Abstract
Background
Inadequate access to breast reconstruction was a motivating factor underlying passage of the Women’s Health and Cancer Rights Act. It remains unclear whether all patients interested in breast reconstruction undergo this procedure. The aim of this study was to determine whether geographic disparities are present that limit the rate and method of postmastectomy reconstruction.
Methods
Travel distance in miles between the patient’s residence and the hospital reporting the case was used as a quantitative measure of geographic disparities. The American College of Surgeons National Cancer Database was queried for mastectomy with or without reconstruction performed from 1998 to 2011. Reconstructive procedures were categorized as implant or autologous techniques. Standard statistical tests including linear regression were performed.
Results
Patients who underwent breast reconstruction had to travel farther than those who had mastectomy alone (p < 0.01). A linear correlation was demonstrated between travel distance and reconstruction rates (p < 0.01). The mean distances traveled by patients who underwent reconstruction at community, comprehensive community, or academic programs were 10.3, 19.9, and 26.2 miles, respectively (p < 0.01). Reconstruction rates were significantly greater at academic programs. Patients traveled farther to undergo autologous compared with prosthetic reconstruction.
Conclusions
Although greater patient awareness and insurance coverage have contributed to increased breast reconstruction rates in the United States, the presence of geographic barriers suggests an unmet need. Academic programs have the greatest reconstruction rates, but are located farther from patients’ residences. Increasing the number of plastics surgeons, especially in community centers, would be one method of addressing this inequality.
Access to health care is a major source of outcomes variation among populations.1 Inadequate access to breast reconstruction was a motivating factor underlying passage of the Women’s Health and Cancer Rights Act in 1998, which mandated all-payer coverage for postmastectomy reconstruction.2 Although passage of this law represented progress, additional legislation was needed to ensure that patients were aware of this health insurance benefit. For example, New York State passed legislation requiring surgeons to discuss the availability of breast reconstruction with patients before mastectomy, provide information about insurance coverage and, if necessary, refer them to a hospital where reconstruction is available.3 Ratification of such laws may be one reason immediate breast reconstruction rates rose in the United States from 20.8 percent to 37.8 percent between 1998 and 2008.4 Despite these improvements, it is unclear whether all patients interested in breast reconstruction are aware of or undergo this procedure.
The impact of disparities, such as race and insurance type, on access to services such as breast reconstruction has been documented.5–9 Geography is an additional barrier10 evaluated to a lesser extent. Geographic disparities within breast reconstruction may arise from regional differences in plastic surgeon density. In addition, greater numbers of autologous transfers are now being performed in a limited number of centers (i.e., market concentration), potentially restricting patient access to this method of reconstruction.11 The impact of geography on the method of breast reconstruction (i.e., implants versus autologous tissue) has not been specifically evaluated.
Travel distance serves as a quantitative measurement to assess the presence of geographic disparities. The aim of this study is to determine whether travel distance influences the rate and method of breast reconstruction services. The primary hypothesis is that a greater travel distance to undergo reconstruction is necessary compared with mastectomy alone. The secondary hypothesis is that a greater travel distance is needed for autologous than for prosthetic reconstruction because of a recent market concentration for these procedures.12
PATIENTS AND METHODS
An analysis of travel distance for women undergoing mastectomies for breast cancer was performed using the National Cancer Database. The National Cancer Database is a joint project of the Commission on Cancer of the American College of Surgeons and the American Cancer Society that collects information from more than 1500 Commission on Cancer–accredited facilities in the United States and Puerto Rico. These data represent approximately 70 percent of new cancer diagnoses nationwide. Approval was obtained from the Commission on Cancer’s review board.
Patients were included in the study if they underwent a unilateral or bilateral mastectomy with or without reconstruction for breast cancer from 1998 to 2011. Surgical procedures were recorded in the National Cancer Database using specific codes for mastectomy alone and mastectomy with immediate reconstruction. Reconstructive procedures were categorized as implant-based reconstruction or autologous techniques. For analysis of travel distance by specific method of reconstruction, combined (e.g., latissimus flap with an implant) and unspecified reconstructions were excluded.
