Abstract
Background:
There is little data as to what extent national Emergency Medical Services (EMS; 911) utilize poison control centers (PCCs). A review of data from our PCC was done to better understand this relationship and to identify potential improvements in patient care and health care savings.
Methods:
Retrospective chart review of a single PCC to identify calls originating from 911 sources over a 4-year study period (1/1/08–12/31/11). Recorded variables included the origin of call to the PCC, intent of exposure, symptoms, management site, hospital admission, and death. Odds ratios (OR) were developed using multiple logistic regressions to identify risk factors for EMS dispatch, management site, and the need for hospital admission.
Results:
A total of 7556 charts were identified; 4382 (58%) met inclusion criteria. Most calls (63.3%) involved accidental exposures and 31% were self-harm or misuse. A total of 2517 (57.4%) patients had symptoms and 2044 (50.8%) were transported to an Emergency Department (ED). Over 38% of calls (n = 1696) were handled primarily by the PCC and did not result in EMS dispatch; only 6.5% of cases (n = 287) with initial PCC involvement resulted in crew dispatch. There were 955 (21.8%) cases that resulted in admission, and five deaths. The OR for being transported to an ED was 45.4 (95% confidence interval [CI]: 30.2–68.4) when the crew was dispatched by the PCC. Hospital admission was predicted by intent for self-harm (OR 5.0; 95% CI: 4.1–6.2) and the presence of symptoms (OR 2.43; 95% CI: 1.9–3.0). The ORs for several other predictive variables are also reported.
Conclusions:
When 911 providers contact a PCC about poisoning-related emergencies, a history of intentional exposure and the presence of symptoms each predicted EMS dispatch by the PCC, patient transport to an ED, and hospital admission. Early involvement of a PCC may prevent the need for EMS activation or patient transfer to a health care facility.
Keywords: 911 triage, emergency medical services, poison center
Introduction
An estimated 240 million 911 calls are placed each year in the US many of which are made to access Emergency Medical Services (EMS) for medical reasons. In 2012, U.S poison control centers (PCCs) handled over 3.3 million calls related to poisonings and drug information, including 2.27 million human exposures.[1] Previous work shows that PCC involvement in the care of poisoned patients results in health care savings.[2,3,4,5,6,7,8] Little is known about the extent of which EMS providers utilize PCCs related to human poisoning exposures. Previous work on the interaction between PCCs and EMS have included the use of dispatch protocols (to identify low-acuity patients via secondary triage; MPDS Omega protocol) and the nature of poisonings to require prompt evaluation and treatment.[9,10,11] A review of regionalized emergency care identified the role that PCCs should play, despite “working in silos” in a “shift in paradigm of bring the doctor to the patient, at the right place, at the right time.”[12] These papers identified the lack of a true understanding of how EMS and PCCs work together within a shared emergency care delivery system.
We conducted a retrospective analysis of a single PCC's data to document and analyze the role that a PCC serves for an urban 911 service. We abstracted specific data (i.e., intention of the exposure, self-harm versus accidental, and symptoms) based on our understanding of previous triage protocols for EMS agencies.[11] A better understanding of this relationship may foster more cooperation that enhances patient care while saving health care resources.
Methods
A retrospective review of PCC charts was done by running a search using Visual Dotlab Enterprise® (version 4.3.1; 2014) software of all calls received over the 4-year study period between January 2008 and December 2011. This search yielded a total of 421,343 calls to our PCC; 7556 (1.8%) of which originated from either EMS crew members or 911 dispatchers (collectively referred to as 911 sources). These calls were then filtered for human exposures. Calls related to scorpion envenomations, EMS drills, hazmat incidents (without an identified patient), and information only were excluded. Such calls were excluded due to their unique nature to our area (i.e., scorpion calls) or our preexisting partnership for drills and hazmat events. The numbers for excluded calls are shown in Figure 1. Calls involving patients that were lost to follow-up (unknown outcomes) were also excluded. Most of the calls lost to follow-up lacked case-specific information due to the caller refusing further PCC involvement or no record of their arrival to the intended facility. All charts meeting inclusion criteria were manually reviewed by investigators trained in the systematic chart review. The abstracted data were stored using an electronic spreadsheet on password protected computers.
Figure 1.
