Abstract
Background and Objectives
Temporal trends in mortality from congenital heart disease (CHD) vary among regions. It is therefore necessary to study this problem in each country. In Mexico, congenital anomalies were responsible for 24% of infant mortality in 2013 and CHD represented 55% of total deaths from congenital anomalies among children under 1 year of age. The objectives of this study were to analyze the trends in infant mortality from CHD in Mexico (1998 to 2013), its specific causes, age at death and associated socio-demographic factors.
Methods
Population-based study which calculated the compounded annual growth rate of death rom CHD between 1998 and 2013. Specific causes, age at which death from CHD occurred and risk factors associated with mortality were analyzed for the year 2013.
Results
Infant mortality from CHD increased 24.8% from 1998 to 2013 (114.4 to 146.4/ 100,000 live births). A total of 3,593 CHD deaths occurred in 2013; the main causes were CHD with left-to-right shunt (n = 487; 19.8/100,000 live births) and cyanotic heart disease (n = 410; 16.7/100,000). A total of 1,049 (29.2%) deaths from CHD occurred during the first week of life. Risk factors associated with mortality from CHD were, in order of magnitude: non-institutional birth, rural area, birth in a public hospital and male sex.
Conclusions
Mortality from CHD has increased in Mexico. The main causes were CHD with left-to-right shunt, which are not necessarily fatal if treated promptly. Populations vulnerable to death from CHD were identified. Approximately one-third of the CHD occurred during the first week of life. It is important to promote early diagnosis, especially for non-institutional births.
Introduction
Worldwide, mortality of children under 5 years of age decreased 47% from 1990 to 2015, from 90.6 to 42.5 deaths per 1,000 live births [1]. This was achieved primarily by decreasing diarrheal and respiratory infections as well as diseases that can be prevented by vaccinations. Meanwhile, congenital anomalies have become a more significant cause of death among children under 5 years of age, increasing from 5% of deaths in 2000 to 7% in 2013; and this increase was even larger in the Americas, from 15 to 21% during this same period [2]. Furthermore, congenital heart disease accounts for nearly one-third of congenital anomalies [3].
Temporal trends in congenital heart disease (CHD) vary among countries. Mortality from CHD decreased over recent years in Canada and in 16 European countries, particularly for children under 1 year of age [4–6]. A decrease in mortality from CHD was also observed in the United States (U.S.) between 1970 and 1997, contributing to a 59% reduction in infant mortality during this period [7]. In contrast, the overall mortality rate from CHD in China increased 62% between 2003 and 2010 [8].
Mortality from CHD has increased in some countries, which may actually reflect a higher number of CHD patients diagnosed and registered at birth and higher necropsy rates for perinatal deaths, rather than an increase in the prevalence of the disease. This deserves further research.
In Mexico, significant efforts have been undertaken over recent years to decrease infant mortality among children under 1 year of age. Thus, between 1990 and 2010 the infant mortality rate decreased from 24.0 to 11.8 per 1000 live births [9]. Nevertheless, mortality from CHD was found to increase in both absolute and relative terms. In the year 2000, CHD caused the death of 2,596 children under 1 year of age, representing 6.7% of total deaths in this age group. By 2008, mortality from CHD increased to 2,848, representing 9.6% of the total [10].
Current and detailed information is required to identify national mortality trends related to all CHD in the infant population, and needs to be based on the ICD-10 in order to make international comparisons. Information is also needed that is useful to those responsible for making decisions about children’s public health in Mexico as well as to international health agencies, about a problem which seems to be on the rise in developing nations and which is a global health concern.
The main objective of the present study is to analyze trends in mortality from CHD in Mexico between 1998 and 2013. Secondary objectives are identifying the principal causes of death from CHD, determining the age at death from CHD and analyzing socio-demographic factors associated with death from CHD.
Methods
Study period and variables included
This is a population-based study conducted in Mexico which analyzes trends in infant mortality from CHD from 1998—the year when this country began to use the 10th revision of the ICD (ICD-10) [11]—until 2013. This made it possible to obtain a more detailed and specific description of CHD. For the purpose of international comparisons, all deaths from CHD corresponding to ICD-10 codes Q20-Q28 were included [12]. The study also included the following variables contained in the death certificates: sex, age, primary place of residence, state, size of locality and place where the death occurred. These data did not allow for estimating the proportion of preterm patients or determining diagnoses associated with chromosomal abnormalities. Fetal deaths were not included in the analysis because Mexico does not have a national surveillance program to collect all diagnoses of fetal cardiac disease.
The number of surgeons, cardiologists and pediatricians registered in Mexico in 2003 and 2012 were included in the analysis; these are the years with known information and were used for comparison purposes.
Data sources
The information was obtained from all death certificates. These are routinely coded by the General Department of Health Information (DGIS, Spanish acronym) which produces electronic databases available to the public through the National System for Health Information (SINAIS, Spanish acronym), at the DGIS webpage [10]. The data for number of live registered births (LB) and socio-demographic information were obtained from the webpage provided by the National Institute of Statistics and Geography (INEGI, Spanish acronym) [13].
The number of surgeons, cardiologists and pediatricians registered in Mexico corresponds to the job positions reported by public hospitals and the Social Security Institute, according to the information from the DGIS [14]. This information was used to calculate rates of specialists per 1,000 LB.
Operational definitions
Rates were calculated based on the number of deaths from CHD analyzed by this study for each specific year divided by the number of LB for each corresponding year, multiplied by 100,000.
The Functional Classification of CHD proposed by Reller et al [15] was adapted for this specific analysis, which divides heart defects into four subgroups: left-to-right shunt, cyanotic heart disease, obstructive defects of the left heart and obstructive defects of the right heart. All cases of patent ductus arteriosus were included since gestational age was not available.
