Abstract
Socioeconomic position (SEP) is an important risk factor for malaria, but there is no consensus on how to measure SEP in malaria studies. We evaluated the relative strength of four indicators of SEP in predicting malaria risk in Nagongera, Uganda. A total of 318 children resident in 100 households were followed for 36 months to measure parasite prevalence routinely every 3 months and malaria incidence by passive case detection. Household SEP was determined using: 1) two wealth indices, 2) income, 3) occupation, and 4) education. Wealth Index I (reference) included only asset ownership variables. Wealth Index II additionally included food security and house construction variables, which may directly affect malaria. In multivariate analysis, only Wealth Index II and income were associated with the human biting rate, only Wealth Indices I and II were associated with parasite prevalence, and only caregiver's education was associated with malaria incidence. This is the first evaluation of metrics beyond wealth and consumption indices for measuring the association between SEP and malaria. The wealth index still predicted malaria risk after excluding variables directly associated with malaria, but the strength of association was lower. In this setting, wealth indices, income, and education were stronger predictors of socioeconomic differences in malaria risk than occupation.
Introduction
Malaria is closely associated with poverty, with the odds of malaria infection doubled on average in the poorest children within a community compared with the least poor.1 Measuring socioeconomic position (SEP), the suite of social and economic factors that determine the position held by individuals and groups within a society,2,3 is therefore critical both to studying the socioeconomic determinants of malaria and to most observational malaria research, since SEP confounds many relationships. However, as for many other health outcomes,4,5 the relative strength of metrics for evaluating the association between SEP and malaria has been little considered.
SEP can be measured directly using household consumption, expenditure or income, or indirectly using proxy metrics such as wealth indices, occupation, household vulnerability, and education.6 Consumption is generally considered to be the “gold standard” since it is the most direct indicator of SEP, is accurate to measure, and is relatively stable over time, yet it is expensive to collect, requiring detailed data on rental income, reported household consumption, and fees from durable items owned.7,8 Household income is another direct indicator of SEP, but also requires lengthy interviewing, is difficult to measure when derived from multiple sources, and is subject to temporal fluctuation.9,10
Wealth indices derived from assets have been developed as an alternative to consumption and are widely used as indirect metrics of SEP in malaria studies since they are simple to do and less subject to reporting biases. Wealth indices can have similar predictive values to consumption in estimating the relationship between SEP and health outcomes.6,11–13 However, findings can be affected by the weighting strategy and choice of included assets.14 For example, the inclusion of assets in the wealth index that are associated directly with the outcome of interest can increase the association between SEP and the outcome of interest.12 This is often relevant to malaria; for instance, house construction materials are sometimes included in wealth indices, especially if the Demographic and Health Survey (DHS) model is used.15,16 Yet house construction may be independently assessed as a risk factor for malaria, since it can influence house entry by mosquito vectors.17 SEP may also be measured indirectly using classes of occupation,18 and education, typically by measuring years of formal education completed, qualifications attained, or literacy.19,20
Previous studies of health inequalities have compared the household rankings produced by different SEP indicators12,14,21–24 and evaluated the association of different indicators with specific health outcomes.14,25–27 However, to our knowledge, only one study has previously evaluated indicators for measuring socioeconomic inequalities in relation to malaria risk.28 In that study, three indices were developed using data from 25 Tanzanian villages: a consumption index and two wealth indices derived from principal component analysis (PCA). Little difference was found between household rankings from the two wealth indices while a weak relationship was found between the wealth index and consumption index, with the household rankings based on PCA being less discriminatory than those based on consumption. However, a higher score in both the consumption and wealth index was associated with a reduced risk of malaria infection, indicating that the wealth index was a reasonable empirical and logistical alternative to consumption in that context.28
In this study, we evaluate the agreement between four indicators of SEP and explore how the risk of malaria in children varies with these indicators in Nagongera, rural Uganda. The four indicators compared are 1) two wealth indices derived from PCA, 2) income, 3) occupation, and 4) female caregiver's education. To our knowledge, this is the first evaluation of metrics other than wealth indices and consumption indices for measuring the association between SEP and malaria.
Materials and Methods
Study site.
The study was carried out between August 2011 and September 2014 in Nagongera sub-country, Tororo District, Uganda (00°46′10.6″N, 34°01′34.1″E). Rainfall is bimodal, with long rains from March to June and short rains from August to December. Malaria transmission is intense with an estimated annual Plasmodium falciparum entomological inoculation rate of 125.29 Anopheles gambiae s.s. (81.5%) and Anopheles arabiensis (18.5%) are the primary vectors.
Data source.
This study was part of a cohort study described elsewhere.29,30 All children aged 6 months to 10 years and their primary caregivers were enrolled from 100 randomly selected households in Nagongera in August–September 2011. Recruitment was dynamic, such that children reaching 6 months of age and meeting the eligibility criteria were enrolled and children reaching 11 years were withdrawn. Households with no remaining study participants were withdrawn, and seven additional households were recruited in September 2013. Participants were followed for all their health-care needs at the designated study clinic in Nagongera for 36 months, until September 2014. Outcomes measured were 1) human biting rate (HBR), measured by one night of CDC light trap (Model 512; John W. Hock Company, Gainesville, FL) catches per month in each home; 2) prevalence of parasitemia measured routinely every 3 months and confirmed by microscopy; and 3) incidence of all malaria episodes measured by passive case detection.
Household and women's surveys.
Data on indicators of SEP were collected from three surveys: 1) a baseline household survey conducted at the time of enrollment, 2) a second household survey conducted after 24 months of follow-up in September–October 2013, and 3) a women's survey, administered as a separate structured questionnaire after the second household survey. Both household surveys were administered to one designated adult respondent from each household, if they met four inclusion criteria: 1) usually resident, 2) present in the sampled household the night before the survey, 3) aged at least 18 years, and 4) agreed to provide informed written consent. The women's survey was administered to all adult women of childbearing age (18–49 years), resident in each study household, who met three inclusion criteria: 1) usual female resident, 2) present in the sampled household the night before the survey, and 3) agreed to provide informed written consent. Households were excluded if no adult respondent could be located on more than three occasions over 2 weeks (Table 1).
Table 1.
Variables included in two wealth indices for 100 households in Nagongera, Uganda, and their impact on household wealth index score
| Item | Proportion of households with item | Weight | |
|---|---|---|---|
| Wealth index I* | Wealth index II† | ||
| Radio | 0.53 | 0.29 | 0.18 |
| Mobile telephone | 0.61 | 0.30 | 0.27 |
| Table | 0.62 | 0.37 | 0.31 |
| Cupboard | 0.07 | 0.45 | 0.27 |
| Clock | 0.12 | 0.43 | 0.29 |
| Sofa | 0.05 | 0.41 | 0.31 |
| ≤ 2 people per sleeping room | 0.23 | 0.19 | 0.14 |
| Improved toilet | 0.18 | 0.29 | 0.20 |
| Transport to health facility other than walking | 0.33 | 0.10 | 0.05 |
| Tiled or metal roof | 0.65 | Not included | 0.21 |
| Cement or plaster wall | 0.24 | Not included | 0.35 |
| Wood, brick, or cement floor | 0.17 | Not included | 0.38 |
| Meat eaten ≥ 3 days in the past week | 0.40 | Not included | 0.26 |
| ≥ 3 meals per day in past week | 0.28 | Not included | 0.33 |
Wealth Index I: variables entered into principal component analysis: ownership of a 1) radio, 2) mobile telephone, 3) table, 4) cupboard, 5) clock, and 6) sofa; 7) people per sleeping room; 8) access to an improved toilet facility; and 9) main mode of transport to the health facility. Individual household wealth index scores are calculated by summing the coefficients of assets or characteristics possessed by each household.
