Abstract
Objective:
To delineate the factors contributing to overdiagnosis of idiopathic intracranial hypertension (IIH) among patients seen in one neuro-ophthalmology service at a tertiary center.
Methods:
We retrospectively reviewed new patients referred with a working diagnosis of IIH over 8 months. The Diagnosis Error Evaluation and Research taxonomy tool was applied to cases referred with a diagnosis of IIH and a discrepant final diagnosis.
Results:
Of 1,249 patients, 165 (13.2%) were referred either with a preexisting diagnosis of IIH or to rule out IIH. Of the 86/165 patients (52.1%) with a preexisting diagnosis of IIH, 34/86 (39.5%) did not have IIH. The most common diagnostic error was inaccurate ophthalmoscopic examination in headache patients. Of 34 patients misdiagnosed as having IIH, 27 (27/34 [79.4%]; 27/86 [31.4%]) had at least one lumbar puncture, 29 (29/34 [85.3%]; 29/86 [33.7%]) had a brain MRI, and 8 (8/34 [23.5%]; 8/86 [9.3%]) had a magnetic resonance/CT venogram. Twenty-six had received medical treatment, 1 had a lumbar drain, and 4 were referred for surgery. In 8 patients (8/34 [23.5%]; 8/86 [9.3%]), an alternative diagnosis requiring further evaluation was identified.
Conclusions:
Diagnostic errors resulted in overdiagnosis of IIH in 39.5% of patients referred for presumed IIH, and prompted unnecessary tests, invasive procedures, and missed diagnoses. The most common errors were inaccurate ophthalmoscopic examination in headache patients and thinking biases, reinforcing the need for rapid access to specialists with experience in diagnosing optic nerve disorders. Indeed, the high prevalence of primary benign headaches and obesity in young women often leads to costly and invasive evaluations for presumed IIH.
Idiopathic intracranial hypertension (IIH) with papilledema is a syndrome characterized by isolated elevated intracranial pressure (ICP) of unknown cause, occurring most commonly in young obese women.1 Identification of optic nerve head edema in a young woman with chronic headaches and normal brain imaging is highly suggestive of IIH.2 However, the high incidence of primary headache disorders among young women3 and the increasing prevalence of obesity4 make identification of patients who truly have IIH difficult for the care provider who cannot adequately examine the optic nerve. With growing awareness of IIH, many overweight women with isolated headache are subjected to invasive and costly tests and sometimes aggressive treatments before they are referred to neuro-ophthalmologists.2 The aim of our study was to delineate the factors contributing to diagnostic error and overdiagnosis of IIH among patients seen for presumed IIH in the neuro-ophthalmology service of a tertiary health care institution.
METHODS
Standard protocol approvals, registrations, and patient consents.
The study was approved by our institutional review board.5,6
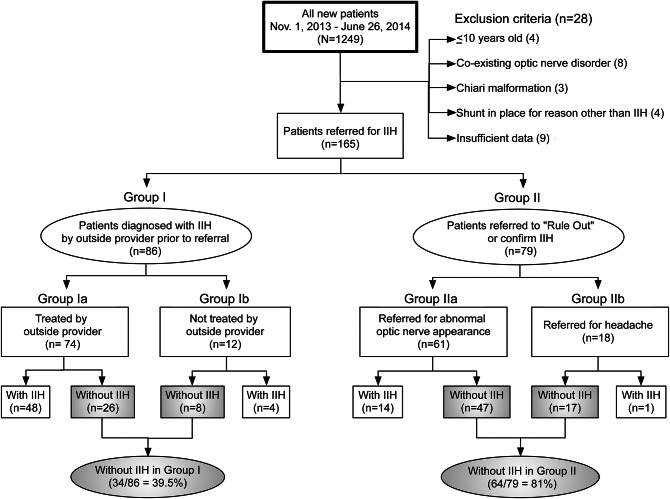
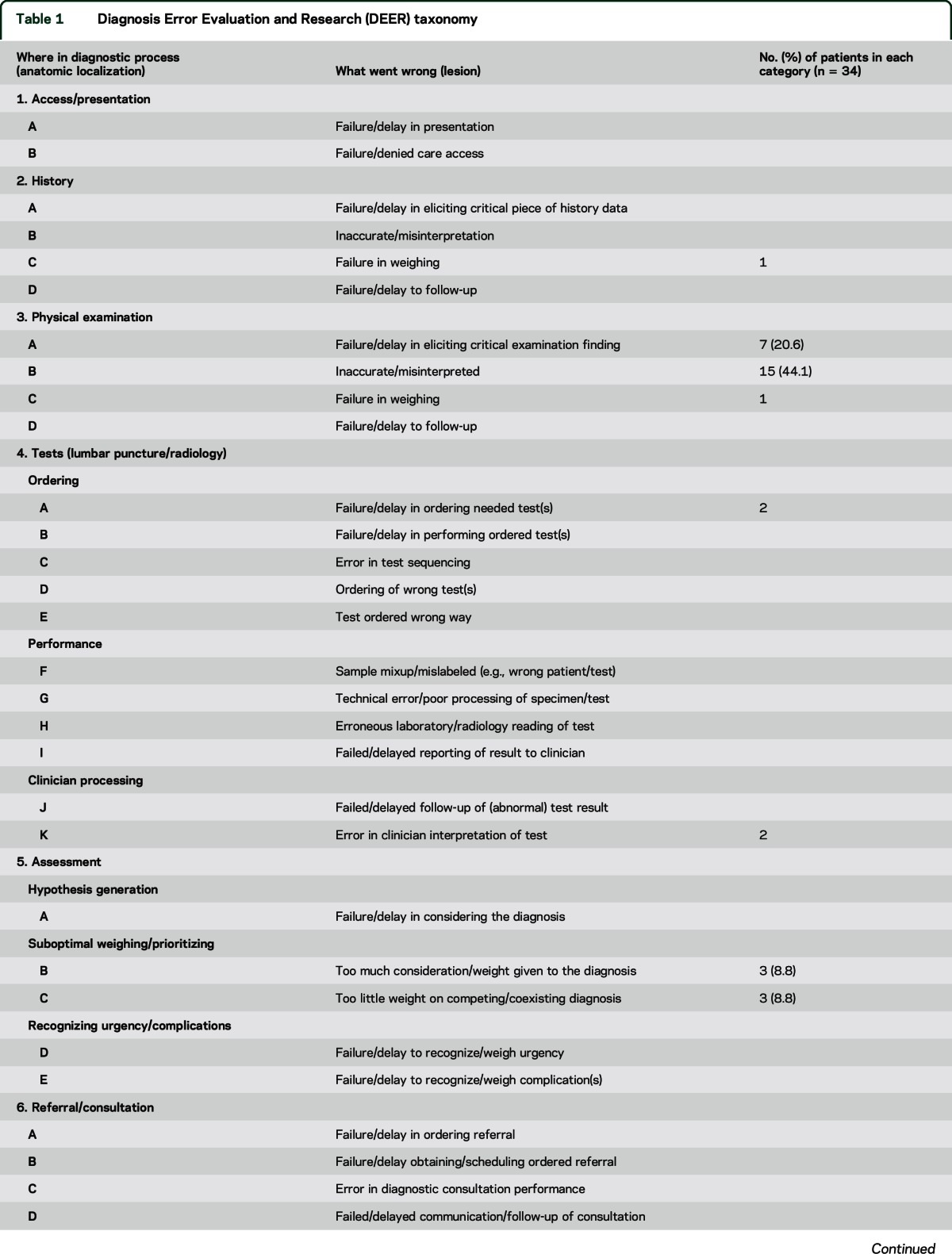