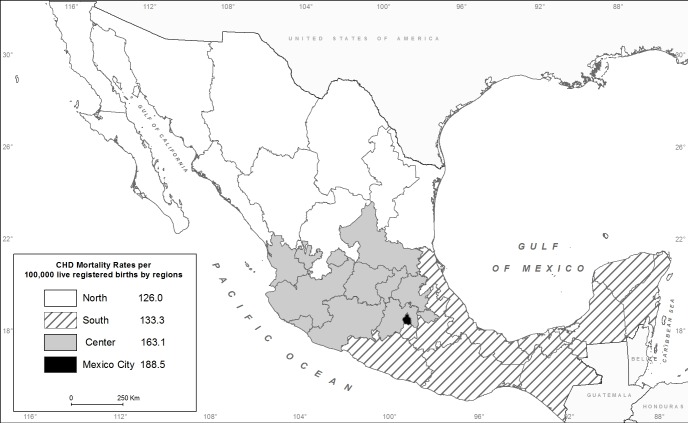
The classification proposed by the 2012 Mexican National Health and Nutrition Survey [16] was used to define the regional geographic distribution of the 32 states in the country, as follows: North (Baja California, Baja California Sur, Coahuila, Chihuahua, Durango, Nuevo León, Sinaloa, Sonora, Tamaulipas and Zacatecas); Central (Aguascalientes, Colima, Guanajuato, Hidalgo, Jalisco, Mexico State, Michoacán, Nayarit, Querétaro, San Luis Potosí and Tlaxcala); Mexico City (Federal District); and South (Campeche, Chiapas, Guerrero, Morelos, Oaxaca, Puebla, Quintana Roo, Tabasco, Veracruz and Yucatán). Rural areas were defined as residential localities with 2,500 or less inhabitants and urban areas as regions with a larger population [9].
Statistical analysis
The trend in CHD mortality rates per 100,000 LB was determined for the years 1998 to 2013. The CHD mortality rate and the compounded annual rate of growth (CARG) were calculated to determine the accumulated adjusted change in the rate for the period 1998–2013, according to the following formula: [final value/beginning value][1/number of years]
In 2013, the total deaths from CHD that occurred during the first year of life were calculated by postnatal period, classified by our data source as follows: first 24 hours of life, 1 to 6 days of life, 7 to 27 days of life and 28 days to 11 months of life. The number of deaths from CHD per day was estimated for each period.
For the year 2013, a univariate analysis was performed [(odds ratio (OR); 95% confidence interval (95%CI)] and the Mantel-Haenszel X2 was used to identify the factors associated with deaths from CHD. A value of p<0.05 was considered statistically significant.
IBM SPSS Statistics 19 statistical package was used for the statistical analysis [17]. OpenEpi version 3.03 was used to calculate the odds ratio and confidence intervals [18].
Results
Trends in mortality from CHD and descriptive analysis
A total of 41,717,421 births were registered from 1998 to 2013 and 50,759 deaths from CHD were diagnosed, resulting in a mortality rate for the period of 121.7 per 100,000 LB. Fig 1 shows an increasing trend in the CHD mortality rate over time for children under 1 year of age in Mexico—from 114.4 per 100,000 LB in the year 1998 to 146.4 per 100,000 LB in the year 2013, an increase of 24.8%. Fig 1 also shows a higher overall CHD mortality rate for males than for females. While the mortality rate for both sexes increased from 1998 to 2013, the increase was greater for females.
Fig 1. Infant mortality rate from congenital heart disease by sex.
Deaths per 100,000 live registered births, Mexico 1998–2013.
Table 1 presents the change in the CHD infant mortality rate from 1998 to 2013 in the 32 states in Mexico. Durango and Nayarit registered the highest increases in mortality from CHD (roughly 150 to 180%) while 11 states registered decreases in the CHD mortality rate. In the year 2013, a total of 1,876 deaths from CHD (52%) occurred in Mexico City and five states (State of Mexico, Jalisco, Puebla, Guanajuato and Veracruz).
Table 1. Mortality rate from congenital heart disease by state, Mexico 1998 and 2013.
| State | 1998 | 2013 | CARG† | |||
|---|---|---|---|---|---|---|
| Rate per 100,000 LB* | (n) | Rate per 100,000 LB* | (n) | 1998–2013 | ||
| 1 | Aguascalientes | 138.5 | 35 | 106.6 | 28 | -26.0 |
| 2 | Baja California | 141.5 | 82 | 132.0 | 81 | -6.9 |
| 3 | Baja California Sur | 110.0 | 11 | 104.9 | 13 | -4.8 |
| 4 | Campeche | 90.7 | 17 | 195.7 | 37 | 78.9 |
| 5 | Coahuila | 88.2 | 52 | 104.2 | 65 | 16.8 |
| 6 | Colima | 229.9 | 29 | 60.5 | 8 | -127.7 |
| 7 | Chiapas | 63.1 | 84 | 87.5 | 143 | 33.0 |
| 8 | Chihuahua | 90.5 | 72 | 131.8 | 87 | 38.1 |
| 9 | Mexico City | 162.3 | 293 | 188.5 | 272 | 15.0 |
| 10 | Durango | 32.7 | 15 | 132.4 | 52 | 146.5 |
| 11 | Guanajuato | 161.4 | 216 | 145.6 | 172 | -10.3 |
| 12 | Guerrero | 39.9 | 39 | 100.0 | 102 | 94.7 |
| 13 | Hidalgo | 81.0 | 54 | 127.8 | 75 | 46.3 |
| 14 | Jalisco | 140.7 | 231 | 163.9 | 260 | 15.3 |
| 15 | State of Mexico | 155.9 | 517 | 215.4 | 681 | 32.7 |
| 16 | Michoacán | 74.1 | 91 | 111.7 | 117 | 41.6 |
| 17 | Morelos | 161.8 | 55 | 131.8 | 49 | -20.4 |
| 18 | Nayarit | 27.8 | 7 | 149.5 | 36 | 178.1 |
| 19 | Nuevo León | 143.4 | 130 | 137.9 | 129 | -3.9 |
| 20 | Oaxaca | 92.4 | 98 | 124.1 | 114 | 29.7 |
| 21 | Puebla | 121.6 | 186 | 202.1 | 280 | 51.7 |
| 22 | Querétaro | 176.2 | 68 | 151.7 | 63 | -14.9 |
| 23 | Quintana Roo | 135.3 | 30 | 136.3 | 38 | 0.7 |
| 24 | San Luis Potosí | 127.2 | 84 | 118.0 | 64 | -7.4 |
| 25 | Sinaloa | 46.4 | 34 | 115.6 | 65 | 94.1 |
| 26 | Sonora | 113.1 | 63 | 127.7 | 67 | 12.2 |
| 27 | Tabasco | 117.2 | 58 | 148.1 | 77 | 23.6 |
| 28 | Tamaulipas | 92.9 | 59 | 134.0 | 80 | 37.1 |
| 29 | Tlaxcala | 125.0 | 35 | 122.8 | 33 | -1.8 |
| 30 | Veracruz | 83.5 | 181 | 132.2 | 211 | 46.7 |
| 31 | Yucatán | 150.8 | 57 | 143.5 | 55 | -4.9 |
| 32 | Zacatecas | 93.0 | 36 | 111.9 | 39 | 18.5 |
| National | 114.4 | 3019 | 146.4 | 3593 | 24.8 | |
*LB = Live registered births
†CARG = Compounded annual rate of growth
Source: INEGI/SSA
Fig 2 presents the distribution of the CHD mortality rates in the study regions for the year 2013.
