Abstract
Long-term objectives associated with cancer survivors have been suggested by Healthy People 2020, including increasing the proportion of survivors living beyond 5 years after diagnosis and improving survivors’ mental and physical health-related quality of life. Prior to reaching these objectives, several intermediate steps must be taken to improve the physical, social, emotional, and financial well-being of cancer survivors. Public health has a role in developing strategic, actionable, and measurable approaches to facilitate change at multiple levels to improve the lives of survivors and their families. The social ecological model has been used by the public health community as the foundation of multilevel intervention design and implementation, encouraging researchers and practitioners to explore methods that promote internal and external changes at the individual, interpersonal, organizational, community, and policy levels. The survivorship community, including public health professionals, providers, policymakers, survivors, advocates, and caregivers, must work collaboratively to identify, develop, and implement interventions that benefit cancer survivors. The National Action Plan for Cancer Survivorship highlights public health domains and associated strategies that can be the impetus for collaboration between and among the levels in the social ecological model and are integral to improving survivor outcomes. This paper describes the Public Health Action Model for Cancer Survivorship, an integrative framework that combines the National Action Plan for Cancer Survivorship with the social ecological model to demonstrate how interaction among the various levels may promote better outcomes for survivors.
Introduction
Healthy People 2020 Objectives for Cancer Survivorship
The definition of a cancer survivor includes individuals from the point of a cancer diagnosis throughout the reminder of their life. 1 In the U.S., there are nearly 14 million cancer survivors,2 many of whom face health-related quality of life (QOL) concerns (physical, emotional, psychosocial, spiritual, and financial) associated with their diagnosis and subsequent treatment.3,4 In order to address these concerns and realize improvements in their overall health, Healthy People 2020 (HP 2020) has set two objectives related to cancer survivors. HP 2020 objective C-13 aims to increase the percent of cancer survivors living 5 years or longer after diagnosis.5 HP 2020 objective C-14 aims to improve the mental and physical health status among cancer survivors.5 This latter objective is developmental and does not currently have national baseline data. Its inclusion, however, underscores the need to make investments in interventions that improve the QOL of cancer survivors.
Public health has an important role in advancing the nation toward the fulfillment of these objectives and improving the overall health and QOL of cancer survivors. Achieving important intermediate outcomes and more distal objectives will require collaboration between and among survivors, communities, organizations, and policymakers. Key components of public health, such as the use of key partnerships to facilitate the development of strategic, actionable, and measureable approaches to improving the health and QOL of cancer survivors, are also essential to this effort. Although “The Action Model to Achieving HP 2020 Goals” serves as a framework for addressing HP 2020 objectives and achieving desired outcomes through an ecological approach, achieving objectives related to cancer survivors may benefit from additional components specific to public health action and cancer survivorship outcomes.6,7 The current articles describes:
social ecological approaches used to drive public health action in cancer survivorship;
the National Action Plan for Cancer Survivorship (NAPCS), which offers strategies to address the needs of cancer survivors; and
an innovative model, the Public Health Action Model for Cancer Survivorship (PHAM-CS), which combines both the social ecological model (SEM) and NAPCS domains to address HP 2020 cancer survivor objectives.
