Abstract
Background:
Southeast Asian countries with better-skilled primary care physicians have been shown to have better health outcomes. However, in Indonesia, there has been a large number of inappropriate referrals, leading to suboptimal health outcomes. This study aimed to examine the reasons underlying the unnecessary referrals as related to Indonesian physicians’ standard of abilities.
Materials and Methods:
This was a multiple-case study that explored physicians’ self-evaluation of their abilities. Self-evaluation questionnaires were constructed from the Indonesian Standards of Physicians Competences of 2006-2012 (ISPC), which is a list of 155 diseases. This study was undertaken in three cities, three towns, and one “border-less developed” area during 2011-2014. The study involved 184 physicians in those seven districts. Data were collected using one-on-one, in-depth interviews, focus group discussions (FGDs), and clinical observations.
Results:
This study found that primary care physicians in Indonesia felt that they were competent to handle less than one-third of “typical” primary care cases. The reasons were limited understanding of person-centered care principles and limited patient care services to diagnosis and treatment of common biomedical problems. Additionally, physical facilities in primary care settings are lacking.
Discussions and Conclusions:
Strengthening primary health care in Indonesia requires upscaling doctors’ abilities in managing health problems through more structured graduate education in family medicine, which emphasizes the bio-psycho-socio-cultural background of persons; secondly, standardizing primary care facilities to support physicians’ performance is critical. Finally, a strong national health policy that recognizes the essential role of primary care physicians in health outcomes is an urgent need.
Keywords: Ability, competency, family medicine, physicians’ competences/abilities, primary health care
Introduction
The World Health Organization (WHO) constitution 2004 states that health is one of the fundamental rights of every human.[1] The WHO explained that primary care involves essential care, which should be done practically, scientifically, and in such a way as to be socially acceptable by all people, irrespective of their gender, disease, and organ system. It is to be carried out with a focus on affordable cost, and should include social and economic development. Primary care is often the first contact and step in the establishment of continuous and comprehensive health care.[2]
Starfield noted that primary care contributes greatly to the quality of health care in a country.[3] Countries such as Australia, the Netherlands, and the United Kingdom have shown that 95% of all cases can be handled by primary care practitioners.[4,5] These countries apply family medicine principles in their primary care service. Features of good family medicine include continuity, comprehensiveness, coordination, collaborativeness, and community-oriented and family-focused care.[6] The continuity of the relationship and person-centered care allows the family physicians’ ability to analyze the needs of, and risks to the individual.[7] Well-trained family medicine doctors are in an ideal position to improve community health practice by virtue of their long-term functional relationship with the local community.[8] A study in Southeast Asian countries showed that training family doctors has been shown to have an impact on better health outcomes.[9] However, this type of training is currently lacking in Indonesia.
The quality of primary care in Indonesia is lower than that in other Association of Southeast Asian Nations (ASEAN) countries. In 2007, the WHO published health profiles from various countries. Indonesia ranked unfavorably compared with other countries in ASEAN.[10] There are some unique challenges in Indonesia. Indonesia is an archipelago with 17,508 islands. There are 9,559 primary health centers throughout Indonesia, with approximately 40,000 primary care practitioners. The number of primary care physicians is insufficient to meet the needs of Indonesia's 256 million people.[11,12]
The ideal competencies of Indonesian primary care physicians have been set by the Indonesian Standards of Physicians Competences (ISPC) in 2006 and these were renewed in 2012.[13] Critical to this standard is physicians’ understanding of the scope of their clinical abilities. Physicians who believe they are incapable of caring for patients make more referrals to specialists.[14] In 2011, data on physicians’ self-evaluation were obtained from 18 general practitioners in a district of northern Indonesia. Only eight diseases are perceived to be within their area of competence.[15] Moreover, a national survey showed that fewer than 5% of normal deliveries were attended to by a primary care physician.[16]
Objectives
This study aimed to assess Indonesian physicians’ self-perceived abilities in primary care settings using ISPC (2006, renewed 2012) as a benchmark. The study was conducted in seven districts among 33 provinces in Indonesia.