The variable of interest was travel distance, which is recorded in the National Cancer Database as “great circle distance.” The great circle distance measures the distance in miles between the patient’s residence and the hospital that reported the case. The patient’s residence latitude and longitude were based on the patient’s zip code or on the city if the zip code was not available. Hospital locations were based on the street address. A distance of 0 can result when the patient lives in the same zip code where the facility is located.13 The mean travel distance by patients who underwent mastectomies with and without reconstruction, and with different method of reconstruction, was compared using the t test and the Mann-Whitney U test as needed. Trends in travel distance over time were analyzed with Poisson regression and expressed as the annual mean changes in rates over time (incidence rate ratio). A value of p < 0.05 was considered significant.
To analyze whether there was a relationship between travel distance and immediate breast reconstruction, a linear regression was performed. This relationship was also analyzed for the different types of cancer programs (community, comprehensive community, and academic comprehensive cancer program). All Commission on Cancer–accredited cancer programs provide a full range of diagnostic and therapeutic services on site or by referral, participate in research activities, but differ in residency training and number of new cancer cases diagnosed each year. Community cancer programs provide care to 100 to 500 new cancer diagnoses per year, and residency training is optional. Comprehensive community cancer programs take care of more than 500 new cases per year, and residency training is also optional. Academic comprehensive cancer programs are those with at least 500 new cancer diagnoses every year and provide postgraduate medical education in at least four program areas, including internal medicine and general surgery.14
High-volume autologous centers were defined as those performing more than 45 cases per year, as defined by previous research.15 These trends were analyzed with Poisson regression. All statistical analyses were performed using Stata 11.0 (StataCorp, College Station, Texas).
RESULTS
A total of 1,031,343 patients were included. Table 1 demonstrates trends in immediate reconstruction rates and method as recorded in the National Cancer Database. The immediate reconstruction rate increased from 10.6 percent to 32.2 percent from 1998 to 2011. Autologous reconstructions increased from 44.3 per 1000 to 98.9 per 1000 mastectomies, whereas implant-based reconstructions increased at a greater rate, from 22.3 per 1000 to 113.3 per 1000 mastectomies.