Wealth Index II: variables entered into PCA were those included in Wealth Index I in addition to: 10) main roof material, 11) main wall material, 12) main floor material, 13) frequency of meat consumption, and 14) number of meals per day.
Variables for the wealth indices were collected in the first household survey (main mode of transport to the health facility) and in the second household survey (all other wealth index variables). House construction was recorded through separate house visits by the entomology field teams during 2013 and confirmed by the second household survey. Household income and occupation were measured in the second household survey. Educational status of each child's mother or the eldest female caregiver in each child's household was recorded in the women's survey.
Data analysis.
Data were collected using standardized case record forms entered into Microsoft Access (Microsoft Corp., Redmond, WA) for follow-up of study participants and using a paperless system for the household and women's surveys. Analyses were performed with Stata Version 13 (StataCorp, College Station, TX).
Wealth indices.
Two wealth indices were produced using PCA.11 Since there remains a paucity of underlying theory to support the choice of variables for PCA,10 we chose which variables to include based on a review of the literature, the 2006 Uganda DHS and the 2009 Uganda Malaria Indicator Survey.31,32 To avoid a narrow or skewed distribution of wealth index scores,16 we aimed to include a balance of variables on asset ownership and access to infrastructure.33
For Wealth Index I, the following variables were included in the PCA: ownership of a 1) radio, 2) mobile telephone, 3) table, 4) cupboard, 5) clock, and 6) sofa; 7) people per sleeping room; 8) access to an improved toilet; and 9) main mode of transport to the health facility. Wealth indices often include food security and house construction variables,34 but these factors may be independently associated with malaria in the study area.35,36 To evaluate whether including food security and house construction variables altered the association between the wealth index and malaria outcomes, Wealth Index II additionally included five variables: 10) main roof material, 11) main wall material, 12) main floor material, 13) frequency of meat consumption, and 14) number of meals per day. Households were ranked by wealth scores and grouped into tertiles. This was done for both wealth indices to give two categorical measures of SEP. Standardized, continuous wealth index scores were created by subtracting mean index scores and dividing by the standard deviation. In addition, the association between Wealth Index I and the five variables additionally included in Wealth Index II was assessed using Pearson's χ2 test.
Agreement between SEP indicators.
Rankings of households by Wealth Indices I and II were compared using kappa coefficients and Spearman rank correlation coefficients. Cross tabulations and Pearson's χ2 test were used to explore the associations between household-level indicators of SEP and tertiles of Wealth Index I.
Sensitivity of SEP indicators to malaria risk.
Each indicator of SEP was evaluated as a predictor of HBR, parasite prevalence, and incidence of clinical malaria. Negative binomial regression was used to model the number of Anopheles caught per household per night and the number of malaria cases per child with the number of catch nights and person years included as offset terms. The prevalence of malaria infection at the time of each routine clinic visit was modeled using logistic regression. First, a crude analysis was done in which the models for HBR included no covariates and the models for parasite prevalence and malaria incidence were minimally adjusted for age and gender. Second, to evaluate the relative sensitivity of SEP indicators to inequalities in malaria risk, all indicators of SEP were included in multivariable models for HBR, parasite prevalence, and malaria incidence. In all models, robust standard errors were used to adjust for clustering at the household level.
Ethics.
Ethical approval was given by the Uganda National Council for Science and Technology; Makerere University School of Medicine Research and Ethics Committee; University of California, San Francisco Committee for Human Research; and London School of Hygiene and Tropical Medicine Ethics Committee.
Results
Study population.
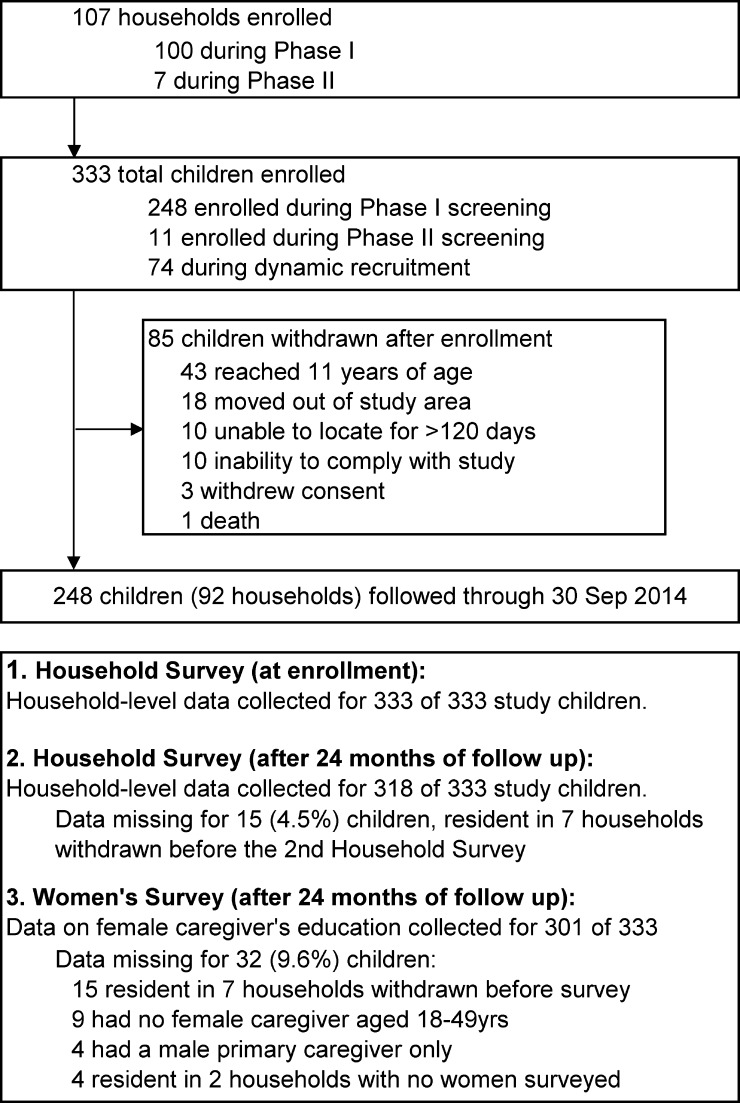
A total of 333 children in 107 total households were enrolled into the cohort study between August 2011 and September 2014. The mean age of study children during follow-up was 5.7 years, and 153 (46%) were female. All households were surveyed at enrollment in the first household survey. Seven households were withdrawn and replaced immediately before the second household survey in September 2013, such that the second household survey collected data for 100 households and 318 (95%) children. A total of 105 women were surveyed, such that data on female caregivers' education was collected for 301 (90%) children enrolled (Figure 1 ).
