Abstract
Background:
Kangaroo mother care (KMC) is the most implementation intervention in caring of the infants, as in this method, both the mothers and infants are cared. The World Health Organization recommends implementation of KMC for all infants. However, there are some barriers in the way of its application. The purpose of this study was evaluation of the practical application of KMC and nurses’ perspective about its implantation barriers in the neonatal intensive care units (NICUs) in Iran.
Materials and Methods:
The descriptive study was conducted on 96 infants and 80 nurses working in the NICUs of two university hospitals in Isfahan, Iran. Data were collected by a two-section questionnaire and analyzed by t-test through SPSS 14.
Results:
Study findings indicated that mean weight and age of the infants with KMC were 1510 g and 32 weeks, respectively. KMC was implantation for 32 min in a day. From nurses’ perspective, mother-related barriers were the main barriers in the implantation of KMC as mothers were not present by their infants. Another barrier was the mothers’ fear of touching their infants. In the domain of organizational barriers, physician's order was found to be the most important barrier in application of KMC.
Conclusions:
Identifying barriers in implantation of KMC is essential to support the mothers. Regarding mother-related barriers, organizational barriers, and the need for a physician's order for implementation of KMC, policy makers must provide facilities and equipment for applying KMC practice for mothers and improve the protocol of KMC in the NICU.
Keywords: Barriers, infants, Iran, kangaroo mother care, neonatal intensive care units, nurses, nurses’ perspective, premature
INTRODUCTION
A high number of patients hospitalized in neonatal intensive care units (NICUs) are premature infants.[1] Care of such infants imposes a high burden to public health systems as many of them have to be hospitalized in NICU.[2] One of the interventional strategies used for them is kangaroo mother care (KMC) that, based on family-centered approach, has been suggested to promote mother's role.[3] In this mode of care, necked infant is placed on mother's breasts.[4] Numerous studies have recommended the application of KMC. This method is notably effective on reduction of fetal mortality, speeding up weight gain, increasing sleep hours, and stabilization of infants’ physiological indexes[5,6,7] and, consequently, leads to increase of mothers’ self-confidence and establishment of a more powerful mother–infant emotional bond.[8] Overall, all studies have recommended application of KMC as an efficient care for all infants, especially premature infants.
In recent years, this type of care has been noticed by infants’ health and breast-feeding office of the Ministry of Health, Treatment and Medical Education in Iran, and several workshops and conferences have been conducted to familiarize the personnel with this method.
A package of KMC and related equipment has been prepared to facilitate and improve its application and make this method as a routine treatment for all infants.
What is important in KMC is immediate skin touch after birth and stabilization of infants’ hemodynamic condition, and then, its continuation at least several times a day with least length of 1 h. In this direction, various countries investigated application of KMC method concerning the time of initiation, length, and the number of times of its application daily. For instance, Blomqvist et al. in Sweden showed that infants with a body weight of 516–4500 g receive an average of KMC with a mean of 2.25 times a day and a length of 135 min 3 days after birth.[9] On the other hand, some studies showed some barriers in application of KMC, such as lack of privacy and inadequate space for mothers’ accommodation,[10] and the difficulty in educating mothers to practice KMC,[11] which result in fewer KMC applications. There is limited research on the level of application and application barriers of KMC in the world and it is believed that any care is influenced by socio-cultural and religious status of a country and its facilities; therefore, application of KMC in Iran should be considered with respect to culture, facilities, and the number of personnel in NICUs. As nurses play a vital role in caring the infants and helping mothers to make relationship with their infants and are the most basic members of treatment team, they have a key role in KMC application program. Investigation of their approach to detect the barriers of KMC and its more efficient application and promotion is important; therefore, the present study aimed to evaluate the implementation of KMC and nurses’ perspective about its application barriers in NICUs in Iran.
MATERIALS AND METHODS
With regard to the first stage of the study to investigate the level of KMC, 96 infants were selected by convenient sampling from the infants hospitalized in NICUs of university hospitals in Isfahan from May to September 2014. As application of KMC in the above-mentioned wards currently depends on a physician's written order, the inclusion criterion was having a written order for such a care. After selection of the infants, the researcher investigated the number and length of KMC in 24 h by a checklist daily until the infants’ discharge. The infants with the following conditions were not entered into the study: Unstable oxygen during 24 h, infant's critical condition in the past 24 h, intracranial hemorrhage of grade 3 and over, a naval chest tube catheter connected to the infant, existence of mental and psychological problems such as depression in mothers diagnosed by a physician, as well as their physical problems needing hospitalization.
