Abstract
Introduction:
Metabolic syndrome is one of the emerging health problems of the world. Its prevalence is high in urban areas. Though pathogenesis is complex, but the interaction of obesity, sedentary lifestyle, dietary, and genetic factors are known as contributing factors. Community-based studies were very few to find out the prevalence or predictors of the syndrome.
Objectives:
To ascertain the prevalence and epidemiological predictors of metabolic syndrome.
Materials and Methods:
A total of 690 study subjects were chosen by 30 clusters random sampling method from 43 wards of Durgapur city. Data were analyzed in SPSS version 20 software and binary logistic regression was done to find out statistical significance of the predictors.
Results:
Among 32.75% of the study population was diagnosed as metabolic syndrome according to National Cholesterol Education Program Adult Treatment Panel III definition with a modification for Asia Pacific cut-off of waist circumference. Odds were more among females (2.43), upper social class (14.89), sedentary lifestyle (17.00), and positive family history.
Conclusion:
The overall prevalence of metabolic syndrome was high in urban areas of Durgapur. Increased age, female gender, higher social status, sedentary lifestyle, positive family history, and higher education were the statistically significant predictors of metabolic syndrome.
Keywords: Metabolic syndrome, obesity, sedentary lifestyle
Introduction
The world is in the phase of epidemiological transition where it is being observed that death due to noncommunicable diseases exceeds death due to communicable diseases. Metabolic syndrome is one emerging health problems. The syndrome is a cluster of risk factors such as central obesity, increased blood pressure, impaired glucose tolerance, altered lipid profile mainly low high density lipoproteins (HDL), and high triglycerides (TGs) which predispose the individual to increased risk for development of diabetes mellitus and cardiovascular diseases.[1,2] Pathogenesis of metabolic syndrome is complex, but the interaction of obesity, sedentary lifestyle, dietary, and genetic factors are known for their contribution.[2,3] Lifestyle factors appear to play an important role as obesity, especially abdominal obesity, and dyslipidemia worsen with urbanization and migration.[4,5]
The prevalence of metabolic syndrome is high among Asians including Indians, and is rising, particularly with the adoption of modernized lifestyle. Many studies in India have reported a high prevalence of metabolic syndrome.[6,7,8] The number of people with the metabolic syndrome also differs by sex, race, and ethnicity.[9] The main drivers causing the syndrome are related to rapid nutritional changes, lifestyle and socioeconomic transitions, consequent to increasing affluence, urbanization, mechanization, and rural-to-urban migration.[10,11] However, community-based study to find out such findings are few. Thus, a community-based study was done with the objective to ascertain the prevalence of metabolic syndrome and its epidemiological predictors in urban areas of West Bengal.
Materials and Methods
The study was a community-based cross-sectional study, carried out during the January to April 2015. Sample size calculation was done considering 33.5% metabolic syndrome in urban areas in India[12] taking 5% of absolute precision and (Z1-α/2)2 = 3.84 at 95% of confidence interval, and design effect 2 for the study design, sample size came to be 684. The population of Durgapur is 566,937. As samples were chosen by 30 cluster sampling, 23 study subjects were interviewed from each selected cluster (ward) by applying principles of cluster sampling design. Hence, the final sample size came to be 23 × 30 = 690. All selected study subjects were examined and interviewed by the principal and co-investigators. A pretested predesigned schedule was used for data collection. The schedule was modified after pretesting and it was validated for content validity by two different experts. The study was conducted after obtaining clearance from the Institution Ethics Committee and informed consent was obtained from each study subject. The samples were collected and examined in a departmental research laboratory. National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) devised a definition for the metabolic syndrome (NCEP, 2002), which was updated by the American Heart Association and the National Heart Lung and Blood Institute in 2005 (Grundy et al., 2005). According to the NCEP ATP III definition, metabolic syndrome is present if three or more of the following five criteria are met: Waist circumference over 40 inches (men), or 35 inches (women), blood pressure over 130/85 mmHg, fasting TG level over 150 mg/dl, fasting HDL cholesterol level <40 mg/dl (men), or 50 mg/dl (women), and fasting blood sugar over 100 mg/dl. Diagnosis of metabolic syndrome was done by NCEP ATP III definition[13] with a modification for Asia Pacific cut-off of waist circumference. Data were analyzed by the principal investigator in IBM Statistical Package for Social Sciences (SPSS) version 20 software and binary logistic regression was done, and the test was done to find out significance at P < 0.05.
