Abstract
Snakebite envenomation affects thousands of people annually in Nepal. Published hospital-based studies of snakebite treatment in Nepal are scarce. Here we present the results of the first prospective, cross-sectional study of hospitalized envenomed snakebite cases in southcentral Nepal, a region characterized by poor pre-hospital care of snakebites, limited supply and excessive use of antivenom, and a high case/fatality ratio. We seek to identify clinical management problems and suggest potential interventions to improve treatment of snakebites. Out of the 342 patients presented with snakebites to an urban emergency department in the Terai region of Nepal between April and September of 2007, 39 patients were enrolled based on development of ptosis or swelling of bitten body parts. We collected patient demographic information and documented circumstances of snakebite, prehospital care, hospital care, and development of complications. Among 39 envenomated patients admitted to Bharatpur Hospital enrolled in the study 34 (92%) exhibited features of clinically significant neurotoxicity and were treated with antivenom. Antivenom use ranged from 4 to 98 vials of Polyspecific Indian Antivenom per patient. Each of victims (n=34) received antivenom an average of 4.3 (median) ±0.73 (standard error of mean) hours after receiving the snakebite. The overall case fatality rate was 21%. Neurotoxicity developed up to 25.8hr after suspected elapid snakebites. This was not observed for viperid snake bites. No enrolled patients received any of the currently recommended first aid for snake bite. The prevalence of nocturnal elapid snake bites, the practice of inappropriate first aid measures and highly variable administration of antivenom were identified as major challenges to appropriate care in this study. To address these issues we suggest development of a comprehensive checklist for identification of snake species, management of envenomation, and an educational program which teaches proper care at all stages of snakebite treatment.
Keywords: Antivenom, envenomation, first aid, mortality, neurotoxicity, snakebite
Introduction
Snakebite envenomation is a frequently fatal condition in the tropical and sub-tropical regions in south Asia, southeast Asia, Africa, and South America (Kasturiratne et al, 2008). Although high snakebite mortality is often reported to occur in India (Westly, 2013), the highest incidence of venomous snakebites in Asia (162 annual deaths per 100,000 population) is in the southeastern Nepal (Sharma et al, 2004a). Among the 18 described species of venomous snakes in Nepal (Sharma et al, 2013), the Common Krait (Bungarus caeruleus) and the Common Cobra (Naja naja) account for the majority of morbidity and mortality (Magar et al, 2013). Case fatality ratios range from 3% to 58% (see Table 1), yet snakebite has not been a prioritized public health issue in Nepal (Nepal Health Research Council, 2013). Published studies of snakebites in Nepal are scarce and mostly retrospective in nature (Joshi, 1983; Heap and Cowan, 1991; Hansdak et al, 1998; Devkota et al, 2000; Sharma et al, 2003; Bista et al, 2005; Pandey, 2006; Thapa and Pandey, 2009; Joshi, 2010; Shrestha, 2011; Paudel and Sharma, 2012; Magar et al, 2013; World Health Organization, 1987). This may be because documentation of snakebites is often incomplete (Magar et al, 2013).
Table 1.
Summary of snakebite mortality reported from Nepal [# = Paper published year; full paper titles are listed in the reference section; * = Epidemiology and Disease Control Division, Ministry of Health, Nepal Government]
| Study author/s | Year (#) | Data sources or location | (CFRs) |
|---|---|---|---|
| WHO | 1987 | 15 district hospitals, Nepal; 1980–1985 | 4.5% |
| Heap and Cowan | 1991 | British Military Hospital, Dharan, the southeastern Nepal; 1989 | 27% |
| Hansdak et al. | 1998 | BPK Institute of Health Sciences, Dharan, the southeastern Nepal; Aug. 1993 to Nov. 1994 | 22% |
| Sharma et al. | 2003 | 10 health institutions, the southeastern Nepal; Jan. to Dec. 2000 | 3–58% |
| Sharma et al. | 2004a | Chulachuli, Itahara, Kerabari, Rajghat, Shivagunj communities; the southeastern Nepal; Dec. 2001 | 27% |
| Sharma et al. | 2004b | Damak Red Cross Sub-center, Jhapa, the southeastern Nepal; Jan. to Dec. 2000 | 3% |
| EDCD* | 2005 | 33 health institutions, Nepal; 2003 | 15% |
| Pandey | 2006 | Bharatpur Hospital, Chitwan and Kaligandaki Community Hospital, Nawalparasi, the south central and the southwestern Nepal, respectively; Sep. 2004 to Sep. 2005 | 27% |
| Chappuis et al. | 2007 | Chulachuli, Itahara, Kerabari, Rajghat communities; the southeastern Nepal; Nov. to Dec. 2003 | 23% |
| Pandey | 2007 | 23 communities; Chitwan and Nawalparasi, the southcentral and the southwestern Nepal; Apr. to Sep. 2005 | 27% |
| Thapa and Pandey | 2009 | 43 health institutions, Nepal; 2005 | 13% |
| Joshi | 2010 | Health institutions in six mid-hill and 24 lowland districts, Nepal; 2008 | 24% |
| Pandey et al. | 2010a | Madi Valley communities, Chitwan, the southcentral Nepal; Oct. 2007 to Oct. 2008 | 22% |
| Paudel | 2012 | Lumbini Zonal Hospital, Butwal, the southwestern Nepal; 2004 to 2010 | 12–28% |
| Magar et al. | 2013 | 10 health institutions in Western Development Region; 2008 to 2010 | 13% |
In this study we present the results of a prospective, observational study of venomous snakebite cases in southcentral Nepal, a region characterized by poor pre-hospital care of snakebites, limited supply and excessive use of antivenom, and a high case fatality ratio.
