Abstract
Introduction
Time‐consuming manual methods have been required to register cone‐beam computed tomography (CBCT) images with plans in the Pinnacle3 treatment planning system in order to replicate delivered treatments for adaptive radiotherapy. These methods rely on fiducial marker (FM) placement during CBCT acquisition or the image mid‐point to localise the image isocentre. A quality assurance study was conducted to validate an automated CBCT‐plan registration method utilising the Digital Imaging and Communications in Medicine (DICOM) Structure Set (RS) and Spatial Registration (RE) files created during online image‐guided radiotherapy (IGRT).
Methods
CBCTs of a phantom were acquired with FMs and predetermined setup errors using various online IGRT workflows. The CBCTs, DICOM RS and RE files were imported into Pinnacle3 plans of the phantom and the resulting automated CBCT‐plan registrations were compared to existing manual methods. A clinical protocol for the automated method was subsequently developed and tested retrospectively using CBCTs and plans for six bladder patients.
Results
The automated CBCT‐plan registration method was successfully applied to thirty‐four phantom CBCT images acquired with an online 0 mm action level workflow. Ten CBCTs acquired with other IGRT workflows required manual workarounds. This was addressed during the development and testing of the clinical protocol using twenty‐eight patient CBCTs. The automated CBCT‐plan registrations were instantaneous, replicating delivered treatments in Pinnacle3 with errors of ±0.5 mm. These errors were comparable to mid‐point‐dependant manual registrations but superior to FM‐dependant manual registrations.
Conclusion
The automated CBCT‐plan registration method quickly and reliably replicates delivered treatments in Pinnacle3 for adaptive radiotherapy.
Keywords: Adaptive radiotherapy, automated registration, cone‐beam computed tomography, treatment planning system
Introduction
Online‐adaptive radiotherapy protocols routinely require cone‐beam computed tomography (CBCT) scans acquired for image‐guided radiotherapy (IGRT) to be registered with the patient's treatment plan in the treatment planning system (TPS).1, 2 Developing ‘plan of the day’ treatments based on the first week of delivered treatments requires the CBCTs to be aligned with the plan's treatment fields in order to replicate treatment field positioning in the patient after online IGRT. Pham et al.3 describes the different CBCT‐plan registration methods required for seven combinations of multi‐vendor systems in a multi‐centred adaptive radiotherapy bladder cancer trial. The drawback of multi‐vendor radiotherapy systems when attempting to replicate delivered treatments in a TPS is that time‐consuming, manual methods are often required.
The radiotherapy systems in use at the Radiation Oncology Mater Centre (ROMC) include the Pinnacle3 TPS (Philips Healthcare, Fitchburg, WI), ClinaciX linear accelerators (Varian Medical Systems, Palo Alto, CA) with the On Board Imager (OBI) kilovoltage (kV) imaging system and the MOSAIQ Oncology Information Management System (Elekta, Stockholm, Sweden). During online IGRT, the OBI software creates a folder with Digital Imaging and Communications in Medicine (DICOM) image files, and DICOM‐Radiotherapy (DICOM‐RT) Structure Set (RS) and Registration (RE) files.4 RS files define areas of significance associated with an image, and contain geometrical and display parameters and generation technique information.5 RE files (also termed Spatial Registration Objects) contain the transformation information of an image's reference coordinate system to those of an image with which it has been registered.5 Currently, importing CBCTs to Pinnacle3 is supported via DICOM‐RT file export from the Varian OBI computer to MOSAIQ. Only the CBCT images and RS files are then able to be exported to the Pinnacle3 DICOM server via MOSAIQ's DICOM image export option. MOSAIQ does not currently support RE file export.6
Replicating delivered treatments in Pinnacle3 with this combination of radiotherapy systems has relied on placement of three fiducial markers (FMs) on the skin at the anterior and lateral setup points prior to CBCT acquisition on the linear accelerator (Linac).3 The FMs are used to localise the CBCT acquisition isocentre (CBCTacqiso) in Pinnacle3 and then manual translations are applied to register the CBCTacqiso with the treatment plan isocentre (Planiso). If couch shifts were applied during online IGRT, this initial registration has to be offset using data extracted from the patient's MOSAIQ record. Alternatively the CBCT image mid‐point (CBCTmidpt) has been used for localising the CBCTacqiso. 7 This method assumes that a CBCT image is always acquired symmetrically in all planes around the Linac's isocentre. This does not occur in cases where the kV source and the detector have been offset in the patient's superior‐inferior (SI) direction.
A potential automated solution for replicating delivered treatments was identified while conducting another study.8 Importing the OBI‐generated DICOM‐RT RS and RE files into Pinnacle3 automatically creates and associates points of interest (POIs) with the CBCT (labelled AcqIsocentre, InitLaserIso and InitMatchIso) and registers the CBCT with the plan. This paper describes a quality assurance (QA) study using phantom and retrospective patient data to verify (1) the relationship between the CBCT image acquisition isocentre and the three CBCT POIs created when the DICOM‐RT RS file is imported into Pinnacle3, (2) that importing the DICOM‐RT RE file correctly registers the CBCT with the Pinnacle3 plan so treatment field positioning after online IGRT is replicated and (3) the automated CBCT‐plan registration method is reliable and more effective than the time‐consuming FM‐dependant or CBCTmidpt manual methods, enabling its implementation with clinical adaptive radiotherapy protocols.
