Abstract
Alcoholic ketoacidosis (AKA) is a cause of severe metabolic acidosis usually occurring in malnourished patients with a history of recent alcoholic binge, often on a background of alcohol dependency. AKA can be fatal due to associated electrolyte abnormalities and subsequent development of cardiac arrhythmias. This is a diagnosis that is often delayed or missed, in patients who present with a severe lactic and ketoacidosis. Here we report the case of a 64-year-old female who presented with generalized abdominal pain, nausea and shortness of breath. Blood gas analysis showed significant acidaemia with a pH of 7.10, bicarbonate of 2.9 mmol/l, and lactate of 11.7 mmol/l. Serum ketones were raised at 5.5 mmol/l. The diagnosis of AKA was suspected, and subsequent aggressive fluid resuscitation, management and monitoring were instituted. Given the early recognition of AKA and appropriate multidisciplinary team management, our patient had a good outcome and was discharged home without any complication.
INTRODUCTION
Alcoholic ketoacidosis (AKA) is a condition that presents with a significant metabolic acidosis in patients with a history of alcohol excess. The diagnosis is often delayed or missed, and this can have potentially fatal consequences. There are a variety of non-specific clinical manifestations that contribute to these diagnostic difficulties. In particular, cases of AKA can be misdiagnosed as diabetic ketoacidosis (DKA). Subsequent mismanagement can lead to increasing morbidity and mortality for patients. AKA typically presents with a severe metabolic acidosis with a raised anion gap and electrolyte abnormalities, which are treatable if recognized early and appropriate management instituted. Given the increasing epidemic of alcohol-related healthcare admissions, this is an important condition to recognize and we aim to offer guidance on how to approach similar cases for the practising clinician.
CASE REPORT
We present a 64-year-old female who presented with generalized abdominal pain, nausea, vomiting and shortness of breath. Arterial blood gas analysis showed significant acidaemia with a pH of 7.10, bicarbonate of 2.9 mmol/l and lactate of 11.7 mmol/l. Serum ketones were raised at 5.5 mmol/l. Capillary blood glucose was noted to 5.8 mmol/l. The anion gap was calculated and was elevated at 25 mmol/l.
The diagnosis of DKA was queried after initial triage. However, following senior medical review, given a recent history of drinking alcohol to excess, the diagnosis of AKA was felt more likely. Whilst a decreased conscious level may have been expected, our patient was lucid enough to report drinking one to two bottles of wine per day for the past 30 years, with a recent binge the day prior to admission.
Subsequent fluid resuscitation and monitoring were instituted. Further biochemical investigation after treatment showed a rapid decline in the level of ketones and normalization of pH.
Our patient had a multidisciplinary team (MDT) looking after her care, whilst she was an inpatient, including acute medical and gastroenterology doctors and nurses, dietitians, alcohol specialist nurse, physiotherapists and occupational therapists.
Following resuscitation, our patient had plasma electrolyte levels corrected, nutritional supplementation provided and completed an alcohol detoxification regimen. Given the early recognition of AKA and concurrent management, our patient had a good outcome. She was discharged home and has been well on follow-up appointments.
DISCUSSION
AKA can be an unrecognized cause of patients presenting with a severe metabolic acidosis, including the presence of ketones. It should be suspected in any patient who has a history of chronic alcohol dependency, malnutrition or recent episode of binge drinking [1].
Patients typically present with non-specific features including nausea, vomiting and generalized abdominal pain. Vomiting and/or diarrhoea is common and can lead to hypovolaemia and potassium depletion. Signs of shock including tachycardia and hypotension can be complicated by overlap of alcohol withdrawal [2]. Electrolyte abnormalities are common to this condition and can precipitate fatal cardiac arrhythmias [3, 4].
The severe metabolic acidosis that occurs in AKA is multifactorial (Fig. 1). First, there is the presence of ketone bodies, which are inherently acidic [5, 6]. Ketones are produced by the body for energy, in times of low glucose availability. This is more likely to occur in patients with alcohol excess due to poor oral intake and nutrition. As ethanol at high concentrations inhibits lipolysis, significant production of ketone bodies (particularly beta-hydroxybutyrate) occurs once ethanol levels fall, hence why presentation typically occurs after and not during an alcoholic binge [6]. Second, due to dehydration associated with alcohol excess, there is peripheral tissue hypoperfusion, with subsequent build-up of lactic acid [5]. Third, alcohol is metabolized by the alcohol dehydrogenase and subsequently acetaldehyde dehydrogenase to give the product acetate, which is itself acidic [5, 6]. Excess alcohol intake, as demonstrated by recent binge by our patient, therefore can lead to a significant and severe metabolic acidosis.
Figure 1:
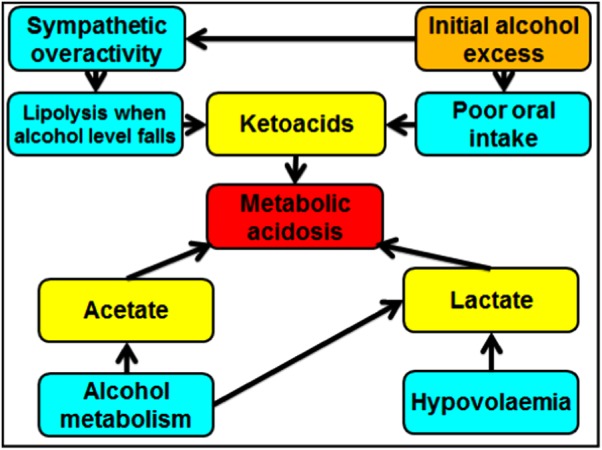
Aetiology of acidosis in AKA.