Table 1.
Reconstruction Rates from 1998 to 2011
| Year | No. of Mastectomies |
No. of Immediate Breast Reconstructions |
Immediate Reconstruction Rate (%) |
Autologous Rate (per 1000 mastectomies) |
Implant Rate (per 1000 mastectomies) |
|---|---|---|---|---|---|
| 1998 | 74,593 | 7895 | 10.6 | 44.3 | 22.3 |
| 1999 | 74,802 | 10,333 | 13.8 | 57.2 | 28.4 |
| 2000 | 72,997 | 10,973 | 15.0 | 59.9 | 32.6 |
| 2001 | 73,023 | 11,570 | 15.8 | 60.9 | 35.5 |
| 2002 | 70,488 | 11,046 | 15.7 | 57.6 | 34.6 |
| 2003 | 65,554 | 10,432 | 15.9 | 54.9 | 41.3 |
| 2004 | 65,398 | 11,132 | 17.0 | 57.4 | 47.9 |
| 2005 | 65,881 | 11,866 | 18.0 | 62.4 | 53.0 |
| 2006 | 69,189 | 13,516 | 19.5 | 65.5 | 56.6 |
| 2007 | 75,074 | 16,866 | 22.5 | 72.3 | 70.0 |
| 2008 | 79,913 | 19,992 | 25.0 | 78.9 | 84.5 |
| 2009 | 83,611 | 23,756 | 28.4 | 88.3 | 100.4 |
| 2010 | 80,777 | 24,309 | 30.1 | 90.3 | 105.4 |
| 2011 | 80,043 | 25,741 | 32.2 | 98.9 | 113.3 |
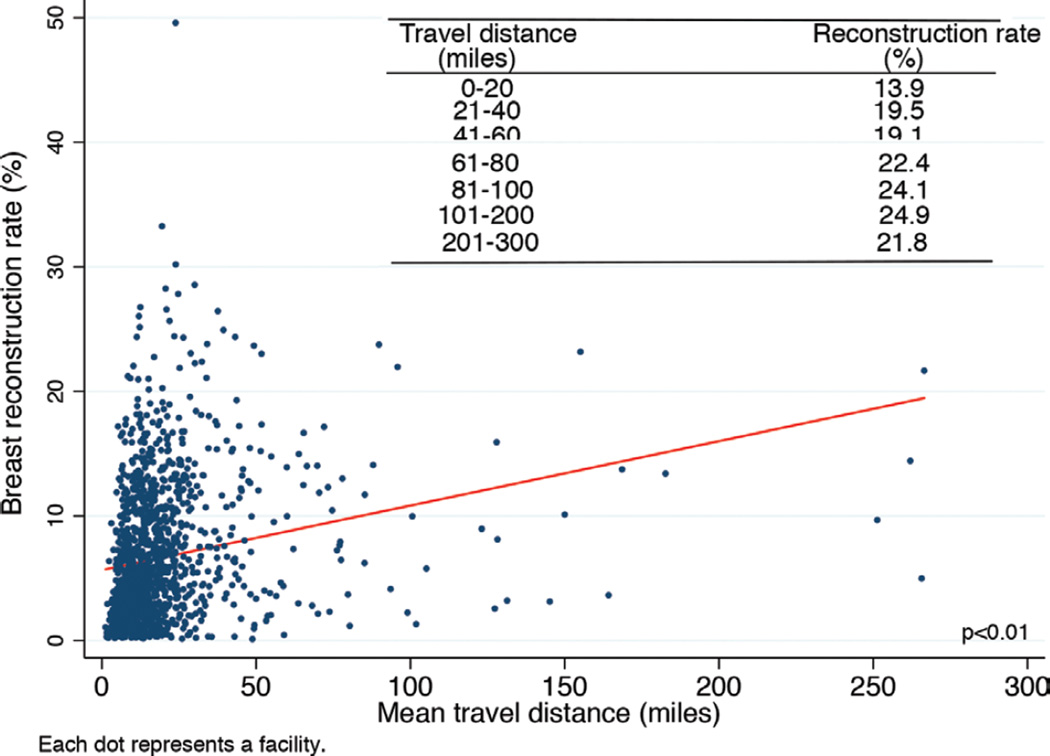
Table 2 shows that patients who underwent mastectomy with immediate reconstruction had to travel significantly greater distances than patients who did not undergo reconstruction (p < 0.01). Furthermore, the mean travel distance for patients with immediate reconstruction increased at a rate of 2 percent per year, from 26.3 miles in 1998 to 34.0 miles in 2011 (p = 0.04), whereas the mean travel distance for patients with mastectomy alone was unchanged (incidence rate ratio, 1.00; p = not significant). Figure 1 illustrates a positive linear correlation between travel distance and immediate reconstruction rates: a patient who travels 0 to 20 miles from her home zip code undergoes reconstruction at rate of 13.9 percent, whereas one who travels 201 to 300 miles undergoes reconstruction at a rate of 21.8 percent.
Table 2.
Travel Distance for Mastectomy with and without Reconstruction
| Year | Mastectomy without Reconstruction (miles) |
Mastectomy with Reconstruction (miles) |
|---|---|---|
| Mean* | 25.8 | 31.3 |
| 1998 | 25.2 | 26.3 |
| 1999 | 25.0 | 24.7 |
| 2000 | 25.0 | 29.2 |
| 2001 | 25.3 | 28.9 |
| 2002 | 24.2 | 26.5 |
| 2003 | 25.4 | 29.3 |
| 2004 | 26.1 | 32.0 |
| 2005 | 24.7 | 34.3 |
| 2006 | 25.9 | 32.0 |
| 2007 | 27.3 | 37.9 |
| 2008 | 26.9 | 33.0 |
| 2009 | 26.6 | 35.1 |
| 2010 | 25.6 | 33.0 |
| 2011 | 27.1 | 34.0 |
| IRR | 1.00† | 1.02‡ |
IRR, incidence rate ratio.
p < 0.01.
p = not significant.
p = 0.04.
Fig. 1.
Travel distance for immediate breast reconstruction.
