JE. CT and sonography for suspected acute appendicitis: a commentary. AJR Am J Roentgenol 2006; 186: 1094–6. [DOI] [PubMed] [Google Scholar]
- 23. Rice HE, Frush DP, Harker MJ, Farmer D, Waldhausen JH. Peer assessment of pediatric surgeons for potential risks of radiation exposure from computed tomography scans. J Pediatr Surg 2007; 42: 1157–64. [DOI] [PubMed] [Google Scholar]
- 24. Saito JM, Yan Y, Evashwick TW, Warner BW, Tarr PI. Use and accuracy of diagnostic imaging by hospital type in pediatric appendicitis. Pediatrics 2012; 131: e37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Michailidou M, Sacco Casamassima MG, Karim O, et al. Diagnostic imaging for acute appendicitis: interfacility differences in practice patterns. Pediatr Surg Int 2015; 31: 355–61. [DOI] [PubMed] [Google Scholar]
- 26. Herliczek TW, Swenson DW, Mayo‐Smith WW. Utility of MRI after inconclusive ultrasound in pediatric patients with suspected appendicitis: retrospective review of 60 consecutive patients. AJR Am J Roentgenol 2013; 200: 969–73. [DOI] [PubMed] [Google Scholar]
- 27. Orth RC, Guillerman RP, Zhang W, Masand P, Iii GSB. Prospective comparison of MR imaging and US for the diagnosis of pediatric appendicitis. Radiology 2014; 272: 233–40. [DOI] [PubMed] [Google Scholar]
- 28. Moore MM, Brian JM, Methratta ST, et al. MRI for clinically suspected pediatric appendicitis: case interpretation. Pediatr Radiol 2014; 44: 605–12. [DOI] [PubMed] [Google Scholar]
- 29. Kulaylat AN, Moore MM, Engbrecht BW, et al. An implemented MRI program to eliminate radiation from the evaluation of pediatric appendicitis. J Pediatr Surg 2015; 50: 1359–63. [DOI] [PubMed] [Google Scholar]
- 30. Johnson AK, Filippi CG, Andrews T, et al. Ultrafast 3‐T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis. Am J Roentgenol 2012; 198: 1424–30. [DOI] [PubMed] [Google Scholar]
- 31. Moore MM, Gustas CN, Choudhary AK, et al. MRI for clinically suspected pediatric appendicitis: an implemented program. Pediatr Radiol 2012; 42: 1056–63. [DOI] [PubMed] [Google Scholar]
- 32. Trout AT, Sanchez R, Ladino‐Torres MF, Pai DR, Strouse PJ. A critical evaluation of US for the diagnosis of pediatric acute appendicitis in a real‐life setting: how can we improve the diagnostic value of sonography? Pediatr Radiol 2012; 42: 813–23. [DOI] [PubMed] [Google Scholar]
- 33. Ramarajan N, Krishnamoorthi R, Gharahbaghian L, Pirrotta E, Barth RA, Wang NE. Clinical correlation needed: what do emergency physicians do after an equivocal ultrasound for pediatric acute appendicitis? J Clin Ultrasound 2014; 42: 385–94. [DOI] [PubMed] [Google Scholar]
- 34. Lee MW, Kim YJ, Jeon HJ, Park SW, Jung SI, Yi JG. Sonography of acute right lower quadrant pain: importance of increased intraabdominal fat echo. Am J Roentgenol 2009; 192: 174–9. [DOI] [PubMed] [Google Scholar]
- 35. Hahn HB, Hoepner FU, Kalle TV, et al. Sonography of acute appendicitis in children: 7 years experience. Pediatr Radiol 1998; 28: 147–51. [DOI] [PubMed] [Google Scholar]
- 36. Kessler N, Cyteval C, Gallix B, et al. appendicitis: evaluation of sensitivity, specificity, and predictive values of US, Doppler US, and laboratory findings. Radiology 2004; 230: 472–8. [DOI] [PubMed] [Google Scholar]
- 37. Rodriguez DP, Vargas S, Callahan MJ, Zurakowski D, Taylor GA. Appendicitis in young children: imaging experience and clinical outcomes. AJR Am J Roentgenol 2006; 186: 1158–64. [DOI] [PubMed] [Google Scholar]
