Abstract
The majority of individuals with Parkinson’s disease (PD) experience voice and speech difficulties at some point over the course of the disease. Voice therapy has been found to help improve voice and speech in individuals with PD, but the majority of these individuals do not enroll in voice therapy. The purpose of this study was to determine whether watching short videos about voice symptoms and treatment in Parkinson’s disease influences readiness to change, stages of change, and self-efficacy in individuals with PD. Eight individuals with PD participated in the study. Fifteen videos were chosen, three representing each of the five stages of change. We chose videos from YouTube that represented variety in speakers, content, and genre. We found that readiness to change significantly increased after watching videos, suggesting that watching videos helped these individuals move closer to actively improving their voice and speech. In addition, five of the eight participants showed forward movement in stages of change. Finally, self-efficacy demonstrated a positive trend following video watching. Overall, our results demonstrate that watching videos available on the internet can influence individuals with Parkinson’s disease in changing vocal behavior. Implications for future wireless health applications are described.
Keywords: Stages of Change, Self-Efficacy, Readiness to Change, Parkinson’s Disease
1. INTRODUCTION
Parkinson’s disease (PD) is a progressive neurodegenerative disorder [6, 35] with an estimated incidence rate of 13.4 per 100,000 person-years [12]. The highest rate of incidence of PD occurs in individuals over the age of 60 years [12]. Approximately 89% of individuals diagnosed with PD will experience problems with their voice and speech [35]. The voice and speech of individuals with PD is often marked by a combination of the following: reduced range of articulation, reduced pitch range, reduced loudness range, and imprecise articulation [5, 10]. Due to the progressive nature of the disease, these problems can worsen over time and make it difficult for listeners to understand speakers with PD. Voice therapy provided by a speech-language pathologist (SLP), such as the Lee Silverman Voice Treatment®, have been shown to benefit individuals with voice and speech disorders related to PD [35].
Despite the potential benefit of voice therapy for individuals with PD, it has been estimated that less than 5% of individuals with PD enroll in voice therapy [35]. The exact reason why more individuals with PD do not seek therapy is unknown. One potential explanation may be related to individuals’ motivation and confidence in their ability to change their voice and speech. Stages of change, readiness to change, and self-efficacy are metrics that previous researchers have applied in voice therapy literature [20–22, 34].
Stages of change is one dimension of change described in the transtheoretical model of behavior change [7, 31]. Five basic stages of change have been described in the literature: (1) precontemplation where individuals have a lack of knowledge that change is needed or lack of motivation to change, (2) contemplation where individuals are considering behavior change but are not currently committed to initiating the behavior change process, (3) preparation where individuals are committed to behavior change in the near future, (4) action where individuals are in the process of behavior change, and (5) maintenance where individuals continue to display the changed behavior and avoid relapse [8, 31]. Readiness to change estimates the likelihood that an individual will work toward making a behavioral change from one stage to the next [9, 34]. Self-efficacy estimates an individual’s confidence in his/her ability to change his/her own behavior [3].
Potential change strategies are recommendations by the National Cancer Institute to personalize intervention in a way that encourages individuals to move from one stage of change to a later stage of change [13]. These include personalizing information about the consequences of behavior change for individuals in the precontemplation stage, and encouraging problem solving for individuals in the action stage [13]. Behavioral interventions using appropriate change strategies should be able to increase readiness to change and self-efficacy, moving individuals from earlier stages to later stages of change.
Video may be a useful medium for persuading individuals to engage in the behavior change process. Lian (2011) described internet video sharing as the fastest growing internet-based multimedia service [24]. In addition, marketing researchers are evaluating the persuasive potential of online video [15]. Video as a persuasive system could potentially benefit from the principles of tailoring and suggestion [28]. The principle of tailoring suggests that the more a system is tailored to an individual, the more persuasive it is likely to be. In addition, the principle of suggestion provides support for the idea of offering targeted messages at “opportune moments” to increase persuasion [28].
In this study, we wanted to determine whether watching short videos influence readiness to change, stages of change, and self-efficacy in individuals with PD at risk for voice and speech disorders. We discuss the use of videos in voice behavior change.
2. RELATED WORK
2.1 Voice problems in Parkinson’s disease
Patients with Parkinson’s disease benefit from voice treatment to address to reduce voice and speech deficits attributed to the disease [33, 35]. The current problem that remains is motivating patients to take action to improve their voice and speech. This is true across all voice therapy patients, not just those with PD.