Social Ecological Approaches to Influence Health
Numerous behavioral, anthropological, and health models have been used as frameworks to drive public health action. The SEM, developed by Bronfrenbrener8 and McLeroy et al.,9 articulates a framework for understanding the reciprocal interrelationships between individual and population-level determinants of behavior. The model describes factors influencing behavior at multiple levels, including the:
individual level, which embodies characteristics of one person’s knowledge, attitudes, behavior, developmental history, demographic characteristics (gender, race/ethnicity, economic status), and health literacy;
interpersonal level, where social networks and support systems include family members, coworkers, and friends;
organizational/institutional level, pertaining to characteristics of social institutions with organizational characteristics and operational rules and regulations;
community level, which involves relationships among organizations, institutions, and informational networks within defined boundaries; and
policy level, which pertains to local, state, national, and global laws and policies.8,9
Adaptations of the SEM have been used by many public health organizations, including CDC, as a framework for facilitating behavior change related to mental and physical health.10 Cancer-specific adaptations of the SEM have also served as a roadmap to multilevel intervention design and implementation by encouraging and supporting change at the individual, interpersonal, organizational, community, and policy levels.11,12 These models have been used to promote cervical13,14 and colorectal cancer screening,15 improve human papillomavirus vaccination uptake,16 and reduce indoor tanning among adolescents17 by enhancing communication, commitment, and collaboration among stakeholders at all levels. To date, however, no model has addressed the unique needs of cancers survivors and supplied a framework for public health action at the multiple levels. The model described here is an innovative attempt at providing a framework to address the public health needs of survivors. This model uses the SEM to acknowledge the complex and multilevel system of influences on the survivor. It also proposes that the NAPCS domains encourage collaborative work across these levels.
Domains for Public Health Action: The National Action Plan for Cancer Survivorship
The NAPCS identifies public health strategies that are positioned to address many of the needs of cancer survivors and their families.3 Ninety-six strategies are grouped into four public health domains: surveillance and applied research; communication, education, and training; programs, policies, and infrastructure; and access to quality care and services, as well as a fifth crosscutting domain to provide an integrated and multi-disciplinary public health roadmap for improving cancer survivorship.3 A recent assessment of organizational implementation of the NAPCS strategies related to these domains demonstrated that these are substantially addressed by some of the nation’s leading public health and cancer survivorship organizations. Some additional areas, however, such as developing clinical guidelines and assuring a quality workforce, require additional attention and reflect strategies more appropriate for organizations that provide clinical service delivery.18 The assessment also found that an increased emphasis on evaluation and translation of research to practice were warranted—a particular strength of public health organizations.18 There is a unique opportunity to integrate the SEM and NAPCS to provide an integrated model for public health action for cancer survivorship that is strategic, comprehensive, actionable, and measurable.
Overview of the Public Health Action Model for Cancer Survivorship
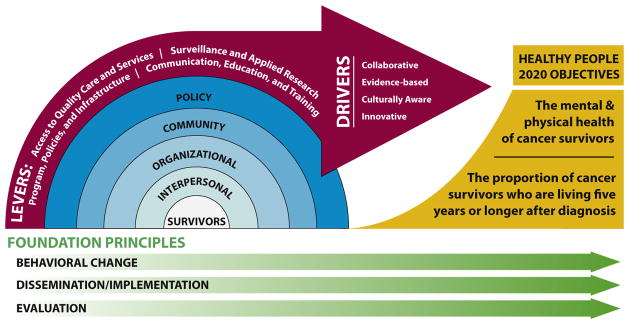
The PHAM-CS represents how the NAPCS strategies can be operationalized to promote collaboration; some strategies include intrapersonal and interpersonal networks of survivors, organizations, community advocacy and programmatic groups, and policymakers (Figure 1). The PHAM-CS was generated using components of adapted SEMs13–16 and was further expanded to include NAPCS-specific levers, drivers, and foundational principles. The inclusion of NAPCS-specific levers, drivers, and foundational principles makes the PHAM-CS uniquely suited to promote systemic collaboration while incorporating actionable strategies to achieve improved mental, physical, social, and financial outcomes among cancer survivors. The domains and strategies in the NAPCS were the result of an iterative process of consensus agreement among more than 100 experts in public health and cancer survivorship.3 CDC developed the PHAM-CS through a deliberative process of a team with expertise in cancer survivorship and public health research, programmatic initiatives, and policy efforts. The PHAM-CS acknowledges the efforts of public health stakeholders at the various levels and provides opportunities to improve quality, outcomes, and potential sustainability of their work.
Figure 1.
Public health action model for cancer survivorship (PHAM-CS).