Materials and methods
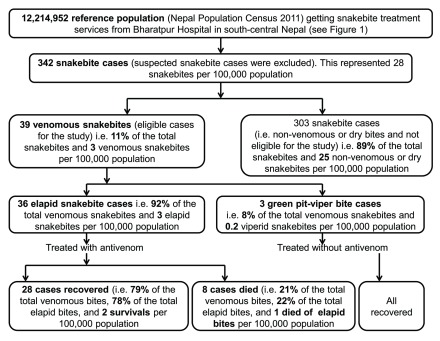
This was a prospective, cross-sectional, and descriptive study of snakebite victims during the snakebite season of 2007 (from April to September). This study was conducted at Bharatpur Hospital, a 435-bed tertiary hospital which serves a major city and multiple rural areas in the regions of the southcentral lowlands (Terai region). Out of 342 patients with a history of snakebite, we enrolled 39 envenomated cases (Figure 1). Patients who developed ptosis or swelling of bitten body parts were selected. Study participants were consented and enrolled by the Emergency Department physician on call and a study coordinator. Patients were excluded if they were discharged after observation of 12 to 24 hours without clinical symptoms of envenomation or required no treatment with antivenom. All enrolled patients received inpatient level hospital care.
Figure 1.
Schematic diagram of the snakebite cases selected for the study
Demographic data and hospital course were recorded (shown in Table 2). Patients, medical decision makers, bystanders and prehospital care providers provided historical information. Determination of snake species was done by examination of available snake specimens when possible. All collected snakes were identified using published snake identification keys (Schleich and Kästle, 2002) and archived in the Madi Valley Educational Museum, Chitwan.
Table 2.
Socio-demographic factors, circumstances of envenomation and prehospital intervention [SEM = standard error of mean, # = unequal time frame signify the period indicating risk time segment of the day].
| Features of envenomed snakebite cases | Number (%) |
|---|---|
| A. Socio-demographic features | |
| Age (years) of all patients [range = 2–75, median = 36, mean±SEM = 34.49±2.67] | |
| 1–17 (children) [range = 2–17, median = 15, mean±SEM = 12.88±1.83] | 8 (24) |
| 18–40 (adults) [range = 20–37, median = 29, mean±SEM = 29.12±1.62] | 16 (47) |
| 41–65 (elders) [range = 42–75, median = 50, mean±SEM = 51.73±2.24] | 15 (44) |
| Gender [sex (male and female) ratio = 1.2] | |
| Male | 21 (54) |
| Female | 18 (46) |
| Education | |
| Illiterate (unable to read and write their own name) | 20 (51) |
| Literate (able to read and write their own name) | 19 (49) |
| Occupation | |
| Farmer | 24 (62) |
| Student | 7 (18) |
| Housewife | 3 (8) |
| Security personnel | 1 (3) |
| Businessman | 1 (3) |
| Social worker | 1 (3) |
| Mason | 1 (3) |
| Clerk | 1 (3) |
| Unknown | 1 (3) |
| B. Circumstances of snakebites | |
| Time# | |
| Early morning (03:00–04:59) | 9 (23) |
| Morning (05:00–09:59) | 3 (8) |
| Day (10:00–16:59) | 3 (8) |
| Evening (17:00–19:59) | 4 (10) |
| Night (20:00–02:59) | 20 (51) |
| Months | |
| June | 10 (26) |
| August | 10 (26) |
| September | 8 (21) |
| July | 7 (18) |
| April | 2 (5) |
| May | 2 (5) |
| Bitten body parts | |
| Leg (2 patients received bite below ankle on toes and foot) | 8 (21) |
| Hand (4 patients received bite below wrist on palm and fingers) | 5 (13) |
| Head | 2 (5) |
| Head and hand | 1 (3) |
| Trunk | 1 (3) |
| Unidentified | 8 (21) |
| Not available | 8 (21) |
| Locations where bite occurred | |
| Indoor | 15 (38) |
| Premises of house (roof, yard, the outskirts of house, e.g., verandah, outer corridor, etc.) | 12 (31) |
| Crop field | 5 (13) |
| Forest | 1 (3) |
| Not available | 6 (15) |
| Districts | |
| Nawalparasi | 24 (62) |
| Chitwan | 14 (36) |
| Gorkha | 1 (3) |
| Snakes involved in bite | |
| Snakes seen after bite | 11 (28) |
| Killed and brought to hospital | 7 (18) |
| Killed snake brought | |
| Bungarus caeruleus | 6 (15) |
| Trimeresurus albolabris | 1 (3) |
| Trimeresurus albolabris (snake seen) | 2 (5) |
| Bungarus caeruleus (snake seen) | 1 (3) |
| Naja naja (not killed in fear of revenge by its partner) | 1 (3) |
| C. Pre-hospital interventions adopted | |
| a. Medical treatment sought | 6 (15) |
| 2 to 6 antivenom vials received in Kali Gandaki Hospital, Kawaswoti, Nawalparasi | 2 (5) |