Fig 2. Infant mortality rate from congenital heart disease by region.
Deaths per 100,000 live registered births, Mexico, 2013. Reprinted from Instituto de Geografía de la Universidad Nacional Autonóma de México under the Creative Commons Attribution License CC BY 3.0, with permission from Stephan André Couturier, original copyright 2015.
Table 2 presents some of the socio-demographic characteristics of infants who died from CHD in 2013. Mexico City reported the highest rate (188.5 per 100,000 LB) and the North reported the lowest (126 per 100,000 LB) for that year.
Table 2. Social and demographic characteristics of infant deaths from congenital heart disease.
Mexico 2013.
| Variable | CHD deaths*(n) | Births (n) | Rate† | |
|---|---|---|---|---|
| Total | 3,593 | 2,454,929 | 146.4 | |
| Sex | ||||
| Female | 1,638 | 1,212,556 | 135.1 | |
| Male | 1,946 | 1,242,232 | 156.7 | |
| NS¶ | 9 | 141 | - | |
| Regions | ||||
| North | 678 | 538,212 | 126.0 | |
| Central | 1,537 | 942,608 | 163.1 | |
| Mexico City | 272 | 144,278 | 188.5 | |
| South | 1,106 | 829,831 | 133.3 | |
| Area | ||||
| Urban | 2,813 | 2,047,323 | 137.4 | |
| Rural | 703 | 218,429 | 321.8 | |
| NS¶ | 77 | 189,177 | - | |
| Birth site | ||||
| Public hospital | 2,508 | 1,829,008 | 137.1 | |
| Private hospital | 241 | 317,113 | 76.0 | |
| Home and others | 802 | 167,104 | 479.9 | |
| NS¶ | 42 | 141,703 |
* CHD = Congenital heart disease
† Rate per 100,000 live registered births
¶NS = Not-specified
Source: INEGI/SSA
The majority of births as well as deaths from CHD occurred in the urban area. In 2013, there were roughly four times more deaths from CHD in this area than in the rural area. Nevertheless, the mortality rates from CHD were higher in the rural area.
In the year 2013, a total of 69.8% of infant deaths from CHD occurred in public hospitals and 6.7% in private hospitals. The latter had the lowest CHD mortality rate while home births had the highest rate—22.3% of total deaths from CHD. Home and other non-institutional births represented 6.8% of the total births.
In the year 2003, the rate of pediatricians, surgeons and cardiologists per 1,000 LB was 2.4, 1.9 and 0.3, respectively. These rates increased to 4.0, 3.6 and 0.6 by the year 2012, respectively.
Specific causes of death from CHD
Fig 3 presents the temporal analysis of specific and individual causes of death from CHD for the period 1998–2013. There was an increase in infant deaths from CHD with left-to-right shunt—specifically, patent ductus arteriosus and ventricular septal defect—which were the main causes of death in 2013, followed by discordant ventriculo-arterial connections and obstruction of the left heart.
Fig 3. Main causes of infant mortality from congenital heart disease, Mexico 1998–2013.
According to an analysis of causes of death from CHD for the year 2013, based on the adaptation of the functional classification proposed by Reller et al [15], CHD with left-to-right shunt were the main causes of death in the first year of life. Topping the list were patent ductus arteriosus, ventricular septal defect and auricular septal defect (Table 3). Cyanotic heart diseases, as a group, took second place, most notably discordant ventriculo-arterial connection and Tetralogy of Fallot.
Table 3. Functional classification of deaths from congenital heart disease in children under 1 year of age.
Rates and frequencies, Mexico 2013.
| ICD- | Cause | Male | Female | NS* | Total | Male | Female | Total |
|---|---|---|---|---|---|---|---|---|
| 10 | n | n | n | n | rate† | rate† | rate† | |
| I | LEFT TO RIGHT SHUNT | 250 | 237 | 0 | 487 | 20.1 | 19.5 | 19.8 |
| Q25.0 | Patent ductus arteriosus | 107 | 128 | 0 | 235 | 8.6 | 10.6 | 9.6 |
| Q21.0 | Ventricular septal defect | 78 | 64 | 0 | 142 | 6.3 | 5.3 | 5.8 |
| Q21.1 | Atrial septal defect | 38 | 22 | 0 | 60 | 3.1 | 1.8 | 2.4 |
| Q21.2 | Atrioventricular septal defect | 25 | 17 | 0 | 42 | 2.0 | 1.4 | 1.7 |
| Q21.9 | Congenital malformations of cardiac | 0 | 5 | 0 | 5 | 0.0 | 0.4 | 0.2 |
| septum, unspecified | ||||||||
| Q21.4 | Aortopulmonary septal defect | 1 | 1 | 0 | 2 | 0.1 | 0.1 | 0.1 |
| Q21.8 | Other congenital malformations of | 1 | 0 | 0 | 1 | 0.1 | 0.0 | 0.0 |
| cardiac septum | ||||||||
| II | CYANOTIC CONGENITAL | 239 | 171 | 0 | 410 | 19.2 | 14.1 | 16.7 |
| HEART DEFECTS | ||||||||
| Q20.3 | Discordant ventriculo-arterial | 68 | 28 | 0 | 96 | 5.5 | 2.3 | 3.9 |
| connections | ||||||||
