Abstract
Background
Despite lithium’s being the most effective drug for bipolar disorder and in clinical use for decades, we still know very little about its early effects relevant to its mode of action.
Methods/design
The Oxford Lithium Trial is a double-blind, randomised, placebo-controlled study of 6-week lithium treatment in participants with bipolar disorder and mood instability. Its aim is to identify early clinical, neurocognitive and biological effects. Participants (n = 40) will undergo an intensive battery of multi-modal investigations, including remote monitoring of mood, activity and physiology, as well as cognitive testing, fMRI and magnetoencephalography, together with biochemical and gene expression measurements to assess renal, inflammatory and circadian effects.
Discussion
The findings derived from this trial may be of value in predicting subsequent therapeutic response or side effects, not only relevant to the use of lithium but also providing a potential signature to help in more rapid evaluation of novel mood stabilisers. In this respect, OxLith is a step towards the development of a valid experimental medicine model for bipolar disorder.
Trial registration
ISRCTN91624955. Registered on 22 January 2015.
Keywords: Bipolar disorder, Mood instability, Lithium, Experimental medicine
Background
Bipolar disorder is a mood disorder which affects around 2 % of the population worldwide [1]. Lithium remains the only pharmacological agent primarily indicated for the treatment of bipolar disorder and has a robust evidence base for efficacy, especially in the long term [2, 3]. It also significantly reduces suicidal behaviour [4]. However, lithium treatment has serious limitations, including toxicity in overdose, many side effects and lack of efficacy in some participants [5]. New treatments are urgently needed because, despite its efficacy, many participants do not respond to or cannot tolerate lithium, or have to stop the drug due to toxicity. Moreover, the depressive episodes of bipolar disorder are difficult to treat [6] and are often prolonged, and, even when not meeting criteria for a depressive or manic episode, participants often have residual mood instability, cognitive difficulties and other complaints [7]. Despite the widespread use of lithium in bipolar disorder for over 50 years, we still know little about its mechanism of action or about the early predictors of therapeutic response. Such information would be of value, both for optimising the clinical utility of lithium and in providing potential early markers of efficacy which could be targeted in investigations of novel candidate mood stabilisers. At present, such investigations require lengthy clinical trials which are expensive and therefore risky [8, 9]. For example, the researchers in the BALANCE trial, comparing lithium, divalproex and combination lithium plus divalproex in the prevention of relapse in bipolar disorder, followed participants for up to 2 years after randomisation, starting in 2000 and reported in 2010 [10]. The field badly needs more proximal, early or intermediate outcomes that can be used reliably in early-phase trials to provide initial evidence of efficacy. Together, the absence of validated targets and the consequent difficulties of conducting clinical development programmes contribute to the dearth of therapeutic innovation in this field.
Further, as more has been discovered about the typical course of bipolar disorder, it has become clear that the definition of bipolar disorder as an episodic condition in which depression and mania are interspersed with normal mood (and its implication of normal functioning) is over-simplistic and potentially misleading [11]. More commonly, people with bipolar disorder experience prominent inter-episodic sub-syndromal mood symptoms [12, 13]. Indeed, there is increasing evidence that chronic mood instability, which persists between clinically significant mood episodes, is an important component of the clinical picture [12]. Self-reported mood instability is a risk factor for the emergence of bipolar disorder [14] and often is a disabling feature for people with bipolar disorder, particularly in those of young age or at the beginning of their illness [15]. Reactivity of mood to external events is also greater in bipolar disorder compared with other mood disorders [16]. We have demonstrated the realities of mood instability in participants, and how it can be captured longitudinally at scale and over long periods of time, using a mood-monitoring system called True Colours (https://oxfordhealth.truecolours.nhs.uk/www/en/), [17]; other groups also have provided similar evidence [18, 19]. The Oxford Lithium Trial (OxLith) will take place within our ongoing programme of research, the Collaborative Network for Bipolar Research to Improve Outcomes (CONBRIO), in which we are exploring the nature and significance of mood instability.