Major components of the PHAM-CS (Figure 1) illustrate the levels of the SEM at which key stakeholder groups have influence: NAPCS domains that promote action in core public health areas (levers); the importance of collaboration, cultural competence, evidence-based interventions, and innovation in enhancing survivorship initiatives (drivers); and foundational principles that include concepts of behavioral change, evaluation, and dissemination/implementation, which support the other PHAM-CS components.
The levers—NAPCS domains—enable effective implementation of survivorship activities that impact survivors, family, caregivers, providers, and others working at the interpersonal level; health system, insurers, or other organizations addressing the needs of cancer survivors; community organizations such as local affiliates of advocacy organizations, support groups, or community health workers; and state, local, or national policies or guidelines. The levers, representing NAPCS strategies, enable stakeholders working across the SEM to address priority survivorship needs in the major public health domains.
Drivers can enhance the reliability and validity of the approaches being used by individuals working across SEM levels and may maximize PHAM-CS’s effect on intermediate and longer-term outcomes. Collaboration between and among organizations may positively influence and facilitate change at the various levels. Evidence-based methods and programs need to be used and, when appropriate, public health efforts need to be culturally competent to effectively address factors that contribute to differences in survivor outcomes.19 The PHAM-CS illustrates a paradigmatic approach to address the needs of cancer survivors by fully integrating the SEM and the NAPCS domains into a system that acknowledges the importance of collaboration, the use of evidence, cultural competency, and innovation. This system is further optimized through behavioral change, dissemination and implementation, and evaluation.
The first principle, behavioral change (explained by theories of organizational behavior),20,21 may require stakeholders to think globally and inclusively about their work. Behavioral change would require support of an ideology22 that collaboration across disciplines and levels is necessary to facilitate progress in the area of survivor-ship in which these stakeholders (e.g., organizations) are currently working. This foundational principle encourages and challenges stakeholders to think of their work as part of a larger interconnected system. These connections may exist between stakeholders who were not previously identified as usual allies.
The second principle, dissemination and implementation, assumes that the work conducted in this integrative framework will, when appropriate, be designed with the intent to encourage or promote translation into practice.23,24 Specifically, collaborators will support the application of evidence-based interventions. Dissemination and implementation are bidirectional activities—research informs program practice, and program practice helps identify gaps in the knowledge base and spurs the development of a research agenda.23,24 These activities can support efforts to develop programs that are specific for survivors and increase opportunities for sustainability and scalability.23–25
Evaluation, the third foundational principle, requires action to be taken to systematically monitor and collect information on survivorship activities and outcomes.26 These efforts will support program improvement, assess program effectiveness, and aid informed decision making about the future of survivorship activities. The third principle also requires a commitment to establish indicators to monitor process and progress over time.27
Capacity for Public Health Action Model for Cancer Survivorship Implementation
Public health organizations are uniquely positioned to operationalize PHAM-CS. The application of research for the public good is a core function of public health and this goal is exemplified by partnerships with diverse groups of stakeholders at the various SEM levels. One example of the capacity of the public health community to implement PHAM-CS is comprehensive cancer control,28 an integrated approach to addressing the burden of cancer in the U.S. This approach is evident in CDC’s National Comprehensive Cancer Control Program (NCCCP) and the Comprehensive Cancer Control National Partnership, a network of 15 national organizations that provide ongoing support to coalitions that work collaboratively with NCCCP grantees.29 The NCCCP funds all states, the District of Columbia, several tribes and tribal organizations, and U.S. Affiliated Pacific Island jurisdictions to convene a diverse group of stakeholders to form collaborative and comprehensive partnerships with the goal of developing and implementing cancer plans to address issues within their respective geographic areas. Core activities of the NCCCP include use of cancer surveillance data to inform program practice; maintenance of partnerships uniquely positioned to implement the plan; implementation of cancer plan strategies that facilitate policy, system, and