Materials and Methods
Study design and settings
This study evaluated physicians’ self-evaluation of their ability to manage patients in primary care settings in seven districts of Indonesia. The robustness of the results was assured by using three methods of assessment: In-depth interviews, focus group discussions (FGDs), and clinical observations.
Ethical clearence was issued by the Medical and Health Research Ethics Committee (MHREC) of the Faculty of Medicine, Gadjah Mada University, in 2010: KE/FK/492/EC.
The study areas were based on the preexisting primary care districts as defined by the Ministry of Health, 2011-2013. Indonesia has 34 provinces and 514 districts encompassing three time zones with 17,000 islands; the people speak 13,000 local languages and one national language, Bahasa Indonesia.[17]
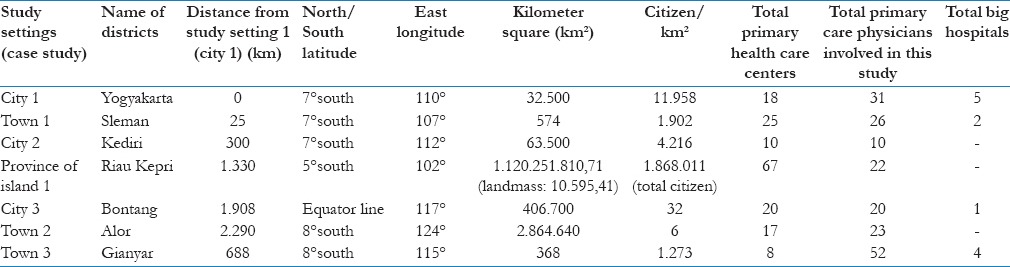
The researchers used snowball sampling until sufficient data were collected that saturation was achieved. After studying seven districts, a repeating pattern of results was found, making it unlikely that new information would be gained by involving additional districts. Table 1 contains detailed descriptions of the seven study settings. The study settings are geographically separated throughout Indonesia, ranging from between 25 km and 2,290 km from the first study setting.[10,11,12] The cities and towns involved in this study were: Yogyakarta - middle Java Island, Sleman - middle Java Island, Kediri - eastern Java Island, Bontang - eastern Kalimantan Island, Gianyar - Bali Island, and underdeveloped-border areas or islands such as Alor - western Timor Island and Riau Islands Province - middle Sumatra Island [Table 1].
Table 1.
Detail descriptions of 7 study settings based on Indonesian Ministry of Health reports
Subjects
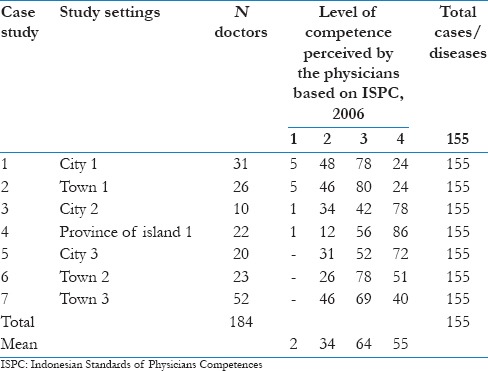
This study included all of the primary care physicians in each seting who were part of the Primary Care Project of the Ministry of Health, 2010-2014.[11] Table 2 provides details of the number of physicians involved.
Table 2.
Results of self-evaluation on physicians’ ability in managing 155 diseases listed by ISPC (2006, renewed 2012)
Instruments
The construction of the self-evaluation questionnaire was based on attachment 3 of the 2006 (renewed 2012) ISPC, i.e., the list of diseases that could and should be managed independently by physicians working in primary care.[13] The perceived level of competence of the physicians was measured based on scaled levels, namely: Level 1: Ability to recognize and explain the clinical picture of the disease; Level 2: Ability to recognize the clinical disease and referring only those patients who are outside the scope of practice of a primary care physician; Level 3: (A) ability to diagnose nonemergent cases, perform initial management, and only refer to secondary care if needed, or (B) ability to diagnose emergency cases and perform initial management; (4) Level 4: Ability to diagnose cases and conduct management independently and thoroughly, the ideal scenario.