Using our appointment logs, we retrospectively reviewed all new patient encounters between November 2013 and June 2014 in one neuro-ophthalmology service of a tertiary center. We systematically reviewed all consultation letters and medical records for all new patients seen during the study period. Our goal was to identify patients referred either for management of previously diagnosed IIH by the outside provider (group I) or for evaluation of possible IIH (i.e., to rule out or to confirm IIH) (group II) (figure). Patients were excluded if they were younger than 10 years or had any condition known to cause optic nerve dysfunction, a Chiari malformation, a CSF shunting procedure for any reason besides presumed IIH, or if there was insufficient information in the outside medical records to arrive at a final diagnosis. Patients from group I, who had been diagnosed with IIH by the outside provider before referral, were further subdivided into one group that had already been treated for IIH (group Ia) and another group that had not yet been treated, but were referred to us for management (group Ib). Patients from group II, who were referred to us for evaluation of possible IIH, were further subdivided into one group that had been referred primarily because of abnormal optic nerve appearance suspicious for papilledema (group IIa) and another group that had been referred primarily because of chronic headaches presumed to be related to increased ICP (group IIb). The 4 groups are summarized in the figure. Demographic data, including age, sex, body mass index (BMI), and race, were collected. Referral data, including specialty of referring physician and number and specialties of other physicians seen prior to referral were also obtained. Initial symptoms (subjective visual loss, transient visual obscurations, diplopia, pulsatile tinnitus, headaches) were recorded. We also collected information about diagnostic testing and treatments offered. When appropriate neuroimaging was available, we recorded how many signs suggestive of chronically elevated ICP were present (including posterior globe flattening, optic nerve head protrusion, optic nerve sheath dilation, optic nerve tortuosity, empty sella, and transverse sinus stenosis). When a lumbar puncture was performed, the number of lumbar punctures and CSF opening pressures were recorded. The diagnosis of definite IIH was determined by experienced neuro-ophthalmologists (V.B., B.B.B., N.J.N.) using the updated modified Dandy criteria,7,8 including 1) symptoms and signs of generalized intracranial hypertension such as headache, papilledema, and sixth nerve palsies; 2) documented elevated ICP (≥25 cm water); 3) normal CSF composition; and 4) no evidence of hydrocephalus, mass, or structural or vascular lesion on brain MRI (specifically, no evidence of cerebral venous thrombosis). For cases referred with a diagnosis of IIH (included in group I) and a discrepant final diagnosis, we applied the Diagnosis Error Evaluation and Research (DEER) taxonomy tool (table 1)9 to classify each case according to the location and type of error in the diagnostic process. The DEER classification was assigned (by all authors) based on the major cause of diagnostic error. Additionally, we assigned primary responsibility for the diagnostic error to one of the clinicians who had evaluated the patient prior to our evaluation, based on review of outside medical records.