environmental changes that promote primary prevention of cancer, facilitate screening and treatment, and address the needs of cancer survivors; and demonstration of outcomes through evaluation.30 The Comprehensive Cancer Control National Partnership also provides technical assistance and training to support partnership building and use of evidence-base strategies to attain goals related to increasing colorectal cancer screening, human papillomavirus vaccinations, and tobacco cessation among cancer survivors.29 NCCCP grantees have coalitions that consist of organizations that work across the SEM levels, and grantees work collaboratively with these organizations to implement survivorship activities that are based on the NAPCS. Recent assessment of these grantees found that 64% included recommended NAPCS strategies in their program action plan.30 The NCCCP’s broad-based partnerships. composed of representatives working across all levels of the SEM,30 current endorsement of NAPCS strategies, and implementation of core activities provide opportunities for this public health program to implement the PHAM-CS.31–33
Another example that highlights the applicability of the PHAM-CS is CDC’s research, program, and media campaign efforts to support initiatives for young breast cancer survivors. CDC convened federal advisory committees comprising a diverse group of stakeholders to address the burden of breast cancer among women diagnosed before age 50 years.34 CDC worked collaboratively with partners to employ activities across all NAPCS domains to develop a research agenda that informs program practice,35 implement programs and media campaigns,36 conduct research and evaluation to inform relevant initiatives,37,38 and lead ongoing evaluations that assess effectiveness.39,40
Operationalizing the Public Health Action Model for Cancer Survivorship and Implications for Use
Full implementation of the PHAM-CS requires organizational behavior change that seeks collaborative relationships with stakeholders working across SEM levels, a commitment to facilitating the translation of research into practice, and organizational support for and emphasis on evaluation. The model encourages individuals, interpersonal networks, organizations, communities, and policymakers across all levels and sectors to focus on the priority public health domains, or levers, and the associated NAPCS strategies. This critical work is best supported in a collaborative environment, which strives to implement activities that are evidence-informed, culturally competent, and innovative.
Activities associated with surveillance offer an instructive example. Those conducting surveillance are encouraged to seek out innovative ways to ensure that data are routinely used to inform research, program practice, service delivery, and policy development. Their activities may be enhanced by establishing partnerships with organizations that work across the SEM levels but may not traditionally partner with organizations that administer surveillance systems.
To stimulate behavior change among stakeholders and facilitate implementation of the model, surveillance activities could be seen as an integral step to furthering research, programs, and policies and providing a foundation for effective and informed initiatives. Surveillance organizations may adopt strategies that ensure that data systems are available for widespread use, encourage innovative use of high-quality data, and assure the results of these efforts are disseminated broadly. This may require providing technical assistance and training to organizations that may not currently use high-quality surveillance data to inform their work. Surveillance is an important lever that can be used to assess progress toward realizing improved outcomes among cancer survivors.
The PHAM-CS model can expand and enhance research in the area of cancer survivorship by compelling researchers to engage with programmatic and community stakeholders and seek out collaborations with other individuals working across the SEM levels. Research organizations could benefit from using traditional stakeholder engagement strategies seen in community-based participatory research as well as expand their relationships to those that develop programs and policy. This support may come in the form of expanding pre-existing Communities of Practice to include programmatic and community stakeholders or providing technical assistance and trainings through initiatives like the Cancer Prevention and Control Research Network (cpcrn.org/). Researchers could continue to collaborate with program implementers and evaluators to assess how research is informing program practice.
Public health programs have great potential to make notable contributions to the area of survivorship. Although these programs have multiple partnerships with the capacity to develop and implement cancer survivorship strategies that are aligned with PHAM-CS levers, it is important that interventions are based on current surveillance data, research, and policy. Programs are also encouraged to continue to evaluate their efforts and identify opportunities for research, surveillance, and policy development.
