Abstract
A thyroid ultrasound examination programme has been conducted in Fukushima Prefecture, Japan, after the nuclear disaster in 2011. Although remarkably high prevalence of thyroid cancer was observed, no relevant quantitative evaluation was conducted. We calculated the observed/expected (O/E) ratio of thyroid cancer prevalence for the residents aged ≤20 years. Observed prevalence was the number of thyroid cancer cases detected by the programme through the end of April 2015. Expected prevalence was calculated as cumulative incidence by a life-table method using the national estimates of thyroid cancer incidence rate in 2001–10 (prior to the disaster) and the population of Fukushima Prefecture. The underlying assumption was that there was neither nuclear accident nor screening intervention. The observed and estimated prevalence of thyroid cancer among residents aged ≤20 years was 160.1 and 5.2, respectively, giving an O/E ratio of 30.8 [95% confidence interval (CI): 26.2, 35.9]. When the recent increasing trend in thyroid cancer was considered, the overall O/E ratio was 22.2 (95% CI: 18.9, 25.9). The cumulative number of thyroid cancer deaths in Fukushima Prefecture, estimated with the same method (annual average in 2009–13), was 0.6 under age 40. Combined with the existing knowledge about radiation effect on thyroid cancer, our descriptive analysis suggests the possibility of overdiagnosis. Evaluation including individual-level analysis is required to further clarify the contribution of underlying factors.
Keywords: early detection of cancer, radioactive hazard release, thyroid neoplasms, ultrasonography
Following the Fukushima Daiichi nuclear disaster on 11 March 2011, a thyroid ultrasound examination programme (Thyroid Screening Program) was established for residents aged ≤18 years of Fukushima Prefecture, Japan (1). The purpose of this programme was to assess the effect of the disaster on the incidence of childhood or adolescent thyroid cancer in the devastated area. The first 3 years were allocated to an ‘Initial’ phase, which served as a control period for evaluating the following ‘Full-scale’ phase (2,3). As of 30 April 2015, 300 476 children have been tested in the Initial phase (screening rate, 81.7%) (4). A total of 113 cases were either found to have or were suspected of having thyroid malignancy, of whom 99 underwent surgical treatment. However, no relevant quantitative evaluation was conducted so far. We recently estimated the prevalence of age-specific thyroid cancer in Fukushima Prefecture prior to the disaster (5). Here, we aimed to compare the observed prevalence of thyroid cancer in the Thyroid Screening Program with the estimated historical controls on the assumption that there was neither nuclear accident nor screening intervention.
We calculated the observed/expected (O/E) ratio of thyroid cancer prevalence for residents in Fukushima Prefecture aged ≤20 years. Observed prevalence was calculated by the number of thyroid cancer cases detected by the Thyroid Screening Program through the end of April 2015. Participants of the programme are residents of Fukushima Prefecture, including those who evacuated outside the prefecture, who were born between 2 April 1992 and 1 April 2011. Age range at the time of the disaster was 0–19 years. The number of detected cases was corrected for screening rate by multiplying the inverse of the age-specific screening rate (4).
Expected prevalence was obtained from our previous report (5,6), calculated by a life-table method using the national estimates of thyroid cancer incidence rate in 2001–10 (prior to the disaster) and the population of Fukushima Prefecture. In brief, using a life-table method, 5-year age-specific cumulative risk of thyroid cancer incidence in 2010 was calculated from thyroid cancer incidence and mortality rates, and all-cause mortality rates (7,8). Then, the calculated 5-year cumulative risk was converted into 1-year cumulative risk using spline smoothing. Finally, age-specific prevalence of thyroid cancer was estimated by multiplying the age-specific cumulative risk in 2010 by the 0-year-old population in the corresponding calendar year.
Because thyroid cancer incidence rate in Japan has recently been increasing (9), expected prevalence in 2014 was also estimated by multiplying the average annual percent change during the 10 years (males 1.2% per year; females 4.5% per year; 0–19 years old). The 95% confidence interval (CI) of O/E ratio was calculated assuming a Poisson distribution. The age-specific cumulative risk of thyroid cancer deaths under age 40 was calculated by applying the same life-table method to the mortality data in the latest 5 years (2009–13).
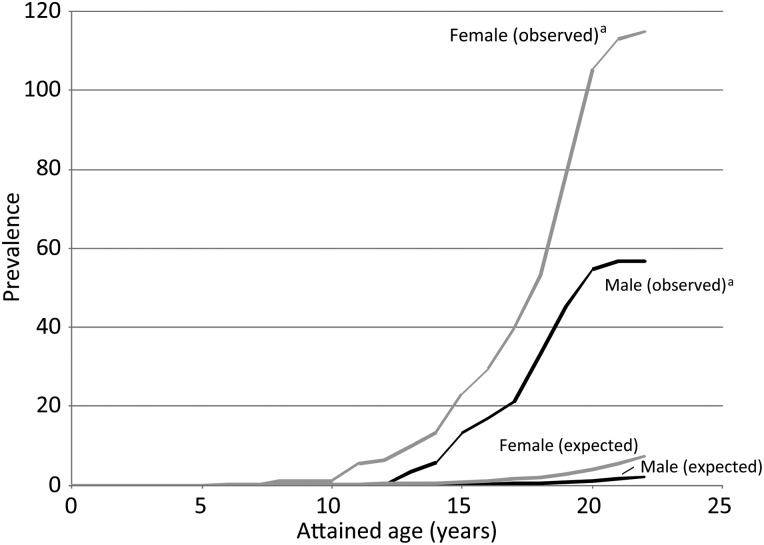
Figure 1 shows the estimated thyroid cancer prevalence and number of malignant cases (including suspected malignancy) detected by the Thyroid Screening Program. The estimated prevalence of thyroid cancer among residents aged ≤20 years in 2010 in Fukushima Prefecture was 1.2 for males and 4.0 for females. The corresponding observed number of malignant cases was 54.8 for males and 105.3 for females.