Results and Analysis
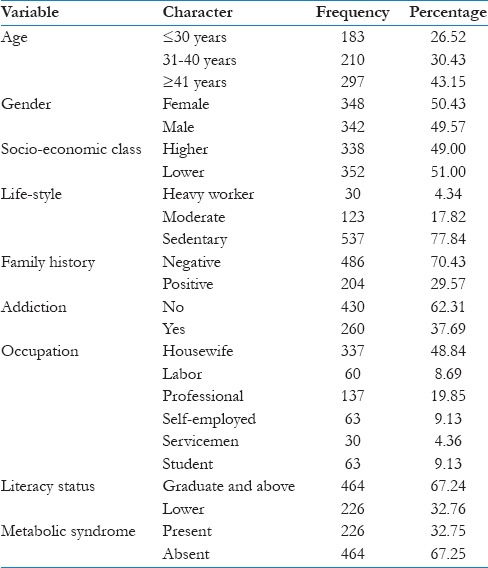
The study was conducted among 690 study population to ascertain the prevalence and epidemiological predictors of metabolic syndrome. The present study revealed [Table 1] that the majority of the study population belonged to 41 years of age and above [43.15%], with the almost equal distribution of males and females. Regarding socioeconomic status it was found that the percentage of Class III and below and Class IV and above were almost equal but regarding lifestyle, more than three-fourth of the population had a sedentary lifestyle (77.84%). The maximum of the study population did not have a family history of metabolic syndrome (70.43%). Among the study population of 37.69% were having some form of addiction. Most of the study population were housewives (48.84%), whereas only 19.85% were professionals. Most of the study population were graduate or above in regard to education (67.24%).
Table 1.
Distribution of study population according to prevalence and different epidemiological factors (n=690)
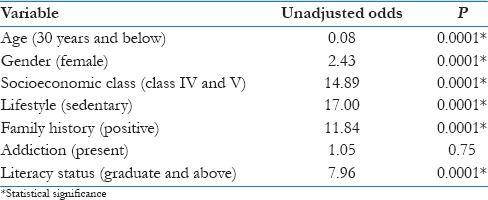
Among the study population of 32.75% had metabolic syndrome and the present study also revealed the unadjusted odds of different predictors of metabolic syndrome [Table 2]. The binary logistic regression revealed that age below 30 years was protective with odds of 0.08. The females had greater chances of having metabolic syndrome with odds of 2.43. The higher socioeconomic class (Class IV an above) had 14.89 times chances of having metabolic syndrome than those belonging to the lower socioeconomic class. Sedentary lifestyle had 17 times greater chances of having metabolic syndrome. Furthermore, positive family history and education level of graduate and above had odds of 11.84 and 7.96, respectively, with respect to the occurrence of metabolic syndrome. All the odds were found to be statistically significant [Table 2]. Multivariate regression was not done due to poor model fit.
Table 2.
Unadjusted odds of various predictors of metabolic syndrome
Discussion
The present study revealed that the overall prevalence of metabolic syndrome [Table 1] in the particular industrial city was 32.75% of diagnosed by NCEP ATP III definition with modification for Asia Pacific cut-off of waist circumference. Study finding was very similar to studies conducted by Prasad et al.[12] (33.5%), Misra et al.,[6] Ramachandran et al.,[14] etc.
Age as a predictor
Odds of having metabolic syndrome was less (0.08) in lower age group [Table 2], which was indirectly supported by many studies such as Sarkar et al.,[5] Ford et al.,[9] Qiao et al.,[15] and many others similar studies[16,17,18] which showed that the occurrence of metabolic syndrome increases with advancement of ages and was low in lower ages.
Gender as a predictor
Females [Table 2] had more odds (2.43) of having metabolic syndrome in comparison to males. Result regarding gender effect are conflicting with the majority of the studies finding the highest prevalence in women as compared to men[18,19] while the collaborative European analysis found no gender difference.[16,17]
Socioeconomic class as a predictor
The present study also revealed that the upper social class [Table 2] had 14.89 odds of having metabolic syndrome in comparison to lower social class which was just opposite in comparison to studies by Matthews et al.,[20] Zhan et al.,[21] etc., which showed chances of metabolic syndrome was more among lower socioeconomic status people but was similar to study by Prasad et al.[11] which revealed increased chances among higher socioeconomic status people.
Lifestyle as a predictor
A sedentary lifestyle was a proven factor for development of metabolic syndrome, as found by Kamble et al.,[22] and this study was not an exception. The present study revealed that odds of metabolic syndrome [Table 2] were 17 in comparison to moderate and heavy lifestyle.
Family history as a predictor
Positive family history as a predictor of metabolic syndrome was scarce, particularly in the community-based study and the present study [Table 2] revealed it as an important predictor with odds of 11.84.