With regard to the second stage of the study to investigate nurses’ approach concerning the barriers for KMC, 80 questionnaires were given to all nurses meeting the inclusion criteria and working in NICUs of Al-Zahra and Shahid Beheshti hospitals, and were collected after completion. Nurses’ inclusion criteria were having a bachelor's degree, having at least 6 months of work experience in NICU, being familiar with KMC and experiencing its application. Data collection tool was a checklist containing infants’ background information (infants’ age, cause of hospitalization, birth weight, and gestational age at birth, infants’ age at the time of KMC application), the length of KMC in each session, and the number of its application. The data were collected by the researcher. In the present study, KMC refers to skin-to-skin touch between mothers’ and infants’ chests. The data collection tool in the second stage of research was a two-section questionnaire. The first section included demographic characteristics such as age, sex, work experience in NICU, location of service, education degree, and working shift. The second section contained 26 questions on mothers’ barrier domain (questions 1–6), institutional barriers (questions 1–24), and educational barriers (questions 25–29). The items were answered with a five-point Likert's scale (never, seldom, sometimes, often, always). Option of “always” showed that from the nurses’ perspective, the item was always a barrier for KMC. To investigate the content validity of the tool, after extraction of the items from valid sources, a 29-item questionnaire of KMC application barriers was designed.
The questionnaire was handed to 10 academic members in the nursing and midwifery school of Isfahan University of Medical Sciences as well as the staff working in NICUs to indicate their modifications concerning its appropriateness, and it was confirmed after modifications were made based on their indications.
For reliability and internal consistency, the questionnaire was completed by 10 nurses and the Cronbach alpha was calculated to be 0.95. The answers were scored in a five-point Likert's scale of never to always (0–4) with the highest score of 100 and the lowest of zero. The collected data were analyzed by paired t-test in SPSS 14. P < 0.05 was considered significant.
Ethical considerations
Ethical considerations were confirmed by Ethic Committee of Isfahan University of Medical Sciences for their cooperation and permission to perform the study in the educational hospital of the university.
RESULTS
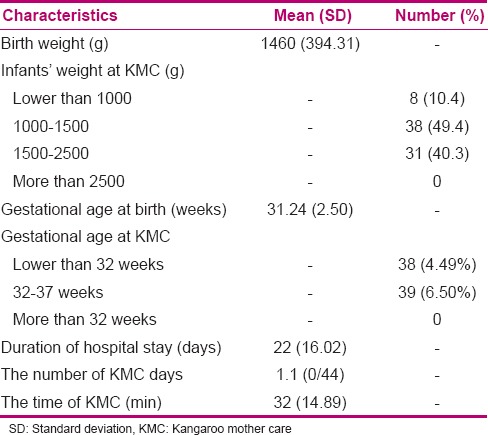
The findings showed that the infants had a mean birth weight of 1510 g and gestational age of 32.2 weeks at birth, the number of KMC application was between 0 and 3 times, and the KMC length was 15–180 min. Mean daily number of KMC application was once with a length of 32 min. Infants’ background variables have been presented in Table 1.
Table 1.
Background variables of the newborns
The subjects who were studied to determine the KMC application barriers from nurses’ perspectives had a mean (SD) age of 32.92 (5.6) years, mean total work experience of 4.9 (9) years, and NICU work experience of 6.59 (4.5) years. Nurses had attended KMC workshop once. About 94% of the nurses had a bachelor's degree and the rest had a master's degree, and were working in circulating shifts. The findings showed that the most frequently mentioned barrier in KMC application among institutional and mother-related barriers was mother-related barrier [Table 2]. Based on paired t-test, mean mother-related barrier score was significantly higher than the institutional barrier score (P < 0.05).
Table 2.
Mean score of nurses’ perspective about KMC barriers
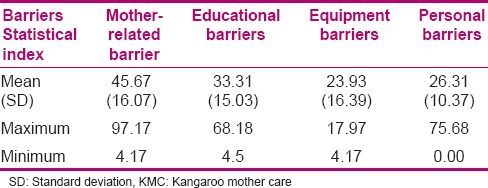
In this domain, 60% of the nurses claimed that lack of continuous attendance of mothers in the ward was the main KMC barrier. Other mother-related barriers were mothers’ fear of touching a premature infant, mothers’ fear of ward equipments, and twin or triplet of the infants. Mean (SD) score of institutional barriers was 28.9 (13.4). This domain had three sub-domains including educational barriers, personal barriers, and equipment and space barriers. In the domain of educational barriers, the most important KMC barrier was parents’ inadequate education and understanding about the importance of KMC. In the domain of personal barriers, the need for physician's order for KMC was the most important, and in the domain of equipment and space, lack of a private environment for the mothers was the most important.