Method
Phantom QA study
A phantom QA study was designed to replicate the transfer of data between the Pinnacle3, MOSAIQ and Varian systems used for CBCT‐guided IGRT. Clinical scanning protocols for the pelvic and head and neck (HN) regions were used as CBCTs are most frequently acquired for these sites. An overview of the phantom QA study workflow is provided in Figure 1.
Figure 1.
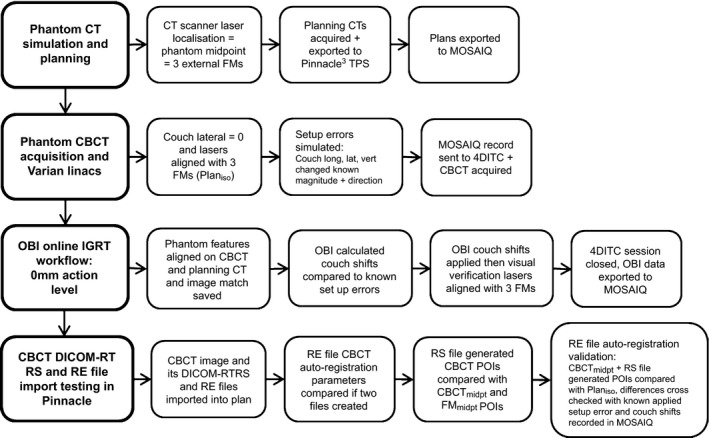
Workflow for the phantom QA study.
CT simulation and treatment plan setup
Two planning computed tomography (CT) scans were acquired of the Computerised Imaging Reference Systems (CIRS) Electron Density (ED) phantom (Norfolk, VA) on a Somatom Sensation Open 20‐slice scanner (Siemens Medical Solutions, Forchheim, Germany) using clinical scanning protocols (see Table 1). The phantom was configured to represent pelvic patient dimensions for the first scan and then HN patient dimensions for the second, with customised tissue equivalent wax blocks added to simulate typical treatment cranio‐caudal dimensions. For both scans, three FMs were placed on the phantom in anterior and lateral positions coinciding with the mid‐point of the central insert. The two planning CT scans were imported into Pinnacle3 v9.4 and a 4‐field pelvis and a 2‐field HN plan created. The isocentre of each treatment plan (Planiso) was selected to coincide with the three FM positions. Each plan was exported to MOSAIQ and CBCT imaging fields added for each site.
Table 1.
Departmental planning CT and CBCT scan acquisition protocols
| Planning CT scan acquisition protocols | |
| Pelvis | 120 kVp, 35 mAs, 650 mm FOV, pitch = 0.75, 2 mm slice width |
| Head and neck | 120 kVp, 35 mAs, 650 mm FOV, pitch = 1.2, 3 mm slice width |
| CBCT scan acquisition protocols | |
| Pelvis | 125 kVp, 80 mA, scan mode: half‐fan, image matrix: 512 × 512, filter: sharp, slice thickness: 2 mm |
| Head and neck | 100 kVp, 20 mA, scan mode: Full‐fan, image matrix: 512 × 512, filter: sharp, slice thickness: 2 mm |
CBCT acquisition
Multiple series of CBCT images of the phantom were acquired on the four departmental ClinaciX Linacs (1, 2, 3 and 4) with two investigators present to cross‐check the phantom setup and the online IGRT process. For each scan, the phantom was positioned on the treatment couch with the couch lateral set to 0 cm and the lasers coincident with the three FM markers placed on the phantom during CT simulation (i.e. the Planiso). Predetermined couch offsets from the Planiso, varying in magnitude (0, 0.5, 1.0 or 2.0 cm) and direction (anterior or posterior, left or right, and superior or inferior) were then applied to simulate setup errors. The treatment and imaging fields for either the pelvis or HN treatment site were sent from MOSAIQ to the 4D Integrated Treatment Console (4DITC) and a CBCT acquired using the relevant clinical scanning protocol (see Table 1). The typical clinical OBI console workflow for online IGRT with a 0 mm action level was followed after CBCT reconstruction. Once online image matching was performed, the magnitude and direction of the software‐determined couch shifts necessary to realign the phantom to the Planiso were cross‐checked against the applied setup error. The laser alignment with the FMs on the phantom was visually verified after automated couch shifts had been applied. The treatment session was then closed in the 4DITC and the OBI DICOM files exported to MOSAIQ.