The main differential diagnoses for ketosis in our patient included AKA, starvation/fasting ketosis and DKA. In starvation ketosis, a mild ketosis is noted to develop in most after 12–24 h of fasting. However, the body copes with this physiologically by peripherally utilizing ketone bodies, stimulating increased insulin release (despite the presence of low glucose levels), and direct inhibition of further lipolysis by the ketone bodies themselves [7]. Therefore, only a mild acidosis is observed in starvation ketosis.
The key differential diagnosis to consider, and exclude, in these patients is DKA. Although DKA can also present with a severe metabolic acidosis, with a raised anion gap and the presence of ketones, the history and examination are quite distinct from that of someone presenting with AKA (Table 1).
Table 1:
Characteristics of AKA and DKA
| AKA | DKA | |
|---|---|---|
| Past medical history | Alcohol excess | Might be known diabetic or new presentation |
| Clinical presentation | Non-specific features | Non-specific features |
| Alertness | Alert and lucid usually | Variable but often decreased alertness |
| Examination | Dehydrated and clinically more well than expected | Dehydrated and clinically very unwell |
| Blood gas analysis | Metabolic acidosis with raised anion gap | Metabolic acidosis with raised anion gap |
| Blood glucose | Usually low or normal, can be modestly raised | Usually significantly raised |
| Ketones | Present on both urinary and blood testing | Present on both urinary and blood testing |
| Beta-hydroxybutyrate | Significantly raised | Mildly raised |
| Electrolyte abnormalities | Often low potassium, phosphate and magnesium | Total body potassium low (serum potassium is either low or normal) |
Although AKA can cause a modest elevation in serum glucose, significant hyperglycaemia in patients with metabolic acidosis, the presence of ketones and a suggestive history would make DKA the more likely diagnosis. The clinical importance in recognizing AKA from DKA is demonstrated by cases of patients who were treated as DKA and developed severe hypoglycaemia as a result of inappropriate insulin administration [8].
The presence of a high anion gap, although not specific, is suggestive of AKA in a patient with an appropriate clinical history [9]. Additional measurements that may help determine the diagnosis of AKA include beta-hydroxybutyrate levels (high in AKA, low in DKA) and serum alcohol concentration (typically low or undetectable) [8]. The key principle of emergency management is adequate fluid resuscitation [10]. Increasing volume status and providing increased perfusion to tissues help reduce lactic acid, ketoacids and acetic acid, which would all have been contributing to the severe acidosis.
Appropriate MDT management is key to promoting rapid recovery from AKA, but also in helping prevent complications associated with alcohol excess, in particular treating malnutrition and electrolyte deficiencies [2, 5]. Electrolyte correction should be instituted as a matter of urgency, as the main of cause of mortality is attributed to cardiac arrhythmias from electrolyte deficiencies [10].
This case demonstrates the importance of considering AKA in the differential diagnosis of a patient presenting with non-specific symptoms, significant metabolic acidosis and a history of alcohol excess. It is essential to differentiate AKA from DKA to ensure that inappropriate insulin administration does not occur. The key tenants to management of AKA include fluid resuscitation and electrolyte correction.
CONFLICT OF INTEREST
None declared.
FUNDING
None.
ETHICAL APPROVAL
Not applicable.
CONSENT
Written consent was obtained from the patient.
GUARANTOR
Nurulamin M. Noor.
REFERENCES
- 1.Wrenn KD, Slovis CM, Minion GE, Rutkowski R. The syndrome of alcoholic ketoacidosis. Am J Med 1991;91:119. [DOI] [PubMed] [Google Scholar]
- 2.Allison MG, McCurdy MT. Alcoholic metabolic emergencies. Emerg Med Clin North Am 2014;32:293–301. [DOI] [PubMed] [Google Scholar]
- 3.Palmiere C, Augsburger M. The post-mortem diagnosis of alcoholic ketoacidosis. Alcohol Alcohol 2014;49:271–281. [DOI] [PubMed] [Google Scholar]
- 4.Yanagawa Y, Sakamato T, Okada Y. Six cases of sudden cardiac arrest in alcoholic ketoacidosis. Intern Med 2008;47:113–117. [DOI] [PubMed] [Google Scholar]
- 5.Palmer JP. Alcoholic ketoacidosis: clinical and laboratory presentation, pathophysiology and treatment. Clin Endocrinol Metab 1983;12:381. [DOI] [PubMed] [Google Scholar]
- 6.Halperin ML, Hammeke M, Josse RG, Jungas RL. Metabolic acidosis in the alcoholic: a pathophysiologic approach. Metabolism 1983;32:308. [DOI] [PubMed] [Google Scholar]
- 7.Balasse EO, Féry F. Ketone body production and disposal: effects of fasting, diabetes, and exercise. Diabetes Metab Rev 1989;5:247. [DOI] [PubMed] [Google Scholar]
- 8.Matsuzaki T, Shiraishi W, Iwanaga Y, Yamamoto A. Case of alcoholic ketoacidosis accompanied by severe hypoglycemia. J UOEH 2015;37:43–47. [DOI] [PubMed] [Google Scholar]
- 9.Schelling JR, Howard RL, Winter SD, Linas SL. Increased osmolal gap in alcoholic ketoacidosis and lactic acidosis. Ann Intern Med 1990;113:580. [DOI] [PubMed] [Google Scholar]
- 10.McGuire LC, Cruickshank AM, Munro PT. Alcoholic ketoacidosis. Emerg Med J 2006;23:417–420. [DOI] [PMC free article] [PubMed] [Google Scholar]