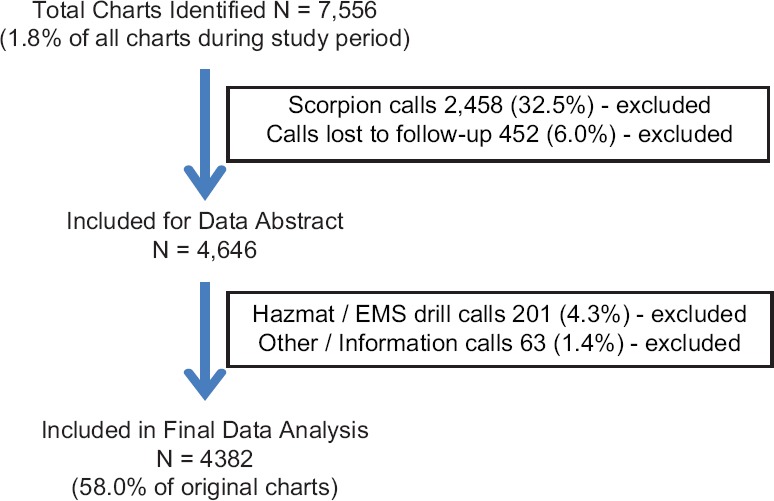
Total charts and exclusion criteria
Descriptive statistics were used on continuous variables and reported as means. Individual analyses of categorical variables are reported with percentages based on the total number of cases with complete data. Multiple logistic regressions were used to identify outcome predictors. Predictors with univariate P values < 0.10 were entered into the models. Forward LR regression was used; adjusted P < 0.05 was required for a predictor to remain in the final model. Goodness of fit was evaluated using the Breslow-Day test. A total of 34 (5.2%) cases were coded as “unable to follow” but contained sufficient outcome data to be included in the analysis.
A random sample of 125 (2.8%) charts was reviewed by a second investigator to ensure the accuracy of data abstraction. This re-analysis found a recording accuracy of 98.6% (95% confidence interval: 97.7–99.1) for 1250 data points. This study received approval from our institution's investigational review board.
Results
A total of 7556 charts from 911 sources were identified during the 4-year study period. Of these, 3174 (42%) were excluded for various reasons [Figure 1]. The remaining 4382 (58%) charts met inclusion criteria and were analyzed. The subjects’ mean age was 24.4 years (interquartile range: 2–40) and 53.3% were women [Note: Some charts had missing data for specific variables. In such cases, only the number of charts with recorded data for that variable is included in the analysis, [Table 1].
Table 1.
Chart data and subjects characteristics
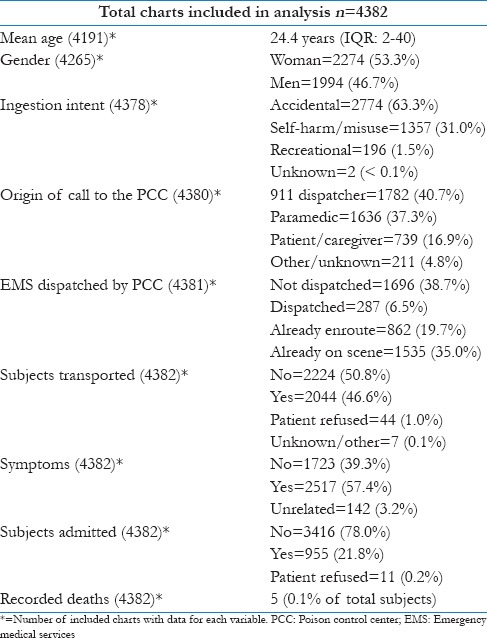
Overall data concerning subject characteristics and recorded variables are reported in Table 1. A total of 78% (3418 out of 4380) of all included calls to the PCC originated from a 911 source. Of these 3418 calls, the EMS crew was either already en route (19.7%) or on the scene (35%). Almost 17% (739 out of 4380) of calls originated from a layperson (i.e., patient or caregiver) who called 911 directly but was transferred to our center.
Most (n = 2774; 63.3%) of all included calls (n = 4378) were related to accidental exposures; 31% were coded as self-harm or misuse and 1.5% as recreational use. A total of 2517 (57.4%) patients had symptoms coded as being related to the reported exposure. Over 38% of all included calls (n = 1696) were handled primarily by the PCC and did not result in the dispatch of an EMS crew. In fact, only 6.5% of calls (287 of 4381) with initial PCC involvement resulted in the PCC, dispatching an EMS crew. EMS crews transported 2044 (50.8%) patients for further evaluation in an Emergency Department (ED) and 955 (21.8%) cases resulted in hospital admission. These admissions included patients who were medically cleared for inpatient psychiatric care.
The percentages for different subgroup comparisons are shown in Tables 2-5. Several findings suggest that early (and increased) involvement of a PCC may decrease the need for EMS involvement and patient transfers, particularly in patients without a history of self-harm or symptoms.
Table 2.