On the basis of these data and considerations, we hypothesise that persistent mood instability is a risk factor for clinically significant mood episodes and that better mood stabilisation may improve outcomes. If true, and if robust markers of mood instability can be identified, this raises the possibility that measuring a change in mood stability in response to lithium over a short period such as a few weeks could predict long-term therapeutic efficacy). In turn, this would be a major contribution to the development of an experimental medicine model allowing more rapid and efficient early-phase testing of novel treatments, helping to overcome the current impasse. A precedent is provided by the Oxford Emotional Test Battery (ETB) [20], which facilitates early detection of (and gives a cognitive model for) anti-depressant efficacy. The ETB is a set of emotion-related paradigms that have been shown to be sensitive to the acute effects of anti-depressants and is now in use in development programs for novel anti-depressant drugs. Importantly, the ETB works in healthy subjects as well as in participants with depression, enhancing its utility such that, if our hypothesis is correct, novel bipolar disorder treatments could also be tested in non-clinical populations selected for high mood instability.
We have designed OxLith, an innovative randomised controlled trial, to investigate the effects of lithium on mood stability and on a wide range of cognitive, neural and physiological indices. OxLith will take place within CONBRIO, a research programme funded by the Wellcome Trust, which is seeking to (1) determine the nature and significance of mood instability, its physiological correlates, and the factors influencing it; (2) find novel ways to measure mood stability in routine clinical practice using a range of measures and devices; (3) apply mathematically sophisticated methods for data analysis and interpretation; and (4) develop an experimental medicine model for mood stabilisation and bipolar disorder.
Methods/design
The schedule for the OxLith trial is displayed in Fig. 1.
Fig. 1.
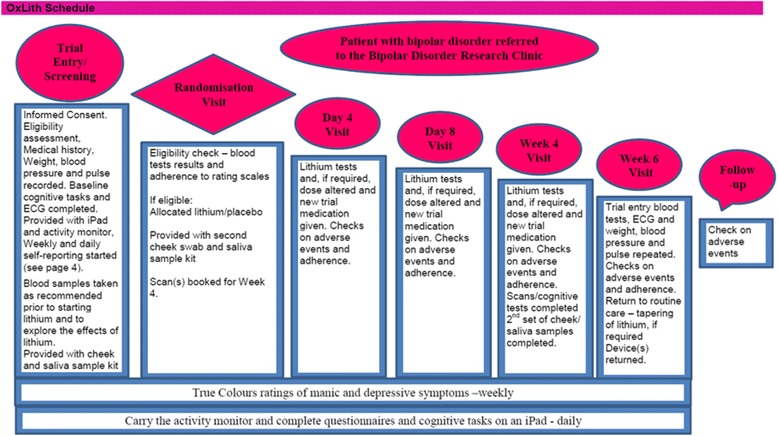
OxLith trial schedule. ECG electrocardiogram
Study objectives
The study objectives are as follows:
To compare the effects of lithium and placebo on mood instability
To measure the cognitive effects of lithium and to look for correlations with current mood state
To explore the effects of lithium on the variability in neural dynamics during magnetoencephalography (MEG) and functional magnetic resonance imaging (fMRI) scans
To explore the effects of lithium on physical activity and sleep
To explore the short-term effects of lithium on gene expression; circadian hormones; and thyroid, parathyroid and renal function
Study design
The trial is designed as a single-centre, prospective, randomised, double-blind, placebo-controlled trial. Eligible participants will be randomised in a 1:1 allocation to lithium or placebo. The randomisation algorithm will minimise separately on two variables age (<25 and ≥25 years) and sex (male, female) which are related to prognosis. Routine psychiatric follow-up with be arranged outside the trial as required. Participants will be randomised following a 2-week run-in period and take the study drug for 6 weeks.
Ethics
Written consent will be obtained from all participants. The consent form will include agreement for the results of any blood tests performed before consent to be used as baseline measures for the trial, negating the need for additional venepuncture. The study protocol was approved on 14 April 2015 by the National Research Ethics Service Committee South Central – Oxford A (reference number 15/SC/0109) and on 10 July 2015 by Oxford Health NHS Foundation Trust.
Participants and recruitment
Participants will be recruited from the bipolar disorders research clinic in Oxford. All participants will have a diagnosis of bipolar disorder (I, II or not otherwise specified) based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria and will report clinically significant mood instability. In addition, they will be individuals for whom there is uncertainty about the benefits of lithium (for example, for an individual who has recently been diagnosed or has had relatively few major mood episodes). Participants will be aged 18 years or older; will have pre-treatment renal, cardiac, thyroid and parathyroid function acceptable for the initiation of lithium; and will be willing and able to consent to participate in the trial. Exclusion criteria include any contraindication to taking lithium, concomitant psychotropic medication which cannot be withdrawn, clinically significant substance abuse, the need for treatment of an acute mood episode where placebo would be unethical, pregnancy or being of childbearing age not using effective contraception, and current suicidal ideation.