In a previous study, the researchers found that only 61% of patients adhered to physician referrals for voice therapy [30]. In a second study, the researchers found that only 35.4% of those patients who initiated voice therapy actually completed the recommended therapy [30].
Results from a study by Teixeira et al. [34] may provide some insight into the lack of therapy initiation and follow through. These authors administered the stages of change questionnaire (URICA-VOICE) to 66 voice patients at the beginning of therapy. They found that 87.9% of the patients were in the early stages of change: precontemplation and contemplation. The researchers suggested that being in these earlier, less action-oriented stages may lead to decreased adherence in voice therapy.
Another research team offered suggestions to facilitate the transition to later stages of change in voice therapy patients [22]. These suggestions are similar to the potential change strategies [13]. For example, they suggested that for a patient in the precontemplation stage, one possible strategy would be to increase the patient’s awareness of behaviors that may negatively impact the voice [22]. This is similar to the precontemplation stage potential change strategy of increasing the patient’s awareness that change is needed [13].
Despite clinician knowledge that both initiation and adherence to voice therapy are problematic, few studies have empirically studied this issue. In addition, these studies have examined a general population of voice disorder patients, rather than a specific subset. The current study seeks to determine whether videos can influence behavior change in a specific subset of voice therapy patients: individuals with PD.
2.2 Health videos
The idea of using video as a persuasive system for patients is actively being explored. Huh et al. [16] discussed the benefit of health video blogs (health vlogs) for both informational and emotional support. In the study, the researchers examined health vlogs created by patients with HIV, diabetes, and cancer. They found that health vloggers used video for multiple purposes, including: educating others, inspiring others, and both seeking and offering social support. In the paper, some suggested potential design implications for this rich medium included: (1) supporting education and (2) self-monitoring: video could be used to capture changes in the self over time.
Another study addressed the importance of content presentation in persuasive videos. In the study, the researchers compared an annotated how-to video with a non-annotated video [17] viewed prior to an image manipulation task. The researchers found that annotated videos led to greater self-efficacy, satisfaction, and ratings in the subsequent task.
In voice therapy literature, video has been examined as an alternative augmentation to home practice of therapy exercises. Van Leer and Connor [21] compared two methods of intervention in a randomized crossover design: written therapy instructions and video demonstrations (by both a clinician and the patient) [21]. In the study, they found that patients’ practice frequency and overall self-efficacy were significantly greater after a week of video demonstrations for home practice than written instructions. A second study by the same authors (2015) compared home practice with written instructions against a combination of written instructions and MP4 videos. The authors found that those in the MP4 group reported significantly greater generalization and self-efficacy for generalization of target voice production than those in the control group. These studies together suggest that video can be instrumental in increasing adherence and self-efficacy for voice therapy.
Researchers under-explored how videos can persuade individuals not currently enrolled in voice therapy to take action. In the current study, we look at individuals with Parkinson’s disease because even if they are not currently experiencing voice and speech difficulties, there is a high likelihood that these problems may develop over time.
2.3 Wireless health for behavior change
A myriad of literature targeted the use of wireless health technologies, such as smart phones, web interactive systems, and wearable devices to influence motivation for behavior change. In Wireless Health proceedings [11, 26], interactive systems have focused on improving diet and exercise habits in order to prevent later health problems. Du, Youngblood, and Pirolli [11] introduced a goal-setting system for tracking changes, such as diet and exercise, that allowed for social interaction among group members. The researchers found the following changes: increased healthy eating, decreased stress, and increased physical activity. Murray et al. [26] introduced an avatar connected to automatic measure of physical activity based on accelerometer readings. Both of these studies address changing behavior as a preventative measure, similar to our goal in preventing PD patients from experiencing further voice problems.
Behavior change is possible with short-term interventions. Park and Gweon [29] examined the impact of a short intervention on motivation for behavior change in smartphone use. The researchers compared two groups on moderation of smartphone use: a group who participated in a decisional balance exercise and those who did not. The authors found that even a short, 5 minute intervention trended toward increased likelihood of movement to later stages of change and decreased smartphone usage time to a greater degree than the control group. In addition, the researchers found statistically significant increased seeking and complying with interventions, as well as significantly more intervention applications used by the test group, which used decisional balance exercise.
A study by Lee et al. looked at providing a short intervention to educate individuals about behavior-change techniques for personal goals, with follow-up sessions to assess use of the behavior change strategies [19]. The researchers found that the richness of the content provided through the intervention was important to later implementation.