The PHAM-CS also encourages collaboration with those who develop public health policy and guidelines for cancer survivors. Policy development and implementation are often dependent on economic, political, and societal contextual factors. Expansion of partnerships between organizations engaged in research, surveillance, and program development may facilitate sustainable policies and guidelines. The PHAM-CS calls for a commitment to create collaborations that result in an integrated, coordinated response to the needs of cancer survivors.
Broad Application of the Public Health Action Model for Cancer Survivorship
Though PHAM-CS was created to facilitate approaches to attain HP 2020 cancer survivorship objectives, core elements of the PHAM-CS model (SEM levels, foundational principles, levers, and drivers) can be applied to future public health initiatives that address other chronic disease conditions. The SEM and foundation principles (behavioral change, dissemination/implementation, and evaluation) are concepts extensively used in public health, especially in chronic disease prevention and control. The NAPCS strategies also resonate with public health organizations working on chronic disease conditions. Recent work by CDC identifies epidemiology and surveillance to monitor trends and inform programs, environmental approaches that promote health and support healthy behaviors, health system interventions to improve the effective use of clinical and other preventive services, and community resources linked to clinical services that sustain improved management of chronic conditions as viable approaches to address chronic disease.41 Public health uses HP 2020 to monitor and evaluate progress made toward meeting health outcome objectives. Each component described in PHAM-CS can be used and adapted to address other chronic diseases. Organizations that address public health concerns related to heart disease, diabetes, and tobacco use may have the infrastructure and capacity to implement the model through their partnerships, programs, research, and policy offices.
The PHAM-CS represents the implementation of NAPCS strategies in an environment in which public health works collaboratively with key stakeholders to effect change at the survivor, interpersonal, organizational, community, and policy levels with the aim of increasing the quality of life and survival rate of cancer survivors. This integrated model can support changes in multiple areas addressed by public health because its components reflect the needs of research and program constituents. Possibly the most significant challenge in implementing the PHAM-CS is the investment and commitment of organizations to work collaboratively and effectively to focus on distal outcomes. Organizations that make this commitment may make notable, lasting contributions to improving the health status and QOL of individuals diagnosed with cancer.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
No financial disclosures were reported by the authors of this paper.
Publication of this article was supported by the Centers for Disease Control and Prevention, Division of Cancer Prevention and Control.
References
- 1.Fairley TL, Pollack LA, Moore AR, Smith JL. Addressing cancer survivorship through public health: an update from the Centers for Disease Control and Prevention. J Women Health. 2009;18(10):1525–1531. doi: 10.1089/jwh.2009.1666. http://dx.doi.org/10.1089/jwh.2009.1666. [DOI] [PubMed] [Google Scholar]
- 2.De Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22(4):561–570. doi: 10.1158/1055-9965.EPI-12-1356. http://dx.doi.org/10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.A national action plan for cancer survivorship: advancing public health strategies. Atlanta, GA: U.S. DHHS, CDC; 2004. [Accessed September 8, 2015]. www.cdc.gov/cancer/survivorship/pdf/plan.pdf. [Google Scholar]
- 4.Underwood JM, Townsend JS, Stewart SL, et al. Surveillance of demographic characteristics and health behaviors among adult cancer survvors - Behavioral Risk Factor Surveillance System, United States, 2009. MMWR Surveill Summ. 2012;61(1):23. [PubMed] [Google Scholar]
- 5.U.S. DHHS Office of Disease Prevention and Health Promotion. Healthy People 2020. Washington, DC: 2015. [Accessed September 8, 2015]. www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives. [Google Scholar]
- 6.U.S. DHHS. [Accessed September 8, 2015];Phase I. Report - recommendations for the framework and format of Healthy People 2020. http://healthypeople.gov/2020/about/advisory/Reports.aspx.