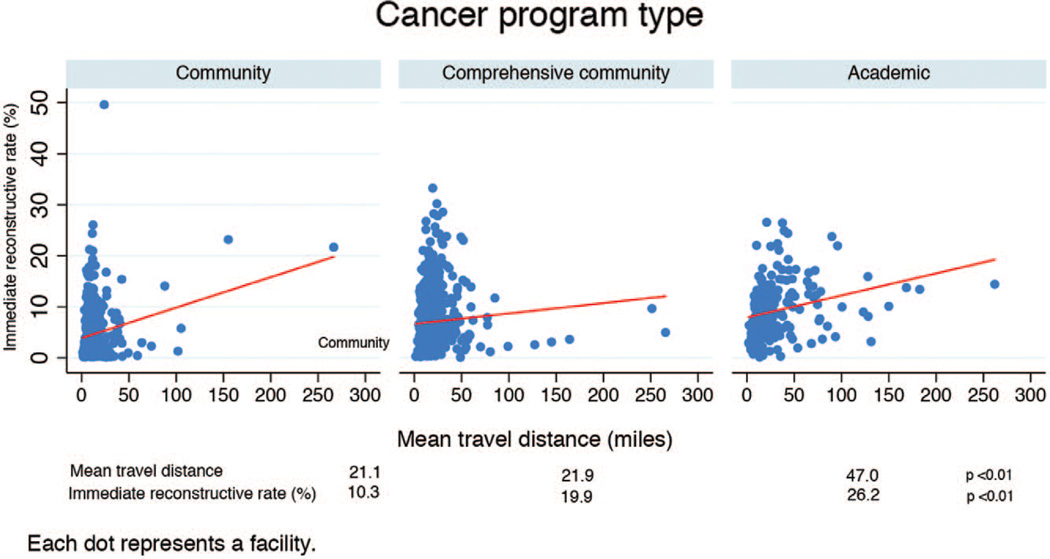
Figure 2 shows the relationship between travel distance and immediate reconstruction rate by cancer program type. The mean distances traveled by patients who received care at community, comprehensive community, or academic programs were 21.1, 21.9, and 47.0 miles, respectively (p < 0.01). Similarly, reconstruction rates increased from 10.3 percent in community, to 19.9 percent in comprehensive community, and to 26.2 percent in academic programs (p < 0.01).
Fig. 2.
Immediate reconstruction rates and travel distance by cancer program type.
Table 3 shows travel distance by method of reconstruction. The mean distance traveled by patients who underwent autologous reconstruction was greater than the distance traveled by patients who underwent immediate implant-based reconstruction (p < 0.01). The mean travel distance for both types of procedures increased significantly at a rate of 2 percent per year.
Table 3.
Travel Distance for Method of Reconstruction
| Year | Autologous (miles) | Implant (miles) |
|---|---|---|
| Mean* | 34.0 | 32.0 |
| 1998 | 30.1 | 18.9 |
| 1999 | 26.7 | 21.6 |
| 2000 | 24.0 | 34.9 |
| 2001 | 32.8 | 29.0 |
| 2002 | 27.6 | 25.6 |
| 2003 | 34.4 | 29.6 |
| 2004 | 37.7 | 27.4 |
| 2005 | 38.8 | 34.7 |
| 2006 | 29.5 | 35.9 |
| 2007 | 38.9 | 37.9 |
| 2008 | 32.5 | 29.0 |
| 2009 | 37.5 | 31.5 |
| 2010 | 35.2 | 34.4 |
| 2011 | 36.8 | 33.6 |
| IRR | 1.02† | 1.02‡ |
IRR, incidence rate ratio.
p < 0.01.
p < 0.05.
p = 0.01.