| 2 antivenom vials received in Chormara Primary Healthcare Center | 1 (3) |
| Accessed in Kaligandaki Hospital, but responsible doctor for antivenom administration was absent | 1 (3) |
| Health Post in Dumkauli, Nawalparasi supplied with no antivenom | 2 (5) |
| b. Treatment seeking behaviour | |
| Consultation with Dhami/ Jhakri (local healers) | 7 (18) |
| Application of Jagmohar (Garud Dhunga) i.e., Snake Stone | 2 (5) |
| Testing of poisoning by eating chillies | 2 (5) |
| Incision of wound | 1 (3) |
| Application of paste by eroding sickle with stone | 1 (3) |
| Consultation with local healers and use of kerosene in wound | 1 (3) |
| Drinking alcohol | 1 (3) |
| Consultation with local healers, incision of wound, and ringing/deepening in potash solution | 1 (3) |
| c. Modes of transport used | |
| Ambulance | 14 (36) |
| Cycle, ambulance | 9 (23) |
| Bike | 4 (10) |
| Bus | 2 (5) |
| Bike, ambulance | 2 (5) |
| Cycle | 1 (3) |
| Van | 1 (3) |
| Truck | 1 (3) |
| Cycle, bike, ambulance | 1 (3) |
| Cycle, van | 1 (3) |
| Bike, van | 1 (3) |
| Cart, ambulance | 1 (3) |
| Cycle, cart, ambulance | 1 (3) |
To measure in-hospital observation hours to the time of first antivenom administration, we set time zero as the time of presentation at the emergency department. The antivenom administered (10ml each) was freeze-dried polyspecific enzyme refined equine immunoglobulins and manufactured by Vins Bioproducts Ltd (Andra Pradesh, India). It was used following the national protocol (Shah et al, 2003). Initially, patients received 2 vials of antivenom in 20ml. distilled water via intra-venous (i.v.) push injection over 10min. Then, 4 vials antivenom dissolved in 500ml of 5% dextrose solution (in adult, 5–10ml. fluid per kg and in children, at the rate of 3–5ml per kg body weight) were infused over 4hr interval for 8 to 12hrs. During the infusion, the patients were closely monitored every hour. If clinical signs deteriorated, they received 2 vials of antivenom via i.v. push injection and supportive treatment. After the sign and symptoms improved, the dose was tapered off to 2 vials of antivenom dissolved in 5% dextrose solution given 4 hourly for 8 to 12hrs. Then on further improvement, 2 vials of antivenom dissolved in 5% dextrose solution were given 6 hourly till symptoms of envenoming disappeared.
For the analyses of annual incidence of snakebites, envenomations, and deaths, our data covered the peak time of snakebites during April and Septemmber. In other months, there occurs rare or no snakebites. Therefore, we presented a reasonable estimate of the annual incidence. We managed data using Microsoft Excel® and calculated results using R statistical program (R version 3.1.2 (2014-10-31), The R Foundation for Statistical Computing Platform for Windows XP 2010). We interpreted the data using percent, measures of central tendency including standard deviation, standard error of mean, figures and tables. This study was approved by the Ethical Review Board of the Nepal Health Research Council.
Results
Incidence of snakebite, envenomation, and deaths
A total of 342 patients with history of snakebites from the catchment area of Bharatpur Hospital presented in the emergency department of the hospital between April and September of 2007. This amounts to an annual incidence of 28 snake-bitten patients per 100,000 people in the region. Thirty nine of these patients (11%) developed signs of envenomation resulting in an annual incidence of 3 envenomations per 100,000. In the study group 21 patients were male and 18 patients were female. Mean age of study participants was 35 years.
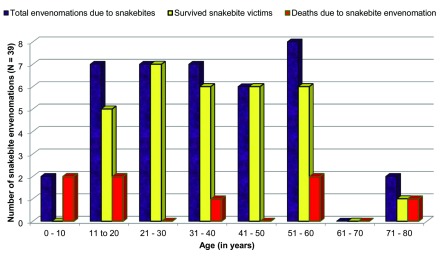
Eight of the 39 envenomed victims admitted in the hospital had a fatal outcome resulting in 21% case fatality rate and an annual incidence of snakebite deaths of one per 100,000 (Figure 1). Four of the total eight deaths (50% of deaths) and nine envenomations (23% of the total envenomations) occurred in the 0–20 year age group (Figure 2).