Intent of exposure versus origin of call to PCC
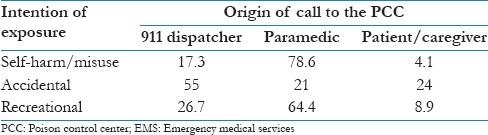
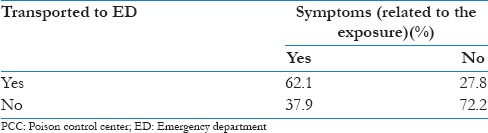
Table 5.
Transport versus symptoms
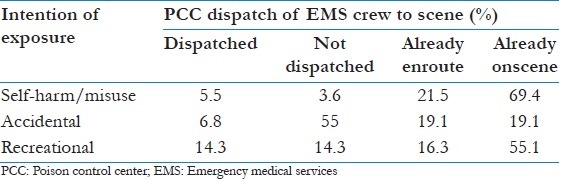
When comparing the origins of PCC calls with exposure intent, most cases, regardless of intent, originated from 911 sources: 78.6% of cases involving self-harm or misuse and the majority of calls regarding accidental or recreational exposures [Table 2]. Relatively few (8.9%) recreational exposures were called into the PCC by a patient or caregiver. Table 3 shows that most (71.4%) recreational calls already had an EMS crew en route or on the scene.
Table 3.
Intent of exposure versus EMS dispatch
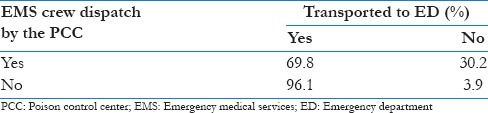
Data suggest that when EMS was dispatched prior to PCC involvement the patient was more likely to be transferred to an ED. This trend of increased patient transport without PCC involvement is suggested in Table 4, where 96.1% of patients without PCC involvement were transferred to an ED compared to 69.8% of those where EMS was dispatched by the PCC.
Table 4.
EMS dispatch by the PCC versus transported to ED
Finally, Table 5 shows no strong trend between symptoms (independently) and transport, suggesting that other factors (such as intent or EMS presence on the scene) influenced transfer patterns.
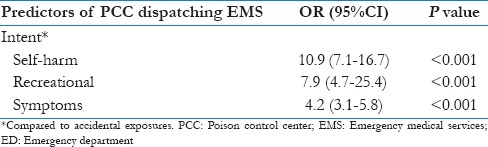
Multiple logistic regressions were used to identify independent predictors of the three main outcomes: EMS dispatch by the PCC, patient transport to an ED, and patient admission. When predicting if the PCC would dispatch an EMS crew, those patients with intentional (compared to accidental) exposures or symptoms were more likely to have EMS dispatched [Table 6].
Table 6.
Odd ratios of EMS dispatch by the PCC
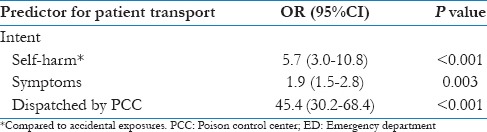
In cases involving EMS transported to an ED, intent of self-harm, presence of symptoms, and EMS dispatch by the PCC, were each predictive of transport. These odds ratio are shown in Table 7.
Table 7.
Odd ratios for patient transport to the ED
For admission to a heath care facility, intent for self-harm and the presence of symptoms were again predictive [Table 8]. Not surprisingly, ED arrival via EMS for a poisoning-related exposure was strongly associated with subsequent admission. Again, these admissions included medical and psychiatric diagnoses.
Table 8.
Odd ratios for patient admission to a hospital

There were five recorded deaths. These included three intentional ingestions of prescription medications, one accidental death of a man who fell into a vat of sulfuric acid, and one intentional herbicide ingestion. All five calls originated from EMS personnel caring for symptomatic patients who were transported to an ED and subsequently died.
Discussion
There is little previously reported work in the area of shared patient care between EMS agencies and PCCs. One prospective study followed 262 EMS calls, diverted to a PCC by 911 dispatchers, and found no adverse effects or treatment delays.[9] Another, retrospective work concluded that the involvement of PCC services for 911 calls related to accidental ingestions may improve patient care and save health care resources.[10]
Most PCCs are staffed with nurses and pharmacists, specifically trained and certified in poisoning emergencies, who answer calls 24 h a day from the public and medical professionals. These calls concern exposures to medications, chemicals, poisonings, and envenomations. In general, all PCCs are tasked with making triage decisions based on limited information that cannot be confirmed. Staff is trained to obtain relevant data prior to make management decisions (e.g., home monitoring vs. ED referral) and determining the frequency of follow-up calls. In addition, to ask about the specific exposure (substance(s) and intent) and active symptoms, comorbidities and patient location. The patient's environment (e.g., home vs. remote area) can introduce variables that influence triage decisions. This case-based evaluation technique is a potentially useful tool for EMS providers who are tasked with other objectives. Combining PCC and 911 data should increase the efficiency of EMS resources.