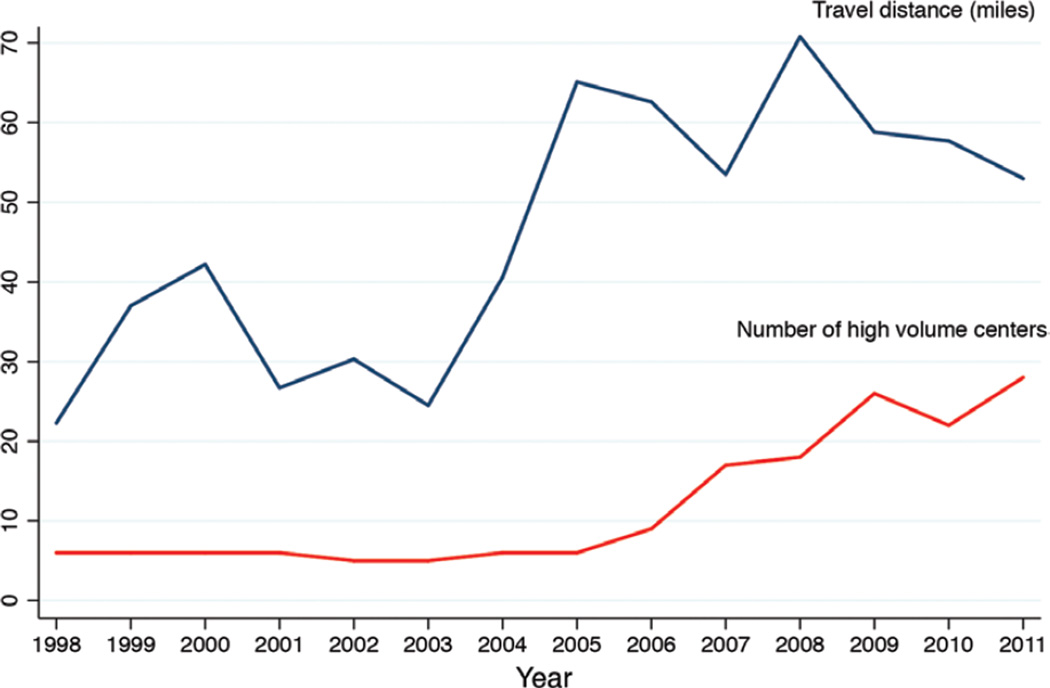
Trends for mean travel distance to high-volume autologous centers are shown in Figure 3. Although the number of high-volume centers increased significantly from six to 28 in 1998 and 2011, respectively (p < 0.01), the mean distance traveled by patients receiving treatment at these centers also increased from 22.3 miles to 53 miles (p < 0.01). The average number of procedures performed by high-volume autologous centers did not change significantly over the study period (p = not significant) (data not shown).
Fig. 3.
Travel distance for high-volume autologous centers.
DISCUSSION
Because unequal access is a major source of health outcome variation, it is a target of many initiatives within the Affordable Care Act.16 Geography affects not only people’s ability to obtain health care services but also the quality of those services.17 For example, high-volume centers are associated with lower complication rates but are often located in metropolitan centers, resulting in increased travel distance for patients residing in rural areas.15,18 Greater travel distance creates both direct (e.g., commute cost) and indirect (e.g., time, foregone wages) economic barriers, thereby restricting health care options for many patients.19 The premise of the current report was to use travel distance as a proxy for measuring the influence of geographic barriers on breast reconstruction rates and methods.
The greater distance traveled by women undergoing breast reconstruction, compared with mastectomy without reconstruction, suggests the presence of a geographic disparity (Table 2). Ideally, women should not have to travel farther to undergo breast reconstruction. Furthermore, a direct relationship was observed between travel distance and reconstruction rate. A woman who traveled 0 to 20 miles from her home zip code underwent reconstruction at a rate of 13.9 percent, whereas those who traveled 100 to 200 miles underwent reconstruction at a rate of 24.9 percent (Fig. 1). Similar findings have been observed in Canada, where universal health coverage is provided. Women who underwent post-mastectomy breast reconstruction traveled farther from their residence to the hospital compared with those undergoing mastectomy alone.20 An undersupply of reconstructive surgeons was posited as an explanation; however, factors such as specific referral patterns and patient preference were also suggested. Within the United States, it has been shown that the number of plastic surgeons at an institution correlates with the likelihood for post-mastectomy reconstruction.21 Considered together, these findings suggest that the Women’s Health and Cancer Rights Act and individual mandate for insurance coverage under the Affordable Care Act will be insufficient to eliminate all access issues to breast reconstruction. Training greater numbers of plastic surgeons who could diffuse into less saturated communities would be one method of addressing this issue.