Figure 2.
Age distribution of the snakebite envenomated victims admitted in Bharatpur Hospital
The majority of snakebites resulting in envenomations occurred at night (51%, n=20), in the early morning (23%, n=9), and in the evening (10%, n=4) during monsoon (in June and August (26%, n=10 in each month) followed by September (21%, n=8)) (Table 2).
Out of 39 envenomed snakebite patients, 36 (92%) victims developed neurotoxicity due to elapid snakebites and three developed painful local swelling (8%) due to viperid snakebites. 11 (28%) victims had seen the offending snake after the bite. Seven (18%) of the 11 patients killed the offending snake and brought it to the hospital. Six of the snake specimens were Bungarus caeruleus, one snake specimen was Trimeresurus albolabris (Table 2). Two of six B. caeruleus caused death of victim.
A total of 69% (n=27) of the envenomation victims received some form of first aid. 54% used a single tourniquet, while 15% used a tight and/or multiple tourniquets. No victims adopted either of the WHO-recommended first aid methods (pressure immobilization bandaging or local compression pad immobilization). Sixteen patients (41%) practiced traditional healing treatments before arrival at the hospital, of these 16 victims, three victims (38%) died. Seven victims (44%) consulted local healers, two applied a “Garud Dhunga” or “Jagmohar” (snake stone), 3 consumed hot peppers or ethanol, one incised the bitten site, two used a topical paste of potash solution, and one used kerosene on the wound after consulting with local healers. Six (15%) victims sought medical treatment in the peripheral healthcare facilities. Three (8%) victims accessed a center where there was no supply of antivenom or trained medical personnel at the time of arrival (Table 2).
Antivenom use and hospitalization duration
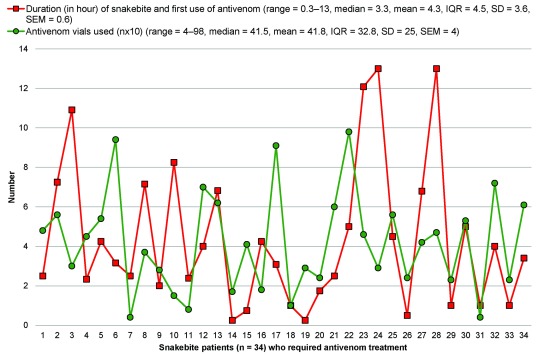
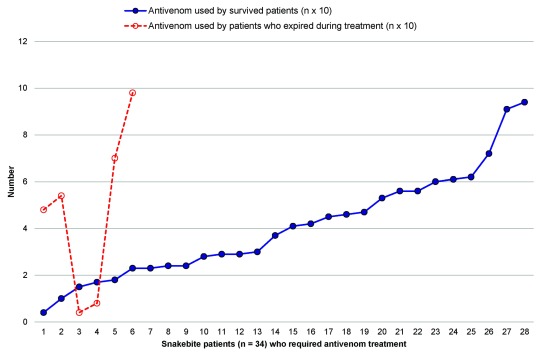
Thirty four patients received antivenom therapy. Patients arrived 4hr (h, median) after being bitten (interquartile range=5). Fourteen cases (41%) who had neurotoxic envenomation received antivenom on arrival, 29% after 0.08 to 0.5hr, 6% after 0.67hr, 12% after 1.5 to 3.5hr, and 6% each after 4.2 to 9.5hr and 11 to 12.5hr of in-hospital observation. Snakebite envenomed victims (n=34) showing neurotoxicity received a median 41.5 vials of VINS Bioproduct antivenom (Andhra Pradesh, India) (range=4–98 vials, Figure 3). Hospital stays were a median of 3.6 days. (range=0.1–6.3 days). Two confirmed Bungarus caeruleus bite victims who developed ptosis, salivation, and semi-consciousness prior to hospital presentation were treated and did not survive despite administration of 70 and 98 ASVS vials, respectively (Figure 4). A range of 60 to 98 ASVS vials were administered to those who arrived at hospital late or with full ptosis, salivation, and semi-consciousness (Figure 4).
Figure 3.
Duration of snakebite and beginning of first dose of antivenom for victims requiring antivenom treatment. IQR = inter quartile range, SD = standard deviation. We excluded two cases declared dead on hospital arrival while plotting this figure.
Figure 4.