Figure. Diagnostic errors in idiopathic intracranial hypertension (IIH).
Table 1.
Diagnosis Error Evaluation and Research (DEER) taxonomy
RESULTS
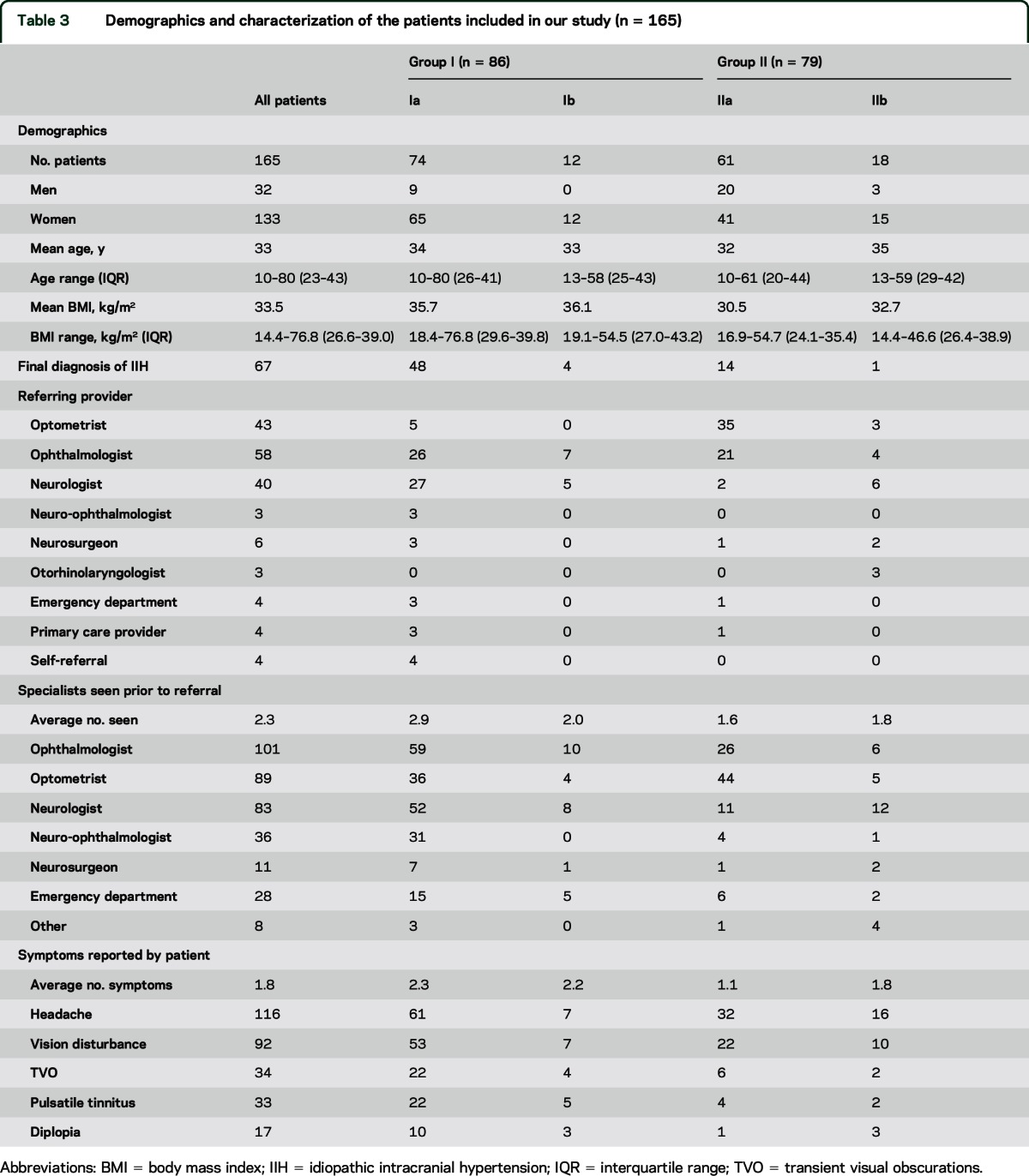
A total of 1,249 new patients were seen in our neuro-ophthalmology service during the study period. After exclusion of 28 patients, we identified 165 patients (13.2%) who had been referred either with a preexisting diagnosis of IIH (group I; n = 86 [52.1%]) or with suspected IIH (group II; n = 79 [47.9%]) (figure; table 1). Young obese women predominated (80.6%), with an average age of 33 years (range [interquartile range (IQR)] 10–80 [23–43]) and average BMI of 33.5 kg/m2 (range [IQR] 14.4–76.8 [26.6–39]). Optometrists referred 43 (26.1%) patients, ophthalmologists 58 (35.2%), and neurologists 40 (24.2%). The average number of specialists seen prior to referral to us was 2.3 (range 1–7). Prior to our evaluation, 101 (61.2%) patients had been seen by at least one ophthalmologist, 89 (54%) by at least one optometrist, 83 (50.3%) by at least one neurologist, 36 (21.8%) by outside neuro-ophthalmologists, and 11 (6.7%) by neurosurgeons, while 28 (17%) patients had been evaluated in emergency departments (ED). The average number of symptoms reported was 1.8 (range 0–5). Headaches were reported by 116 (70.3%) patients, transient visual obscurations by 34 (20.6%), pulsatile tinnitus by 33 (20%), and diplopia by 17 (10.3%).