Addiction as a predictor
Addiction had very little role in metabolic syndrome as revealed by the study (odds 1.05) and readily matches with similar of study by Zhan et al.[21]
Education as a predictor
Those who were a graduate or above had increased odds (7.96) in comparison to lower literate [Table 2] people and result was very close to a study conducted by Khanam et al.[23]
Conclusion
The overall prevalence of metabolic syndrome was high in the Durgapur city. As cluster sampling was done for choosing samples, the result could be generalized to urban areas of West Bengal. Increased age, female gender, higher social status, sedentary lifestyle, positive family history, and higher education were the statistically significant predictors of metabolic syndrome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Balkau B, Valensi P, Eschwège E, Slama G. A review of the metabolic syndrome. Diabetes Metab. 2007;33:405–13. doi: 10.1016/j.diabet.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Misra A, Vikram NK. Factors, definitions, predictive value and Asian Indian ethnicity: Complexities of the metabolic syndrome. Indian J Med Res. 2008;127:293–6. [PubMed] [Google Scholar]
- 3.Sudha V, Radhika G, Mohan V. Current dietary trends in the management of diabetes. Indian J Med Res. 2004;120:4–8. [PubMed] [Google Scholar]
- 4.Misra A, Vikram NK. Insulin resistance syndrome (metabolic syndrome) and obesity in Asian Indians: Evidence and implications. Nutrition. 2004;20:482–91. doi: 10.1016/j.nut.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Sarkar S, Das M, Mukhopadhyay B, Chakrabarti CS, Majumder PP. High prevalence of metabolic syndrome and its correlates in two tribal populations of India and the impact of urbanization. Indian J Med Res. 2006;123:679–86. [PubMed] [Google Scholar]
- 6.Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001;25:1722–9. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Gupta R, Sarna M, Rastogi S, Gupta VP, Kothari K. Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population. Diabetes Res Clin Pract. 2003;61:69–76. doi: 10.1016/s0168-8227(03)00085-8. [DOI] [PubMed] [Google Scholar]
- 8.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: The Chennai Urban Rural Epidemiology Study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 10.Misra A, Khurana L. The metabolic syndrome in South Asians: Epidemiology, determinants, and prevention. Metab Syndr Relat Disord. 2009;7:497–514. doi: 10.1089/met.2009.0024. [DOI] [PubMed] [Google Scholar]
- 11.Prasad DS, Kabir Z, Dash AK, Das BC. Cardiovascular risk factors in developing countries: A review of clinico-epidemiological evidence. CVD Prev Control. 2010;5:115–23. [Google Scholar]
- 12.Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J Cardiovasc Dis Res. 2012;3:204–11. doi: 10.4103/0975-3583.98895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 14.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults – A population study using modified ATP III criteria. Diabetes Res Clin Pract. 2003;60:199–204. doi: 10.1016/s0168-8227(03)00060-3. [DOI] [PubMed] [Google Scholar]
- 15.Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Heine R, Wareham NJ DECODE Study Group. Are insulin resistance, impaired fasting glucose and impaired glucose tolerance all equally strongly related to age? Diabet Med. 2005;22:1476–81. doi: 10.1111/j.1464-5491.2005.01655.x. [DOI] [PubMed] [Google Scholar]
- 16.Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K DECODE Study Group. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Arch Intern Med. 2004;164:1066–76. doi: 10.1001/archinte.164.10.1066. [DOI] [PubMed] [Google Scholar]
- 17.Hu G, Qiao Q, Tuomilehto J, Eliasson M, Feskens EJ, Pyörälä K DECODE Insulin Study Group. Plasma insulin and cardiovascular mortality in non-diabetic European men and women: A meta-analysis of data from eleven prospective studies. Diabetologia. 2004;47:1245–56. doi: 10.1007/s00125-004-1433-4. [DOI] [PubMed] [Google Scholar]
- 18.Gu D, Reynolds K, Wu X, Chen J, Duan X, Reynolds RF, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. 2005;365:1398–405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. Adults. Diabetes Care. 2004;27:2444–9. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 20.Matthews KA, Räikkönen K, Gallo L, Kuller LH. Association between socioeconomic status and metabolic syndrome in women: Testing the reserve capacity model. Health Psychol. 2008;27:576–83. doi: 10.1037/0278-6133.27.5.576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhan Y, Yu J, Chen R, Gao J, Ding R, Fu Y, et al. Socioeconomic status and metabolic syndrome in the general population of China: A cross-sectional study. BMC Public Health. 2012;12:921. doi: 10.1186/1471-2458-12-921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamble P, Deshmukh PR, Garg N. Metabolic syndrome in adult population of rural Wardha, central India. Indian J Med Res. 2010;132:701–5. [PMC free article] [PubMed] [Google Scholar]
- 23.Khanam MA, Qiu C, Lindeboom W, Streatfield PK, Kabir ZN, Wahlin Å. The metabolic syndrome: Prevalence, associated factors, and impact on survival among older persons in rural Bangladesh. PLoS One. 2011;6:e20259. doi: 10.1371/journal.pone.0020259. [DOI] [PMC free article] [PubMed] [Google Scholar]