Figure 1.
Study profile.
Wealth indices.
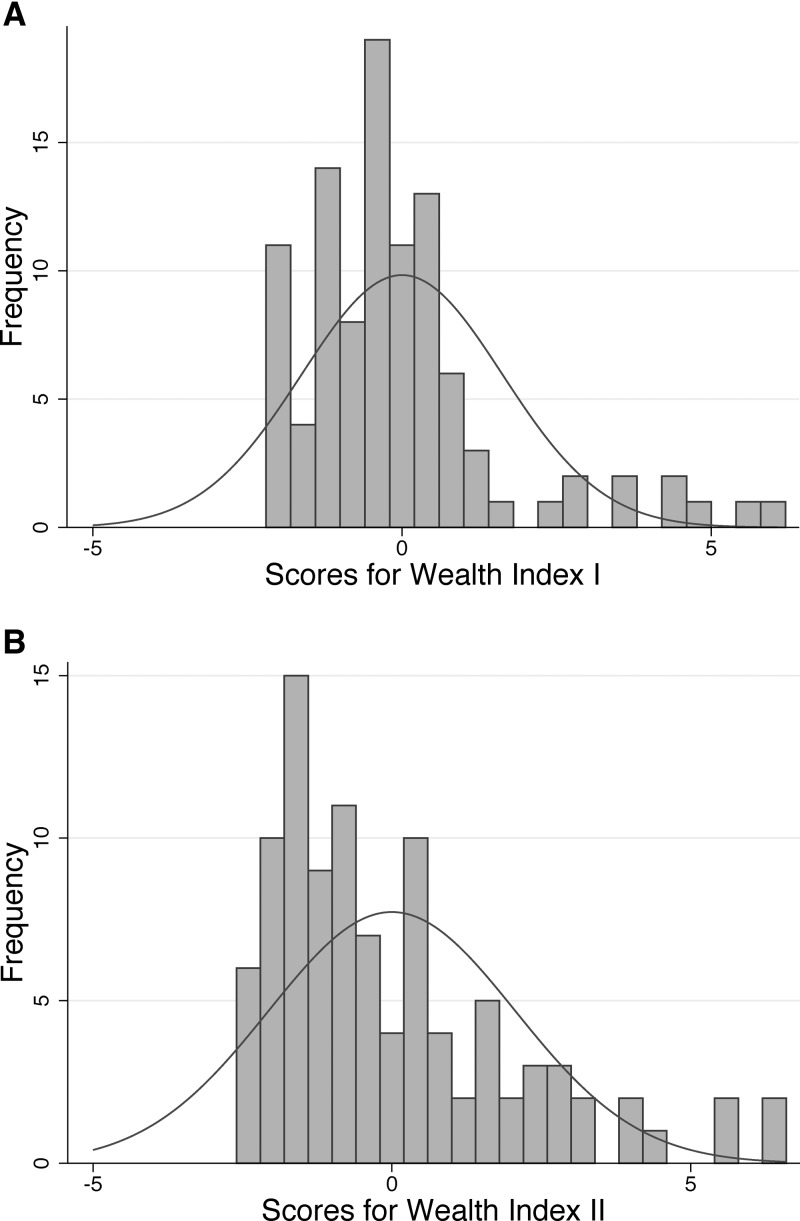
In Wealth Index I (no housing or food security variables), the first principal component explained 29.3% of overall variability in the asset variables. Greatest weight was given to ownership of a cupboard (Table 1). In Wealth Index II (all variables), the first principal component explained 30.5% of the overall variability in the asset variables. Greatest weight was given to main floor material. Both indices were right skewed, with wealth index scores ranging from −2.4 to 6.6 (Figure 2 ). Wealth Index I was strongly associated with the five variables additionally included in Wealth Index II: main roof material (P = 0.001), main wall material (P < 0.001), main floor material (P < 0.001), frequency of meat consumption (P < 0.001), and number of meals per day (P < 0.001).
Figure 2.
Distribution of wealth index scores from principal component analysis (PCA) in 100 households in Nagongera, Uganda. Variables entered into the PCA for Wealth Index I (A): ownership of a 1) radio, 2) mobile telephone, 3) table, 4) cupboard, 5) clock, and 6) sofa; 7) people per sleeping room; 8) access to an improved toilet facility; and 9) main mode of transport to the health facility. Additional variables entered for Wealth Index II (B): 10) main roof material, 11) main wall material, 12) main floor material, 13) frequency of meat consumption, and 14) number of meals per day.
Agreement between SEP indicators.
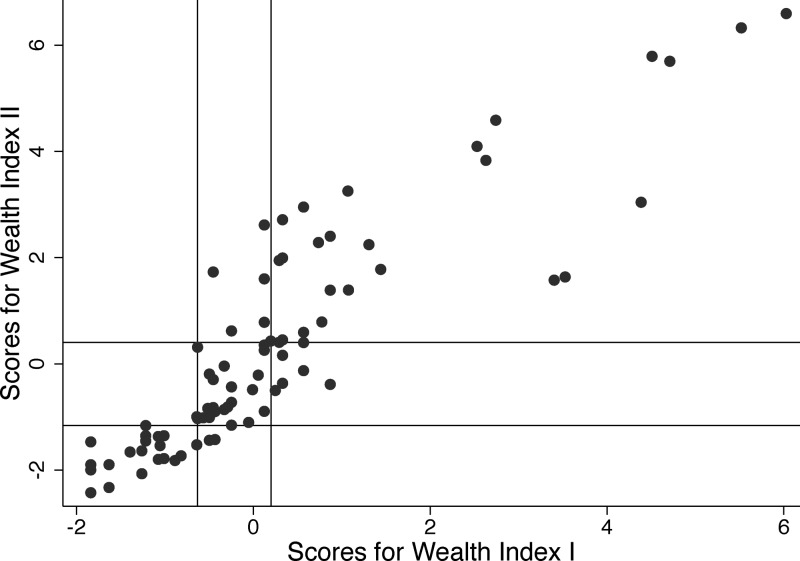
Ranking of households by scores from the two wealth indices was similar but not identical (Spearman's ρ = 0.93, P < 0.001) as was the grouping of households into tertiles (Spearman's ρ = 0.87, P < 0.001; κ = 0.73, P < 0.001), with 82% of households placed into the same tertile by both wealth indices (Figure 3 , Table 2). Households placed in higher tertiles of Wealth Index I (reference index) had greater income and better educated adult women than households in the lowest tertile (Table 2). However, there was no association between Wealth Index I and occupation.
Figure 3.
Association between scores from two wealth indices derived from principal component analysis in 100 households in Nagongera, Uganda. Lines perpendicular to the axes represent cutoffs for tertiles of each wealth index.
Table 2.