A second series of CBCT images was acquired on Linac 1 with the phantom in the pelvic configuration, using the pelvis scanning protocol. Table 2 outlines the applied setup conditions and online IGRT processes for this series, aimed at examining the effects on the DICOM‐RT RS and RE file information when (1) the OBI console and 4DITC workflows are varied from those used for online IGRT with a 0 mm action level and (2) automatic re‐centring of the couch lateral position to 0 cm occurs prior to CBCT acquisition when the initial couch lateral setup position is >5 cm.4
Table 2.
The different setup conditions used to acquire the images for the second series of CBCTs acquired on Linac 1
| Couch lateral position (Planiso = linac isocentre) | Setup error applied after Planiso setup | Image match saved | Couch shifts applied | DICOM‐RT RS file created | DICOM‐RT RE files created |
|---|---|---|---|---|---|
| 0 cm | No | No | No | Yes | 0 |
| Yes | No | Yes | 1 | ||
| No | Yes | Yes | 1 | ||
| Yes | Yes | Yes | 2 | ||
| 0 cm | Yes | No | No | Yes | 0 |
| Yes | No | Yes | 1 | ||
| No | Yes | Yes | 1 | ||
| Yes | Yes | Yes | 2 | ||
| 8 cm | Yes | No | No | Yes | 0 |
| Yes | No | Yes | 1 | ||
| No | Yes | Yes | 1 | ||
| Yes | Yes | Yes | 2 |
The rows in bold equate to the OBI workflow for online IGRT with a 0 mm action level.
Importation of the DICOM RS and RE files into Pinnacle3
The DICOM image, RS and RE files for each CBCT of the phantom were transferred from each Linac OBI computer to the Pinnacle3 DICOM server. Each CBCT image was imported and associated as a secondary image on a copy of either the original pelvis or HN treatment plan. The RS file was imported via the DICOM Import window selecting the CBCT's corresponding Structure Set DICOM‐RT message. The resulting names and coordinates of the POIs automatically created and associated with the CBCT were recorded. The RE file was then imported by selecting the CBCT's corresponding Spatial Registration DICOM‐RT message. The resulting automated CBCT‐plan registration was visually inspected to verify correct alignment of CBCT with the planning CT thus replicating the online image match. The Registration Parameters window (available in Pinnacle's Syntegra platform) was inspected to determine the registration parameters applied to the CBCT. If more than one RE file had been created by the OBI software, the file with the earliest time creation was initially imported, the CBCT then reset to its initial unregistered position and the process repeated for the remaining RE files in order of their creation time.
Comparison of CBCT isocentre localisation and registration
Post‐automated registration, a new POI was associated with each CBCT and manually placed at the CBCTmidpt. POIs were also automatically placed at the mid‐point of contours of the anterior and two lateral FMs visible on each CBCT image. The contours were created by applying thresholds with lower and upper CBCT image thresholds of 1100 and the maximum image value respectively (see Fig. 2). The coordinates of the CBCTmidpt, each FM mid‐point (FMmidpt) and the RS file‐generated POIs on the CBCT image were then compared. Table 3 provides a summary of the naming convention and method of creation for the different CBCT POIs. The RS file‐generated CBCT POIs were then copied and associated with the planning CT to facilitate coordinate comparison with the Planiso. The differences between the Planiso and the RS file‐generated POIs were compared to the known magnitude and direction of the setup errors applied prior to the acquisition of each CBCT image and the couch shifts recorded in MOSAIQ.
Figure 2.
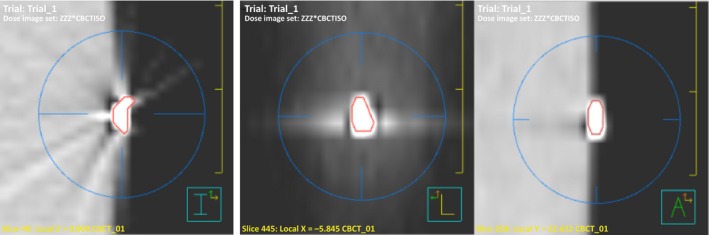
Example of the contour based FM mid‐point localisation, showing from left to right, the mid‐point position of the left FM in the transverse, sagittal and coronal planes.
Table 3.