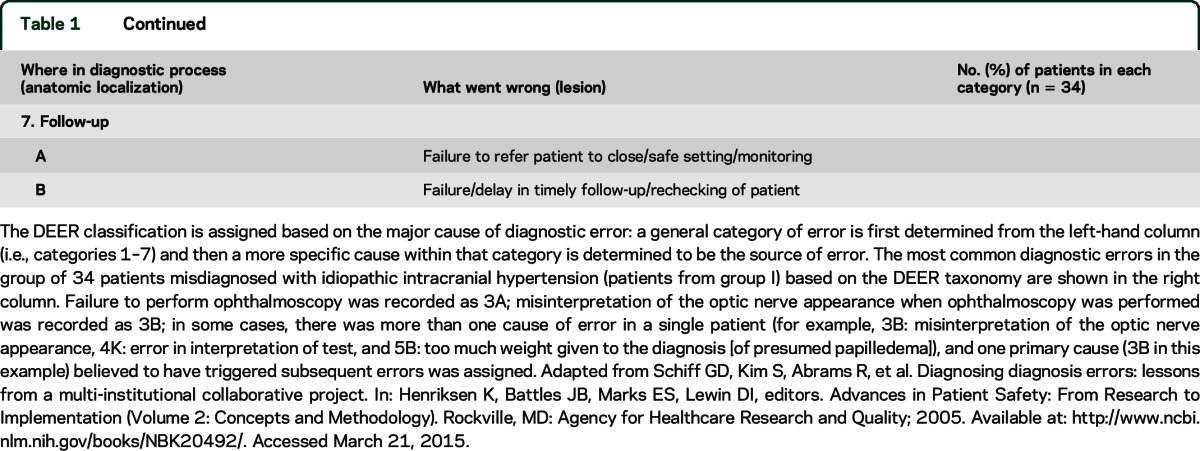
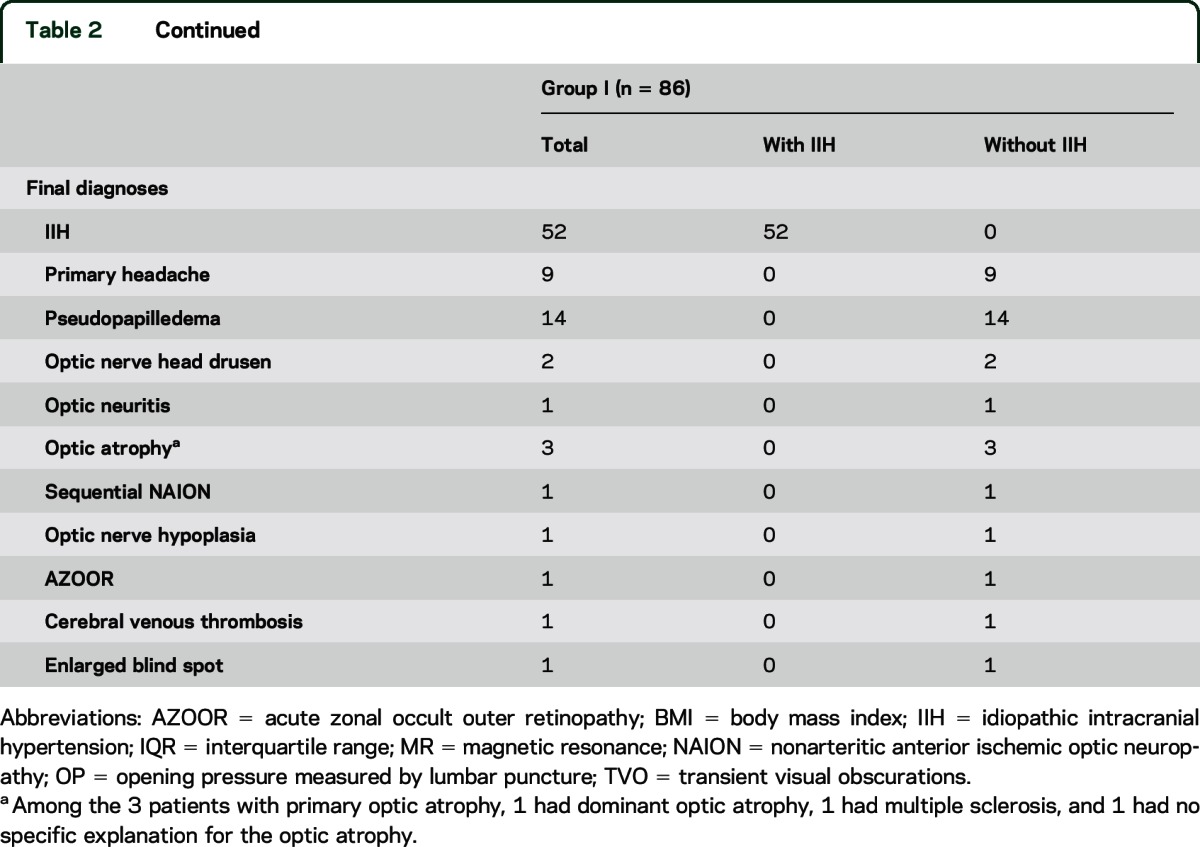
The characteristics of the 86 patients in group I referred to us with a preexisting diagnosis of IIH made by the outside provider had similar characteristics to the total group, and those are summarized in table 2. Thirty-four (39.5%) of the 86 patients referred to us with a preexisting diagnosis of IIH did not have IIH (table 2; figure). The majority of these misdiagnosed patients were women (32 [94%]), with an average age of 38 years (range [IQR] 13–80 [26–46]) and average BMI of 34.9 kg/m2 (range [IQR] 19–67 [27–39]). Optometrists referred 3 patients, ophthalmologists 11 (31.4%), and neurologists 15 (43%). The average number of specialists seen prior to referral to our neuro-ophthalmology service was 2.8 (range 1–5). Prior to our evaluation, 23 (67.6%) of the misdiagnosed patients had been seen by at least one ophthalmologist, 25 (73.5%) by at least one neurologist, 14 (41.2%) by at least one optometrist, 13 (38.2%) by an outside neuro-ophthalmologist, and 4 by neurosurgeons. Ten (29.4%) of these patients had been evaluated in EDs. The average number of symptoms for this cohort was 1.9 (range 0–4); 24 (70.6%) reported headaches, 6 (17.6%) reported transient visual obscurations, 8 (23.5%) reported pulsatile tinnitus, and 4 (11.8%) had diplopia. After evaluation at our institution, final diagnoses included primary headache disorder (9 patients), pseudopapilledema (16 patients, including 2 with optic nerve head drusen), optic atrophy (3 patients), and 1 patient each with optic