Antivenom amount administered to patients who survived and died during treatment in Bharatpur Hospital. 1 vials = 10 ml
Discussion
Incidence of snakebite, envenomation, and deaths
Although snakebite case fatality ratio is high, the incidence of snakebite fatalities in the population inhabiting agricultural regions of southcentral Nepal is comparatively lower (Figure 1) than that reported in the southeastern Nepal. We recorded a 21% case fatality rate (CFR), which is equivalent to a CFR (21%) reported in 2000 from 10 centers in eastern Nepal (Sharma et al, 2003) or slightly greater than the CFR (17%) reported from among 46 confirmed krait bite patients studied during a PhD research in similar communities of Nepal (Pandey, 2015), but it is significantly greater than the CFR (13%) reported from 10 centers in western Nepal (Magar et al, 2013). Table 1 summarizes other prior studies of snakebite mortality from Nepal (Heap and Cowan, 1991; Hansdak et al, 1998; Shah et al, 2003; Sharma et al, 2004b; Sharma et al, 2004a; Bista et al, 2005; Pandey, 2006; Chappuis et al, 2007; Pandey, 2007; Thapa and Pandey, 2009; Pandey et al, 2010; Joshi, 2010; Paudel and Sharma, 2012; Magar et al, 2013). Similarly, the case fatality rates from various snakebite treatment centers of Asia and Africa have ranged from 0.4–54% and 0.1–28%, respectively (Chippaux, 1998). These mortality figures are underscored by a recent study in India (Westly, 2013). Our estimation of the annual incidence of one snakebite death per 100,000 populations (Figure 1) corresponds to the estimate of less than one death per 100,000 population annually during a research in southeastern to southcentral Nepal (Pandey, 2015). However, the snakebite incidence was greatly lower than that reported from eastern lowlands of Nepal (Sharma et al, 2004a). We expected prevalence of deaths due to snakebite in this region to be similar to some parts of India (i.e. six per 100,000 snakebite deaths) (Westly, 2013). Nocturnal elapid snakebites particularly krait species bites, delayed hospital admission, and poor ventilatory supports were the major causes of deaths.
The majority of snakebite envenomations (74%, n=29) which occurred during night i.e., 20:00 to 4:59 hour (Table 2) and 92% (n=34) of the total cases who developed medically significant neurotoxicity. This suggests that the majority of envenomations are due to bites of the nocturnal elapid snake (probably krait) species in this region. Previous studies support this association, as Common Kraits are most injurious during the night hours (Theakston et al, 1990; Kularatne, 2002; Bawaskar and Bawaskar, 2004; Ariaratnam et al, 2008). Approximately half of all snakebite envenomations in Nepal are due to kraits bites (Epidemiology and Disease Control Division, 2011). While our study did not specifically inquire about preventative efforts, the use of anti-mosquito bed-nets at night may prevent nocturnal krait bites (Chappuis et al, 2007), a simple cost-effective intervention which deserves to be tested in more diverse settings and adopted widely if proven to work.
Pre-hospital intervention
Snakebite victims in our study did not apply first aid methods advocated by the World Health Organization (World Health Organization, 2010). Over two-thirds of patients in this series used clinically ineffective and in some cases potentially harmful first aid measures. Recent studies in Nepal (from 10 centers in southwestern Nepal during 2008 to 2010) and Bangladesh (Chittagong Medical College between May 1999 and October 2002) each report 95% snakebite cases who applied ligatures proximal to the bite sites (Harris et al, 2010; Magar et al, 2013). We suggest that the relative lack of application of WHO recommended first aid measures, combined with an inclination of snakebite victims towards the use of tourniquets, incisions and potash solution (Table 2), offers an opportunity for educational intervention.
Our study population relies on traditional medicines and practices (Table 2) which delays definitive and likely increases snakebite mortality rates (David et al, 2012). In our population and in previous studies, many rural snakebite victims consulted traditional healers prior to seeking definitive care (56% (Pandey, 2007); 26% (Pandey et al, 2010); 22% (Sharma et al, 2004a)). This behavior transcends national boundaries. One recent study of snakebite in Bangladesh noted that 86% of the victims go to a “snake charmer” to seek initial treatment, while only three percent go to medical doctor or hospital directly after the bite (Rahman et al, 2010). Similarly, the use of traditional healing tactics prior to evidence-based clinical care (e.g. antivenom) is common in India (74% (Hati et al, 1992), 61% (Inamdar et al, 2010)), Pakistan (75% (Chandio et al, 2000)), Kenya (68% (Snow et al, 1994)), Nigeria (81% (Michael et al, 2011)). Consistent with these previous reports, the present study demonstrated that 41% of victims consulted traditional healers or attempted traditional healing methods by themselves.
In-hospital care of snakebite
An average of 3.3hr passed between snakebite and initiation of antivenom therapy in this study (Figure 3). Thirty six percent of the victims received antivenom therapy within five or more hours. Only 14% of the patient received antivenom therapy within an hour (Figure 3). A prior epidemiological study noted that 27% of patients were treated within half an hour (World Health Organization, 1987). Similar previous studies have noted low rates of patients treated within 1hr (Sharma et al, 2003; Magar et al, 2013). However, delayed access to treatment centers remains a common reason for developing ptosis or other neuro-paralysis earlier prior to definitive treatment.