Point of interest (POI) naming conventions and method of creation
| POI name | Definition | Method of creation |
|---|---|---|
| Plan iso | Treatment plan isocentre = localisation of isocentre on linac prior to online IGRT | The treatment plan isocentre. POI attached to planning CT scan during plan generation |
| CBCTmidpt | Half‐way between coordinates of first and last slice in x, y and z dimensions of the CBCT image | POI manually added to the CBCT image once imported to Pinnacle3 that equates to the mid‐point of the image |
| FMmidpt | The mid‐point of the imaged position of the anterior and right and left lateral fiducial markers on the CBCT image | POIs automatically placed in the middle of threshold‐based contours the FMs |
| AcqIsocenter | The linac isocentre during CBCT acquisition | POI automatically created and associated with the CBCT image when DICOM‐RT RS file imported |
| InitLaserIso | The position of the linac isocentre prior to CBCT scan initialisation | POI automatically created and associated with the CBCT image when DICOM‐RT RS file imported |
| InitMatchIso | The position of linac isocentre after CBCT acquisition, just prior to online image matching | POI automatically created and associated with the CBCT image when DICOM‐RT RS file imported |
Clinical protocol development and validation
The results of the phantom study were used to develop a clinical protocol for the automated method. A QA procedure for verifying correct CBCT‐plan registration was also developed. It incorporates both a mathematical and visual rule‐based system that correlates the ClinaciX and Pinnacle3 coordinate systems and cross‐checks recorded MOSAIQ data. Institutional ethics approval was granted for validating the protocol via a retrospective study using plans and CBCTs acquired during Week 1 of treatment for six consecutive bladder cancer patients. Three patients were treated using an online image‐guided adaptive radiotherapy protocol2 with a 0 mm action level and where FM‐dependant manual CBCT‐plan registration had been performed. The remaining three patients were treated using palliative IGRT protocols. Once automated CBCT‐plan registration was achieved for the Week 1 CBCTs for each patient using the developed protocol, a CBCTmidpt POI was manually added to each CBCT and compared to the RS file‐generated POIs. FMmidpt POIs were added to the CBCTs where all three FMs placed on the skin were visible and their coordinates also compared to the RS file‐generated POIs. The protocol's QA procedure was used to verify the post‐registration CBCTacqiso position relative to the Planiso.
Results
Phantom QA study
A total of forty‐four CBCT scans were acquired of the phantom across four ClinaciX Linacs. Fourteen CBCTs were acquired using the HN protocol and thirty with the pelvis protocol, of which ten were acquired using different workflows other than those used for online IGRT with a 0 mm action level. A DICOM‐RT RS file was always created by the OBI software independent of workflow. In each instance when a DICOM‐RT RS file was imported into a Pinnacle3 plan, three POIs labelled AcqIsocenter, InitLaserIso and InitMatchIso were automatically created on its associated CBCT. The coordinates of these POIs were identical except when automatic anti‐collision couch re‐centring occurred prior to CBCT acquisition (see Fig. 3). When this occurred the AcqIsocenter POI coordinates corresponded to the CBCTacqiso (i.e. after re‐centring to couch lateral = 0 cm). However, the InitLaserIso and InitMatchIso POI coordinates were always identical as they corresponded to the same isocentre position in the phantom; the isocentre position before couch re‐centring (InitLaserIso) and after couch repositioning to the pre‐scanning isocentre position (InitMatchIso).
Figure 3.
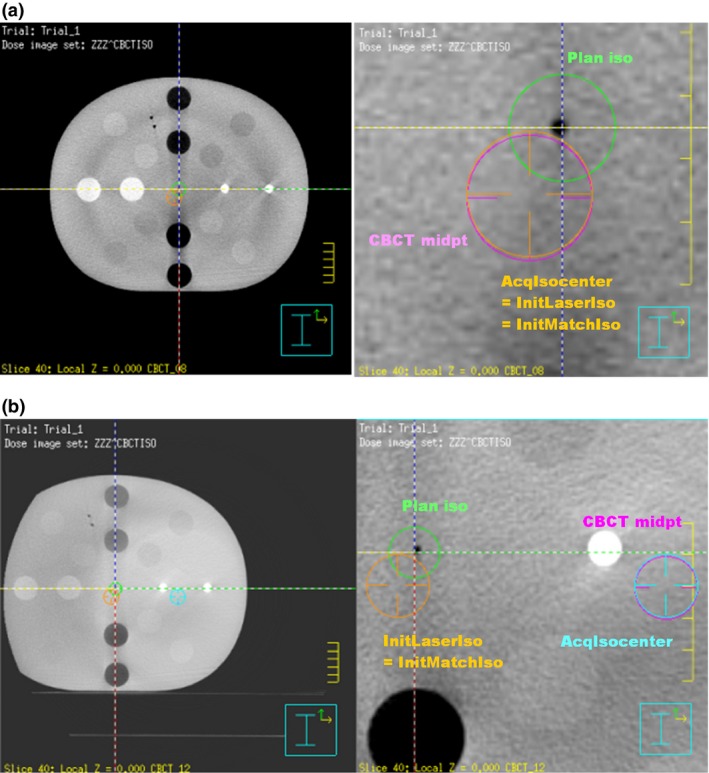
The difference in the RS file created CBCT points when anti‐collision couch re‐positioning has occurred during CBCT acquisition. On each image above the Planiso = the green POI and the CBCT midpt = the purple POI. (a) When no anti‐collision couch repositioning is applied, the DICOM‐RT RS generated POIs have the same coordinates (the orange POI). (b) When anti‐collision couch repositioning occurs, the AcqIsocentre (the light blue POI) = the isocentre during scanning and the InitLaserIso and InitMatchIso POIs = the isocentre position before and after couch repositioning and will have the same coordinates (the orange POI).