While the current literature provides evidence for ways to influence behavior change, none of these prior studies evaluate an intervention using videos to influence behavior change in patients with PD. In addition, prior voice therapy literature has examined inclusion of videos in therapy [21], but not for advocating enrollment in voice therapy. Therefore, we want to determine whether videos can influence stages of change, readiness to change, and self-efficacy in these individuals. The results of this study can provide evidence that a wireless health platform using videos to support behavior change would be beneficial for individuals with PD.
3. METHODS
We hypothesize that after watching videos targeting potential change strategies that individuals with PD will demonstrate forward movement in stages of change, and increases in readiness to change and self-efficacy. To test this hypothesis, we administered stages of change and self-efficacy questionnaires to participants both before and after watching a set of pre-selected videos related to PD.
3.1 Participants
Eight individuals with PD (5M, 3F, 54–86 years old) participated in the study. Inclusion criteria were: (1) individuals must be diagnosed with Parkinson’s disease and (2) have no hearing or vision problems that would significantly impact their ability to interact with a computer screen and watch videos. Prior to inclusion in the study, all participants completed an informed consent document approved by the Michigan State University Institutional Review Board. Participants’ speech ranged from nearly normal to moderately disordered. One individual, P8, had previously received voice therapy for PD-related speech changes.
We recruited most participants from a local support group for individuals with PD, while the remainder of participants was recruited through referral. We chose to recruit from this support group because these individuals are generally motivated to seek information and support from others in coping with Parkinson’s disease. Initially, we had 12 individuals with PD express interest in participating in the study. However, only 8 of the 12 participants were available during the study period. While this was smaller than our targeted number, prior studies have evaluated voice therapy results from eight or fewer individuals with Parkinson’s disease [4, 32, 33] and reported significant results of treatment. Therefore, the sample size was determined to be appropriate for the current study.
3.2 Questionnaires
Each participant completed two questionnaires that measure stages of change, readiness to change, and self-efficacy: URICA-VOICE [34] and health-related self-efficacy [23, 27].
URICA-VOICE [34] is a modified version of the University of Rhode Island Change Assessment (URICA). The URICA and URICA-VOICE consist of questions related to the precontemplation (PC), contemplation (C), action (A), and maintenance (M) stages of change. The URICA-VOICE is specifically designed for individuals with voice disorders and consists of a total of 32 items. Items in the URICA-VOICE are rated using a 5-point scale ranging from “strongly disagree=1” to “strongly agree=5”, and a middle score of “don’t know=3.” Example items include: “Voice treatment is a waste of time for me because my voice does not bother me” and “I am dedicated enough to improve my voice problem.” For the URICA-VOICE, readiness to change is calculated by subtracting the mean PC score from the sum of the mean C, A, and M scores. To measure individuals’ current stages of change, we used the readiness to change scores and the recommended cutoff values: ≤8=PC; 8–11=C; 11–14=PA/A [34].
For measuring self-efficacy, we modified an existing self-efficacy scale [23, 27] to address voice behavior change. We substituted the word “health” with the word “voice” [23, 27]. For instance, “I can have a positive effect on my voice.” Statements in the self-efficacy scale were rated using a 5-point scale ranging from “disagree very much”=0 to “agree very much”=4.
3.3 Videos
YouTube.com provides a myriad of educational and supportive videos helpful for PD patients. For the current study, YouTube videos were included because they are publically available and address a wide array of topics. To select videos to show to participants, one researcher, with domain expertise in voice therapy, conducted a keyword search of YouTube to identify pre-existing, publically available videos related to Parkinson’s disease. Keywords included: “Parkinson’s patient,” “Parkinson’s disease, voice,” and “Parkinson’s disease, speech.” Each search returned over 1,000 results. However, after the first page, the videos quickly started to demonstrate repetitive information. For instance, when using the keywords “Parkinson’s disease, voice”, videos related to three voice therapy programs: LSVT®, Parkinson Voice Project, and Voice Aerobics were contained in the first page of results. The second page included videos of the same voice therapy programs, having a great deal of content overlap with the videos from the first page of results. These were often presented by the same type of speaker [e.g., speech-language pathologist (SLP)].
Accordingly, we started with the first page of the video results and continued to add related videos suggested by YouTube until we had 30 videos total, rather than working down the list of search results. The videos discussed various topics related to PD, including: disease-related changes in voice and speech, the impact of voice therapy, coping with the disease, and strategies to combat disease-related changes. The content and genre of the videos also varied, where some had PD patients talking to the camera, some had clinicians presenting, and some presented fact information about voice problems in PD. While assuming certain video types might be more effective than others for changing behavior of the viewer, we did not know which types were more effective than others (e.g., a patient speaking in the video vs. a doctor). Thus, we diversified the video format and content to help reduce any bias that might occur.