Procedures and analysis
Researchers personally administered the self-evaluation form and followed with interviews or FGDs, and clinical observations. Researchers transcribed results within 48 h of data acquisition. The results were analyzed by all the researchers (except MG), based on the multiple case-study methodology approach.[18] A radar graph was chosen to illustrate the findings. The results of this study were reported as a sequence of multiple cases to show similar patterns that were found in different study settings. These approaches eventually led to data saturation, with a low likelihood that further data would change the outcome.
Results
Table 2 shows that among the 155 diseases that should be managed independently by Indonesian primary care physicians, only 55 were considered comfortably manageable by the physicians. The rest were referred to hospitals. Table 3 showed the list of the 155 diseases from the ISPC. The FGDs or interviews and the observations were consistant with these findings. A “radar graph” [Figure 1] illustrates the pattern of Indonesian physicians’ self-evaluation regarding their abilities in managing patient in all seven study settings. The ideal graph will be a full radar-graph that shows that physicians felt confident that they could handle all the 155 diseases, as expected by the ISPC (2006, renewed 2012) [Tables 2 and 3; Figure 1].
Table 3.
List of diseases in ISPC, 2006-2012 that should be handled independently by primary care physicians
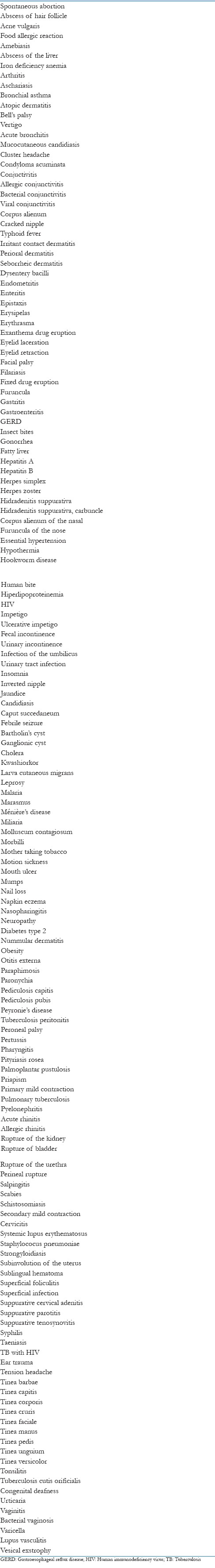
Figure 1.
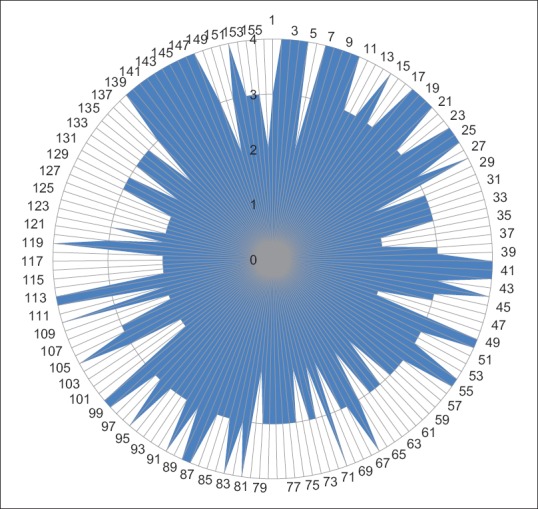
Physicians’ self-evaluation (N = 184) of ability in managing primary health problems in 7 study settings in this multiple-case study. Notes: Numbers 1-155 illustrated in round are diseases listed in ISPC, 2006-2012 that should be handled independently by primary care physicians. The list is explained in Table 3. Numbers 0-4 illustrated in vertical order are levels of independence of primary care physicians in managing health problems, from extremely dependent to totally independent, based on ISPC, 2006-2012
Case study 1 (City 1 study setting)
City 1 is a capital city of a province in middle Java Island. The physicians there felt that they lacked the ability to solve problems completely and independently, and that they could only diagnose and then refer directly (Level 2 of ISPC, 2006, renwed 2012): As noted by one of them, “When I meet patients with health problems, I do not feel confident handling them, so it is better that I refer to hospital specialist. For example, hypertension, and diabetes mellitus.” (FGD with physicians in City 1).