- 7.IOM. The Future of the Public′s Health in the 21st Century. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 8.Bronfrenbrenner U. The Ecology of Human Development. Cambridge: Harvard Press; 1979. [Google Scholar]
- 9.McLeroy KR, Steckler A, Bibeau D. The social ecology of health promotion interventions. Health Educ Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. http://dx.doi.org/10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 10.Glanz K, Rimer BK, Lewis FM. In: Health Behavior and Health Education: Theory, Research, and Practice. 3. Glanz K, Rimer BK, Lewis FM, editors. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 11.Dahlgren G, Whitehead M. Equity in Health. Stockholm: Institute for Future Studies; 1991. [Accessed September 8, 2015]. Policies and strategies to promote social equity in health. http://s2.medicina.uady.mx/observatorio/docs/eq/li/Eq_2007_Li_Dahlgren.pdf. [Google Scholar]
- 12.Friedman D, Hunter E, Parrish R. Shaping a health statistics vision for the 21st century. Washington, DC: U.S. DHHS Data Council, CDC, National Center for Health Statistics, and National Committee on Vital and Health Statistics; 2006. [Accessed September 8, 2015]. www.ncvhs.hhs.gov/wp-content/uploads/2014/05/090922p3.pdf. [Google Scholar]
- 13.Daley E, Alio A, Anstey EH, Chandler R, Dyer K, Helmy H. Examining barriers to cervical cancer screening and treatment in Florida through a socio-ecological lens. J Community Health. 2011;36(1):121–131. doi: 10.1007/s10900-010-9289-7. http://dx.doi.org/10.1007/s10900-010-9289-7. [DOI] [PubMed] [Google Scholar]
- 14.CDC. [Accessed September 8, 2015];National Breast and Cervical Cancer Early Detection Program: Social ecological model. 2013 www.cdc.gov/cancer/nbccedp/sem.htm.
- 15.CDC. [Accessed September 8, 2015];Colorectal Cancer Control Program: Social ecological model. 2013 www.cdc.gov/cancer/crccp/sem.htm.
- 16.Downs LS, Jr, Scarinci I, Einstein MH, Collins Y, Flowers L. Overcoming the barriers to HPV vaccination in high-risk populations in the U.S. Gynecol Oncol. 2010;117(3):486–490. doi: 10.1016/j.ygyno.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 17.Lazovich D, Choi K, Rolnick C, Jackson JM, Forster J, Southwell B. An intervention to decrease adolescent indoor tanning: a multi-method pilot study. J Adoles Health. 2013;52(5 Suppl):S76–S82. doi: 10.1016/j.jadohealth.2012.08.009. http://dx.doi.org/10.1016/j.jadohealth.2012.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith JL, Pollack LA, Rodriguez JL, et al. Assessment of the status of A National Action Plan for Cancer Survivorship in the USA. J Cancer Surviv. 2013;7(3):425–438. doi: 10.1007/s11764-013-0276-8. http://dx.doi.org/10.1007/s11764-013-0276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moore R, Butow P. Culture and oncology: impact of context effects. In: Speigel D, editor. Cancer Communication and Culture. New York: Kluwer Academic; 2005. [Google Scholar]
- 20.Luthans F. Organizational Behavior. 10. McGraw-Hill; 2005. [Google Scholar]
- 21.Shafritz Jm, Ott SJ, Jang YS. Classics of Organizational Theory. 7. Belmont, CA: Wadsworth; 2011. [Google Scholar]
- 22.Alter C, Hage J. Organizations Working Together. California: Sage; 1993. [Google Scholar]
- 23.Wilson KM, Brady TJ, Lesesne C NCCDPHP Work Group on Translation. An organizing framework for translation in public health: the Knowledge to Action Framework. Prev Chronic Dis. 2011;8(2):A46. [PMC free article] [PubMed] [Google Scholar]
- 24.Pollack LA, Hawkins NA, Peaker B, Buchanan N, Risendal BC. Dissemination and translation: a frontier for cancer survivorship research. Cancer Epidemiol Biomarkers Prev. 2011;20(10):2093–2098. doi: 10.1158/1055-9965.EPI-11-0652. http://dx.doi.org/10.1158/1055-9965.EPI-11-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. http://dx.doi.org/10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 26.Patton MQ. Utilization-focused Evaluation. 3. California: Sage; 1997. [Google Scholar]
- 27.CDC. Framework for program evaluation in public health. MMWR Surveill Summ. 1999;48:1–40. [PubMed] [Google Scholar]
- 28.Major AA, Stewart SL. Celebrating 10 years of the National Comprehensive Cancer Control Program, 1998 to 2008. Prev Chronic Dis. 2009;6(4):A133. [PMC free article] [PubMed] [Google Scholar]
- 29. [Accessed October 13, 2015];Comprehensive Cancer Control National Partnership. http://www.cccnationalpartners.org.