Although no firm conclusions can be drawn from these data they do help to better understand the relationship between EMS services and a PCC. These data suggest that PCCs have opportunities to be more involved in 911 calls concerning accidental and recreational poisoning exposures. These findings and previous related works[9] suggest that PCCs can often manage these patients safely at home. Doing so may help prevent unnecessary crew dispatch and patient transport.
As with all retrospective PCC studies, our limitations included the potential for bias related to patient selection and reporting data (e.g., being notified about symptomatic patients). As a retrospective review, coded data in our records was not independently verified by reviewing 911 charts or follow-up with involved subjects. Many of the excluded calls were lost to follow-up. The outcomes of these cases (patients) are unknown but may have affected our results and conclusions. Finally, it is expected that many subjects eligible for inclusion were never reported to our PCC by 911 providers.
Conclusions
A retrospective review of calls from EMS sources to an urban poison center was done to identify descriptive statistics and trends. Three focused outcomes (PCC dispatch of EMS crews, EMS transport of patients to an ED, and patient admissions) were all predicted by the presence of symptoms and the intent of the exposure. These findings suggest that for 911 calls related to poisoning exposures, the history of events (intent of the exposure) and focused assessment (symptoms attributable to exposure) are paramount. Based on these data, the early involvement of a PCC for poisoning-related 911 calls may prevent unnecessary use of EMS and health care resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mowry JB, Spyker DA, Cantilena LR, Jr, Bailey JE, Ford M. 2012 Annual Report of the American Association of Poison Control Centers National Poison Data System (NPDS): 28th Annual Report. Clin Toxicol. 2013;51:949–1229. doi: 10.3109/15563650.2013.863906. [DOI] [PubMed] [Google Scholar]
- 2.LoVecchio F, Curry S, Waszolek K, Klemens J, Hovseth K, Glogan D. Poison control centers decrease emergency healthcare utilization costs. J Med Toxicol. 2008;4:221–4. doi: 10.1007/BF03161204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kearney TE, Olson KR, Bero LA, Heard SE, Blanc PD. Health care cost effects of public use of a regional poison control center. West J Med. 1995;162:499–504. [PMC free article] [PubMed] [Google Scholar]
- 4.Chafee-Bahamon C, Lovejoy FH., Jr Effectiveness of a regional poison center in reducing excess emergency room visits for children's poisonings. Pediatrics. 1983;72:164–9. [PubMed] [Google Scholar]
- 5.Harrison DL, Draugalis JR, Slack MK, Langley PC. Cost-effectiveness of regional poison control centers. Arch Intern Med. 1996;156:2601–8. [PubMed] [Google Scholar]
- 6.Kelly NR, Ellis MD, Kirkland RT, Holmes SE, Kozinetz CA. Effectiveness of a poison center: Impact on medical facility visits. Vet Hum Toxicol. 1997;39:44–8. [PubMed] [Google Scholar]
- 7.King WD, Palmisano PA. Poison control centers: Can their value be measured? South Med J. 1991;84:722–6. [PubMed] [Google Scholar]
- 8.Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C, et al. The impact of poison control centers on poisoning-related visits to EDs – United States, 2003. Am J Emerg Med. 2008;26:310–5. doi: 10.1016/j.ajem.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Anderson BD, Manoguerra AS, Haynes BE. Diversion of 911 poisoning calls to a poison center. Prehosp Emerg Care. 1998;2:176–9. doi: 10.1080/10903129808958867. [DOI] [PubMed] [Google Scholar]
- 10.Bier SA, Borys DJ. Emergency medical services’ use of poison control centers for unintentional drug ingestions. Am J Emerg Med. 2010;28:911–4. doi: 10.1016/j.ajem.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Studnek JR, Thestrup L, Blackwell T, Bagwell B. Utilization of prehospital dispatch protocols to identify low-acuity patients. Prehosp Emerg Care. 2012;16:204–9. doi: 10.3109/10903127.2011.640415. [DOI] [PubMed] [Google Scholar]
- 12.Carr BG, Matthew Edwards J, Martinez R. Academic Emergency Medicine Consensus Conference, Beyond Regionalization: Integrated Networks of Care. Regionalized care for time-critical conditions: Lessons learned from existing networks. Acad Emerg Med. 2010;17:1354–8. doi: 10.1111/j.1553-2712.2010.00940.x. [DOI] [PubMed] [Google Scholar]