The physicians’ lack of self-confidence is supported by the observation that the physician was unable to perform person-centered care, unable to explore the patient's biopsychosocial aspects, and only facilitated a minimal intensity in doctor-patient communication. On top of that, the laboratory facilties in Puskesmas were only used by visiting hospital specialists: “Actually our lab facilities in Puskesmas are complete enough, including routine blood test urine test, lipid profile, kidney function and ECG. However, those who operate it usually are visiting specislists. We are not so confident in using it.” (FGD with physicians in City 1).
Case study 2 (Town 1 study setting)
The same pattern as in City 1 was also found in City 2. Most physicians felt only capable of dealing with approximately half of the diseases, requiring referral for the rest. (Level 3). As noted by one physician, “I pay attention to the patient's biopsychosocial aspects when the patients who I serve are the influential official/people.” (FGD with physicians in Town 1).
Physicians in this setting noted that that there is lack of time allowed and limited financial support from the government to pursue graduate study in primary care. As noted by one participant, “We have difficulties in joining any graduate course of family medicine, because there is no time allowed for formal education. Maybe, only few days in a year.” (FGD with physicians in Town 1).
Case study 3 (City 2 study setting)
Physicians felt that they were able to deal with less than half of 155 diseases completely and independently. FGDs revealed a lack or orientation toward family and community care, seeing illness as only a biomedical process limited to clinical diagnosis and treatment.
“My duty as a non-permanent physician is only assigned in clinics (limited in the patient-care room); I may not handle the others.” (FGD with physicians in City 2).
“We almost never check and evaluate the performance of the lab equipment.” (FGD with physicians in City 2).
Case study 4 (Province of Islands 1 study setting)
Individuals in Island Province 1 fared better than did physicians in other settings. These physicians had adequate confidence in their ability to solve problems completely and independently for slightly more than half of the 155 diseases. There were only 12 diseases that they felt needed to be referred immediately. The result of the qualitative data in this setting showed that physicians in the Province of Islands 1 were supported by structured training about family medicine by the district health care office, although this was not yet a formal education.
“I enjoyed visiting families in the afternoon, that we did everyday in the entire years, we established very good relationship with all families and to see them when they are healthy and when they come to our clinic during the illnesses.” (FGD with physicians in Province of Islands 1).
“Before we were deployed to the islands, we were gathered at the provincial level and then trained in the principles of family medicine for five days, followed by specific assignments for physicians who work on the islands, especially home visits every afternoon and coordination of health services in sub-health center with another health workers.” (FGD with physicians in Province of Islands 1).
These physicians were also supported by adequate health facilities. Moreover, the physicians’ salary was 2 × higher than those of physicians who worked in another case-study setting. In addition, the physicians in province area 1 were given responsibilities for managing health problems on island areas with limited or no backup available. Physicians at this site were assigned daily home visits with patients on a regular basis.
The lack of specialists in this island province was associated with greater perceived abilities of the primary care physicians working in that area when compared to the other areas studied.
“All medication and equipment were provided compeletely by the district health care and we just ordered what we need and they will provide them all.” (FGD with physicians in Province of Islands 1).
Case study 5 (City 3 study setting)
A similar pattern was found as in the previous two urban settings. Physicians felt that they were able to deal wth less than half of the diseases.
“The continuing courses for primary care doctors emphasized more on the management of the clinic instead of clinical skills.” (FGD with a physician in City 3).
“Sometimes the midwives refer their patients to us, and then we refer directy to the specialist.” (FGD with a physician in City 3).
The physicians’ opinion was supported by the observation that the content of the medical record was incomplete and did not reflect any comprehensive treatment plan (incomplete medical record, blank space on genogram) or any information on family dynamics. Individual and community care were also housed in different buildings, with two different managements.