Interventions
The interventions are placebo or lithium carbonate 200-mg prolonged release tablets are to be taken orally at night and titrated to target serum level of 0.7 mmol/L. This dosing is consistent with routine practice.
Measures
Primary outcome
The primary outcome will be mood severity and stability over the 6-week randomised period as measured using a quick inventory of depressive symptoms (16-item Quick Inventory of Depressive Symptoms–Self-Rated), the Altman Self-Rating Mania Scale and daily mood measures recorded using the short form of the Positive and Negative Affect Schedule (PANAS).
Secondary outcomes
Cognition and neural dynamics
Cognitive task performance and neural dynamics will be measured to identify the effects of lithium on physiological variability and to explore the relationship between this variability and the experience of mood instability. The outcome measures will be (1) cognitive task performance for decision making, implicit and explicit reinforcement learning (completed daily using a smart device) in relation to variability in daily measures of mood (PANAS), and (2) the results of two brain scans, one using MEG and the other fMRI. Both will include scans during resting state and whilst performing a decision-making task similar to one of the daily outcomes. Scans will be performed between 3 and 4 weeks post-randomisation when the lithium level has reached a steady state.
Sleep and motor activation
Participants will wear an ActiGraph monitor (ActiGraph, Pensacola, FL, USA) for the duration of the study. This will allow us to monitor daytime activity and sleep patterns.
Circadian system
We will monitor circadian gene expression (including BMALL , PER 1 and PER 2) and genes targeted by lithium (e.g., GSK3, IMP and GAD L1) collected from the cheek. Circadian controlled hormones (cortisol and melatonin) will also be collected from saliva to explore the relationship between the circadian system, mood stability and lithium. Gene expression, melatonin and cortisol levels will all be measured every 4 h over two separate 32-h periods, one prior to randomisation and the other between weeks 3 and 4 post-randomisation.
Physiological effects of lithium
Blood samples will be collected pre-randomisation and at the end of the randomised phase to explore changes in a number of known biomarkers related to thyroid (thyroid-stimulating hormone, thyroid antibodies, triiodothyronine and free thyroxine), parathyroid (parathyroid hormone, calcium and vitamin D) and renal function (urea, creatinine, potassium, glomerular filtration rate, neutrophil gelatinase-associated lipocalin and cystatin C). Blood samples will also be used to explore lithium-associated changes in intracellular protein composition and structure.
Power analysis and sample size
The target sample size is 40 participants (20 of whom will be allocated to treatment with lithium and 20 to placebo). This sample size will give more than 90 % power to detect differences between groups on the main mood outcomes at a significance level of 0.5 %. Pragmatically, this sample size is achievable.
Blinding
All trial psychiatrists and participants will be blinded. For those participants taking placebo, sham lithium level results will be presented to the trial psychiatrist by an unblinded researcher. The sham results will be based upon information about reported adherence, time since most recent dose, and adverse events. At or just before the 6-week visit, the unblinded researcher will reveal the participant’s allocated treatment to enable the participant and psychiatrist to discuss treatment options. In the event of a medical emergency, routine care for a patient who may have been taking lithium and has symptoms consistent with lithium toxicity would be to obtain a lithium level immediately, thus negating the need for the treating doctor to be informed about the trial allocation.
Statistical analysis plan
Multiple pre- and post-randomisation mood measurements will be used in an analysis of covariance model to compare lithium with placebo. Methods from the fMRIB Statistical Library (FSL) will be used to analyse fMRI data. The FSL is a software library containing image analysis and statistical tools for functional, structural and diffusion magnetic resonance imaging brain data. MEG data will be analysed using a generalised linear model (GLM) and analysis of variance. The GLM method is a standard non-linear beam former used to determine the time course of neuronal activation for each point in a predefined source space. Actigraphy data will be correlated with mood and cognitive data.
In addition to these more traditional approaches to analysis, we will apply linear and non-linear time series methods and other advanced mathematical approaches, including machine learning. These techniques can produce binary or multi-level classifications as well as point and density forecasts to quantify confidence intervals. We will also apply the mathematical theory of rough paths [21], providing a method to reduce datasets from complex non-linear systems subjected to rapidly fluctuating stimuli to their critical information, facilitating classification and prediction.