Localisation of the CBCTmidpt POI in Pinnacle3 was based on image matrix sizes of 45 × 45 × 16 cm and 25 × 25 × 16 cm resulting from the pelvis and HN imaging protocols respectively. Across the Linacs, the CBCTmidpt coordinates were consistently the same in the x (left‐right, LR) and y (anterior‐posterior, AP) axes, however differences of up 0.14 cm were observed in the z (SI) axis. Differences between the CBCTmidpt and the AcqIsocentre POI coordinates varied but did not exceed 0.5 mm. Their magnitude was the same for CBCT images acquired consecutively in one session on the same Linac but varied between Linacs (see Table 4). All three FMs on the CBCT images were only visible when the phantom was centred on the couch and imaged using the pelvis protocol. When all three FMs were visible, mean differences of 0.9 ± 0.7 mm AP and 0.6 ± 0.5 mm SI were observed between each corresponding FMmidpt on the phantom CBCT images. Left‐right variations could not be compared as only one anterior FM was used. In the instances where no couch offsets from the Planiso were applied prior to CBCT acquisition, the mean differences between the AcqIsocentre and the FMmidpt POIs were 0.5 ± 0.4 mm (LR), 0.7 ± 0.7 mm (AP) and 0.6 ± 0.4 mm (SI).
Table 4.
The difference between the Pinnacle3 coordinates of the image mid‐point POI and the AcqusitionIso POI for the CBCT images of the phantom
| CBCTmidpt POI – AcqIso POI coordinates (cm): pelvis scanning protocol | CBCTmidpt POI – AcqIso POI coordinates (cm): head and neck CBCT image mid‐point | |||||
|---|---|---|---|---|---|---|
| Linear accelerator | L/R (x‐axis) | A/P (y‐axis) | S/I (z‐axis) | L/R (x‐axis) | A/P (y‐axis) | S/I (z‐axis) |
| Linac 1: series 1 | 0.00 | 0.05 | −0.04 | 0.00 | 0.05 | −0.04 |
| Linac 1: series 2 | 0.00 | 0.05 | −0.04 | |||
| Linac 2 | −0.01 | 0.05 | −0.02 | −0.01 | 0.05 | −0.02 |
| Linac 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Linac 4 | 0.00 | 0.00 | −0.04 | 0.00 | 0.00 | −0.02 |
CBCTmidpt POI, CBCT mid‐point point of interest; AcqIso POI, AcquisitionIso point of interest; L/R, left/right; A/P, anterior/posterior; S/I, superior/inferior.
When the OBI console and 4DITC workflows used for performing online IGRT with a 0 mm action level were followed, two DICOM‐RT RE files with different time stamps were created. The file with the earliest time stamp corresponded to saving an online image match while the latest time stamped file corresponded to application of a couch shift. Importing either one of these files into Pinnacle3 resulted in identical CBCT‐planning CT registrations. Differences between the AcqIsocenter, InitLaserIso and InitMatchIso POIs and the Planiso POI post‐registration corresponded to the known magnitude and direction of the couch offsets applied prior to CBCT acquisition (within 0.5 mm). Table 2 outlines how the creation of the DICOM‐RT RE files are affected by not saving an image match and/or applying a couch shift.
Clinical protocol development and validation
Flow charts in Figure 4 outline the steps in the clinical protocol for performing automated CBCT‐plan registration in Pinnacle3 when CBCTs have been acquired using an online IGRT with a 0 mm action level. Table 5 provides a summary of the protocol's QA procedure rules for mathematically and visually verifying the post‐registration InitMatchIso POI position relative to the Planiso in Pinnacle3 against the couch shifts recorded in the MOSAIQ Localisation Trend Review. Figure 5 demonstrates an example of the visual cross‐checking required between MOSAIQ and Pinnacle3.
Figure 4.
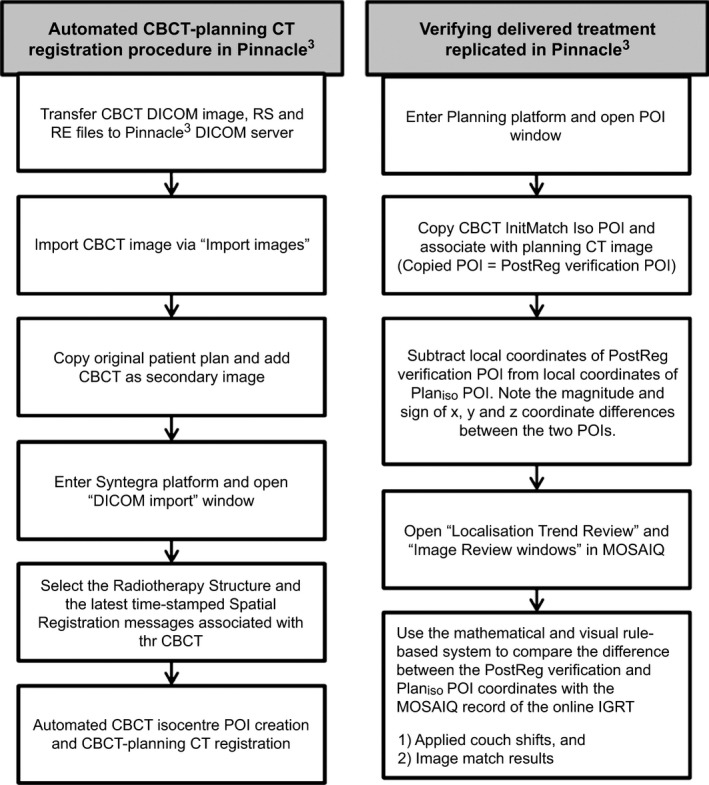
The procedure for automated CBCT‐planning CT registration in Pinnacle3 for replicating delivered treatments after online IGRT with a 0 mm action level.