Case study 6 (Town 2 study setting, a second island setting)
Physicians only felt comfortable dealing with one-third of the selected diseases. Again, the duty of a primary care physician was expressed by noting that, “I do not really pay attention to the social problems of patients, neither health promotion programs; the important things are clinical problems.” (Interview with one physician in Town 2).
The results of observations in this setting showed that many primary care physicians were not involved in public health programs. Much of the medical equipment seemed unstandardized and inadequate. No small boat or canoe was available for transportation across the small islands. Most of the health professionals were using a motorcycle, which is often inadequte given the geographical contour in this region. An ambulance was underused because there was no available budget for regular maintainance.
Case study 7 (Town 3 study settings)
The lack of confidence in their ability to hand primary care problems was also seen in this region.
“Promotion and prevention are done only when there is a program from the District Health Office.” (Interview with Physician 1 in Town 3).
The results of observations in this study setting showed that there was limited involvement in doctor-patient communication and very limted community or family involvement. Moreover, high-quality medical equipment was available but rarely used even by the specialists.
“All equipment was easily gained with supports from the dictrict health care office; we are in the tourism area so we care about appearance of buildings and comfortness of rooms. We have ultrasounds, ECG, which are used by the specialists.” (Interview with Physician 1 in Town 3).
Discussion
This is the first study exploring gaps between the realities of practices of Indonesian primary care physicians in light of the high expectation of ISPC (2006, renewed 2012). The researchers involved hundreds of physicians in seven different areas of Indonesia in a 5-year extensive study. The locations studied varied and included cities, towns, island provinces, and border areas. A repeated pattern was found in seven of the study settings, the consistency of which likely increases the trustworthiness of the case-study data. A change toward better primary care is challenging in most countries. It can take a generation for Western countries to establish a well-trained cadre of primary care physicians who are able to handle most health problems.[4] Many of the ASEAN countries have succeeded, but Indonesia is still on the early learning curve.[9]
The dependence of Indonesian physicians working in primary care was mainly due to, first, orientation towards the minimum curative care (disease-centered care) and no attempt at aspects of promotion and prevention in individuals, families, and communities (person-centered care). Therefore, more structured formal graduate education as a continuation of basic medical education, which emphasizes that mastering the principles of family medicine is strongly needed for Indonesia. Second, the dependence of the physicians is reinforced by the lack of adequate infrastructure and facilities in primary health care in Indonesia. To repair this will require a commitment on the part of national and regional leaders. Appropriate local care will be able to rule out inappropriate referrals. The recent implimentation of the National Insurance system (JKN), since January 1, 2014 and the Act on Medical Education in 2013 have started to move health care orientation toward strengthening Indonesian primary care services. Researchers hope that this effort is effective and continuous.
At the time that this study was done, there were no primary-care educational standards, norms, standards, or guidelines from the Ministry of Health, Republic of Indonesia. Therefore, it was not surprising that there was variation in the competence of physicians working in primary care settings and the supporting facilities.
The results of this study illustrate a phenomenon of gaps that are very amenable to intervention, which will lead to the improvement of the quality of care by physicians who work in primary care settings. The Government of Indonesia issued the JKN in 2013 and the Act of Medical Education, No. 20 of 2013, articles 7 and 8, which state the aims of improving the quality of primary care by upgrading the primary care physicians’ education to equal other countries’ family medicine specialist level.[19,20] Our findings support the need for implementation of changes in medical education, which, at this point, has yet to be realized.
Even the best site only met one of the criteria for good primary care, that of the physician being the first physician to contact the patients, and to follow through with treatment and referral if necessary. The other principles of familly medicine were not implemented, such as comprehensive and holistic case management, patient-focused case management, and the management of community cases.[6,7]
The principle of “comprehensive case management” was inadequately implemented at these primary care sites in in Indonesia. There was limited continuity of care or coordination of the follow-up after the patient was discharged from secondary health care. Physicians in this study felt that their duties were only to give referrals and delegate the responsibilities to the physician in secondary health facilities. Coordination among primary health care teams should appear collaboratively with regard to implementing more “comprehensive care,” which leads to effective illness management.