Agreement between indicators of SEP in 100 households in Nagongera, Uganda
| Indicator | All tertiles (%) | Wealth Index I (reference)* (%) | |||||
|---|---|---|---|---|---|---|---|
| Poorest | Middle | Highest | P | ||||
| Indicators at the level of the household | N = 35 | N = 32 | N = 33 | ||||
| Wealth index | Wealth Index II† (%) | Poorest tertile | 34 | 91.4 | 6.3 | 0.0 | < 0.001 |
| Middle tertile | 34 | 8.6 | 75.0 | 21.2 | |||
| Highest tertile | 32 | 0.0 | 18.8 | 78.8 | |||
| Wealth Index II† | Mean score (95% CI)‡ | – | −0.9 (−0.9, −0.8) | −0.1 (−0.3, 0.0) | 1.0 (0.7, 1.4) | < 0.001 | |
| Income | Total income from agriculture in the past 12 months, UGX (%) | < 100,000 | 37 | 51.4 | 40.6 | 18.8 | 0.001 |
| 100,000 to < 300,000 | 35 | 37.1 | 40.6 | 28.1 | |||
| ≥ 300,000 | 27 | 11.4 | 18.8 | 53.1 | |||
| Remittances received in the past 12 months (%) | No | 85 | 94.3 | 87.5 | 72.7 | 0.04 | |
| Yes | 15 | 5.7 | 12.5 | 27.3 | |||
| Occupation | Main occupation of the household head (%) | Agriculture or unskilled | 72 | 80.0 | 78.1 | 57.6 | 0.08 |
| Skilled | 28 | 20.0 | 21.9 | 42.4 | |||
| Main source of household income (%) | Agriculture or unskilled | 80 | 85.7 | 84.4 | 69.7 | 0.27 | |
| Skilled | 16 | 11.4 | 15.6 | 21.2 | |||
| Remittances or other | 4 | 2.9 | 0.0 | 9.1 | |||
| Indicator at the level of the child | N = 110 | N = 107 | N = 101 | ||||
| Education | Female caregiver ever attended school (%) | No | 24.9 | 29.9 | 21.9 | 22.5 | 0.33 |
| Yes | 75.1 | 70.1 | 78.1 | 77.6 | |||
| Female caregiver's highest level of school completed (%) | None | 24.9 | 29.9 | 21.9 | 22.5 | 0.003 | |
| Incomplete primary | 55.2 | 62.6 | 52.1 | 50.0 | |||
| Primary or higher | 19.9 | 7.5 | 26.0 | 27.6 | |||
SEP = socioeconomic position; UGX = Ugandan shilling.
Wealth Index I: variables entered into principal component analysis (PCA): ownership of a 1) radio, 2) mobile telephone, 3) table, 4) cupboard, 5) clock, and 6) sofa; 7) people per sleeping room; 8) access to a toilet facility; and 9) main mode of transport to the health facility.
Wealth Index II: variables entered into PCA were those included in Wealth Index I in addition to: 10) main roof material, 11) main wall material, 12) main floor material, 13) meat consumption, and 14) number of meals per day.
Standardized wealth index scores were created by subtracting mean index scores and dividing by the standard deviation. The P value for this variable was calculated using analysis of variance.
Sensitivity of SEP indicators to malaria risk.
Human biting rate.
A total of 124,746 adult female Anopheles were caught over 3,489 collection nights, yielding an overall HBR of 35.8 Anopheles per house per night. All households contributed at least one collection night. Controlling for all other SEP indicators, HBR was associated only with Wealth Index II (highest versus lowest tertile: adjusted incidence rate ratio (aIRR) = 0.67, 95% confidence intervals (CIs) = 0.49–0.92, P = 0.01) and income from remittances (received versus did not receive remittances in past 12 months: aIRR = 0.67, 95% CI = 0.47–0.96, P = 0.03) (Table 3).
Table 3.
Association between household-level indicators of SEP and the HBR in 100 households in Nagongera, Uganda
| Characteristic | HBR* | Crude IRR (95% CI) | P | Adjusted IRR (95% CI)† | P |
|---|---|---|---|---|---|
| Wealth index | |||||
| Wealth Index I | |||||
| Poorest tertile | 41.5 (1,136) | 1 | – | 1 | – |
| Middle tertile | 34.4 (1,132) | 0.86 (0.65–1.13) | 0.27 | 0.88 (0.68–1.14) | 0.34 |
| Highest tertile | 28.8 (1,110) | 0.71 (0.54–0.93) | 0.01 | 0.75 (0.56–1.02) | 0.06 |
| Continuous score‡ | – | 0.87 (0.77–0.99) | 0.03 | 0.92 (0.81–1.05) | 0.22 |
| Wealth Index II | |||||
| Poorest tertile | 40.8 (1,124) | 1 | – | 1 | – |
| Middle tertile | 35.8 (1,173) | 0.90 (0.68–1.18) | 0.44 | 0.93 (0.72–1.20) | 0.58 |
| Highest tertile | 27.9 (1,081) | 0.69 (0.52–0.91) | 0.008 | 0.67 (0.49–0.92) | 0.01 |
| Continuous score‡ | – | 0.79 (0.71–0.89) | < 0.001 | 0.80 (0.69–0.91) | 0.001 |
| Income | |||||
| Total income from agriculture in past 12 months (UGX) | |||||
| < 100,000 | 37.0 (1,291) | 1 | – | 1 | – |
| 100,000 to < 300,000 | 29.3 (1,142) | 0.80 (0.61–1.04) | 0.10 | 0.77 (0.59–1.01) | 0.06 |
| ≥ 300,000 | 40.0 (910) | 1.05 (0.79–1.40) | 0.72 | 1.16 (0.86–1.58) | 0.34 |
| Remittances received in the past 12 months | |||||
| No | 37.0 (2,872) | 1 | 1 | 1 | – |
| Yes | 23.0 (506) | 0.63 (0.46–0.86) | 0.004 | 0.67 (0.47–0.96) | 0.03 |
| Occupation | |||||
| Primary occupation of the household head | |||||
| Agriculture, unskilled, or cannot work | 35.3 (2,431) | 1 | 1 | 1 | – |
| Skilled | 34.1 (947) | 0.95 (0.74–1.24) | 0.72 | 0.98 (0.71–1.34) | 0.89 |
| Main source of household income | |||||
| Agriculture or unskilled | 36.8 (2,690) | 1 | – | 1 | – |
| Skilled | 30.0 (544) | 0.82 (0.60–1.13) | 0.23 | 0.83 (0.57–1.23) | 0.36 |
| Remittances or other | 19.2 (144) | 0.53 (0.30–0.95) | 0.03 | 0.80 (0.42–1.50) | 0.48 |
CI = confidence interval; HBR = human biting rate; IRR = incidence rate ratio; SEP = socioeconomic position; UGX = Ugandan shilling.
HBR: total female Anopheles/total collection nights. Total collection nights are shown in brackets.
IRR adjusted for categorical Wealth Index I and all other SEP indicators, excluding all other wealth index variables. IRRs for the categorical Wealth Index II and continuous Wealth Indices I and II variables were adjusted for all other indicators of SEP, excluding all other wealth index variables.