We defined the video content and format by: potential change strategy shown in the video, media type (e.g., speaker, PowerPoint), speaker type (e.g., patient, doctor, SLP), speaker gender, and speaker age. Two coders coded the videos together and negotiated any disagreements to determine which content and format each video contained. From 30 total videos, we ended up with 15 video segments that included a variety of content and format as shown in Table 1.
Table 1.
Video segment descriptions.
| Video | Stage of Change | Potential Change Strategy | Length (min) | Speaker(s) |
|---|---|---|---|---|
| 1 | PC | Awareness | 1:57:06 | patient, friend, doctor, SLP |
| 2 | PC | Awareness | 0:39:13 | patient |
| 3 | PC | Awareness | 0:14:60 | SLP |
| 4 | C | Motivation | 0:11:20 | none (PPT) |
| 5 | C | Motivation | 0:48:43 | exercise expert |
| 6 | C | Motivation | 0:56:96 | SLP |
| 7 | PA | Concrete action plan | 0:07:43 | patient, SLP |
| 8 | PA | Concrete action plan | 1:00:30 | SLP |
| 9 | PA | Concrete action plan | 0:40:83 | patient, SLP |
| 10 | A | Problem solving | 1:40:93 | none (PPT) |
| 11 | A | Problem solving | 1:34:36 | patient |
| 12 | A | Reinforcement | 0:06:83 | patient, SLP |
| 13 | M | Coping | 2:05:45 | SLP |
| 14 | M | Coping | 0:43:13 | patient |
| 15 | M | Avoiding slips | 1:01:66 | patient, SLP |
3.4 Procedures
Each participant completed an individual session of less than 1.5 hours. Participants completed the questionnaires both before and after watching the videos. We presented videos as icons on a PowerPoint slide, with the order of the icons randomized for each participant. Examples of these icons are featured in Figure 1. Participants chose the order in which videos were viewed.
Figure 1.

Left: an individual with PD. Right: a doctor. The screenshots of the video clips have been intentionally anonymized.
3.5 Analysis
We used a linear mixed effects model (LME) for readiness to change and a Wilcoxon signed rank test for self-efficacy. We chose LME and Wilcoxon based on the response variable type and the distribution of the data. We conducted descriptive analysis for stages of change. Data points were missing for P7 in the readiness to change analysis (one page of the three page questionnaire for a total of 12 missing data points) and P5 and P6 (1 missing value for P5 and for P6 post-video measurement) in the self-efficacy analysis. These values appeared to be missing at random, as the events leading to the loss of data were unrelated to observed variables (answers were omitted accidentally).
4. RESULTS
4.1 Stages of Change
Table 2 shows the stages of change scores for all participants before (pre) and after (post) watching videos. In the table, columns 2–5 show the average results for the URICA-VOICE. The participant’s readiness to change (column 6) determined the participant’s stage of change (column 7). Two consecutive rows represent the data for a single participant, with the first showing questionnaire results before watching the videos and the second showing results after watching the videos. As indicated by the asterisk (*), P7 was the only participant who did not complete all items in the questionnaire (one page was left blank).
Table 2.
Stages of change (SOC) and readiness to change (RTC) scores.
| Time | PC | Stages of Change | RTC | SOC | ||
|---|---|---|---|---|---|---|
| C | A | M | ||||
| P1: Pre | 1.71 | 4.00 | 2.29 | 2.29 | 6.86 | PC |
| P1: Post | 1.00 | 5.00 | 4.14 | 3.29 | 10.43 | C |
| P2: Pre | 1.86 | 4.29 | 3.80 | 3.14 | 9.00 | C |
| P2: Post | 1.57 | 4.86 | 4.67 | 4.57 | 11.71 | PA/A |
| P3: Pre | 3.14 | 3.00 | 3.00 | 3.00 | 5.57 | PC |
| P3: Post | 1.29 | 4.29 | 4.29 | 4.29 | 10.00 | C |
| P4: Pre | 2.14 | 3.57 | 2.93 | 2.43 | 6.43 | PC |
| P4: Post | 1.86 | 4.00 | 3.73 | 3.43 | 8.71 | C |
| P5: Pre | 2.86 | 2.29 | 2.07 | 1.57 | 2.43 | PC |
| P5: Post | 1.57 | 4.29 | 3.80 | 3.43 | 8.29 | C |
| P6: Pre | 2.00 | 3.29 | 3.21 | 3.14 | 8.14 | C |
| P6: Post | 2.14 | 3.29 | 3.47 | 3.57 | 8.57 | C |
| P7: Pre* | 1.17 | 4.67 | 4.86 | 5.00 | 13.00 | PA/A |
| P7: Post | 0.86 | 4.43 | 3.80 | 3.14 | 11.00 | C |
| P8: Pre | 1.71 | 3.43 | 3.43 | 3.43 | 8.29 | C |
| P8: Post | 1.86 | 3.14 | 3.67 | 4.00 | 8.57 | C |
Five of the eight participants demonstrated forward movement in stages of change. All four participants in the PC showed forward movement to either C or PA/A. One of three participants starting in the C stage showed forward movement to PA/A. Only one participant, P7, showed backward movement in stages of change from PA/A to C, but this maybe attributed to the incomplete data.