Table 5.
The mathematical and visual rule‐based system developed for verifying the CBCT isocentre alignment with the treatment plan isocentre
| If the recorded MOSAIQ shifts are | The sign of the value after performing: Coordinatestreatment plan isocentre − CoordinatesInitMatchIso should be: | The InitMatchIso POI should be visually on the transverse, coronal and sagittal 2D views in Pinnacle3 |
|---|---|---|
| Left | +ve (positive) | To the right of the treatment plan isocentre POI |
| Right | −ve (negative) | To the left of the treatment plan isocentre POI |
| Ant | +ve (positive) | To the post of the treatment plan isocentre POI |
| Post | −ve (negative) | To the ant of the treatment plan isocentre POI |
| Sup | −ve (negative) | To the inf of the treatment plan isocentre POI |
| Inf | +ve (positive) | To the sup of the treatment plan isocentre POI |
Figure 5.
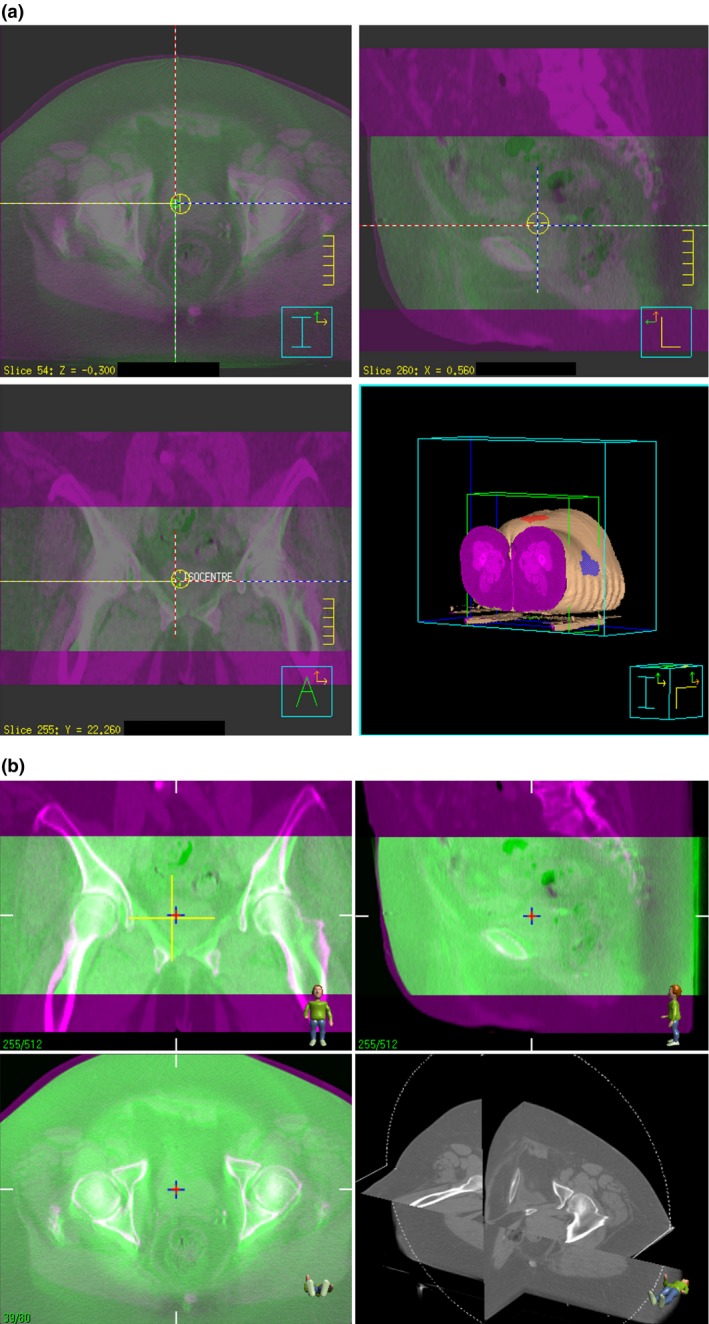
Visual check of CBCT‐plan registration in Pinnacle3 against the MOSAIQ record of the online image match. (a) CBCT‐plan registration in Pinnacle3 produced by the automated method, (b) Recorded online soft‐tissue matching of the bladder in MOSAIQ corresponding to the CBCT registered in Pinnacle3.