Standardized wealth index scores were created by subtracting mean index scores and dividing by the standard deviation.
Parasite prevalence.
A total of 3,367 routine blood smears were taken of which 1,037 (30.8%) were positive. All participants contributed at least one blood smear. Controlling for age, gender, and all other SEP indicators, parasite prevalence was associated with the wealth indices only (highest versus lowest tertile of Wealth Index I: adjusted odds ratio (aOR) = 0.57, 95% CI = 0.40–0.82, P = 0.003; Wealth Index II: aOR = 0.57, 95% CI = 0.40–0.82, P = 0.002) (Table 4).
Table 4.
Association between indicators of SEP and malaria infection in children aged six months to 10 years in Nagongera, Uganda
| Characteristic | % Positive* | Crude OR (95% CI)† | P | Adjusted OR (95% CI)‡ | P |
|---|---|---|---|---|---|
| Age at the time of the blood smear | |||||
| 6 months to < 3 years | 19.2 (657) | 1 | – | 1 | – |
| 3 to < 5 years | 27.6 (699) | 1.60 (1.18–2.18) | 0.002 | 1.60 (1.16–2.20) | 0.004 |
| 5 to < 11 years | 35.7 (2,011) | 2.34 (1.77–3.09) | < 0.001 | 2.40 (1.83–3.17) | < 0.001 |
| Gender | |||||
| Female | 29.9 (1,518) | 1 | – | 1 | – |
| Male | 31.5 (1,849) | 1.07 (0.86–1.35) | 0.54 | 1.04 (0.82–1.30) | 0.75 |
| Wealth index | |||||
| Wealth Index I | |||||
| Poorest | 38.4 (1,087) | 1 | – | 1 | – |
| Middle | 29.6 (1,170) | 0.65 (0.48–0.87) | 0.003 | 0.69 (0.51–0.94) | 0.02 |
| Highest | 25.3 (1,010) | 0.52 (0.35–0.78) | 0.001 | 0.57 (0.40–0.82) | 0.003 |
| Continuous score§ | – | 0.82 (0.64–1.04) | 0.10 | 0.80 (0.65–0.99) | 0.04 |
| Wealth Index II | |||||
| Poorest | 37.7 (1,109) | 1 | – | 1 | – |
| Middle | 28.9 (1,210) | 0.63 (0.46–0.87) | 0.004 | 0.64 (0.47–0.88) | 0.005 |
| Highest | 26.4 (948) | 0.58 (0.40–0.84) | 0.004 | 0.57 (0.40–0.82) | 0.002 |
| Continuous score§ | – | 0.73 (0.60–0.88) | 0.001 | 0.71 (0.59–0.86) | < 0.001 |
| Income | |||||
| Total income from agriculture in the past 12 months (UGX) | |||||
| < 100,000 | 34.0 (1,180) | 1 | – | 1 | – |
| 100,000 to < 300,000 | 29.7 (1,136) | 0.79 (0.56–1.11) | 0.17 | 0.77 (0.55–1.09) | 0.15 |
| ≥ 300,000 | 28.0 (908) | 0.75 (0.53–1.07) | 0.12 | 0.87 (0.62–1.22) | 0.43 |
| Remittances received in the past 12 months | |||||
| No | 32.2 (2,847) | 1 | – | 1 | – |
| Yes | 23.8 (420) | 0.62 (0.37–1.04) | 0.07 | 0.65 (0.40–1.05) | 0.08 |
| Occupation | |||||
| Primary occupation of the household head | |||||
| Agriculture or unskilled | 32.9 (2,416) | 1 | – | 1 | – |
| Skilled | 26.3 (851) | 0.76 (0.51–1.15) | 0.19 | 0.77 (0.55–1.08) | 0.13 |
| Main source of household income | |||||
| Agriculture or unskilled | 32.1 (2,635) | 1 | – | 1 | – |
| Skilled | 27.0 (497) | 0.82 (0.48–1.41) | 0.48 | 1.03 (0.58–1.81) | 0.93 |
| Remittances or other | 28.9 (135) | 0.83 (0.33–2.07) | 0.68 | 1.04 (0.49–2.20) | 0.93 |
| Education | |||||
| Female caregiver ever attended school | |||||
| No | 33.4 (788) | 1 | – | 1 | – |
| Yes | 30.4 (2,296) | 0.90 (0.65–1.25) | 0.54 | 0.87 (0.59–1.29) | 0.49 |
| Female caregiver's highest level of school completed | |||||
| None | 33.4 (788) | 1 | – | 1 | – |
| Incomplete primary | 31.7 (1,703) | 0.96 (0.68–1.36) | 0.83 | 1.26 (0.92–1.74) | 0.16 |
| Primary or higher | 26.6 (593) | 0.74 (0.48–1.15) | 0.18 | Omitted due to collinearity | – |
CI = confidence interval; OR = odds ratio; SEP = socioeconomic position; UGX = Ugandan shilling.
Percentage of blood slides positive with malaria parasites. Total blood slides are shown in brackets.
OR minimally adjusted for age at the time of the blood smear and gender.
OR adjusted for mean age during follow-up, gender, categorical Wealth Index I, and all other SEP indicators, excluding all other wealth index variables. ORs for the categorical Wealth Index II and continuous Wealth Indices I and II variables were adjusted for mean age during follow-up, gender, and all other indicators of SEP, excluding all other wealth index variables.
Standardized wealth index scores were created by subtracting mean index scores and dividing by the standard deviation.
Incidence of clinical malaria.
A total of 2,399 uncomplicated malaria episodes were diagnosed after 802 person-years of follow up, yielding an overall incidence of 3.0 episodes per person-year at risk. One participant was withdrawn immediately after enrollment and did not contribute person-time. Controlling for age, gender, and all other SEP indicators, only female caregiver's education was associated with malaria incidence (attended school versus never attended school: aIRR = 0.70, 95% CI = 0.49–0.98, P = 0.04). Malaria incidence was not associated with either of the wealth indices nor income or occupation (Table 5).
Table 5.