neuritis, sequential nonarteritic anterior ischemic optic neuropathy, acute zonal occult outer retinopathy, physiologic blind spot, and thrombosis of the superior sagittal sinus. We ascribed the misdiagnoses primarily to an ophthalmologist in 11 (32.4%), a neurologist in 10 (29.4%), an outside neuro-ophthalmologist in 10 (29.4%), an optometrist in 2 (5.9%), and an ED physician in 1. Of these 34 patients misdiagnosed with IIH, 27 (79.4%) had 1 lumbar puncture, 10 (29.4%) had 2 to 4 lumbar punctures, 29 (85.3%) had a brain MRI, and 8 (23.5%) had magnetic resonance venogram or CT venogram. Twenty-six (76.5%) had received medical treatment for IIH, 1 had a lumbar drain, and 4 were referred for surgery. The CSF opening pressure recorded in 23 of the 34 patients who were not ultimately diagnosed with IIH ranged from 14 to 45 cm of water. The patient with a CSF opening pressure of 45 cm of water was diagnosed with cerebral venous thrombosis. The median CSF opening pressure of the other 22 patients was 25 cm of water. Only 3 of the 34 patients had radiologic signs suggestive of intracranial hypertension, including isolated dilation of the optic nerve sheaths in 1, both an empty sella and distal transverse sinus stenosis in 1, and both an empty sella and dilated optic nerve sheaths in 1; among these 3 patients, the CSF opening pressure was 18 cm of water in 1, 25 cm in 1, and was not measured in 1. None of these patients had headaches, 2 had pseudopapilledema edema, and 1 had normal-appearing optic nerves but was unusually aware of her physiologic blind spot.
Table 2.