Dissemination
Regardless of the magnitude or direction of effect, the main findings of the trial will be compiled and published in an appropriate journal and made available to participants.
Discussion
OxLith has two main goals. The first is to better characterise the early effects and mechanism of action of lithium, together with its tolerability profile, compared with placebo. The second is to establish whether mood instability, of a higher frequency than clinical episodes of depression or mania, is sensitive to lithium. The exploratory design of OxLith is intended to provide a paradigm and generate new experimental medicine outcomes and methods which can be used to expedite the development of new medicines for bipolar disorder. Drugs such as ebselen which have effects similar to those of lithium in vitro and in available mouse models of bipolar disorder are likely early candidates for such approaches.
Trial status
Recruitment has started. The duration of the study is 3 years.
Acknowledgements
CONBRIO is funded by a Wellcome Trust Strategic Award (102616).
Abbreviations
- CONBRIO
Collaborative Network for Bipolar Research to Improve Outcomes
- ECG
E lectrocardiogram
- ETB
Oxford Emotional Test Battery
- fMRI
F unctional magnetic resonance imaging
- FSL
fMRIB Statistical Library
- GLM
G eneralised linear model
- MEG
M agnetoencephalography
- OxLith
Oxford Lithium Trial
- PANAS
Positive and Negative Affect Schedule
Footnotes
Competing interests
GMG holds shares in P1vital and has served as consultant, advisor or CME speaker for AstraZeneca, AbbVie, Cephalon/Teva, Convergence Pharmaceuticals, Eli Lilly, GlaxoSmithKline, Lundbeck, Medscape, Merck, Otsuka, P1vital, Servier, Sunovion Pharmaceuticals and Takeda Pharmaceutical Co. CJH has received consultancy fees from Lundbeck, P1vital, AstraZeneca and Servier. CJH is a company director of Oxford Psychologists Ltd and holds shares in the same company. CJH has received grant funding from UCB, Johnson & Johnson, AstraZeneca, Lundbeck and Sunovion. GC has filed a patent entitled ‘Treatment of bipolar disorder’ (WO/2012/107735 A2). KEAS, AC, SRV, JR, NN, MJA, ACB, ACN, PJH and JRG declare that they have no competing interests.
Authors’ contributions
Trial design: JRG, PJH, CJH, ACN, SRV, GC, AC and GMG. Trial implementation: JR, MJA, AC, KEAS, ACB, NN, JRG, PJH, ACN, CJH, SRV and GC. Manuscript preparation: KEAS, PJH, JRG, CJH, ACN, NN, MJA and JR. All authors read and approved the final manuscript.
Contributor Information
Kate E. A. Saunders, Email: kate.saunders@psych.ox.ac.uk
Andrea Cipriani, Email: andrea.cipriani@psych.ox.ac.uk.
Jennifer Rendell, Email: jennifer.rendell@psych.ox.ac.uk.
Mary-Jane Attenburrow, Email: mary-jane.attenburrow@psych.ox.ac.uk.
Natalie Nelissen, Email: natalie.nelissen@psych.ox.ac.uk.
Amy C. Bilderbeck, Email: amy.bilderbeck@psych.ox.ac.uk
Sridhar R. Vasudevan, Email: sridhar.vasudevan@psych.ox.ac.uk
Grant Churchill, Email: grant.churchill@psych.ox.ac.uk.