Association between indicators of SEP and malaria incidence in children aged 6 months to 10 years in Nagongera, Uganda
| Characteristic | Malaria incidence* | Crude IRR (95% CI)† | P | Adjusted IRR (95% CI)‡ | P |
|---|---|---|---|---|---|
| Mean age during follow-up | |||||
| 6 months to < 3 years | 4.1 (134) | 1 | – | 1 | – |
| 3 to < 5 years | 4.2 (177) | 1.01 (0.85–1.19) | 0.93 | 0.99 (0.82–1.20) | 0.96 |
| 5 to < 11 years | 2.3 (491) | 0.54 (0.46–0.65) | < 0.001 | 0.54 (0.46–0.65) | < 0.001 |
| Gender | |||||
| Female | 2.7 (361) | 1 | – | 1 | – |
| Male | 3.2 (441) | 1.13 (0.97–1.32) | 0.12 | 1.14 (0.97–1.35) | 0.11 |
| Wealth index | |||||
| Wealth Index I | |||||
| Poorest | 3.0 (258) | 1 | – | 1 | – |
| Middle | 3.1 (280) | 1.12 (0.90–1.40) | 0.31 | 1.16 (0.93–1.43) | 0.18 |
| Highest | 2.9 (241) | 1.05 (0.83–1.34) | 0.68 | 1.08 (0.86–1.37) | 0.51 |
| Continuous score§ | – | 0.95 (0.86–1.06) | 0.35 | 0.96 (0.88–1.06) | 0.46 |
| Wealth Index II | |||||
| Poorest | 3.2 (264) | 1 | – | 1 | – |
| Middle | 2.9 (289) | 1.03 (0.83–1.29) | 0.77 | 1.10 (0.90–1.35) | 0.33 |
| Highest | 2.9 (226) | 1.00 (0.78–1.27) | 0.98 | 1.04 (0.80–1.36) | 0.75 |
| Continuous score§ | – | 0.95 (0.84–1.07) | 0.38 | 0.97 (0.86–1.10) | 0.67 |
| Income | |||||
| Total income from agriculture in the past 12 months (UGX) | |||||
| < 100,000 | 3.1 (283) | 1 | – | 1 | – |
| 100,000 to < 300,000 | 2.5 (270) | 0.84 (0.66–1.06) | 0.14 | 0.79 (0.62–1.00) | 0.05 |
| ≥ 300,000 | 3.5 (215) | 1.13 (0.90–1.42) | 0.29 | 1.11 (0.88–1.40) | 0.37 |
| Remittances received in the past 12 months | |||||
| No | 3.1 (679) | 1 | – | 1 | – |
| Yes | 2.6 (100) | 0.88 (0.65–1.20) | 0.42 | 1.10 (0.76–1.57) | 0.62 |
| Occupation | |||||
| Primary occupation of the household head | |||||
| Agriculture or unskilled | 3.0 (576) | 1 | – | 1 | – |
| Skilled | 3.0 (203) | 0.93 (0.74–1.19) | 0.58 | 0.90 (0.66–1.23) | 0.51 |
| Main source of household income | |||||
| Agriculture or unskilled | 3.1 (628) | 1 | – | 1 | – |
| Skilled | 2.8 (118) | 0.93 (0.70–1.23) | 0.59 | 1.01 (0.69–1.48) | 0.97 |
| Remittances or other | 2.5 (33) | 0.77 (0.43–1.36) | 0.37 | 0.67 (0.38–1.19) | 0.17 |
| Education | |||||
| Female caregiver ever attended school | |||||
| No | 3.5 (188) | 1 | – | 1 | – |
| Yes | 2.9 (546) | 0.80 (0.67–0.95) | 0.01 | 0.70 (0.49–0.98) | 0.04 |
| Female caregiver's highest level of school completed | |||||
| None | 3.5 (188) | 1 | – | 1 | – |
| Incomplete primary | 3.0 (406) | 0.83 (0.69–1.01) | 0.06 | 1.26 (0.91–1.74) | 0.16 |
| Primary or higher | 2.4 (140) | 0.69 (0.53–0.91) | 0.008 | Omitted due to collinearity | – |
CI = confidence interval; IRR = incidence rate ratio; SEP = socioeconomic position; UGX = Ugandan shilling.
Malaria incidence: episodes per person-years at risk. Total person-years at risk shown in brackets.
IRR minimally adjusted for mean age during follow-up and gender.
IRR adjusted for mean age during follow-up, gender, categorical Wealth Index I, and all other SEP indicators, excluding all other wealth index variables. IRRs for the categorical Wealth Index II and continuous Wealth Indices I and II variables were adjusted for mean age during follow-up, gender, and all other indicators of SEP, excluding all other wealth index variables.
Standardized wealth index scores were created by subtracting mean index scores and dividing by the standard deviation.
Discussion
We compared two wealth indices and three additional indicators of SEP for measuring socioeconomic inequalities in relation to malaria risk in children in a rural, high transmission area of Uganda. HBR was 29–31% lower in households in the highest tertile of Wealth Indices I and II, compared with the lowest tertile, and 37% lower in households that received any remittances in the past 12 months. However, after controlling for all other SEP indicators, only access to remittances and Wealth Index II (which included house construction and food security variables) were significantly associated with lower HBR. Controlling for age, gender, and all other SEP indicators, the odds of malaria infection were 43% lower in children in the highest tertile of both Wealth Indices I and II, compared with the lowest tertile, and malaria incidence was 30% lower in children whose primary female caregiver had attended school compared with those whose caregiver had not. No association was found between occupation and malaria.
Since their early development and adoption by the DHS and World Bank,11,37 wealth indices have become widely used to measure SEP in epidemiological studies in low- and middle-income settings.1 Although there is a continuing debate over how well wealth indices agree with consumption,13 they are a pragmatic means to assess SEP rapidly and can theoretically represent long-term SEP, similar to consumption expenditure, because assets are relatively resilient to short-term economic shocks.6 We observed that the wealth index was sensitive to socioeconomic inequalities in HBR and parasite prevalence, and indeed it is possible that this metric was less subject to measurement error than other metrics and more indicative of long-term living conditions.38 The one previous comparison of indicators for measuring socioeconomic inequalities in malaria risk found that the wealth index was a reasonable alternative to consumption in rural Tanzania.28
Although there is a paucity of underlying theory to guide the choice of included variables in wealth indices,10 the inclusion of assets directly associated with the outcome of interest may increase the observed socioeconomic inequalities in health.12 Furthermore, variables often included in the wealth index, such as house type, are sometimes evaluated independently as malaria risk factors.17 We therefore sought to evaluate how the choice of variables included in the wealth index affected the association with malaria outcomes. Household rankings from the two wealth indices were highly correlated, but controlling for other SEP indicators, only the wealth index that included house construction and food security variables was associated with HBR. House structure may explain part of the association between SEP and malaria in Nagongera since it is both a malaria risk factor36 and associated with relative wealth, so it is plausible that its inclusion strengthens the association between the wealth index and malaria risk and that there is a trade-off between house type and SEP in the model. Previous wealth indices based on assets alone39 and on assets and food security36 in the same district were not significantly associated with parasite prevalence.
We observed that female caregiver's education was better able to predict differences in malaria incidence than other metrics of SEP. Good education is commonly associated with improved health outcomes elsewhere26,40 and generally considered to be a useful metric of SEP since it is a proxy for knowledge-based assets and can be strongly related to other measures of SEP such as income and occupation.6,20 However, education was not associated with HBR nor parasite prevalence, and the epidemiological meaning of this remains unclear. The use of education as a metric of SEP can be complicated by changes in the cost, ease, and social expectations of educational attendance over time.6 While we restricted our analysis to female education only, removing gender differences, variation across women's age groups or ethnic groups may have persisted, making it difficult to identify variation in malaria risk reflecting education alone.