4.2 Readiness to Change
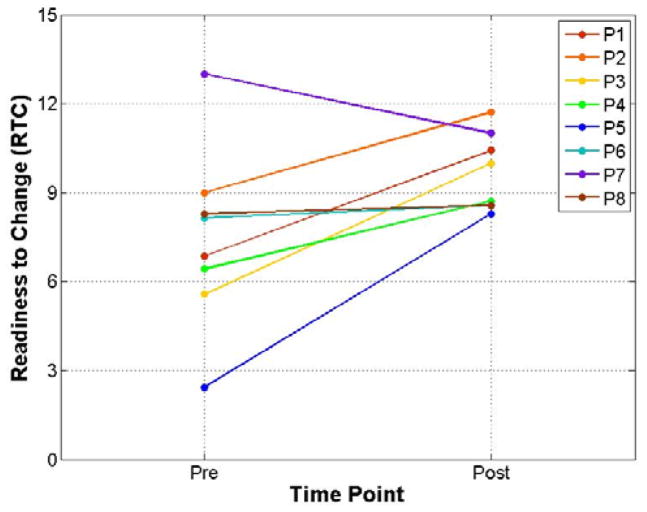
A LME model was run with readiness to change as the response variable. In the model, participant was treated as a random factor and time (pre/post) was treated as a fixed factor. Posttest readiness to change scores were found to be significantly higher than pretest readiness to change scores, β = 2.2, SE = 0.9, df = 7, t = 2.4, p < 0.05, 95% CI [0.54 4.06]. Figure 2 shows the change in readiness to change pre- to post-video watching.
Figure 2.
Participant readiness to change over time.
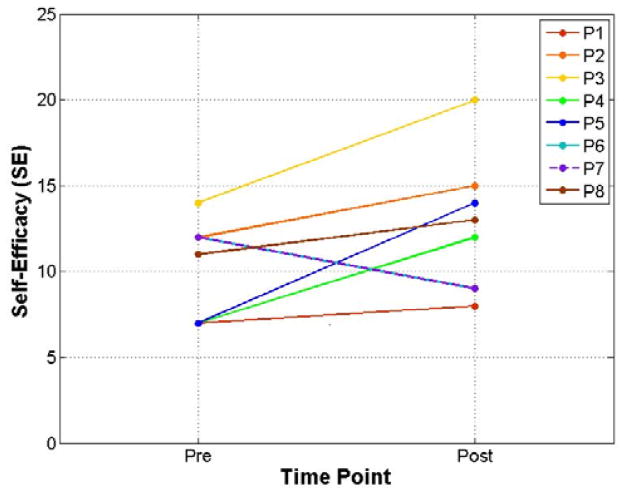
4.3 Self-Efficacy
The effect of targeted video watching on self-efficacy was analyzed by means of a Wilcoxon signed rank test. Post-test self-efficacy scores were not found to be significantly different from pretest self-efficacy scores, V = 8, p = 0.181. However, Figure 3 demonstrates a trend of increasing self-efficacy from pre- to post-video watching.
Figure 3.
Participant self-efficacy over time.
4.4 Video Watching
Participants were instructed that they were not required to watch all 15 videos, but could choose to stop watching the videos at any time. Seven of the eight participants watched all videos in the study. Only one participant, P6, did not watch all 15 videos. When asked about watching another video after the 12th one, he stated: “No, I don’t think so.” P6 did not provide any additional information for stopping the video watching. P6 still completed the two questionnaires following video watching.
5. DISCUSSION
5.1 Influence of Videos on Behavior Change
Overall, the results of this study demonstrate that watching videos available on the internet can influence individuals with Parkinson’s disease in changing vocal behavior.