The principle of “holistic case management” was not seen in this study because the concept of illness did not include psychosociocultural-spiritual backgrounds. The recorded data in the medical records were only the records of case-handling based on the biomedical problems. Using principles of “holistic care,” meaning, to manage health problems based on each individual's unique and specific background, may increase patients’ satisfaction and, furthermore, health outcomes.[6,7,8]
Physicians also did not think of involving the patients and their family (if nessecary) in clinical decisionmaking. Part of this is due to the high number of patients who need to be served. More context-sensitive cultural communication skills should be taught optimally.[21]
The principle of “community-oriented case management” in primary care was also lacking. The current primary care system seems to separate public health education from individual/personal empowerment. Individual patient education was very limited in posing a problem for patient self-management. With the growing rate of noncommunicable diseases within the community, self-management is a key element of patient care. Primary health care facilities only carried out public health programs as dictated by the central government, without confirming that any particular program was relevant to a particular area.[15]
Physicians in this study described themselves as waiting for an opportunity to continue with further education or a specialization. Specialization in family medicine, which has seven principles of case management in primary care, was not yet established in Indonesia when this study was done. Other hospital specializations do exist. Physicians working in primary care who have improved their abilities considerably and have managed their patients for several years usually moved to hospital specialization programs. Therefore, the position of a physician in a primary care setting in Indonesia is always filled by newly graduated physicians who have minimal experience and a lack of understanding of the principles of primary health care and who lack adequate supervision by senior primary care physicians. There was limited assurance of a viable career in primary care and a vaccuum of continuing medical education relevant to primary care services. In addition, facilities and infrastructure for primary care clinics, such as buildings, equipment, transportation, emergency facilities, logistical needs, and drugs should be available continuously in primary care to support the diagnostic and treatment processes.
It is interesting to note that the data from study setting 4 showed that physicians were slightly more independent than those in other research areas. This result showed the commitment of a local government to support the employment of a qualified practitioner in the primary care setting.
Ideally, the culture of service in primary care settings is typically different from that in hospital settings. The culture of prevention and curing of diseases in primary care depends on the role of the individual, the family, and their immediate communities. The skills to seek the empowerment of a patient's family and the surrounding environment need to be mastered by physicians working in primary care. The entity of healthy society should continuously receive prevention and promotion services, as the principles of family medicine set out.
Future directions of this study includes identification of details of the factors that contributed to better primary care services, as found in study setting 4. Piloting graduate programs in family medicine and evaluating their impact on the patient care services will make for an interesting study, which will be challenging and require much support from many stakeholders.
Conclusions
Strengthening primary care services should be a priority of all nations, especially in highly populated countries such as Indonesia. Several steps could be taken by providing a more structured and formal graduate education with family medicine principles that emphasize person-centered care, family participation, collaborative care between health care teams, continuous and intensive relationship with the health providers, and community-oriented care. On top of that, commitment from the government to provide facilities to support diagnostic and treatment in primary care settings as part of the national obligation to recognize the role of high-quality primary care physicians as gatekeepers, is essential. Through these efforts, high-quality primary health care services for the people can be accomplished.