We found no association between agricultural income and malaria, but we observed that HBR was lower in households that had received remittances in the past 12 months. We also observed that both agricultural income and access to remittances were strongly associated with the reference wealth index. It is plausible that income may be a reasonable proxy for underlying SEP, but our specific measures of income were inadequate to fully detect differences in malaria risk related to SEP. Income is difficult to measure in low-income settings such as Nagongera, because of multiple household income sources, home production, and seasonal or annual variation in income.6 Thus, we simply estimated the total estimated income from the sale of crops and livestock and recorded whether households had access to remittances. Our approach did not account for other income sources and this, together with measurement error due to recall bias, unwillingness to divulge income, and interviewing only the household head, may help explain the inconsistent association with malaria outcomes.9 Of course, our findings may alternatively reflect a scenario of no underlying relationship between income and malaria if a lack of cash income is not a barrier to having those characteristics that offer some protection against malaria.
We did not observe any association between malaria infection risk and occupation, when classed as unskilled and agricultural versus skilled. Occupational life can be complex and therefore difficult to measure in low-income settings since people often have casual, seasonal, or multiple jobs.41 In Nagongera, where households predominantly rely on smallholder farming and small home enterprises, further differentiation between commercial and subsistence farmers may have been needed to determine underlying SEP.27 For example, the DHS typically classifies households using occupation-based social class measures that include subdivisions of types of agricultural activity.18
Overall, our study supports the continued use of wealth indices as a pragmatic approach to estimating SEP in malaria studies. Although we did not compare the wealth index with consumption, the wealth index was consistently more sensitive to inequalities in malaria risk than income and occupation. However, there remains a need to better understand how to select and weight the included variables. Although the inclusion of variables directly associated with the outcome may inflate health inequalities,12 such variables may be an important part of what makes wealth protective. Moreover, the inclusion or exclusion of different variables can improve our understanding of the causal pathway between SEP and health outcomes.12 However, it may be pragmatic to remove from the wealth index any variables being investigated as exposures of interest. Individual studies should consider what is appropriate for the study setting and design.
Our study has a number of limitations. First, to avoid excessive questioning, we did not evaluate consumption, yet this is the gold standard measure of SEP.6 Second, metrics such as income and occupation may be subject to measurement error due to recall bias, inaccurate reporting during lengthy interviews, and social desirability bias when asking questions related to socioeconomic conditions. Third, our findings may not be generalizable outside the study population in Nagongera. For example, in generating both wealth indices the smallest weight was assigned to mode of transport to the health facility, possibly reflecting reimbursement of clinic travel expenses to study participants. In addition, we compared two wealth indices only, limiting the conclusions that may be drawn. Fourth, we used PCA as a weighting strategy, but this was originally designed for use with continuous data. We also did not analyze other weighting strategies, such as factor analysis or multiple correspondence analysis, although a recent study concluded that the weighting strategy is less important than other considerations, such as variable coding, in improving wealth index agreement with consumption.24 Finally, variables used to construct the wealth index were collected at more than one time point. However, we consider household assets to be relatively stable over time.6
In conclusion, wealth indices, income, and education were stronger predictors of socioeconomic differences in malaria risk than occupation in this setting. The wealth index was still a predictor of malaria risk after excluding variables directly associated with malaria, but the strength of association was lower.
ACKNOWLEDGMENTS
We are grateful to the study participants and their families. We thank the Infectious Diseases Research Collaboration (IDRC) for administrative and technical support and the Malaria Centre at the London School of Hygiene and Tropical Medicine.
Footnotes
Financial support: This work was supported by NIH/NIAID (U19AI089674); the Leverhulme Centre for Integrative Research in Agriculture and Health; Research and Policy for Infectious Disease Dynamics (RAPIDD) programme of the Science and Technology Directorate, U.S. Department of Homeland Security, the Fogarty International Center (U.S. National Institutes of Health) and the Bill & Melinda Gates Foundation (OPP1053338).
Authors' addresses: Lucy S. Tusting and Jo Lines, Department of Disease Control, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mails: lucy.tusting@lshtm.ac.uk and jo.lines@lshtm.ac.uk. John C. Rek and Emmanuel Arinaitwe, Infectious Disease Research Collaboration, Mulago Hospital Complex, Kampala, Uganda, E-mails: jrek@idrc-uganda.org and earinaitwe@idrc-uganda.org. Sarah G. Staedke, Department of Clinical Research, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mail: sarah.staedke@lshtm.ac.uk. Moses R. Kamya, School of Medicine, Makerere University College of Health Sciences, Kampala, Uganda, E-mail: mkamya@idrc-uganda.org. Christian Bottomley, MRC Tropical Epidemiology Group, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mail: christian.bottomley@lshtm.ac.uk. Deborah Johnston, Department of Economics, School of Oriental and African Studies, London, United Kingdom, E-mail: dj3@soas.ac.uk. Grant Dorsey, Department of Medicine, University of California at San Francisco, San Francisco, CA, E-mail: grant.dorsey@ucsf.edu. Steve W. Lindsay, School of Biological and Biomedical Sciences, Durham University, Durham, United Kingdom, E-mail: s.w.lindsay@durham.ac.uk.
References
- 1.Tusting LS, Willey B, Lucas H, Thompson J, Kafy HT, Smith R, Lindsay S. Socioeconomic development as an intervention against malaria: a systematic review and meta-analysis. Lancet. 2013;382:963–972. doi: 10.1016/S0140-6736(13)60851-X. [DOI] [PubMed] [Google Scholar]
- 2.Lynch J, Kaplan G. Socioeconomic position. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York, NY: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- 3.Boccia D, Hargreaves J, De Stavola B, Fielding K, Schaap A. The association between household socioeconomic position and prevalent tuberculosis in Zambia: a case-control study. PLoS One. 2011;6:e20824. doi: 10.1371/journal.pone.0020824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shavers V. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99:1013–1023. [PMC free article] [PubMed] [Google Scholar]
- 5.Braveman P, Cubbin C, Egerter S, Chideya S, Marchi K. Socioeconomic status in health research: one size does not f𝚤t all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 6.Howe L, Galobardes B, Matijasevich A, Gordon D, Johnston D, Onwujekwe O, Patel R, Webb EA, Lawlor DA, Hargreaves JR. Measuring socio-economic position for epidemiological studies in low- and middle-income countries: a methods of measurement in epidemiology paper. Int J Epidemiol. 2012;41:871–886. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deaton A, Zaidi S. Guidelines for Constructing Consumption Aggregates for Welfare Analysis. Princeton, NJ: World Bank; 1999. [Google Scholar]
- 8.Makinen M, Waters H, Rauch M. Inequalities in health care use and expenditures: empirical data from eight developing countries and countries in transition. Bull World Health Organ. 2000;78:55–65. [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher M, Reimer JJ, Carr ER. Who Should Be Interviewed in Surveys of Household Income? Washington, DC: International Food Policy Research Institute; 2010. [Google Scholar]
- 10.Montgomery M, Gragnolati M, Burke K, Paredes E. Measuring living standards with proxy variables. Demography. 2000;37:155–174. [PubMed] [Google Scholar]
- 11.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data-or tears: an application to educational enrolments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 12.Houweling TA, Kunst AE, Mackenbach JP. Measuring health inequality among children in developing countries: does the choice of the indicator of economic status matter? Int J Equity Health. 2003;2:8. doi: 10.1186/1475-9276-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howe LD, Hargreaves JR, Gabrysch S, Huttly SRA. Is the wealth index a proxy for consumption expenditure? A systematic review. J Epi Comm Health. 2009;63:871–877. doi: 10.1136/jech.2009.088021. [DOI] [PubMed] [Google Scholar]
- 14.Boccia D, Hargreaves J, Howe L, De Stavola B, Fielding K, Ayles H, Godfrey-Faussett P. The measurement of household socio-economic position in tuberculosis prevalence surveys: a sensitivity analysis. Int J Tuberc Lung Dis. 2013;17:39–45. doi: 10.5588/ijtld.11.0387. [DOI] [PubMed] [Google Scholar]
- 15.Rutstein SO. Steps to Constructing the New DHS Wealth Index. Rockville, MD: ICF International; 2015. [Google Scholar]
- 16.Vyas S, Kumuranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;6:459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- 17.Tusting LS, Ippolito M, Kleinschmidt I, Willey B, Gosling R, Dorsey G, Lindsay S. The evidence for improving housing to reduce malaria: a systematic review and meta-analysis. Malar J. 2015;14:209. doi: 10.1186/s12936-015-0724-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ganzeboom HBG, Treiman DJ, Stephenson E. The International Stratification and Mobility File, 2009. 2009. http://www.harryganzeboom.nl/ISMF/index.htm Available at.