A second important observation was that the distance traveled for breast reconstruction has increased over time, whereas it is unchanged for those who do not undergo reconstruction. Since 1998, the distance traveled by women who underwent breast reconstruction increased by 2 percent each year (p = 0.04) (Table 2). A variety of factors may contribute to this trend. Although the overall rate of breast reconstruction is increasing nationwide, plastic surgeons who perform these procedures may be saturated geographically, requiring patients to seek care at a greater distance. It is estimated that by 2020 there will be a significant shortage of plastic surgeons because of the growing U.S. population, a significant number of retiring surgeons, and a fixed number of training positions.22 Alternatively, the number of plastic surgeons performing breast reconstruction may be decreasing because of falling reimbursement rates, particularly for autologous breast reconstruction.23 Lastly, although microsurgical breast reconstruction was not specifically measured in this study, it creates a number of barriers that may negatively impact the ability to perform these procedures widely. Not only is specialized training necessary to perform microsurgery techniques, it is also commonly performed in urban academic centers where residents are available.11,24
The type of institution where a woman received care was observed to impact her rate of reconstruction, creating the observed geographic disparity. For example, women treated at academic centers needed to travel more than double the distance than those who received care at community or comprehensive community hospitals, but underwent reconstruction at the highest rates (Fig. 2) (p < 0.01). Although other studies have shown the association between academic centers and reconstruction rates, none has demonstrated travel distance as a factor.25 Academic centers provide subspecialty care, which may affect referral patterns, and also possess extra resources, including residents, skilled nursing staff, and financial incentives, which may promote reconstruction.11,21,23,24,26–28 Alternatively, women may choose academic centers because of their reputation, prestige, or research notoriety.
A secondary aim of the current study was to determine whether the distance traveled by patients to undergo autologous reconstruction was greater than that for implant reconstruction. When travel distance was dichotomized by method of reconstruction (Table 3), the average distance to undergo autologous reconstruction was greater than that for prosthetic techniques. Moreover, the distance traveled for autologous reconstruction was greater than for implants in 12 of the 14 years evaluated. Whereas autologous transfer used to be the most common method, implants are now the predominant method of breast reconstruction.12 Furthermore, with widespread adoption of perforator flaps, autologous reconstruction has become increasingly specialized, requiring advanced training and more resources, including but not limited to microscopes, flap monitoring devices, and specially trained nursing staff.24 The greater impact of these changes to the health care system has been a smaller number of hospitals providing this service, with the downstream effect of increased travel distance for the patient.4
Recent evidence of a market concentration of autologous reconstructions to high-volume centers led us to question whether this created an inadvertent barrier.12 Figure 3 demonstrates a simultaneous increase in the number of high-volume centers and the distance traveled for patients to reach them. Although the proliferation of high-volume centers could be interpreted in a positive light because of their association with favorable outcomes,18 reconstruction needs to be offered widely because of the prevalence of breast cancer.15 Thus, a shift to high-volume centers can create a bottleneck that limits access to care. The Centers for Medicare & Medicaid Services restricted coverage of Medicare patients undergoing bariatric surgery to Centers of Excellence in 2006, hoping to improve outcomes.29 Not only were outcomes unchanged,30 there was a decline in nonwhite Medicare patients undergoing weight-loss surgery.31 The policy was subsequently reversed in 2013.32
Although the study provides important insights, it has limitations. The National Cancer Database was chosen because it is the only database that contains information on the unique variable of travel distance. Although some of the absolute values reported in this study differ from previous large database studies, the long-term data trends are congruent (e.g., implant reconstructions have surpassed autologous reconstructions as the most common method of U.S. breast reconstruction).12 Moreover, the fidelity of national databases has been shown to correlate with individual centers.33 Unfortunately, the National Cancer Database does not allow for assessment of outcomes such as complications or patient satisfaction. This is important because greater travel distance could impact quality as well. Although in most cases greater travel distance can be interpreted as a geographic disparity, there may be instances when a woman chooses to seek care at a greater distance for a particular surgeon or academic medical center. Finally, the National Cancer Database differentiates reconstruction as tissue or prosthetic based, but does not report specific methods of autologous transfer. The investigation of microsurgery would likely show greater travel distance for these highly technical procedures.
CONCLUSIONS
Surgeons should be aware of an ongoing unmet need for breast reconstruction in the United States. Although greater patient awareness and insurance coverage have contributed to increased breast reconstruction rates in the United States, geographic barriers to access this service remain, particularly with regard to academic centers. Greater numbers of plastics surgeons, especially in community centers, would be one method of addressing this inequality.
Acknowledgments
The data used in the study are derived from a deidentified National Cancer Database file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology used, or the conclusions drawn from these data by the investigator.
No specific funding was used for this research.