The protocol included manual workarounds required when CBCTs are not acquired with an online 0 mm action level. For an online IGRT protocol with a non‐zero action level, only one RE file is created when the image match is saved and couch shifts are not applied if they are less than the action level. Manual adjustment of the RE file‐generated CBCT translations in Syntegra are required to re‐align the InitMatchIso POI with the Planiso reflecting that no setup corrections were applied. If CBCTs are acquired for offline review only, as no online image matching is performed, no RE files are created. In these circumstances only manual CBCT‐plan registration is possible to align the InitMatchIso and Planiso POIs.
The clinical protocol was validated by automatically registering a total of twenty‐eight CBCTs with Pinnacle3 plans for six bladder patients. Two CBCTs were not included due to missing data resulting from export failures from the OBI system to MOSAIQ. As with the phantom CBCTs, RS file‐generated POIs on the patient CBCTs were labelled AcqIsocenter, InitLaserIso and InitMatchIso, however their coordinates were always identical, indicating no anti‐collision couch re‐centring had been required. The observed differences between the CBCTmidpt and the AcqIsocentre POI coordinates did not exceed 0.5 mm in any direction, agreeing with the observations from the phantom QA study. All three FMs were visible on only eight of the fifteen patient CBCTs in which they had been applied. Intra‐fraction variations between the FMmidpt coordinates on these images were routinely observed, the largest being 8.3 mm, with mean differences of 2.9 ± 3.4 mm (AP) and 3.1 ± 2.5 mm (SI). Intra‐fraction mean differences between the FMmidpt and the AcqIsocenter POIs were 2.7 ± 2.4 mm (LR), 3.8 ± 2.9 mm (AP) and 2.1 ± 2.2 mm (SI). The protocol's QA procedure confirmed correct directional offset of the InitMatchIso and the Planiso POIs for each of the RE‐file generated automated CBCT‐plan registrations. The QA procedure identified post‐registration variations up to 0.5 mm between the relative position of the InitMatchIso and the Planiso POIs when compared to the couch shifts recorded in MOSAIQ.
Discussion
This study validated an automated CBCT‐plan registration method that directly uses the information in the CBCT DICOM files generated on the ClinaciX Linacs to replicate delivered treatments in the Pinnacle3 TPS. The phantom QA study demonstrated the reliability of the data in the OBI DICOM RS and RE files when they are imported into a plan. The POIs created on the CBCT when the RS file is imported effectively localise the CBCTacqiso as they correspond to those associated with CBCT by the OBI software during acquisition (as per the manufacturer's reference guide).4 Importing the RE files automatically reproduces treatment field positioning relative to the CBCT after couch shifts have been applied during online IGRT. The developed protocol for the automated method has been approved for implementation following successful testing via the retrospective bladder patient study. It should be noted that this study tested the automated method for patients in the head‐first‐supine orientation only. When the study was conducted all patients requiring daily CBCT‐guided IGRT were treated in this position. Having established the reliability of the method, additional phantom CBCTs to test other orientations can be acquired as required.
While automated replication of delivered treatments in Pinnacle3 is now possible, the multi‐vendor radiotherapy systems in our department still impose some workflow limitations. Currently the CBCT DICOM files are copied to CD and then transferred to the Pinnacle3 DICOM server via file transfer protocol software due to export restrictions on the ClinaciX Linacs. Manual registration steps, only taking a few minutes, are still required to replicate treatment delivery when CBCTs haven't been acquired using online IGRT protocols with a 0 mm action level. However these workarounds have negligible impact on the efficiency gains achieved by implementing the automated method when compared to the time‐consuming FM‐based manual registration method previously relied on. FM‐dependant localisation of the CBCTacqiso relies on accurate marker placement on the patient's skin, the FMs being within the CBCT field of view and patient stability. Out of interest, one of the patient CBCT images was registered with their Pinnacle3 plan using the FM‐based manual registration method and the process timed. It took more than 20 mins to perform compared to instantaneous registration for the automated method, due to efforts to compensate for the difference in the FM mid‐points.
CBCT isocentre localisation discrepancies caused by inaccurate gantry rotation or kV source and detector movements,9, 10, 11 will affect the accuracy of the AcqIsocentre POI relative to the true Linac isocentre position. While identical CBCTmidpt and the AcqIsocenter POI coordinates were observed on Linac 3 after installation of new OBI hardware, observed variations of ±0.5 mm between these two POIs on the other Linacs indicate either could be used to localise the CBCTacqiso in Pinnacle3. However, the AcqIsocenter POI is preferable as it corresponds to the point that the OBI software uses to calculate and apply couch shifts during online IGRT.4 Importing the RE files into the Pinnacle3 plan resulted in observed variations of ±0.5 mm between the post‐registration InitMatchIso POI position relative to the Planiso and the couch shifts recorded in MOSAIQ. This is due to the RE file saving the online CBCT‐planning CT registration parameters to two decimal places, while the displayed offsets on the OBI console and the applied couch shifts recorded in the MOSAIQ are only to one decimal place.