| Q21.3 | Tetralogy of Fallot | 41 | 40 | 0 | 81 | 3.3 | 3.3 | 3.3 |
| Q20.4 | Double inlet ventricle | 35 | 20 | 0 | 55 | 2.8 | 1.6 | 2.2 |
| Q26.4 | Anomalous pulmonary venous | 22 | 19 | 0 | 41 | 1.8 | 1.6 | 1.7 |
| connection, unspecified | ||||||||
| Q20.0 | Common arterial trunk | 18 | 13 | 0 | 31 | 1.4 | 1.1 | 1.3 |
| Q26.2 | Total anomalous pulmonary venous | 17 | 14 | 0 | 31 | 1.4 | 1.2 | 1.3 |
| connection | ||||||||
| Q22.5 | Ebstein anomaly | 10 | 18 | 0 | 28 | 0.8 | 1.5 | 1.1 |
| Q22.4 | Congenital tricuspid stenosis | 16 | 7 | 0 | 23 | 1.3 | 0.6 | 0.9 |
| Q20.9 | Congenital malformations of cardiac | 5 | 5 | 0 | 10 | 0.4 | 0.4 | 0.4 |
| chambers and connections, | ||||||||
| unspecified | ||||||||
| Q20.8 | Other congenital malformations of | 3 | 3 | 0 | 6 | 0.2 | 0.2 | 0.2 |
| cardiac chambers and connections | ||||||||
| Q20.5 | Discordant auriculoventricular | 3 | 1 | 0 | 4 | 0.2 | 0.1 | 0.2 |
| connection | ||||||||
| Q20.1 | Transposition of the great vessels in | 1 | 3 | 0 | 4 | 0.1 | 0.2 | 0.2 |
| the right ventricle | ||||||||
| III | LEFT HEART OBSTRUCTIVE DEFECTS | 131 | 96 | 0 | 227 | 10.5 | 7.9 | 9.2 |
| Q23.4 | Hypoplastic left heart | 58 | 34 | 0 | 92 | 4.7 | 2.8 | 3.7 |
| syndrome | ||||||||
| Q25.1 | Coarctation of aorta | 41 | 38 | 0 | 79 | 3.3 | 3.1 | 3.2 |
| Q25.4 | Other congenital malformations of | 12 | 10 | 0 | 22 | 1.0 | 0.8 | 0.9 |
| aorta | ||||||||
| Q23.0 | Congenital stenosis of aortic valve | 10 | 8 | 0 | 18 | 0.8 | 0.7 | 0.7 |
| Q23.2 | Congenital mitral stenosis | 4 | 2 | 0 | 6 | 0.3 | 0.2 | 0.2 |
| Q23.3 | Congenital mitral insufficiency | 3 | 2 | 0 | 5 | 0.2 | 0.2 | 0.2 |
| Q23.9 | Congenital malformations of aortic | 1 | 2 | 0 | 3 | 0.1 | 0.2 | 0.1 |
| and mitral valves, unspecified | ||||||||
| Q23.1 | Congenital insufficiency of aortic | 2 | 0 | 0 | 2 | 0.2 | 0.0 | 0.1 |
| valve | ||||||||
| IV | RIGHT HEART OBSTRUCTIVE | 60 | 59 | 0 | 119 | 4.8 | 4.9 | 4.8 |
| DEFECTS | ||||||||
| Q25.5 | Atresia of pulmonary artery | 32 | 32 | 0 | 64 | 2.6 | 2.6 | 2.6 |
| Q22.8 | Other congenital malformations of | 10 | 3 | 0 | 13 | 0.8 | 0.2 | 0.5 |
| tricuspide valves | ||||||||
| Q22.6 | Hypoplastic right heart syndrome | 6 | 7 | 0 | 13 | 0.5 | 0.6 | 0.5 |
| Q22.0 | Pulmonary valve atresia | 6 | 6 | 0 | 12 | 0.5 | 0.5 | 0.5 |
| Q25.6 | Stenosis of pulmonary artery | 4 | 4 | 0 | 8 | 0.3 | 0.3 | 0.3 |
| Q22.1 | Congenital pulmonary valve stenosis | 1 | 3 | 0 | 4 | 0.1 | 0.2 | 0.2 |
| Q25.7 | Other congenital malformations of | 1 | 2 | 0 | 3 | 0.1 | 0.2 | 0.1 |
| pulmonary artery | ||||||||
| Q22.3 | Other congenital malformations of pulmonary valve | 0 | 2 | 0 | 2 | 0.0 | 0.2 | 0.1 |
| NON CLASSIFICABLE | 60 | 35 | 0 | 95 | 4.8 | 2.9 | 3.9 | |
| Q24.8 | Other congenital heart malformations | 51 | 32 | 0 | 83 | 4.1 | 2.6 | 3.4 |
| Q24.6 | Congenital heart block | 4 | 0 | 0 | 4 | 0.3 | 0.0 | 0.2 |
| Q24.5 | Malformation of coronary vessels | 3 | 0 | 0 | 3 | 0.2 | 0.0 | 0.1 |
| Q26.9 | Congenital malformations of great veins, | 2 | 3 | 0 | 5 | 0.2 | 0.2 | 0.2 |
| unspecified | ||||||||
| Q27 | Other congenital malformations of | 3 | 4 | 0 | 7 | 0.2 | 0.3 | 0.3 |
| peripheral vascular system | ||||||||
| Q28 | Other congenital malformations of | 2 | 3 | 0 | 5 | 0.2 | 0.2 | 0.2 |
| circulatory system | ||||||||
| Q24.9 | Congenital malformations of heart, | 1201 | 1033 | 9 | 2243 | 96.7 | 85.2 | 91.4 |
| unspecified | ||||||||
| Total | 1946 | 1638 | 9 | 3593 | 156.7 | 135.1 | 146.4 |
*NS = Not specified
†Rate per 100,000 live registered births
Source: INEGI/SSA
CHD deaths by age at death
Table 4 presents the distribution of the specific causes of death from CHD by age at death for the year 2013. Patent ductus arteriosus, obstructive defects of the left heart, discordant ventriculo-arterial connections represented the majority of the known causes of early neonatal death (under 7 days of life). Patent ductus arteriosus was the main cause of death during the neonatal period as well as during the first year of life. Ventricular septal defect, patent ductus arteriosus and coarctation of the aorta were the main causes during the post-neonatal period. Over 60% of the death certificates did not contain a specific diagnosis of the CHD, and this information was missing on 90% of deaths occurring on the first day of life.
Table 4. Main causes of infant mortality from congenital heart disease by age at death (frequencies and proportions).