Footnotes
Disclosure: The authors have no financial to declare in relation to the content of this article.
REFERENCES
- 1.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7:186–188. doi: 10.1258/135581902760082517. [DOI] [PubMed] [Google Scholar]
- 2.Women’s Health and Cancer Rights Act of 1998. Available at: http://www.cms.gov/Regulations-and-Guidance/Health-Insurance-Reform/HealthInsReformforConsume/downloads/WHCRA_Statute.pdf. Accessed.
- 3.Lentol J. Information and Access to Breast Reconstructive Surgery Law. Committee on Codes. Chapter 354; Health. A.10094-B/S.6993-B. Available at: http://assembly.state.ny.us/comm/Codes/2010Annual/index.pdf. Accessed. [Google Scholar]
- 4.Albornoz CR, Bach PB, Pusic AL, et al. The influence of sociodemographic factors and hospital characteristics on the method of breast reconstruction, including microsurgery: A U.S. population-based study. Plast Reconstr Surg. 2012;129:1071–1079. doi: 10.1097/PRS.0b013e31824a29c5. [DOI] [PubMed] [Google Scholar]
- 5.Shippee TP, Kozhimannil KB, Rowan K, Virnig BA. Health insurance coverage and racial disparities in breast reconstruction after mastectomy. Womens Health Issues. 2014;24:e261–e269. doi: 10.1016/j.whi.2014.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrow M, Li Y, Alderman AK, et al. Access to breast reconstruction after mastectomy and patient perspectives on reconstruction decision making. JAMA Surg. 2014;149:1015–1021. doi: 10.1001/jamasurg.2014.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruper L, Holt A, Xu XX, et al. Disparities in reconstruction rates after mastectomy: Patterns of care and factors associated with the use of breast reconstruction in Southern California. Ann Surg Oncol. 2011;18:2158–2165. doi: 10.1245/s10434-011-1580-z. [DOI] [PubMed] [Google Scholar]
- 8.Rosson GD, Singh NK, Ahuja N, Jacobs LK, Chang DC. Multilevel analysis of the impact of community vs patient factors on access to immediate breast reconstruction following mastectomy in Maryland. Arch Surg. 2008;143:1076–1081. doi: 10.1001/archsurg.143.11.1076. discussion 1081. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan CP, Karliner LS, Hwang ES, et al. The effect of system-level access factors on receipt of reconstruction among Latina and white women with DCIS. Breast Cancer Res Treat. 2011;129:909–917. doi: 10.1007/s10549-011-1524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliver A, Mossialos E. Equity of access to health care: Outlining the foundations for action. J Epidemiol Community Health. 2004;58:655–658. doi: 10.1136/jech.2003.017731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Albornoz CR, Cordeiro PG, Mehrara BJ, et al. Economic implications of recent trends in U.S. immediate autologous breast reconstruction. Plast Reconstr Surg. 2014;133:463–470. doi: 10.1097/PRS.0000000000000039. [DOI] [PubMed] [Google Scholar]
- 12.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: Increasing implant rates. Plast Reconstr Surg. 2013;131:15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 13.American College of Surgeons. Great circle distance. [Accessed February 12, 2015]; Available at: http://ncdbpuf.facs.org/?q=node/305. [Google Scholar]
- 14.American College of Surgeons. CoC accreditation categories. [Accessed February 2, 2015]; Available at: https://www.facs.org/quality-programs/cancer/accredited/about/categories. [Google Scholar]
- 15.Albornoz CR, Cordeiro PG, Hishon L, et al. A nationwide analysis of the relationship between hospital volume and outcome for autologous breast reconstruction. Plast Reconstr Surg. 2013;132:192e–200e. doi: 10.1097/PRS.0b013e31829586c1. [DOI] [PubMed] [Google Scholar]
- 16.Kocher R, Emanuel EJ, DeParle NA. The Affordable Care Act and the future of clinical medicine: The opportunities and challenges. Ann Intern Med. 2010;153:536–539. doi: 10.7326/0003-4819-153-8-201010190-00274. [DOI] [PubMed] [Google Scholar]