Readiness to change showed a statistically significant increase following video watching. This result indicates an increase in the likelihood that an individual with PD will work toward making behavior change (pursuing voice therapy) post-video watching. Future longitudinal studies should be conducted to determine whether individuals who watch these videos actually engage in behavior change and how long the changes last [18]. The useful finding here is that health professionals can use videos to persuade patients to make changes toward their illness.
We saw the largest forward movement in stages of change for individuals who began in the PC stage moving to the C stage. One possible explanation is that individuals in the PC stage benefit from any information, regardless of the potential change strategy targeted in the videos.
5.2 Potential for Future Use of Videos in Influencing Behavior Change
The current study used publicly available YouTube videos to demonstrate that short video segments can be used to increase readiness to change for voice and speech in individuals with PD. The videos in this study represented a range of potential change strategies, and were presented to individuals at varying stages of change.
Future research could consider the effect of videos targeting potential change strategies personalized for individuals’ movement in stages of change and level of readiness to change and self-efficacy. In addition, specific effects of one kind of video over another, such as patient videos versus clinician videos, will be a scope for future work. This research will help uncover videos supporting individuals at all stages to move forward in stages of change, increase readiness to change, and self-efficacy.
The information from this future research could be used in building tools that recommend appropriate, personalized videos to individual patients. These tools could then be incorporated into wireless health platforms to provide ease of access for both patients and health care professionals. Since the videos will be selected from YouTube with appropriate meta-data about videos online, the tool can match appropriate videos online with patients based on their stages of change. This real-time access to YouTube videos would additionally allow for viewing updated videos as additional content is posted. Health care professionals can also use such tools to encourage individuals with PD to seek voice therapy for improving voice and speech problems related to the disease.
The same strategy of using videos can be expanded to advocate for enrollment in voice therapy to individuals with other voice disorders who may benefit from voice therapy. For example, patients with vocal fold lesions may benefit from watching videos related to their diagnoses. Voice therapy is often recommended to either determine the necessity of surgery or used before and after surgery to optimize the outcome [2]. Previous research has demonstrated that only about one-third of individuals recommended for voice therapy actually complete the recommended treatment [14]. Therefore, by providing patients with appropriate videos, health care professionals may increase patients’ interest and adherence to therapy, which could improve the overall outcome of intervention.
5.3 Study Limitations
The current study provides preliminary evidence that videos can influence stages of change, readiness to change, and self-efficacy in individuals with Parkinson’s disease. However, the sample size should be increased in future work on this topic. Having a larger sample size may uncover statistically significant increases in self-efficacy after video watching due to the increase in power. In addition, due to this limitation, it is difficult to make strong claims for generalization to the larger population of individuals with PD. Nonetheless, the results are promising and warrant further investigation.
In addition, the current study only assessed stages of change, readiness to change, and self-efficacy immediately before and after watching the videos. In order to assess long-term benefits of watching the videos, additional assessments should be performed at periodic intervals after the video intervention. For example, one self-efficacy study followed smokers 1 month, 3 months, 6 months, and 1 year after an intervention to determine whether participants experienced smoking relapse [25]. These follow-up assessments can be used to determine how long the effects last, and whether increases in these measures lead to enrollment in voice therapy, which would be the ultimate goal of the video intervention.
6. CONCLUSIONS
The results of this study demonstrate that the use of simple wireless health technology, such as watching videos available on the internet, can influence readiness to change for voice and speech in individuals with Parkinson’s disease. The increase in readiness to change demonstrates that, after watching videos, individuals with PD show an increased willingness to work toward making changes in voice and speech.
Our findings demonstrate how low-cost, publicly available online videos can effectively impact patients’ behavior change, contributing to patient-centered care. This pilot study was a necessary initial step in the development of a wireless health platform that incorporates video technology to advocate for voice behavior change in individuals with Parkinson’s disease.
Acknowledgments
Research reported in this publication was supported by NLM of the National Institutes of Health under award number K01LM011980. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Lisa M. Kopf, Email: kopflisa@msu.edu, Michigan State University, Communicative Sciences and Disorders, East Lansing, MI 48824
Simone Graetzer, Email: sgraetz@msu.edu, Michigan State University, Communicative Sciences and Disorders, East Lansing, MI 48824.
Jina Huh, Email: jinahuh@msu.edu, University of California, San Diego, Biomedical Informatics, San Diego, CA.