- 19.Galobardes S, Lawlor MS, Lynch DA, Davey JW, Smith G. Indicators of socioeconomic position (Part 1) J Epidemiol Community Health. 2006;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galobardes S, Lawlor MS, Lynch DA, Davey JW, Smith G. Indicators of socioeconomic position (Part 2) J Epidemiol Community Health. 2006;60:95–101. doi: 10.1136/jech.2004.028092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sahn DE, Stifel D. Exploring alternative measures of welfare in the absence of expenditure data. Rev Income Wealth. 2003;49:463–489. [Google Scholar]
- 22.Morris SS, Carletto C, Hoddinot J, Christiaensen LJM. Validity of rapid estimates of household wealth and income for health surveys in rural Africa. J Epidemiol Community Health. 2000;54:381–387. doi: 10.1136/jech.54.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scoones I. Investigating difference: applications of wealth ranking and household survey approaches among farming households in southern Zimbabwe. Dev Change. 1995;26:67–88. [Google Scholar]
- 24.Howe LD, Hargreaves JR, Huttly SR. Issues in the construction of wealth indices for the measurement of socio-economic position in low-income countries. Emerg Themes Epidemiol. 2008;5:3. doi: 10.1186/1742-7622-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lindelow M. Sometimes more equal than others: how health inequalities depend on the choice of welfare indicator. Health Econ. 2006;15:263–279. doi: 10.1002/hec.1058. [DOI] [PubMed] [Google Scholar]
- 26.Wamani H, Tylleskär T, Astrøm A, Tumwine J, Peterson S. Mothers' education but not fathers' education, household assets or land ownership is the best predictor of child health inequalities in rural Uganda. Int J Equity Health. 2004;13:9. doi: 10.1186/1475-9276-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hargreaves JR, Morison LA, Gear GSS. Assessing household wealth in health studies in developing countries: a comparison of participatory wealth ranking in rural South Africa. Emerg Themes Epidemiol. 2007;4:4. doi: 10.1186/1742-7622-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Somi M, Butler J, Vahid F, Njau J, Kachur S, Abdulla S. Use of proxy measures in estimating socioeconomic inequalities in malaria prevalence. Trop Med Int Health. 2008;13:354–364. doi: 10.1111/j.1365-3156.2008.02009.x. [DOI] [PubMed] [Google Scholar]
- 29.Maxwell K, Smith DL, Hutchinson R, Kigozi R, Lavoy G, Kamya MR, Staedke S, Donnelly MJ, Drakeley C, Dorsey G, Lindsay SW. Estimating the annual entomological inoculation rate for Plasmodium falciparum transmitted by Anopheles gambiae s.l. using three sampling methods in three sites in Uganda. Malar J. 2014;13:111. doi: 10.1186/1475-2875-13-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamya MR, Arinaitwe E, Wanzira H, Katureebe A, Barusya C, Kigozi SP, Kilama M, Tatem AJ, Rosenthal PJ, Drakeley C, Lindsay SW, Staedke SG, Smith DL, Greenhouse B, Dorsey G. Malaria transmission, infection and disease at three sites with varied transmission intensity in Uganda: implications for malaria control. Am J Trop Med Hyg. 2015;92:903–912. doi: 10.4269/ajtmh.14-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Uganda Bureau of Statistics . Uganda Demographic and Health Survey. Kampala, Uganda: Uganda Bureau of Statistics; 2011. [Google Scholar]
- 32.Uganda Bureau of Statistics . Uganda Malaria Indicator Survey. Kampala, Uganda: Uganda Bureau of Statistics; 2009. [Google Scholar]
- 33.McKenzie DJ. Measuring inequality with asset indicators. J Popul Econ. 2005;18:229–260. [Google Scholar]
- 34.de Castro MC, Fisher MG. Is malaria illness among young children a cause or a consequence of low socioeconomic status? Evidence from the united Republic of Tanzania. Malar J. 2012;11:161. doi: 10.1186/1475-2875-11-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arinaitwe E, Gasasira A, Verret W, Homsy J, Wanzira H, Kakuru A, Sandison TG, Young S, Tappero JW, Kamya MR, Dorsey G. The association between malnutrition and the incidence of malaria among young HIV-infected and -uninfected Ugandan children: a prospective study. Malar J. 2012;11:90. doi: 10.1186/1475-2875-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wanzirah H, Tusting LS, Arinaitwe E, Katureebe A, Maxwell K, Rek J, Bottomley C, Staedke S, Kamya M, Dorsey G, Lindsay SW. Mind the gap: house construction and the risk of malaria in Ugandan children. PLoS One. 2015;10:e0117396. doi: 10.1371/journal.pone.0117396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gwatkin DR, Rustsein S, Johnston K, Suliman E, Wagstaff A. Socio-Economic Differences in Health, Nutrition and Population in Developing Countries: An Overview. Washington, DC: World Bank; 2007. [PubMed] [Google Scholar]
- 38.Falkingham J, Namazie C. Measuring Health and Poverty: A Review of Approaches to Identifying the Poor. London, United Kingdom: DFID Health Systems Resource Centre (HSRC); 2002. [Google Scholar]
- 39.Pullan RL, Bukirwa H, Staedke SG, Snow RW, Brooker S. Plasmodium infection and its risk factors in eastern Uganda. Malar J. 2010;9:2. doi: 10.1186/1475-2875-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gakidou E, Cowling K, Lozano RC, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 41.ILO . Women and Men in the Informal Economy: A Statistical Picture. Geneva, Switzerland: International Labor Organization; 2002. [Google Scholar]