- 17.Radley DC, Schoen C. Geographic variation in access to care: The relationship with quality. N Engl J Med. 2012;367:3–6. doi: 10.1056/NEJMp1204516. [DOI] [PubMed] [Google Scholar]
- 18.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 19.Mooney GH. Equity in health care: Confronting the confusion. Eff Health Care. 1983;1:179–185. [PubMed] [Google Scholar]
- 20.Zhong T, Fernandes KA, Saskin R, et al. Barriers to immediate breast reconstruction in the Canadian universal health care system. J Clin Oncol. 2014;32:2133–2141. doi: 10.1200/JCO.2013.53.0774. [DOI] [PubMed] [Google Scholar]
- 21.Greenberg CC, Lipsitz SR, Hughes ME, et al. Institutional variation in the surgical treatment of breast cancer: A study of the NCCN. Ann Surg. 2011;254:339–345. doi: 10.1097/SLA.0b013e3182263bb0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rohrich RJ, McG rath MH, Lawrenc WT, Ahmad J American Society of Plastic Surgeons Plastic Surgery Workforce Task Force. Assessing the plastic surgery workforce: A template for the future of plastic surgery. Plast Reconstr Surg. 2010;125:736–746. doi: 10.1097/PRS.0b013e3181c830ec. [DOI] [PubMed] [Google Scholar]
- 23.Alderman AK, Atisha D, Streu R, et al. Patterns and correlates of postmastectomy breast reconstruction by U.S. plastic surgeons: Results from a national survey. Plast Reconstr Surg. 2011;127:1796–1803. doi: 10.1097/PRS.0b013e31820cf183. [DOI] [PubMed] [Google Scholar]
- 24.Kulkarni AR, Sears ED, Atisha DM, Alderman AK. Use of autologous and microsurgical breast reconstruction by U.S. plastic surgeons. Plast Reconstr Surg. 2013;132:534–541. doi: 10.1097/PRS.0b013e31829ae03e. [DOI] [PubMed] [Google Scholar]
- 25.Brennan ME, Spillane AJ. Uptake and predictors of post-mastectomy reconstruction in women with breast malignancy: Systematic review. Eur J Surg Oncol. 2013;39:527–541. doi: 10.1016/j.ejso.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 26.Habermann EB, Thomsen KM, Hieken TJ, Boughey JC. Impact of availability of immediate breast reconstruction on bilateral mastectomy rates for breast cancer across the United States: Data from the nationwide inpatient sample. Ann Surg Oncol. 2014;21:3290–3296. doi: 10.1245/s10434-014-3924-y. [DOI] [PubMed] [Google Scholar]
- 27.Alderman AK, Storey AF, Nair NS, Chung KC. Financial impact of breast reconstruction on an academic surgical practice. Plast Reconstr Surg. 2009;123:1408–1413. doi: 10.1097/PRS.0b013e3181a0722d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yueh JH, Slavin SA, Bar-Meir ED, et al. Impact of regional referral centers for microsurgical breast reconstruction: The New England perforator flap program experience. J Am Coll Surg. 2009;208:246–254. doi: 10.1016/j.jamcollsurg.2008.10.033. [DOI] [PubMed] [Google Scholar]
- 29.Pratt GM, McLees B, Pories WJ. The ASBS Bariatric Surgery Centers of Excellence program: A blueprint for quality improvement. Surg Obes Relat Dis. 2006;2:497–503. doi: 10.1016/j.soard.2006.07.004. discussion 503. [DOI] [PubMed] [Google Scholar]
- 30.Dimick JB, Nicholas LH, Ryan AM, Thumma JR, Birkmeyer JD. Bariatric surgery complications before vs after implementation of a national policy restricting coverage to centers of excellence. JAMA. 2013;309:792–799. doi: 10.1001/jama.2013.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicholas LH, Dimick JB. Bariatric surgery in minority patients before and after implementation of a centers of excellence program. JAMA. 2013;310:1399–1400. doi: 10.1001/jama.2013.277915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacques L, Syrek Jenson T, Schafer J, Paserchia L, O’Connor D. Reconsideration of Facility Certification Requirement for Coverage of Covered Bariatric Surgery Procedures (Memorandum) Centers for Medicare and Medicaid Services; 2013. Jun 23, Decision memorandum for CAG #00250R3. [Google Scholar]
- 33.Jagsi R, Jiang J, Momoh AO, et al. Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol. 2014;32:919–926. doi: 10.1200/JCO.2013.52.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]