- 38. Jaremko JL, Crockett A, Rucker D, et al. Incidence and significance of inconclusive results in ultrasound for appendicitis in children and teenagers. Can Assoc Radiol J 2011; 62: 197–202. [DOI] [PubMed] [Google Scholar]
- 39. van Atta AJ, Baskin HJ, Maves CK, et al. Implementing an ultrasound‐based protocol for diagnosing appendicitis while maintaining diagnostic accuracy. Pediatr Radiol 2015; 45: 678–85. [DOI] [PubMed] [Google Scholar]
- 40. Ryan C. Sonographic evaluation of acute appendicitis. J Diagnostic Med Sonogr 2012; 28: 320–3. [Google Scholar]
- 41. Holmes JA, Delaney M. Pediatric appendicitis. Pediatr Emerg Med Reports PEMR 2011; 11. [Google Scholar]
- 42. Halm BM, Eakin PJ, Franke AA. Diagnosis of appendicitis by a pediatric emergency medicine attending using point‐of‐care ultrasound: a case report. Hawaii Med J 2010; 69: 208–11. [PMC free article] [PubMed] [Google Scholar]
- 43. Koepsell T, Flum DR. The clinical and economic correlates of misdiagnosed appendicitis. Arch Surg 2002; 137: 799–804. [DOI] [PubMed] [Google Scholar]
- 44. Sonanvane S, Siegel MJ. Sonography of the surgical abdomen in children. Ultrasound Clin 2008; 3: 67–82. [Google Scholar]
- 45. Strouse PJ. Pediatric appendicitis: an argument for US. Radiology 2010; 255: 8–13. [DOI] [PubMed] [Google Scholar]
- 46. Wiersma F, Šrámek A, Holscher HC. US features of the normal appendix and surrounding area in children. Radiology 2005; 235: 1018–22. [DOI] [PubMed] [Google Scholar]
- 47. Schuh S, Man C, Cheng A, et al. Predictors of non‐diagnostic ultrasound scanning in children with suspected appendicitis. J Pediatr 2011; 158: 112–8. [DOI] [PubMed] [Google Scholar]
- 48. Rettenbacher T, Hollerweger A, Macheiner P, et al. Outer diameter of the vermiform appendix as a sign of acute appendicitis: evaluation at US. Radiology 2001; 218: 757–62. [DOI] [PubMed] [Google Scholar]
- 49. Lardenoye SW, Puylaert JB, Smit MJ, Holscher HC. Appendix in children with cystic fibrosis: US features. Radiology 2004; 232: 187–9. [DOI] [PubMed] [Google Scholar]
- 50. Chaudry G, Navarro OM, Levine DS, Oudjhane K. Abdominal manifestations of cystic fibrosis in children. Pediatr Radiol 2006; 36: 233–40. [DOI] [PubMed] [Google Scholar]
- 51. Peletti AB, Baldisserotto M. Optimizing US examination to detect the normal and abnormal appendix in children. Pediatr Radiol 2006; 36: 1171–6. [DOI] [PubMed] [Google Scholar]
- 52. Van Breda Vriesman AC, Puylaert JBCM. Mimics of appendicitis: alternative nonsurgical diagnoses with sonography and CT. AJR Am J Roentgenol 2006; 186: 1103–12. [DOI] [PubMed] [Google Scholar]
- 53. Estey A, Poonai N, Lim R. Appendix not seen: the predictive value of secondary inflammatory sonographic signs. Pediatr Emerg Care 2013; 29: 435–9. [DOI] [PubMed] [Google Scholar]
- 54. Ross MJ, Liu H, Netherton SJ, et al. Outcomes of children with suspected appendicitis and incompletely visualized appendix on ultrasound. Acad Emerg Med 2014; 21: 538–42. [DOI] [PubMed] [Google Scholar]
- 55. Zakaria O, Sultan TA, Khalil TH, Wahba T. Role of clinical judgment and tissue harmonic imaging ultrasonography in diagnosis of paediatric acute appendicitis. World J Emerg Surg 2011; 6: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Aspelund G, Fingeret A, Gross E, et al. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics 2014; 133: 586–93. [DOI] [PubMed] [Google Scholar]