DISCUSSION
The present study was conducted to define the level of KMC application and its barriers from the perspective of the nurses working in NICUs of Isfahan, Iran. Two important and basic factors of KMC including the infants’ age at which KMC was initiated and its length during 24 h were investigated. The obtained results showed that among the infants with a mean weight of 1510 g and gestational age of 32 weeks, KMC was started at the age of 8 days, with a mean length of 32 min once a day. Based on the definition of KMC, to attain the positive effects of KMC, its application is recommended in all infants, especially in premature infants, during 24 h with a minimum length of 1–2 h.[4] Blomqvist et al. in Sweden showed that the infants with gestational ages between 31.2 and 40 weeks and weight between 1715 and 3820 g received mean KMC application of 2.25 times a day with a mean length of 138 min in each session and 24 h KMC of 310 min (100–845) with a least length of 1 h. In their study, term infants also received KMC higher than the recommended length and number.[9] Meanwhile, in the present study, not only the infants with a gestational age higher than 38 weeks and a body weight more than 2500 g weight did not receive KMC, but also the infants receiving KMC did not receive the least amount of KMC. Karlsson et al., in a study conducted on infants with 22–26 weeks of gestational age in Sweden, showed that the mean length of KMC was 90 min (60–180 min).[12] Our obtained results showed that the weight and gestational age of the infants receiving KMC were consistent with other studies, although in the existing conditions, premature infants not only receive KMC later and at a lower number but also with a lower length in 24 h, compared to other countries.
In the present study, the infants with a higher birth weight received KMC earlier, which is consistent with the finding of Blomqvist et al. who reported the same results,[9] as very low birth weight infants firstly need NICU care. With regard to the difference in the length of KMC compared to other countries, detection of KMC barriers in Iran is of great importance. In the present study, the nurses believed that the most important barriers in KMC application were non-continuous attendance of mothers in the ward, necessity of a physician's order, mothers’ fear of touching their premature infant, overload of tasks in the ward, mothers’ fear of the existing equipment in the ward, having twins or triplets, and fear of infants’ catheter dispatch. In the present study, the most important barrier between institutional and mother-related barriers was mother-related barrier (non-continuous attendance of the mother in the ward).
In a similar study conducted in India, the barriers of KMC were categorized into six categories (knowledge, mother-related, environmental, family-related, positional, and infant-related barriers). The authors believed one of the most important barriers of KMC was lack of family members’ cooperation leading to inadequate time left for the mother to stay by her infant constantly, as she had to do other household affairs and, consequently, spend time to rest.[11] In Iran, due to inadequate facilities and space for mothers’ 24 h accommodation in the ward, low quality and hygiene of mothers’ room, mothers having another child at home, and impossibility of the grandparents attendance in the ward, mothers’ constant attendance is impossible. Meanwhile, in other European countries, the condition in the hospitals is such that it lets mothers’ 24 h stay in NICU. In this regard, a study was conducted in Sweden in 2012 to investigate the parents’ approach toward KMC facilitating factors. The results of the study showed that the parents claimed to have the needed facilities for their 24 h stay in the ward with respect to their privacy.[9] Meanwhile, in Iran, due to religious and cultural issues and inadequate facilities, the possibility of mothers’ constant attendance and application of KMC by the father and other family members like grandmothers is limited in NICUs, and fathers just visit their infants. With regard to institutional barriers, the most important barrier from the perspective of the nurses was in educational domain in which inadequate education and lack of parents’ understanding about the importance of KMC were the main issues. Similarly, in a study conducted in India on KMC and its application barriers, the nurses believed one of the major reasons for KMC was the difficulty in convincing the mother about the importance of KMC.[11] Ghasemi et al. showed that only 10% of the mothers had appropriate function concerning KMC in Tehran, Iran. They also indicated the important role of nurses and physicians in educating and transmitting the information to mothers.[13] The most important barrier found in the domain of equipment and space was a “private environment for the mothers.” In other words, mothers had no privacy to stay in the hospital and apply KMC. Similarly, in a study conducted in an NICU in Australia, it was reported that preparation of a physical environment is one of the major principles for KMC application.[10] Meanwhile, in a study conducted on 74 fathers and 76 mothers in Sweden, existing facilities for 24 h stay of parents along with their infants with respect to their privacy was reported as a facilitating factor for KMC application.[9] Another institutional barrier reported in the present study was the need for a physician's order for KMC in infant's file. Generally, the order for KMC is prescribed based on the infant's condition, organizational strategies, and physician's own interest. Chia et al. showed that lack of organizational support and a fixed protocol were among the KMC application barriers.[10] In comparison, Blomqvist et al. in Sweden showed that from parents’ perspective, organizational strategy and nurses’ support lead to encouragement, support, and facilitation of KMC.[9] The findings of the present study showed a significant association between nurses’ perspective concerning personnel-related barriers, and educational barriers and facilities and space barriers. In fact, when existing facilities and equipment are fewer and education is inadequate, personnel are less interested in KMC application.