References
- 1.Alku P, Vilkman E. A comparison of glottal voice source quantification parameters in breathy, normal and pressed phonation of female and male speakers. Folia phoniatrica et logopaedica: official organ of the International Association of Logopedics and Phoniatrics (IALP) 1996;48(5):240–254. doi: 10.1159/000266415. 1996. [DOI] [PubMed] [Google Scholar]
- 2.American Speech-Language-Hearing Association. The Use of Voice Therapy in the Treatment of Dysphonia. American Speech-Language-Hearing Association; 2005. Technical Report #TR2005-00158. [Google Scholar]
- 3.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological review. 1977;84(2):191. doi: 10.1037//0033-295x.84.2.191. 1977. [DOI] [PubMed] [Google Scholar]
- 4.Cannito MP, Suiter DM, Beverly D, Chorna L, Wolf T, Pfeiffer RM. Sentence intelligibility before and after voice treatment in speakers with idiopathic Parkinson’s disease. Journal of Voice: Official Journal of the Voice Foundation. 2012 Mar;26(2):214–219. doi: 10.1016/j.jvoice.2011.08.014. 2012. [DOI] [PubMed] [Google Scholar]
- 5.Darley FL, Aronson AE, Brown JR. Clusters of deviant speech dimensions in the dysarthrias. Journal of speech and hearing research. 1969;12(3):462. doi: 10.1044/jshr.1203.462. 1969. [DOI] [PubMed] [Google Scholar]
- 6.Dawson TM, Dawson VL. Molecular Pathways of Neurodegeneration in Parkinson’s Disease. Science. 2003 Oct;302(5646):819–822. doi: 10.1126/science.1087753. 2003. [DOI] [PubMed] [Google Scholar]
- 7.DiClemente CC, Prochaska JO. Self-change and therapy change of smoking behavior: a comparison of processes of change in cessation and maintenance. Addictive Behaviors. 1982;7(2):133–142. doi: 10.1016/0306-4603(82)90038-7. 1982. [DOI] [PubMed] [Google Scholar]
- 8.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology. 1991;59(2):295–304. doi: 10.1037//0022-006x.59.2.295. 1991. [DOI] [PubMed] [Google Scholar]
- 9.DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. The American Journal on Addictions/American Academy of Psychiatrists in Alcoholism and Addictions. 2004 Apr;13(2):103–119. doi: 10.1080/10550490490435777. 2004. [DOI] [PubMed] [Google Scholar]
- 10.Duffy JR. Motor Speech Disorders: Substrates, Differential Diagnosis, and Management. Elsevier Mosby; 2005. [Google Scholar]
- 11.Du H, Youngblood GM, Pirolli P. Efficacy of a Smartphone System to Support Groups in Behavior Change Programs. Proceedings of the Wireless Health 2014 on National Institutes of Health (New York, NY, USA, 2014) 2014;3(1–3):8. [Google Scholar]
- 12.Eeden SKVD, Tanner CM, Bernstein AL, Fross RD, Leimpeter A, Bloch DA, Nelson LM. Incidence of Parkinson’s Disease: Variation by Age, Gender, and Race/Ethnicity. American Journal of Epidemiology. 2003 Jun;157(11):1015–1022. doi: 10.1093/aje/kwg068. 2003. [DOI] [PubMed] [Google Scholar]
- 13.Glanz K, Rimer BK National Cancer Institute (U.S.) Theory at a glance: a guide for health promotion practice. U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1997. [Google Scholar]
- 14.Hapner E, Portone-Maira C, Johns MM., III A Study of Voice Therapy Dropout. Journal of Voice. 2009 May;23(3):337–340. doi: 10.1016/j.jvoice.2007.10.009. 2009. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh J-K, Hsieh Y-C, Tang Y-C. Exploring the disseminating behaviors of eWOM marketing: persuasion in online video. Electronic Commerce Research. 2012 Mar;12(2):201–224. 2012. [Google Scholar]
- 16.Huh J, Liu LS, Neogi T, Inkpen K, Pratt W. Health Vlogs As Social Support for Chronic Illness Management. ACM Trans Comput-Hum Interact. 2014 Aug;21(4):23:1–23:31. doi: 10.1145/2630067. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim J, Nguyen PT, Weir S, Guo PJ, Miller RC, Gajos KZ. Crowdsourcing Step-by-step Information Extraction to Enhance Existing How-to Videos. Proceedings of the 32Nd Annual ACM Conference on Human Factors in Computing Systems; New York, NY, USA. 2014; 2014. pp. 4017–4026. [Google Scholar]