Acknowledgment
Our great appreciation and respect to all physicians working in primary care in this study for their participation and dedication to continue their work to serve the community. Our great honor to Professor Soenarto Sastrowijoto, the promoter of Dr. Istionos’ PhD study who provides continuing supports for all authors in the Department of Family and Community Medicine UGM, in striving for better primary care services and education in Indonesia. Thank you for Prof. Ali Ghufron Mukti for his encouragement to complete this study. Many thanks to Dr. Fitriana Nurjannah, Dr. Ria Drupadi, Dr. Vincentius Budhiyanto and Hanum Nurmala BSc. Nutr. for their big helps in organizing the data from different regions of Indonesia.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Geneva: World Health Organization (WHO); 2008. World Health Organization. Primary Health Care is Now More than Ever. [Google Scholar]
- 2.Alma Ata: World Health Organization; 1978. World Health Organization. International Conference on Primary Health Care 6-12th September. [Google Scholar]
- 3.Starfield B. Is primary care essential? Lancet. 1994;344:1129–33. doi: 10.1016/s0140-6736(94)90634-3. [DOI] [PubMed] [Google Scholar]
- 4.Grol R. Nijmegen: Radboud University Nijmegen Medical Centre; 2006. Quality Development of Primary Care in the Netherlands. [Google Scholar]
- 5.Green LA, Fryer GE, Jr, Yawn BP, Lanier D, Dovey SM. The ecology of medical care revisited. N Engl J Med. 2001;344:2021–5. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- 6.Europe: WONCA-Europe; 2005. European Academy of Teachers in General Practice (EURACT). The European Definition of General Practice/Family Medicine. [Google Scholar]
- 7.Kidd M. 2nd ed. New Zealand: WONCA Family Doctors Association; 2013. The Contribution of Family Medicine to Improving Health Systems: A Guidebook from the World Organization of Family Physicians. [Google Scholar]
- 8.Claramita M, Sutomo AH, Graber MA, Scherpbier AJ. Are patient-centered care values as reflected in teaching scenarios really being taught when implemented by teaching faculty? A discourse analysis on an Indonesian medical school's curriculum. Asia Pac Fam Med. 2011;10:4. doi: 10.1186/1447-056X-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chongsusivatwong V, Phua KH, Yap MT, Pocock NS, Hashim JH, Chhem R, et al. Health and health-care systems in southeast Asia: Diversity and transitions. Lancet. 2011;377:429–37. doi: 10.1016/S0140-6736(10)61507-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi L, Starfield B, Jiahong X. Validating the adult primary care assessment tool. J Fam Pract. 2001;50:161–75. [Google Scholar]
- 11.Jakarta: Ministry of Health; 2014. Ministry of Health Republic of Indonesia. Data and Information 2013 (Profile of Indonesian Health Status) [Google Scholar]
- 12.Ministry of Health Republic of Indonesia. Maternal Health. [Last accessed on 2014 Jan 10]. Available from: http://www.kesehatanibu.depkes.go.id/archives/7652014 .
- 13.Jakarta: Indonesian Medical Council (IMC); Indonesian Medical Council. Indonesian Standard of Physicians Competence (ISPC) 2006 renewed in 2012. [Google Scholar]
- 14.Kak N, Burkhalter B, Cooper MA. Vol. 2. Bethesda, MD: U.S. Agency for International Development (USAID) by the Quality Assurance (QA) Project; 2001. Measuring the competence of health care providers. In: Operations Research Issue Paper; pp. 1–28. [Google Scholar]
- 15.Istiono W. Yogyakarta: UGM; 2011. Case Study of Physicians’ Ability in Managing Primary Care Health Problems in the North of Sulawesi Island, Based on ISPC, 2006. [Google Scholar]
- 16.Jakarta: National Body of Statistic (NBC); 2014. National Body of Statistic (NBC). National Economic Survey of Indonesia. [Google Scholar]
- 17.World Bank and United Nation Sources. 2014. Available from: http://www. data.worldbank.org/indicator/ Most Populated Countries.
- 18.Yin RK. Thousands Oaks, CA: Sage Publications; 2003. Case Study Research: Design and Methods. [Google Scholar]
- 19.National Act Republic Indonesia No. 1. Body of National Health Insurance. 2012 [Google Scholar]
- 20.National Act Republic of Indonesia No. 20. Medical Education (Family Medicine Specialists) 2013 [Google Scholar]
- 21.Claramita M, Nugraheni MD, van Dalen J, van der Vleuten C. Doctor-patient communication in Southeast Asia: A different culture? Adv Health Sci Educ. 2012;18:15–31. doi: 10.1007/s10459-012-9352-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