Mexico 2013.
| ICD-10 | Cause | Less than 24 hs | 1–6 days | 7–27 days | 28 days-11 months | Less than 1 year | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | N | (%) | |||
| 1 | Q25.0 | Patent ductus | 4 | 1.1 | 45 | 6.4 | 93 | 11.9 | 93 | 5.3 | 235 | 6.5 |
| arteriosus | ||||||||||||
| 2 | Q21.0 | Ventricular septal | 1 | 0.3 | 9 | 1.3 | 27 | 3.5 | 105 | 6.0 | 142 | 4.0 |
| defect | ||||||||||||
| 3 | Q20.3 | Discordant ventriculo- | 3 | 0.9 | 19 | 2.7 | 30 | 3.8 | 44 | 2.5 | 96 | 2.7 |
| arterial connections | ||||||||||||
| 4 | Q23.4 | Hypoplastic left heart syndrome | 5 | 1.4 | 35 | 5.0 | 28 | 3.6 | 24 | 1.4 | 92 | 2.6 |
| 5 | Q21.3 | Coarctation of aorta | 2 | 0.6 | 9 | 1.3 | 14 | 1.8 | 56 | 3.2 | 81 | 2.3 |
| 6 | Q25.1 | Tetralogy of Fallot | 1 | 0.3 | 15 | 2.1 | 31 | 4.0 | 32 | 1.8 | 79 | 2.2 |
| 7 | Q25.5 | Atresia of pulmonary artery | 3 | 0.9 | 12 | 1.7 | 17 | 2.2 | 32 | 1.8 | 64 | 1.8 |
| 8 | Q21.1 | Atrial septal defect | 1 | 0.3 | 8 | 1.1 | 19 | 2.4 | 32 | 1.8 | 60 | 1.7 |
| 9 | Q20.4 | Double inlet ventricle | 0 | 0.0 | 15 | 2.1 | 7 | 0.9 | 33 | 1.9 | 55 | 1.5 |
| 10 | Q21.2 | Atrioventricular septal defect | 0 | 0.0 | 4 | 0.6 | 8 | 1.0 | 30 | 1.7 | 42 | 1.2 |
| 11 | Q26.4 | Common arterial trunk | 0 | 0.0 | 5 | 0.7 | 7 | 0.9 | 29 | 1.6 | 41 | 1.1 |
| 12 | Q20.0 | Anomalous pulmonary, | 0 | 0.0 | 0 | 0.0 | 10 | 1.3 | 21 | 1.2 | 31 | 0.9 |
| venous connection | ||||||||||||
| unspecified | ||||||||||||
| 13 | Q26.2 | Congenital tricuspid | 1 | 0.3 | 3 | 0.4 | 5 | 0.6 | 22 | 1.2 | 31 | 0.9 |
| Stenosis | ||||||||||||
| 14 | Q22.5 | Ebstein anomaly | 2 | 0.6 | 6 | 0.9 | 10 | 1.3 | 10 | 0.6 | 28 | 0.8 |
| 15 | Q22.4 | Congenital stenosis of aortic valve | 0 | 0.0 | 1 | 0.1 | 6 | 0.8 | 16 | 0.9 | 23 | 0.6 |
| Subtotal | 23 | 6.6 | 186 | 26.6 | 312 | 39.9 | 579 | 32.9 | 1100 | 30.6 | ||
| Q24.9 | Congenital | 310 | 88.3 | 471 | 67.5 | 408 | 52.2 | 1054 | 59.8 | 2243 | 62.4 | |
| malformation of heart, unspecified | ||||||||||||
| The rest of Q20-Q28 | 18 | 5.1 | 41 | 5.9 | 62 | 7.9 | 129 | 7.3 | 250 | 7.0 | ||
| Total | 351 | 100 | 698 | 100 | 782 | 100 | 1762 | 100 | 3593 | 100 | ||
Source: INEGI/SSA
In 2013, approximately 10 children under 1 year of age died from CHD per day, on average. Most of the deaths per day occurred on the day of birth—351 deaths per day, representing approximately 10% of total deaths—followed by the period corresponding to day 1 through 6 of life with an average of 116 deaths per day from CHD, representing 19.4% of total deaths from CHD.
Factors associated with mortality from CHD
Factors (OR; 95% CI) associated with mortality from CHD were, in order of magnitude: non-institutional birth (6.34;5.49–7.32) as compared to private hospital, rural area (2.35;2.16–2.55) as compared to urban area, birth in public hospital (2.35;2.16–2.55) as compared to private hospital, and male sex (1.16;1.09–1.24) as compared to females.
Discussion
Trends in mortality
In 2013 in Mexico, congenital anomalies were responsible for 24% of infant mortality and CHD represented 55% of total deaths from congenital anomalies among children under 1 year of age [10]. From 1998 to 2013, a significant increase (24.8%) in mortality from CHD among children under 1 year of age was detected. And by the year 2013, the CHD mortality rate for children under 1 year of age was 146.4 per 100,000 LB—3.5 times higher than that reported for the U.S. from 1999 to 2006 (41.5 per 100,000 LB) [19]. Two interesting studies that have investigated infant mortality from CHD in Mexico also show that it is on the rise. Nevertheless, one [20] of these only included Mexican municipalities presenting high mortality from congenital anomalies and the other [21] did not include CHD corresponding to International Classification of Diseases (ICD-10) code Q25 (congenital anomalies of great arteries), which constitutes a significant proportion (11.5%) of deaths from CHD among children under 1 year of age. These studies also did not include updated information from the past decade in Mexico, nor did they include a detailed analysis of the specific causes of CHD or the age at death. Thus, the information provided by the work herein is very important because it gives a current and complete national overview of this public health problem.
Also notable is that mortality from CHD increased roughly 150 to 180% in some of the states. This information is important to improve planning related to health services in order to address the demand created by this serious public health problem. Furthermore, it is important to perform epidemiological studies to understand the high risk of CHD observed in certain geographic areas. In 2013, 52% percent of the deaths from CHD occurred in Mexico City and five states. It is of interest that lower-income states (Guerrero, Oaxaca Chiapas and others) had lower CHD mortality rates than states with a higher gross domestic product per capita (Mexico City, Mexico State, Campeche) [9]. This could be related to either the presence of high risk genetic or environmental factors in the latter states or, alternatively, it might represent underreporting of deaths in states with fewer resources. A study by Hernandez et al [22] detected that 22.6% (95% confidence interval (CI):12.3–36.2) of deaths among children under 5 years of age were underreported in Mexican municipalities with a very low human development index.