- 18.Klasnja P, Consolvo S, Pratt W. How to Evaluate Technologies for Health Behavior Change in HCI Research. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; New York, NY, USA. 2011; 2011. pp. 3063–3072. [Google Scholar]
- 19.Lee J, Walker E, Burleson W, Hekler EB. Understanding Users’ Creation of Behavior Change Plans with Theory-Based Support. Proceedings of the 33rd Annual ACM Conference Extended Abstracts on Human Factors in Computing Systems; New York, NY, USA. 2015; 2015. pp. 2301–2306. [Google Scholar]
- 20.van Leer E. The role of social-cognitive factors in voice therapy adherence and outcomes. The University of Wisconsin - Madison; 2010. [Google Scholar]
- 21.van Leer E, Connor NP. Use of Portable Digital Media Players Increases Patient Motivation and Practice in Voice Therapy. Journal of Voice. 2012 Jul;26(4):447–453. doi: 10.1016/j.jvoice.2011.05.006. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Leer E, Hapner ER, Connor NP. Transtheoretical model of health behavior change applied to voice therapy. Journal of Voice. 2008 Nov;22(6):688–698. doi: 10.1016/j.jvoice.2007.01.011. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee SY, Hwang H, Hawkins R, Pingree S. Interplay of Negative Emotion and Health Self-Efficacy on the Use of Health Information and Its Outcomes. Communication Research. 2008 Jun;35(3):358–381. 2008. [Google Scholar]
- 24.Lian S. Innovative Internet video consuming based on media analysis techniques. Electronic Commerce Research. 2011 Jan;11(1):75–89. 2011. [Google Scholar]
- 25.McIntyre KO, Lichtenstein E, Mermelstein RJ. Self-efficacy and relapse in smoking cessation: A replication and extension. Journal of Consulting and Clinical Psychology. 1983;51(4):632. doi: 10.1037//0022-006x.51.4.632. 1983. [DOI] [PubMed] [Google Scholar]
- 26.Murray T, Jaimes L, Hekler E, Spruijt-Metz D, Raij A. A Glanceable Mobile Avatar for Behavior Change. Proceedings of the 4th Conference on Wireless Health (New York, NY, USA, 2013) 2013;16(1–16):2. [Google Scholar]
- 27.National Library of Medicine (NLM) Variable: Self-Efficacy. 2012. CHIRr: Consumer health informatics research resource. [Google Scholar]
- 28.Oinas-Kukkonen H, Harjumaa M. Persuasive technology. Springer; 2008. A systematic framework for designing and evaluating persuasive systems; pp. 164–176. [Google Scholar]
- 29.Park H, Gweon G. Initiating Moderation in Problematic Smartphone Usage Patterns. Proceedings of the 33rd Annual ACM Conference Extended Abstracts on Human Factors in Computing Systems; New York, NY, USA. 2015; 2015. pp. 1585–1590. [Google Scholar]
- 30.Portone C, Johns MM, III, Hapner ER. A Review of Patient Adherence to the Recommendation for Voice Therapy. Journal of Voice. 2008 Mar;22(2):192–196. doi: 10.1016/j.jvoice.2006.09.009. 2008. [DOI] [PubMed] [Google Scholar]
- 31.Prochaska JO, DiClemente CC. The transtheoretical approach: crossing traditional boundaries of therapy. Dow Jones-Irwin; 1984. [Google Scholar]
- 32.Schalling E, Gustafsson J, Ternström S, Bulukin Wilén F, Södersten M. Effects of tactile biofeedback by a portable voice accumulator on voice sound level in speakers with Parkinson’s disease. Journal of Voice: Official Journal of the Voice Foundation. 2013 Nov;27(6):729–737. doi: 10.1016/j.jvoice.2013.04.014. 2013. [DOI] [PubMed] [Google Scholar]
- 33.Spielman J, Mahler L, Halpern A, Gilley P, Klepitskaya O, Ramig L. Intensive voice treatment (LSVT®LOUD) for Parkinson’s disease following deep brain stimulation of the subthalamic nucleus. Journal of Communication Disorders. 2011 Dec;44(6):688–700. doi: 10.1016/j.jcomdis.2011.05.003. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teixeira LC, Rodrigues ALV, da Silva AFG, Azevedo R, Gama ACC, Behlau M. The use of the URICA-VOICE questionnaire to identify the stages of adherence to voice treatment. CoDAS. 2013;25(1):8–15. doi: 10.1590/s2317-17822013000100003. 2013. [DOI] [PubMed] [Google Scholar]
- 35.Trail M, Fox C, Ramig LO, Sapir S, Howard J, Lai EC. Speech treatment for Parkinson’s disease. NeuroRehabilitation. 2005;20(3):205–221. 2005. [PubMed] [Google Scholar]