Characterization of patients referred with a preexisting diagnosis of IIH (group I)
The DEER taxonomy tool9 was applied to each of these 34 patients misdiagnosed with IIH (table 1). It showed that that diagnostic errors resulted primarily from failure to appreciate or misinterpretation of a physical examination finding (funduscopic examination) (23/34 [67.6%]), failure to order or misinterpretation of an appropriate test (4/34 [11.8%]), errors in assessment as shown in the DEER taxonomy tool (see point 5 in table 1) (6/34 [17.6%]), and poor history (1/34 [2.9%]).
Of 79 patients referred to us with a suspicion of IIH, only 15 (19%) had IIH. All but 1 of these 79 patients had been referred because of abnormal optic nerve appearance (table 3).
Table 3.
Demographics and characterization of the patients included in our study (n = 165)
DISCUSSION
Diagnostic errors resulted in the overdiagnosis of IIH in 39.5% of patients (34/86) referred to a neuro-ophthalmology service in a tertiary health care center over a period of 8 months. This incorrect diagnosis of IIH prompted unnecessary tests in 33.7% (29/86), invasive procedures in 31.4% (27/86), and missed diagnoses that required further investigations in 9.3% (8/86).
As emphasized in the DEER classification,9 diagnostic errors can result from various mistakes along the course of a patient evaluation. In our study, most errors resulted from inability to perform an accurate physical examination (i.e., ocular fundus examination) and from the difficulty in deviating from a previously suspected diagnosis (based on the intuitive presumption that obese women with headaches must have IIH) (table 1). In a few cases, isolated radiologic findings raised a concern for IIH, or moderately elevated CSF opening pressure in the absence of papilledema or sixth nerve palsies prompted the wrong diagnosis.
Examination of the ocular fundus was often misinterpreted in obese headache patients. In our study, 20% of care providers consulted for headaches did not attempt to perform ophthalmoscopy, while 44% of those who examined the ocular fundus misinterpreted the optic nerve appearance as papilledema. These numbers are consistent with the results of the FOTO-ED I study,5,6 in which ED providers only performed ophthalmoscopy in 12% of patients presenting to an ED with a chief complaint of headaches, and also misinterpreted the ophthalmoscopy findings. Additionally, only 19% (15/79) of patients referred to us for evaluation of possible IIH (group II) were eventually diagnosed with IIH, emphasizing the difficulty for most physicians (including some neurologists and ophthalmologists in our study) to definitely diagnose or rule out IIH. Interestingly, all but one of these patients had been referred because of abnormal optic nerve appearance, reinforcing the fact that even some optometrists and ophthalmologists are not always comfortable definitively ruling out optic nerve head edema and identifying pseudopapilledema in a population of young obese women with headaches. In most situations, anomalous optic nerves were misinterpreted as papilledema, prompting extensive evaluations and inappropriate treatments. It is well-established that most non-ophthalmology trained physicians lack confidence in the use of an ophthalmoscope.10 As a result, few clinicians perform ophthalmoscopy, and many who do are unable to reliably detect abnormalities of the ocular fundus.10 Even neurologists often omit ophthalmoscopy from their clinical examination when evaluating a patient with headache.6,10 This was obvious in our study, in which some neurologists made the diagnosis of IIH and initiated treatment of IIH without any information on the optic nerve appearance. This lack of ability to reliably diagnose or rule out papilledema in headache patients is concerning. Easy and immediate access to brain imaging as well as the lack of training in ophthalmoscopy in many medical schools11,12 often leads clinicians to skip the examination of the ocular fundus when evaluating a patient with headaches.10 It is possible that one way to improve this deficiency is to encourage clinicians to use nonmydriatic retinal fundus photography.6,10,11 Indeed, papilledema (or secondary optic atrophy from previously severe chronic papilledema) should be present in order to make a diagnosis of IIH.8 So-called IIH without papilledema is a rare cause of isolated chronic headaches that is often overdiagnosed.2 Although it is true that rare patients with intracranial hypertension may develop headaches without papilledema, most patients with moderately elevated ICP and no papilledema have primary benign headaches13 that are misdiagnosed as IIH.2 As emphasized in the recently updated diagnostic criteria for IIH,8 the diagnosis of IIH cannot be made on a measurement of CSF opening pressure by a lumbar puncture alone. The cutoff of 25 cm of water in adults14 and 28 cm of water in children15 is arbitrary and what is a normal CSF opening pressure varies based on numerous factors.2,8,14,15 Indeed, wide fluctuations in the measurement of CSF opening pressure by lumbar puncture resulting from poor positioning, use of sedation, failure to relax the legs, and defective needle position are common, and further confound the accurate determination of CSF opening pressure.14,15