Although we do not have a clear explanation for the observed trend in CHD mortality, risk factors associated with CHD are on the rise in Mexico. For example, diabetes and substance abuse—both known to be associated with CHD [16, 23–25]—are more prevalent now in women of reproductive age than 10 years ago. [23–25] Also, the number of specialists per capita increased over recent years; thus, it is possible that CHD deaths that previously went undetected are now diagnosed and registered as causes of infant mortality. This deserves further research. Meanwhile, factors that reduce the risk of CHD [26] need to be promoted. These include: perinatal consumption of folic acid; avoidance of smoking, alcohol and drugs by the mother; control of maternal obesity and diabetes; and avoidance of taking medications beginning early in pregnancy (certain types of analgesics and medications proven to be teratogenic).
Causes of death
The main causes of death from CHD are due to their prevalence and lethality. In Mexico, CHD with left-to-right shunt were the main causes of mortality among children under 1 year of age in 2013. Although CHD with left-to-right shunt are not more severe than others types—such as critical and complex CHD—they are more prevalent [3], which may explain our findings.
Patent ductus arteriosus was the leading cause of mortality from CHD. Although it is known that patent ductus arteriosus could be a physiological manifestation of extreme prematurity, when a death certificate indicates this as a cause of death it is clearly due to a pathological problem that would have received treatment [27]. Therefore, this study included patent ductus arteriosus among the types of CHD responsible for infant mortality, although with the limitation that information about the gestational age of patients with specific CHD was not available for the study population. As has been identified in different populations, the persistence of patent ductus arteriosus is a public health problem. Prevalence studies at the global level and in other countries have reported patent ductus arteriosus to be among the three main causes of congenital heart disease [3]. In a population study performed by Gilboa et al [19] in the U.S., patent ductus arteriosus was the fourth cause of infant mortality from CHD (rate of 1.3/100,000 LB) between 1999 and 2006. This indicates the importance of patent ductus arteriosus during the first year of life even in developed countries. In a report on Mexico by Cervantes-Salazar et al [28], patent ductus arteriosus and ventricular septal defects were the CHD that most frequently required a surgical intervention, according to the Mexican Registry of Pediatric Heart Surgery.
Ventricular septal defects became an increasingly more important cause of mortality from CHD over time, representing the second highest rate (5.8/100,000 per LB) by the year 2013. Given its mortality rate of 1.1/100,000 LB in the U.S. [19], this problem should also be addressed globally, since mortality should not be high when detected early and managed appropriately.
Cyanotic CHD, such as discordant ventriculo-arterial connections, and obstructive defects of the left heart, such as left ventricular hypoplasia and coarctation of the aorta, were among the six main causes of mortality from CHD. The latter are complex CHD which require specialized care and could be associated with worse outcomes. This is especially true for left ventricular hypoplasia, which is the main cause of mortality from CHD among children under 1 year of age in the U.S., with a mortality rate of 8.6/100,000 LB [19].
Age at death
In the year 2013, a total of 3,593 deaths from CHD occurred in Mexico, approximately 10% of which occurred on the first day of life. The analysis of the causes of death during the first 24 hours found that roughly 90% did not have a specific diagnosis, which is a cause for concern. For those that did have a diagnosis, left ventricular hypoplasia, patent ductus arteriosus, discordant ventriculo-arterial connection and pulmonary valve atresia were the leading causes. The lack of a specific diagnosis is a significant weakness in our hospital information system and, therefore, prenatal and early postnatal diagnosis in the first hours of life should be encouraged. This should include a complete physical exam and universal screening for CHD using pulse oximetry [29], a non-invasive procedure which is increasingly used for the timely diagnosis of CHD. Major CHD can be diagnosed during the prenatal period, which provides the opportunity to adequately plan postnatal treatment for these patients. In a systematic review of the literature performed by Holland et al [30], newborns with a prenatal diagnosis of critical congenital heart disease were significantly less likely to die prior to planned cardiac surgery than were those with a comparable postnatal diagnosis (OR, 0.26; 95% CI: 0.08–0.84). Also, a recent paper published by Eckersley et al [31] about a population study in New Zealand showed that early (antenatal or pre-discharge) diagnosis of critical CHD had better outcomes than late diagnosis (post-discharge). This study reported a higher mortality for late diagnosis than for early diagnosis (27% vs 16%, respectively; p<0.04).
Patent ductus arteriosus was the main cause of death from CHD during the neonatal period. The main causes of CHD during the post-neonatal period were ventricular septal defects, patent ductus arteriosus and coarctation of the aorta. A specific diagnosis of the cause of death during these periods was lacking in more than half of the cases. This may indicate a failure to adequately fill out the death certificate or a diagnostic failure by the echocardiography. These problems need to be improved in order to understand the epidemiology of mortality from CHD in Mexico. The absence of this data has also been reported in developed countries. For instance, in the U.S. a specific diagnosis was found to be lacking in as many as 34% of the CHD [19].
The number of deaths from CHD per day reported for different ages indicates the importance of the first week of life as a critical period, when the majority of deaths from CHD occurred, and particularly the first day of life. This situation should enable specialized health teams to design and plan strategies to determine diagnoses during prenatal and early neonatal periods and to provide effective and timely care [32]. To improve the life expectancy of patients with CHD, modern intensive care units are needed as well as health personnel trained to manage them. Finally, the implementation of a good hospital referral system is important.
Factors associated with mortality
Factors associated with mortality from CHD were identified which indicate the social determinants of health that need to be addressed to improve infant survival. While 6.8% of births occurred at home or at other non-institutional sites, roughly 25% of the children under 1 year of age who died from a CHD in 2013 were born in this setting (data not shown), and the odds of dying from CHD were lower for births at private hospitals than for those at home and in public institutions. This fact leads us to emphasize the importance of implementing the WHO recommendation [33] to examine babies born at home as soon as possible during the first 24 hours of life, and to have three more check-ups thereafter. It is also important to promote institutionalized births and to understand the gap between outcomes at public and private institutions. Better outcomes at private institutions could be explained by better socioeconomic conditions and a better health status of the population using private centers, or these hospitals may use better practices to diagnose and treat CHD. In addition, living in a rural area was associated with 2.35 times more likelihood of dying from CHD compared to children living in urban areas. Meanwhile, a different result was observed in China, where a higher probability of dying (OR 1.20; 95%CI: 1.04–1.05) was associated with urban areas for children under 5 years of age [8]. These differences demonstrate the importance of conducting regional analyses. And finally, being a male—a non-modifiable biological risk factor—was associated with higher mortality, as has been previously reported [7].