The clinical protocol developed as a result of this study will be primarily implemented for plan‐of‐the‐day image‐guided adaptive radiotherapy protocols. However, since its implementation, it has also been used for retrospective CBCT‐based planning tumour volume margin evaluations as well as tumour and organ at risk inter‐fraction motion and deformation studies. In the future this method can also be applied to dose accumulation studies, though current CBCT Hounsfield unit‐ED modelling issues need to be resolved.12 Preliminary investigations were conducted to assess the method's applicability when importing CBCTs acquired on the Elekta XVI on‐board imaging system into Pinnacle3. For automated CBCT‐plan registration in Pinnacle3, the CBCT must be reconstructed in the reference image coordinates with corrections applied, then exported directly from the Linac to Pinnacle3. DICOM‐RT RS and RE files are not created during this process; however, these are not required to replicate CBCT‐IGRT in Pinnacle3 if the CBCT has been appropriately reconstructed prior to export.
Conclusion
When DICOM‐RT RS and RE files created by the Varian OBI software are imported into Pinnacle3 plans, automated CBCT isocentre localisation and CBCT‐plan registration instantaneously occurs. This automated method reliably replicates delivered treatments for adaptive radiotherapy, replacing the time‐consuming FM‐dependant manual method previously necessary with multi‐vendor radiotherapy systems and the Pinnacle3 TPS.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
This project was funded in part by the Princess Alexandra Hospital (PAH) Private Practice Trust Fund. Hargrave's research was funded by the Australian Federal Government via an Australian Post‐graduate Award and a Queensland University of Technology Deputy‐Vice Chancellor Scholarship. The authors thank Elizabeth Brown from Radiation Oncology, PAH for her valuable assistance with the Elekta XVI system.
J Med Radiat Sci 63 (2016) 48–58
References
- 1. Gill S, Pham D, Dang K, et al. Plan of the day selection for online image‐guided adaptive post‐prostatectomy radiotherapy. Radiother Oncol 2013; 107: 165–70. [DOI] [PubMed] [Google Scholar]
- 2. Foroudi F, Wong J, Kron T, et al. Online adaptive radiotherapy for muscle‐invasive bladder cancer: Results of a pilot study. Int J Radiat Oncol Biol Phys 2011; 81: 765–71. [DOI] [PubMed] [Google Scholar]
- 3. Pham D, Roxby P, Kron T, Rolfo A, Foroudi F. Introduction of online adaptive radiotherapy for bladder cancer through a multicentre clinical trial (trans‐tasman radiation oncology group 10.01): Lessons learned. J Med Phys 2013; 38: 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Varian Medical Systems . On‐Board Imager (OBI) Advanced Imaging Reference Guide [Instruction manual, version 1.6 software]. Document ID: B505009R01, Revision A. Palo Alto, CA, USA; June 2013.
- 5. National Electrical Manufacturers Association . NEMA PS3/ISO 12052 Digital Imaging and Communications in Medicine (DICOM). Standard Rosslyn, VA, USA.
- 6. IMPAC Medical Systems . MOSAIQ 2.50 DICOM Conformance Statement LEDDCM0042 (2.0).
- 7. Falco MD, Fontanarosa D, Miceli R, Carosi A, Santoni R, D'Andrea M. Preliminary studies for a CBCT imaging protocol for offline organ motion analysis: Registration software validation and CTDI measurements. Med Dosim 2011; 36: 91–101. [DOI] [PubMed] [Google Scholar]
- 8. Moores M, Hargrave C, Harden F, Mengersen K. Segmentation of cone‐beam CT using a hidden Markov random field with informative priors. J Phys Conf Ser 2014; 489: 012076. [Google Scholar]
- 9. Du W, Yang JN, Chang EL, et al. A quality assurance procedure to evaluate cone‐beam CT image center congruence with the radiation isocenter of a linear accelerator. J Appl Clin Med Phys 2010; 11: 3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Varian Medical Systems . On‐Board Imager (OBI) Advanced Imaging Maintenance Manual [Instruction manual, version 1.6 software]. Document ID: B505010R01, Revision A. Palo Alto, CA, USA; May 2013.
- 11. Gao S, Du W, Balter P, Munro P, Jeung A. Evaluation of IsoCal geometric calibration system for Varian linacs equipped with on‐board imager and electronic portal imaging device imaging systems. J Appl Clin Med Phys 2014; 15: 4688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wu QJ, Li T, Wu Q, Yin FF. Adaptive radiation therapy: Technical components and clinical applications. Cancer J 2011; 17: 182–9. [DOI] [PubMed] [Google Scholar]