The high amount of polyvalent ASVS administered to snakebite victims in this study indicates either a lower antivenom efficacy or its overuse. Two recent comprehensive studies of snakebites from 10 different centers from western and eastern Nepal described lower doses of antivenom (average vials = 16, range 2–140 vials (Sharma et al, 2003; Magar et al, 2013)). Two independent randomized control trials have showed no statistical differences between higher and lower dosage of antivenom administration in terms of mortality (Tariang et al, 1999; Paul et al, 2004). Previous studies in a similar patient populations showed 32 vials administered to each of victims (range = 6–89 vials) from hospitals in the southcentral Nepal (Pandey, 2006) which are consistent with our findings (Figure 3). Overall, these results describe very high usage of antivenom in Nepal. This overuse may be based on the possible incompatibility between Nepalese snake venom and antivenom produced against Indian snake species though this will require further study. Also, this high use of antivenom could also be associated to inappropriate storage of antivenom making it less active. It could be that when the krait venom binds to the receptors in the neuromuscular junction, the binding is irreversible rather than competitive. Therefore, giving more ASVS is futile because what is bound is not going to come off no matter what dose of ASVS is given. Giving some antivenom to “mop up” what is in the blood stream would be relevant but giving large amounts is futile.
Thirteen cases developed respiratory paralysis and needed assisted ventilation, six of which died. We suspect that the reasons for high ASVS utilization in the present study include the species of snake involved and the continuation of antivenom therapy in victims who presented late with full ptosis or coma. A recent study in northern India reports that severely envenomed victims received a higher dosage of antivenom than those mildly and moderately envenomed (Ahmed et al, 2012). The reversibility of snake venom paralysis to snake antivenom depends on several factors, including the time since bite and the specific types of neurotoxins present in an involved snake species’ venom (White et al, 2003; White, 2004). Sharma et al (2002) reported higher doses of antivenom required for krait bites. Thus, it is not surprising that our study population, which likely included a great many krait-bitten victims, often did not respond to antivenom even in high doses. We suggest that a further study of Nepalese snake venom and the effectiveness of Indian produced antivenom is indicated.
Because snake species vary by region there is no clear consensus on the appropriate time of hospital observation for snake bite victims. Ptosis, the earliest sign of neurotoxic envenomation due to elapid bites, is widely considered to be the trigger for antivenom administration (Currie, 2000; Shah et al, 2003; World Health Organization, 2010), but the features of envenomation can appear as early as 5–30 minutes or as late as 24 hours after a bite (Currie, 2000). Although majority of victims in our study received antivenom on arrival or within one hour of hospital arrival, time of bite to antivenom therapy was variable (Figure 3).
An 18-year-old woman in our population did not develop symptoms until 25.75hr after being bitten by which time she had already returned home and had to return to the hospital for antivenom therapy. Such stories are typical and are consistent with previous studies. In Nepal, snakebites are generally observed for 12hr although 24hr observation is suggested (Sharma et al, 2013), but our data suggests the need of extended in-hospital observation. We recommend further clinical studies to address the clinical timing of ptosis.
Limitations of our study
We did not have access to the complete medical records in some cases, which may have provided additional laboratory and clinical details (such as vital sign changes) to correlate with the trends we observed. There was no way to assure that the medications used (e.g., antivenom) were consistent in quality and concentration, an uncertainty which may have introduced a considerable amount of variability into the results of the study.
Conclusions
It is evident that snakebite management in southcentral Nepal is affected by nocturnal elapid snakebites, improper first aid measures and variable effectiveness, timing and amount of antivenom administration. This study indicates the need for further clinical studies to suggest the appropriate antivenom dosage and confirm snake species responsible for envenomations. It can be the premises to find out the reasons behind the unexpected use of antivenom exceeding its normal dosage and higher snakebite case fatality in Nepalese hospitals. The time laps between snakebite and onset of antivenom treatment should be reduced, which needs improvement in roads, ambulance service, and other means of transport. There is also a need for further clinical study to determine factors contributing to the wide variation in antivenom dosing. It also shows that the development of educational initiatives to address current first aid practices and the reliance on traditional medicine should be undertaken. The results can be important reference to teach people about the need of special observation hours after elapid snakebite and be basis to promote pre- and in-hospital management of snakebite.
Acknowledgments
This work was supported by America Nepal Medical Foundation (ANMF), USA [06BH001]. We are thankful to medical professionals and administrative staffs of Bharatpur Hospital for their generous supports while studying admitted snakebite cases. We are grateful to Professor Steven Seifert, Department of Emergency Medicine, University of New Mexico, USA and other anonymous reviewers for their critical review comments.
Competing Interest
None declared.