Guy M. Goodwin, Email: guy.goodwin@psych.ox.ac.uk
Anna C. Nobre, Email: kia.nobre@psy.ox.ac.uk
Catherine J. Harmer, Email: catherine.harmer@psych.ox.ac.uk
Paul J. Harrison, Email: paul.harrison@psych.ox.ac.uk
John R. Geddes, Email: john.geddes@psych.ox.ac.uk
References
- 1.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64(5):543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miura T, Noma H, Furukawa TA, Mitsuyasu H, Tanaka S, Stockton S, et al. Comparative efficacy and tolerability of pharmacological treatments in the maintenance treatment of bipolar disorder: a systematic review and network meta-analysis. Lancet Psychiatry. 2014;1(5):351–9. doi: 10.1016/S2215-0366(14)70314-1. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence . Bipolar disorder: the assessment and management of bipolar disorder in adults, children and young people in primary and secondary care. Clinical guideline 185. London: National Institute for Health and Care Excellence; 2014. [Google Scholar]
- 4.Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ. 2013;346:f3646. doi: 10.1136/bmj.f3646. [DOI] [PubMed] [Google Scholar]
- 5.McKnight RF, Adida M, Budge K, Stockton S, Goodwin GM, Geddes JR. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721–8. doi: 10.1016/S0140-6736(11)61516-X. [DOI] [PubMed] [Google Scholar]
- 6.Saunders KEA, Goodwin GM. The course of bipolar disorder. Adv Psychiatr Treat. 2010;16:318–28. doi: 10.1192/apt.bp.107.004903. [DOI] [Google Scholar]
- 7.Bourne C, Aydemir Ö, Balanzá-Martínez V, Bora E, Brissos S, Cavanagh JT, et al. Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: an individual patient data meta-analysis. Acta Psychiatr Scand. 2013;128(3):149–62. doi: 10.1111/acps.12133. [DOI] [PubMed] [Google Scholar]
- 8.Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet. 2013;381(9878):1672–82. doi: 10.1016/S0140-6736(13)60857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malhi GS, Geddes JR. Carving bipolarity using a lithium sword. Br J Psychiatry. 2014;205(5):337–9. doi: 10.1192/bjp.bp.114.148072. [DOI] [PubMed] [Google Scholar]
- 10.BALANCE investigators and collaborators. Geddes JR, Goodwin GM, Rendell J, Azorin JM, Cipriani A, et al. Lithium plus valproate combination therapy versus monotherapy for relapse prevention in bipolar I disorder (BALANCE): a randomised open-label trial. Lancet. 2010;375(9712):385–95. doi: 10.1016/S0140-6736(09)61828-6. [DOI] [PubMed] [Google Scholar]
- 11.Broome MR, Saunders KE, Harrison PJ, Marwaha S. Mood instability: significance, definition and measurement. Br J Psychiatry. 2015;207(4):283–5. doi: 10.1192/bjp.bp.114.158543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. 2003;60(3):261–9. doi: 10.1001/archpsyc.60.3.261. [DOI] [PubMed] [Google Scholar]
- 13.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59(6):530–7. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 14.Howes OD, Lim S, Theologos G, Yung AR, Goodwin GM, McGuire P. A comprehensive review and model of putative prodromal features of bipolar affective disorder. Psychol Med. 2011;41(8):1567–77. doi: 10.1017/S0033291710001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bopp JM, Miklowitz DJ, Goodwin GM, Stevens W, Rendell JM, Geddes JR. The longitudinal course of bipolar disorder as revealed through weekly text messaging: a feasibility study. Bipolar Disord. 2010;12(3):327–34. doi: 10.1111/j.1399-5618.2010.00807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benazzi F. Characteristics of bipolar II patients with interpersonal rejection sensitivity. Psychiatry Clin Neurosci. 2000;54(4):499–501. doi: 10.1046/j.1440-1819.2000.00742.x. [DOI] [PubMed] [Google Scholar]
- 17.Bonsall MB, Wallace-Hadrill SM, Geddes JR, Goodwin GM, Holmes EA. Nonlinear time-series approaches in characterizing mood stability and mood instability in bipolar disorder. Proc Biol Sci. 2012;279(1730):916–24. doi: 10.1098/rspb.2011.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reich DB, Zanarini MC, Fitzmaurice G. Affective lability in bipolar disorder and borderline personality disorder. Compr Psychiatry. 2012;53(3):230–7. doi: 10.1016/j.comppsych.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 19.MacKinnon DF, Zandi PP, Gershon E, Nurnberger JI, Jr, Reich T, DePaulo JR. Rapid switching of mood in families with multiple cases of bipolar disorder. Arch Gen Psychiatry. 2003;60(9):921–8. doi: 10.1001/archpsyc.60.9.921. [DOI] [PubMed] [Google Scholar]
- 20.Harmer CJ, Goodwin GM, Cowen PJ. Why do antidepressants take so long to work? A cognitive neuropsychological model of antidepressant drug action. Br J Psychiatry. 2009;195(2):102–8. doi: 10.1192/bjp.bp.108.051193. [DOI] [PubMed] [Google Scholar]
- 21.Lyons T. Differential equations driven by rough signals. Rev Matematica Iberoamericana. 1988;14:215–310. [Google Scholar]