Numerous studies and editorials have emphasized the deficiencies in specific clinical skills of modern physicians10,16,17 and the risk of overdiagnosis and misdiagnosis related to overinvestigations and misinterpretation of ancillary tests.16–20 In their letter “Neuro-ophthalmology safer than MRI?” Sadun et al.18 emphasized that “ordering the wrong test at the wrong time is not only a waste of resources and a cause of delay to proper diagnosis, it can also lead to the wrong diagnosis path and that can be very dangerous.” “Better thinking” is indeed one of the main solutions proposed by Wachter19 to avoid diagnosis errors and overdiagnosis. Such “better thinking” involves avoiding cognitive shortcuts to try to prevent premature closure, which occurs when a clinician decides on a single diagnosis and fails to consider other diagnostic possibilities (such as deciding prematurely that a young woman with headache must have IIH because she is obese). The process of asking oneself “What else could this be?” when evaluating a patient has been termed cognitive debiasing by Croskerry21 and is an important step in establishing a diagnosis. Improved clinical skills and determination of a pretest probability for each test ordered are simple ways to avoid cognitive traps along the road of making a diagnosis and deciding on a treatment plan.18 One of the striking aspects of our results is the fact that a large majority of patients overdiagnosed with IIH were young obese women. The fact that ED providers or primary care physicians would wrongly suspect IIH in many of these patients is not surprising; however, most misdiagnoses were made by optometrists, ophthalmologists, and neurologists (some previously trained as neuro-ophthalmologists), who should be comfortable examining the optic nerve or evaluating a headache patient. Subconscious and intuitive processes led these providers to overdiagnose IIH because the patients were young obese women; this characteristic pushed the care providers into cognitive errors by the succession of fixed-action patterns.22
Diagnostic error almost universally ranks as the chief reason for malpractice claims,23 with failure or delay in diagnosing cerebrovascular disease or brain tumors ranking as the highest causes of medical malpractice litigation and indemnity dollars in neurology and ophthalmology.24,25 Increased education about the prevalence of misdiagnosis and missed diagnosis, combined with the fear of medical malpractice litigation, has caused a pendulum swing towards overtesting26,27 and overdiagnosis.
Brain imaging, particularly brain MRI, is nowadays almost systematically obtained at some point in patients with chronic headaches. Incidental finding of nonspecific anomalies such as empty sella, dilation of the optic nerve sheath, or anomalies of one or both transverse venous sinuses often leads to an overdiagnosis of IIH and resultant excessive tests, including lumbar punctures.28 In such patients, careful examination of the ocular fundus looking for evidence of papilledema should be enough to either suggest raised ICP, and therefore prompt a lumbar puncture (results of which must also be interpreted with caution), or should reassure the physician when absent.2
We acknowledge several limitations of our study, including the fact that it was retrospective. It is possible that some referring providers used the diagnosis of IIH as a billing code without being certain that the patient did indeed have IIH. We had the benefit, however, of access to medical records from the patients' previous evaluations, which were invaluable in recreating their journey through the health care system, and we excluded patients for whom there were insufficient data. We did not use billing diagnoses from referring providers as indicators of medical diagnoses. It is also possible that in some patients, the referring provider did observe disc edema, which could have resolved by the time the patient was seen in our service. However, careful review of the providers' medical records, sometimes of fundus photographs obtained at initial evaluation, combined with detailed funduscopic examination by us as well as review of our own fundus photographs made this unlikely. To our advantage was that all patients were systematically evaluated in a standardized fashion in a single neuro-ophthalmic center. We recognize that we are also potentially subject to the same cognitive biases, but each subject in the study was independently reviewed by at least another physician before making a final assessment. Additionally, there exists the possibility of referral bias to our tertiary center due to previously established referral patterns.
Our findings are important in light of the high prevalence of primary headaches3 and the growing prevalence of obesity4 in the United States, making identification of patients who truly have IIH difficult for the care provider who cannot adequately examine the optic nerve. Attempting to avoid missing the diagnosis of IIH in such individuals often leads to overdiagnosis of IIH and overutilization of health care resources, which the medical community can ill afford in the present economic milieu. In addition to improving the clinical skills of our trainees, and increasing awareness about the influence of biases and their effect on clinical reasoning, early referral to the appropriate clinical experts may be the best remedy for diagnostic error.18
Supplementary Material
GLOSSARY
- BMI
body mass index
- DEER
Diagnosis Error Evaluation and Research
- ED
emergency department
- ICP
intracranial pressure
- IIH
idiopathic intracranial hypertension
- IQR
interquartile range
Footnotes
Editorial, page 318
AUTHOR CONTRIBUTIONS
Adeniyi Fisayo: study conceptualization and design, data analysis and interpretation, drafting and revising the manuscript. Beau B. Bruce: study conceptualization and design, data analysis and interpretation, drafting and revising the manuscript. Nancy J. Newman: study conceptualization and design, data analysis and interpretation, drafting and revising the manuscript. Valerie Biousse: study conceptualization and design, data analysis and interpretation, drafting and revising the manuscript.