- 30.Underwood M, Lakhani NA, Rohan E, Moore A, Stewart SL. An evaluation of cancer survivorship activities across national comprehensive control programs. J Cancer Surviv. 2015;9(3):554–559. doi: 10.1007/s11764-015-0432-4. http://dx.doi.org/10.1007/s11764-015-0432-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Phillips-Angeles E, Song L, Hannon PA, et al. Fostering partnerships and program success. Cancer. 2013;119:2884–2893. doi: 10.1002/cncr.28157. http://dx.doi.org/10.1002/cncr.28157. [DOI] [PubMed] [Google Scholar]
- 32.Rohan EA, Boehm JE, DeGroff A, Glover-Kudon R, Priessle J. Implementing CDC’s Colorectal Cancer Screening Demonstration Program: wisdom from the field. Cancer. 2013;119(S15 Suppl):2870–2883. doi: 10.1002/cncr.28162. http://dx.doi.org/10.1002/cncr.28162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seeff LC, Major A, Townsend JS, et al. Comprehensive cancer control programs and coalitions: partnering to launch successful colorectal cancer screening initiatives. Cancer Causes Control. 2010;21(12):2023–2031. doi: 10.1007/s10552-010-9664-9. http://dx.doi.org/10.1007/s10552-010-9664-9. [DOI] [PubMed] [Google Scholar]
- 34.CDC. [Accessed September 8, 2015];Advisory Committee on Breast Cancer in Young Women. 2015 www.cdc.gov/cancer/breast/what_cdc_is_doing/young_women.htm.
- 35.Buchanan N, Roland KB, Rodriguez JL, Miller JW, Fairley T. Opportunities for public health communication, intervention, and future research on breast cancer in younger women. J Women Health (Larchmt) 2013;22(4):293–298. doi: 10.1089/jwh.2012.4239. http://dx.doi.org/10.1089/jwh.2012.4239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.CDC. [Accessed September 8, 2015];Breast Cancer in Young Women. 2014 www.cdc.gov/cancer/breast/youngwomen/index.htm.
- 37.Trivers KF, Fink AK, Partridge AH, et al. Estimates of young breast cancer survivors at risk for infertility in the U.S. Oncologist. 2014;19(8):814–822. doi: 10.1634/theoncologist.2014-0016. http://dx.doi.org/10.1634/theoncologist.2014-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bloom JR, Stewart SL, Oakley-Girvan I, Banks PJ, Shema S. Quality of life of younger breast cancer survivors: persistence of problems and sense of well-being. Psychooncology. 2012;21(6):655–665. doi: 10.1002/pon.1965. http://dx.doi.org/10.1002/pon.1965. [DOI] [PubMed] [Google Scholar]
- 39.Johnson-Turbes A, Schlueter D, Moore AR, Buchanan ND, Fairley TL. Evaluation of a web-based program for African American young breast cancer survivors. Am J Prev Med. 2015;49(6S5):S543–S549. doi: 10.1016/j.amepre.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sisters Network, Inc. A young sisters initiative: a guide to a better you. 2012 http://sniyoungsisters.org/
- 41.Bauer UE, Briss PA, Goodman RA, Bowman BA. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. http://dx.doi.org/10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]