Flynn and Leahy-Warren showed that KMC implementation could be facilitated through more education and knowledge of nurses as the barriers such as inadequate equipments and facilities and infant-related problems are modified.[14] The limitations of the present study were participants’ tiredness due to overload of work in NICU, for which the researcher tried to refer to the ward at the beginning of the working shift to complete the questionnaire. In addition, another study with a higher number of participants and other health team members such as mothers and physicians will yield a better approach toward KMC application.
CONCLUSION
The results showed that KMC was applied among premature infants with a mean length of 32 min, averagely once a day despite the recommendation of its application at least three times a day with a minimum length of 1 h. The present study showed that the most important barrier in KMC application was non-continuous attendance of the mothers in the ward, their fear of touching their premature infant, and the staff's need for a written order of the physician for application of KMC. Therefore, to promote and improve infant care program, especially premature infants, actions should be taken to modify such barriers and increase the length of KMC.
Financial support and sponsorship
Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study was derived from a research project (no. 393308) with the financial support of vice-chancellery for research of Isfahan University of Medical Sciences. Researchers greatly appreciate friendly cooperation of the nurses and mothers in Al-Zahra and Shahid Beheshti hospitals.
REFERENCES
- 1.Verklan T, Walden M. 5th ed. St. Loiese: Sunders; 2015. Core curriculum for neonatal intensive care nursing. [Google Scholar]
- 2.Datta P. 2nd ed. New Delhi: Jajpee brothers; 2009. Pediatric Nursing. [Google Scholar]
- 3.Lightbody T. The importance of family-centered care in the NICU. Can Nurse. 2009;105:11–20. [PubMed] [Google Scholar]
- 4.Ludington-Hoe SM. Kangaroo care as a neonatal therapy. Newborn Infant Nurs Rev. 2013;13:73–5. [Google Scholar]
- 5.Anderson GC, Chiu SH, Dombrowski MA, Swinth JY, Albert JM, Wada N. Mother-newborn contact in a randomaized trial of Kangaroo (skin to skin) care. J Obstet Gynecol Neonatal Nurs. 2003;32:604–11. doi: 10.1177/0884217503256616. [DOI] [PubMed] [Google Scholar]
- 6.Ludington-Hoe SM, Johnson MW, Morgan K, Lewis T, Gutman J, Wilson PD, et al. Neurophysiologic assessment of neonatal sleep organization: Preliminary results of a randomized controlled trail of skin contact with preterm infants. Pediatrecs. 2006:e909–23. doi: 10.1542/peds.2004-1422. [DOI] [PubMed] [Google Scholar]
- 7.Saeidi R, Tafazoli M, Robatsangi MG. Kangaroo Mather Care for infantile colic: A randomized clinical trial. Tehran Univ Med J. 2010;67:870–5. [Google Scholar]
- 8.Arzani A, Zahedpasha Y, Ahmadpour-Kacho M, Khafri S, Khairkhah F, Aziznejad P. Kangaroo care effect on self-esteem in the mothers of low birth weight infants. JBUMS. 2012;14:52–8. [Google Scholar]
- 9.Blomqvist Y, Frolund L, Rubertsson C, Nyqvist K. Uppsala, Sweden: Uppsala Universitet; 2012. Provision of Kangaroo Mother Care: Facilators and Barriers Neo-BFHI; p. 27. [Google Scholar]
- 10.Chia P, Sellick K, Gan S. The attitudes and practices of neonatal nurses in the use of kangaroo care. Aust J Adv Nurs. 2006;23:20–7. [PubMed] [Google Scholar]
- 11.Parikh S, Banker D, Shah U, Bala DV. Barriers in implementing community based kangaroo mother care in low income community. NHL Journal of Medical Science. 2013;2:36–8. [Google Scholar]
- 12.Karlsson V, Heinemann AB, Sjörs G, Nykvist KH, Agren J. Early skin-to-skin care in extremely preterm infants: Thermal balance and care environment. J Pediatr. 2012;161:422–6. doi: 10.1016/j.jpeds.2012.02.034. [DOI] [PubMed] [Google Scholar]
- 13.Ghasemi M, Dehdari T, Mohagheghi P, Gohari MR, Zargarzade Z. Mothers’ performance on caring for their premature infant: A pilot study. IJN. 2012;25:24–33. [Google Scholar]
- 14.Flynn A, Leahy-Warren P. Neonatal nurses’ knowledge and beliefs regarding kangaroo care with preterm infants in an Irish neonatal unit. Journal of Neonatal Nursing. 2010;16:221–8. [Google Scholar]