STUDY FUNDING
Supported in part by an unrestricted departmental grant (Department of Ophthalmology) from Research to Prevent Blindness, Inc., New York, and by NIH/NEI core grant P30-EY006360 (Department of Ophthalmology). Dr. Bruce receives research support from the NIH/NEI (K23-EY019341).
DISCLOSURE
A. Fisayo reports no disclosures relevant to the manuscript. B. Bruce is a consultant for MedImmune (data and safety monitoring board) and Bayer (medicolegal). N. Newman is a consultant for GenSight Biologics, Trius Therapeutics, and Santhera. V. Biousse is a consultant for GenSight Biologics. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Wall M. Idiopathic intracranial hypertension. Neurol Clin 2010;28:593–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ducros A, Biousse V. Headache arising from idiopathic changes in CSF pressure. Lancet Neurol 2015;14:655–668. [DOI] [PubMed] [Google Scholar]
- 3.Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies [erratum 2015;55:356]. Headache 2015;55:21–34. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thulasi P, Fraser CL, Biousse V, Wright DW, Newman NJ, Bruce BB. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology 2013;80:432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruce BB, Biousse VB, Newman NJ. Nonmydriatic ocular fundus photography in neurologic emergencies. JAMA Neurol 2015;72:455–545. [DOI] [PubMed] [Google Scholar]
- 7.Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002;59:1492–1495. [DOI] [PubMed] [Google Scholar]
- 8.Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013;81:1159–1165. [DOI] [PubMed] [Google Scholar]
- 9.Schiff GD, Kim S, Abrams R, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project. In: Henriksen K, Battles JB, Marks ES, Lewin DI, editors. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology) [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US); 2005. Available at: http://www.ncbi.nlm.nih.gov/books/NBK20492/. Accessed March 21, 2015. [Google Scholar]
- 10.Mackay DD, Garza PS, Bruce BB, Newman NJ, Biousse V. The demise of direct ophthalmoscopy: a modern clinical challenge. Neurol Clin Pract 2015;4:150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching ophthalmoscopy to medical students (the TOTeMS study). Am J Ophthalmol 2013;156:1056–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackay DD, Garza PS, Bruce BB, et al. Teaching ophthalmoscopy to medical students (TOTeMS) II: a one-year retention study. Am J Ophthalmol 2014;157:747–748. [DOI] [PubMed] [Google Scholar]
- 13.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808. [DOI] [PubMed] [Google Scholar]
- 14.Lee SC, Lueck CJ. Cerebrospinal fluid pressure in adults. J Neuroophthalmol 2014;34:278–283. [DOI] [PubMed] [Google Scholar]
- 15.Avery RA. Interpretation of lumbar puncture opening pressure measurements in children. J Neuroophthalmol 2014;34:284–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel K. Is clinical examination dead? BMJ 2013;346:f3442. [DOI] [PubMed] [Google Scholar]
- 17.Richardson B. Clinical examination is essential to reduce overdiagnosis and overtreatment. BMJ 2014;348:g2920. [DOI] [PubMed] [Google Scholar]
- 18.Sadun AA, Chu ER, Boisvert CJ. Neuro-ophthalmology safer than MRI? Ophthalmology 2013;120:879. [DOI] [PubMed] [Google Scholar]
- 19.Wachter RM. Why diagnostic errors don't get any respect: and what can be done about them. Health Aff 2010;29:1605–1610. [DOI] [PubMed] [Google Scholar]
- 20.Newman-Toker DE, Pronovost PJ. Diagnostic errors: the next frontier for patient safety. JAMA 2009;301:1060–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 2003;78:775–780. [DOI] [PubMed] [Google Scholar]
- 22.Croskerry P. From mindless to mindful practice: cognitive bias and clinical decision making. N Engl J Med 2013;368:2445–2448. [DOI] [PubMed] [Google Scholar]
- 23.Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf 2013;22:672–680. [DOI] [PubMed] [Google Scholar]
- 24.Coysh T, Breen DP. A nationwide analysis of successful litigation claims in neurological practice. JRSM Open 2014;5:2042533313518914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathew RG, Ferguson V, Hingorani M. Clinical negligence in ophthalmology: fifteen years of National Health Service litigation authority data. Ophthalmology 2013;120:859–864. [DOI] [PubMed] [Google Scholar]
- 26.Newman-Toker DE, Camargo CA, Hsieh YH, Pelletier AJ, Edlow JA. Disconnect between charted vestibular diagnoses and emergency department management decisions: a cross-sectional analysis from a nationally representative sample. Acad Emerg Med 2009;16:970–977. [DOI] [PubMed] [Google Scholar]
- 27.Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA 2005;293:2609–2617. [DOI] [PubMed] [Google Scholar]
- 28.Kelly LP, Saindane AM, Bruce BB, et al. Does bilateral transverse cerebral venous sinus stenosis exist in patients without increased intracranial pressure? Clin Neurol Neurosurg 2013;115:1215–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.