References
- Ahmed SM, Nadeem A, Islam MS, Agarwal S, Singh L. Retrospective analysis of snake victims in northern India admitted in a tertiary level institute. J Anaesthesiol Clin Pharmacol. 2012;28:45–50. doi: 10.4103/0970-9185.92434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariaratnam CA, Sheriff MHR, Theakston RDG, Warrell DA. Distinctive epidemiologic and clinical features of Common Krait (Bungarus caeruleus) bites in Sri Lanka. Am J Trop Med Hyg. 2008;79:458–462. [PubMed] [Google Scholar]
- Bawaskar HS, Bawaskar PH. Envenoming by the Common Krait (Bungarus caeruleus) and Asian Cobra (Naja naja): clinical manifestations and their management in a rural setting. Wilderness Environ Med. 2004;15:257–266. doi: 10.1580/1080-6032(2004)015[0257:ebtckb]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Bista MB, Banerjee MK, Thakur GD, Shrestha JM, Upadhyay PK, Bhandari R. Annual report 2002 and 2003. Department of Health Services, Epidemiology and Disease Control Division, Ministry of Health; Kathmandu, Nepal: 2005. Incidence of poisonous snakebite in Nepal; pp. 58–64. [Google Scholar]
- Chandio AM, Sandelo P, Rahu AA, Ahmed ST, Dahri AH, Bhatti R. Snakebite: treatment seeking behaviour among Sindh rural population. J Ayub Med Coll. 2000;12:3–5. [Google Scholar]
- Chappuis F, Sharma SK, Jha N, Loutan L, Bovier PA. Protection against snakebites by sleeping under a bed net in southeastern Nepal. Am J Trop Med Hyg. 2007;77:197–199. [PubMed] [Google Scholar]
- Chippaux JP. Snakebites: appraisal of the global situation. Bull World Health Organ. 1998;76:515–524. [PMC free article] [PubMed] [Google Scholar]
- Currie BJ. Snakebite in tropical Australia, Papua New Guinea and Irian Jaya. Emerg Med. 2000;12:285–294. [Google Scholar]
- David S, Matathia S, Christopher S. Mortality predictors of snakebite envenomation in southern India - a ten-year retrospective audit of 533 patients. J Med Toxicol. 2012;8:118–123. doi: 10.1007/s13181-011-0204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devkota UN, Steinmann JP, Shah LN. Snakebite in Nepal: a study from Siraha District. J Nepal Med Assoc. 2000;39:203–209. [Google Scholar]
- Epidemiology and Disease Control Division. EDCD second edition 2068, Department of Health Services, Epidemiology and Disease Control Division, Ministry of Health and Population, Kathmandu, Nepal, 2nd ed 2011 [Google Scholar]
- Hansdak SG, Lallar KS, Pokharel P, Shyangwa P, Karki P, Koirala S. A clinico-epidemiological study of snakebite in Nepal. Trop Doct. 1998;28:223–226. doi: 10.1177/004947559802800412. [DOI] [PubMed] [Google Scholar]
- Harris JB, Faiz MA, Rahman MR, et al. Snakebite in Chittagong Division, Bangladesh: a study of bitten patients who developed no signs of systemic envenoming. Trans R Soc Trop Med Hyg. 2010;104:320–327. doi: 10.1016/j.trstmh.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Hati AK, Mandal M, De MK, Mukherjee H, Hati RN. Epidemiology of snakebite in the district of Burdwan, West Bengal. J Indian Med Assoc. 1992;90:145–147. [PubMed] [Google Scholar]
- Heap BJ, Cowan GO. The epidemiology of snakebite presenting to British military hospital Dharan during 1989. J R Army Med Corps. 1991;137:123–125. doi: 10.1136/jramc-137-03-03. [DOI] [PubMed] [Google Scholar]
- Inamdar IF, Aswar NR, Ubaidulla M, Dalvi SD. Snakebite: admissions at a tertiary health care center in Maharashtra India. S Afr Med J. 2010;100:456–458. doi: 10.7196/samj.3865. [DOI] [PubMed] [Google Scholar]
- Joshi D. An epidemiological study of snakebite cases in children of Nepal. J Nepal Paediatr Soc. 2010;30:135–140. [Google Scholar]
- Joshi DD. An epidemiological survey of snakebite cases in Dhanusha District. J Nepal Med Assoc. 1983;21:1–11. [Google Scholar]
- Kasturiratne A, Wickremasinghe AR, de Silva N, et al. The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008;5:e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kularatne SAM. Common Krait (Bungarus caeruleus) bite in Anuradhapura. Sri Lanka: a prospective clinical study. Postgrad Med J. 2002;1996-98;78:276–280. doi: 10.1136/pmj.78.919.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magar CL, Devkota K, Gupta R, Shrestha RK, Sharma SK, Pandey DP. A hospital based epidemiological study of snakebite in Western Development Region Nepal. Toxicon. 2013;69:98–102. doi: 10.1016/j.toxicon.2013.04.002. [DOI] [PubMed] [Google Scholar]
- Michael GC, Thacher TD, Shehu MIL. The effect of pre-hospital care for venomous snakebite on outcome in Nigeria. Trans R Soc Trop Med Hyg. 2011;105:95–101. doi: 10.1016/j.trstmh.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Nepal Health Research Council, 2013. National health research priority areas, Nepal Health Research Council, Kathmandu, Nepal, Second ed [Google Scholar]