National strategies need to focus on these vulnerable populations in the country and provide more investment and infrastructure for public hospitals, as well as eliminate the social barriers to accessing health services. Studies should also be conducted to determine whether rural areas present more exposure to factors that can increase the risk of CHD.
The strengths of this study include its population-based design and covering a long period of time, as well as the use of the ICD-10 on death certificates in Mexico which enabled making international comparisons. Another strength is the functional sub-classification presented. The inclusion of the age at death from CHD and the geographic analysis of these deaths are also very important since they contribute to establishing public health strategies to improve the prognosis of patients with CHD.
The weaknesses of the study include a lack of connection between birth certificates and death certificates in Mexico, not knowing the gestational age of CHD-specific deaths and not having identified deaths from CHD associated with chromosomal abnormalities. Another weakness is the high proportion of unspecified diagnoses, particularly on the first day of life, and the lack of fetal data which certainly underestimates the magnitude of this problem.
Conclusions
In Mexico, CHD presents a serious public health problem and has been increasing over recent years, as is occurring in several developing countries. Research is needed to understand this finding. The persistence of ductus arteriosus and other CHD with left-to-right shunt are the main causes of death among children under 1 year of age who have CHD. The neonatal period is the stage when most infant deaths from CHD occur.
Improving the early detection and epidemiological monitoring of CHD is also needed in Mexico. And linking the health information system to data from death and birth certificates is indispensable.
Finally, it is important for Mexico’s health system to promote comprehensive postnatal medical visits as recommended by the WHO.
Acknowledgments
The authors are grateful to Gerardo Sierra-Murguía for his help creating figures and data analysis and Gabriela Gómez Rodríguez for creating Fig 2.
Data Availability
Data are available from: http://www.sinais.salud.gob.mx/basesdedatos/std_defunciones.html.
Funding Statement
The authors have no support or funding to report.
References
- 1.You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, et al. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet. 2015. Epub 2015/09/13. 10.1016/s0140-6736(15)00120-8 . [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization: World Health Statistics 2015. 2015 ed. Luxembourg: WHO Press; 2015. Available: http://www.who.int/gho/publications/world_health_statistics/2015/en/. Accessed: 18 September 2015. [Google Scholar]
- 3.van der Linde D, Konings EE, Slager MA, Witsenburg M, Helbing WA, Takkenberg JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58(21):2241–7. Epub 2011/11/15. 10.1016/j.jacc.2011.08.025 . [DOI] [PubMed] [Google Scholar]
- 4.Ionescu-Ittu R, Marelli AJ, Mackie AS, Pilote L. Prevalence of severe congenital heart disease after folic acid fortification of grain products: time trend analysis in Quebec, Canada. BMJ. 2009;338:b1673 Epub 2009/05/14. 10.1136/bmj.b1673 ; PubMed Central PMCID: PMCPmc2682153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khoshnood B, De Vigan C, Vodovar V, Goujard J, Lhomme A, Bonnet D, et al. Trends in prenatal diagnosis, pregnancy termination, and perinatal mortality of newborns with congenital heart disease in France, 1983–2000: a population-based evaluation. Pediatrics. 2005;115(1):95–101. Epub 2005/01/05. 10.1542/peds.2004-0516 . [DOI] [PubMed] [Google Scholar]
- 6.Khoshnood B, Loane M, Garne E, Addor MC, Arriola L, Bakker M, et al. Recent decrease in the prevalence of congenital heart defects in Europe. J Pediatr. 2013;162(1):108–13.e2. Epub 2012/07/28. 10.1016/j.jpeds.2012.06.035 . [DOI] [PubMed] [Google Scholar]
- 7.Lee K, Khoshnood B, Chen L, Wall SN, Cromie WJ, Mittendorf RL. Infant mortality from congenital malformations in the United States, 1970–1997. Obstet Gynecol. 2001;98(4):620–7. Epub 2001/09/29. . [DOI] [PubMed] [Google Scholar]
- 8.Hu Z, Yuan X, Rao K, Zheng Z, Hu S. National trend in congenital heart disease mortality in China during 2003 to 2010: a population-based study. J Thorac Cardiovasc Surg. 2014;148(2):596–602.e1. Epub 2013/11/26. 10.1016/j.jtcvs.2013.08.067 . [DOI] [PubMed] [Google Scholar]
- 9.Instituto Nacional de Geografía e Informática (INEGI). Página oficial con información geográfica y demográfica de México. Instituto Nacional de Geografía e Informática.Bases de datos de: Economía [Internet]. Available: http://www3.inegi.org.mx/sistemas/mexicocifras. Accessed: 10 September 2015.
- 10.Secretaría de Salud. Dirección General de Informacion en Salud (DGIS). Sistema Nacional de Información en Salud. Bases de datos: Defunciones [Internet]. Available: http://www.dgis.salud.gob.mm/contenidos/basesdedatos/estandar.html. Accessed: 1 September 2015.
- 11.Organización Panamericana de la Salud-Organización Mundial de la Salud. Clasificación Estadística Internacional de Enfermedades y Problemas relacionados con la Salud. 10° Revisión. 2003 ed. Washington (DC) US: WHO Press; 1995.