- Pandey DP. Epidemiology of snakebite based on hospital survey in Chitwan and Nawalparasi Districts Nepal. J Nepal Health Res Counc. 2006;4:51–57. doi: 10.1007/BF03160933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey DP. Epidemiology of snakebites based on field survey in Chitwan and Nawalparasi Districts Nepal. J Med Toxicol. 2007;3:164–168. doi: 10.1007/BF03160933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey DP. Venomous snakes of medical relevance in Nepal: study on species, epidemiology of snake bite and assessment of risk factors of envenoming and death, PhD thesis, Faculty of Biosciences, Goethe University, Frankfurt, Germany 2015 [Google Scholar]
- Pandey DP, Thapa CL, Hamal PK. Impact of first aid training in management of snakebite victims in Madi Valley. J Nepal Health Res Counc. 2010;8:5–9. [PubMed] [Google Scholar]
- Paudel KM, Sharma S. Study of clinico-epidemiological profile and outcome of poisonous snakebites in children. J Nepal Paediatr Soc. 2012;32:47–52. [Google Scholar]
- Paul V, Pratibha S, Prahlad KA, Earali J, Francis S, Lewis F. High-dose anti-snake venom versus low-dose anti-snake venom in the treatment of poisonous snakebites - a critical study. J Assoc Physicians India. 2004;52:14–17. [PubMed] [Google Scholar]
- Rahman R, Faiz MA, Selim S, et al. Annual incidence of snakebite in rural Bangladesh. PLoS Negl Trop Dis. 2010;4:e860. doi: 10.1371/journal.pntd.0000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleich HH, Kästle W. Amphibians and reptiles of Nepal: biology, systematics, field guide, A.R.G. Gantner Verlag Kommanditgesellschaft, Ruggell, Germany 2002 [Google Scholar]
- Shah KB, Sherstha JM, Thapa CL. Snakebite management guideline, Epidemiology and Disease Control Division, Department of Health Services, Kathmandu, Nepal, First ed 2003 [Google Scholar]
- Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, Koirala S. Impact of snakebites and determinants of fatal outcomes in southeastern Nepal. Am J Trop Med Hyg. 2004a;71:234–238. [PubMed] [Google Scholar]
- Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S. Snakebite-reappraisal of the situation in eastern Nepal. Toxicon. 2003;41:285–289. doi: 10.1016/s0041-0101(02)00289-1. [DOI] [PubMed] [Google Scholar]
- Sharma SK, Koirala S, Dahal G. Krait bite requiring high dose antivenom: a case report. Southeast Asian J Trop Med Public Health. 2002;33:170–171. [PubMed] [Google Scholar]
- Sharma SK, Koirala S, Dahal G, Sah C. Clinico-epidemiological features of snakebite: a study from eastern Nepal. Trop Doct. 2004b;34:20–22. doi: 10.1177/004947550403400108. [DOI] [PubMed] [Google Scholar]
- Sharma SK, Pandey DP, Shah KB, et al. Venomous snakes of Nepal: a photographic guide, B. P. Koirala Institute of Health Sciences, Dharan, Lalitpur, Nepal, First ed 2013 [Google Scholar]
- Shrestha BM. Outcomes of snakebite envenomation in children. J Nepal Paediatr Soc. 2011;31:192–197. [Google Scholar]
- Snow RW, Bronzan R, Roques T, Nyamawi C, Murphy S, Marsh K. The prevalence and morbidity of snakebite and treatment-seeking behaviour among a rural Kenyan population. Ann Trop Med Parasitol. 1994;88:665–671. doi: 10.1080/00034983.1994.11812919. [DOI] [PubMed] [Google Scholar]
- Tariang DD, Philip PJ, Alexander G, et al. Randomized controlled trial on the effective dose of anti-snake venom in cases of snakebite with systemic envenomation. J Assoc Physicians India. 1999;47:369–371. [PubMed] [Google Scholar]
- Thapa CL, Pandey DP. Situation of snakebite envenomation in Nepal. J Nepal Disaster Emerg Med NewsHealth. 2009;1:96–100. [Google Scholar]
- Theakston R, Phillips R, Warrell D, et al. Envenoming by the Common Krait (Bungarus caeruleus) and Sri Lankan Cobra (Naja naja naja): efficacy and complications of therapy with Haffkine antivenom. Trans R Soc Trop Med Hyg. 1990;84:301–308. doi: 10.1016/0035-9203(90)90297-r. [DOI] [PubMed] [Google Scholar]
- Westly E. One million deaths. Nature. 2013;504:22–23. doi: 10.1038/504022a. [DOI] [PubMed] [Google Scholar]
- White J. Elapid snakes. In: Dart, RC (Ed), Medical Toxicology, Lippincott Williams & Wilkins, Philadelphia, USA, pp 1566-1578 2004 [Google Scholar]
- White J, Warrell D, Eddleston M, Currie BJ, Whyte IM, Isbister GK. Clinical toxinology - Where are we now? J Toxicol Clin Toxicol. 2003;41:263–276. doi: 10.1081/clt-120021112. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2010. Guidelines for the management of snakebites, World Health Organization, New Delhi, 2nd ed [Google Scholar]
- World Health Organization Zoonotic disease control: baseline epidemiological study on snakebite treatment and management. Wkly Epidemiol Rec. 1987;42:319–320. [Google Scholar]