- 12.Yeh SJ, Chen HC, Lu CW, Wang JK, Huang LM, Huang SC, et al. Prevalence, mortality, and the disease burden of pediatric congenital heart disease in Taiwan. Pediatr Neonatol. 2013;54(2):113–8. Epub 2013/04/18. 10.1016/j.pedneo.2012.11.010 . [DOI] [PubMed] [Google Scholar]
- 13.Instituto Nacional de Geografía e Informática (INEGI). Página oficial con información geográfica y demográfica de México. Consulta interactiva de datos. Base de datos de: Nacimientos [Internet]. Available: http://www.inegi.org.mx/est/lista_cubos/consulta.aspx?p=adm&c=5. Accessed: 1 September 2015. [Google Scholar]
- 14.Secretaría de Salud. Dirección General en información en Salud (DGIS). Base de datos: Recursos Humanos [Internet]. Available: http://www.dgis.salud.gob.mx/contenidos/sinais/estadisticas.html. Accessed: 3 March 2014. [Google Scholar]
- 15.Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A. Prevalence of congenital heart defects in metropolitan Atlanta, 1998–2005. J Pediatr. 2008;153(6):807–13. Epub 2008/07/29. 10.1016/j.jpeds.2008.05.059 ; PubMed Central PMCID: PMCPmc2613036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gutiérrez JP R-DJ, Shamah-Levy T, Villalpando-Hernández S, Franco A, Cuevas-Nasu L, Romero-Martínez M, et al. Encuesta Nacional de Salud y Nutrición 2012 Resultados Nacionales. 1st ed. Cuernavaca, Morelos, México: Instituto Nacional de Salud Pública; 2012. [Google Scholar]
- 17.SPSS Inc., and IBM Compay. Manual del usuario del sistema básico de IBM SPSS Statistics, version 19. New York, USA; 2010.
- 18.Dean AG SK, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health. 2015 [updated 2015/05/042015/10/03]. Versión 3.03a: Available: www.openepi.com/Menu/OE_Menu.htm. Accessed: 3 September 2015.
- 19.Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, Correa A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation. 2010;122(22):2254–63. Epub 2010/11/26. 10.1161/circulationaha.110.947002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valdes-Hernandez J, Canun-Serrano S, Reyes-Pablo AE, Navarrete-Hernandez E. [Birth defects mortality in five-year-old minors of age, Mexico, 1998–2006]. Salud Pública Mex. 2009;51(5):381–9. Epub 2009/11/26. . [DOI] [PubMed] [Google Scholar]
- 21.Gomez-Alcala AV, Rascon-Pacheco RA. [Infant mortality from congenital malformations in Mexico: an issue of opportunity and access to treatment]. Rev Panam Salud Pública. 2008;24(5):297–303. Epub 2009/01/15. . [DOI] [PubMed] [Google Scholar]
- 22.Hernandez B, Ramirez-Villalobos D, Duarte MB, Corcho A, Villarreal G, Jimenez A, et al. [Underreporting of deaths in children and birth certification in a representative sample of the 101 municipalities with lowest human development index in Mexico]. Salud Publica Mex. 2012;54(4):393–400. Epub 2012/07/27. . [DOI] [PubMed] [Google Scholar]
- 23.Instituto Nacional de Psiquiatiría Ramón de la Fuente Muñiz; Instituto Nacional de Salud Pública; Secretaría de Salud. Encuesta Nacional de Adicciones 2011: Reporte de Drogas. Villatoro-Velázquez JA, Medina-Mora ME, Fleiz-Bautista C et al. México D.F. México: INPRFM; 2012. Available: www.inprf.gob.mx. Accessed: 3 September 2015.
- 24.Simeone RM, Devine OJ, Marcinkevage JA, Gilboa SM, Razzaghi H, Bardenheier BH, et al. Diabetes and congenital heart defects: a systematic review, meta-analysis, and modeling project. Am J Prev Med. 2015;48(2):195–204. Epub 2014/10/19. 10.1016/j.amepre.2014.09.002 ; PubMed Central PMCID: PMCPmc4455032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aryana A, Williams MA. Marijuana as a trigger of cardiovascular events: speculation or scientific certainty? Int J Cardiol. 2007;118(2):141–4. Epub 2006/09/29. 10.1016/j.ijcard.2006.08.001 . [DOI] [PubMed] [Google Scholar]
- 26.Oster ME, Riehle-Colarusso T, Simeone RM, Gurvitz M, Kaltman JR, McConnell M, et al. Public health science agenda for congenital heart defects: report from a Centers for Disease Control and Prevention experts meeting. J Am Heart Assoc. 2013;2(5):e000256 Epub 2013/08/30. 10.1161/jaha.113.000256 ; PubMed Central PMCID: PMCPmc3835228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammerman C, Bin-Nun A, Kaplan M. Managing the patent ductus arteriosus in the premature neonate: a new look at what we thought we knew. Seminars in perinatology. 2012;36(2):130–8. Epub 2012/03/15. 10.1053/j.semperi.2011.09.023 . [DOI] [PubMed] [Google Scholar]
- 28.Cervantes-Salazar J, Calderon-Colmenero J, Ramirez-Marroquin S, Palacios-Macedo A, Bolio-Cerdan A, Vizcaino Alarcon A, et al. [Pediatric cardiovascular surgical data base registry in Mexico. First report]. Revista de investigacion clinica; organo del Hospital de Enfermedades de la Nutricion. 2013;65(6):476–82. Epub 2014/04/02. . [PubMed] [Google Scholar]
- 29.Good RJ, Canale SK, Goodman RL, Yeager SB. Identification of Critical Congenital Heart Disease in Vermont: The Role of Universal Pulse Oximetry Screening in a Rural State. Clinical pediatrics. 2015;54(6):570–4. Epub 2014/11/16. 10.1177/0009922814558247 . [DOI] [PubMed] [Google Scholar]
- 30.Holland BJ, Myers JA, Woods CR Jr. Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: a meta-analysis. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2015;45(6):631–8. Epub 2015/04/24. 10.1002/uog.14882 . [DOI] [PubMed] [Google Scholar]
- 31.Eckersley L, Sadler L, Parry E, Finucane K, Gentles TL. Timing of diagnosis affects mortality in critical congenital heart disease. Archives of disease in childhood. 2015. Epub 2015/07/02. 10.1136/archdischild-2014-307691 . [DOI] [PubMed] [Google Scholar]
- 32.Amsbaugh S, Scott SD, Foss K. Pulse Oximetry Screening for Critical Congenital Heart Disease: Bringing Evidence Into Practice. Journal of pediatric nursing. 2015;30(4):591–7. Epub 2014/12/03. 10.1016/j.pedn.2014.10.013 . [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization. WHO Recommendations on Posnatal care of the mother and newborn, 2013 Geneva, Switzerland: WHO Press; 2014. Available: http://apps.who.int/iris/bitstream/10665/97603/1/9789241506649_eng.pdf. Accessed: 3 Jun 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from: http://www.sinais.salud.gob.mx/basesdedatos/std_defunciones.html.