Figure 1.
Age-specific prevalence of thyroid cancer in Fukushima Prefecture, expected in 2010 and observed as of the end of April 2015. aConfirmed by aspiration biopsy (including suspected malignancy). The detected number was corrected for screening rate.
Table 1 shows results for the O/E ratio. The observed and estimated prevalence of thyroid cancer among residents in Fukushima Prefecture aged ≤20 years was 160.1 and 5.2, respectively, giving an O/E ratio of 30.8 (95% CI: 26.2, 35.9). The O/E ratio was higher for males than for females: 46.1 (95% CI: 34.5, 59.8) and 26.6 (95% CI: 21.7, 32.0), respectively. When we assume that the recent increasing trend in thyroid cancer continues, the overall O/E ratio was 22.2 (95% CI: 18.9, 25.9).
Table 1.
Observed and expected thyroid cancer prevalence in Fukushima Prefecture, as of the end of 2014
| Sex | Number of malignant casesa | Percentage among target population | O/E ratio | 95% CI | |
|---|---|---|---|---|---|
| Observed (age at screening ≤20)b | Males | 54.8 | 0.032 | ||
| Females | 105.3 | 0.064 | |||
| Total | 160.1 | 0.047 | |||
| Expected (attained age ≤20) | |||||
| Based on average incidence rate in 2001–10c | Males | 1.2 | 0.001 | 46.1 | 34.5, 59.8 |
| Females | 4.0 | 0.002 | 26.6 | 21.7, 32.0 | |
| Total | 5.2 | 0.002 | 30.8 | 26.2, 35.9 | |
| Based on incidence rate in 2014d | Males | 1.3 | 0.001 | 41.4 | 31.0, 53.7 |
| Females | 5.9 | 0.004 | 17.9 | 14.6, 21.6 | |
| Total | 7.2 | 0.002 | 22.2 | 18.9, 25.9 | |
O/E, observed/expected; CI, confidence interval.
aIncluding suspected malignancy.
bCorrected for age-specific screening rate.
cCalculated using the national incidence rate between 2001 and 2010.
dCalculated using the national incidence rate extrapolated to 2014 using the average annual percent change between 2001 and 2010.
The estimated cumulative number of thyroid cancer deaths in Fukushima Prefecture (annual average in 2009–13) was 0.10 (0.02 for males and 0.08 for females) by age 29, and 0.60 (0.27 for males and 0.33 for females) by age 39.
Using a modelling approach, Jacob et al. estimated that the screening factor in Fukushima Prefecture was 7.4 (95% CI: 0.96, 17.3) (10). Our estimate of screening impact was three to four times higher than this previous result. In their estimation, the detection rate of the screening programme was assumed to be 2.1 times higher in Fukushima than that in Chernobyl, based on the ratio of the numbers of nodules larger than 10 and 5 mm. However, the actual ratio observed in the Fukushima program was 3.4 (4). Screening in Chernobyl was performed nearly 15 years ago; recent improvements in diagnosis would have further increased the detection rate. The upper limit of 95% CI of their estimate would be 28.0 when applying the ratio observed in the Fukushima program. This value is close to our estimates.
Radiation-induced thyroid cancer cases are not expected to be detected before 3 years after the exposure according to the finding in Chernobyl (11). That is why the first 3 years were allocated to the Initial phase of the Thyroid Screening Program (it was actually extended by 1 year). We limited our analysis to those aged 20 years, which corresponds to 3 years at maximum after the potential radiation exposure. Even when we extended the analysis to age 21 years, no increase in O/E ratio was observed [males and females: 23.9 (95% CI: 20.4, 27.8), based on incidence rate in 2001–2010]. An estimated effective radiation exposure dose was available for 65 (57.5%) of the 113 detected cases, and was 2.2 mSv maximum and <1 mSv among 45 cases (71.4%) (4). This is within the annual effective dose from natural sources (2.4 mSv on average, with elevated values up to 10–20 mSv) (12).
The excess relative risk of thyroid cancer among children exposed to radiation from the Chornobyl accident was estimated to be 5.25 per gray (95% CI: 1.70, 27.5) (13). If this dose–response gradient can be applied to the Fukushima case within a short latency period, the observed high prevalence of thyroid cancer is unlikely to be explained by radiation exposure. Additionally, our estimate of cumulative number of thyroid cancer deaths in Fukushima was less than 1 under age 40, suggesting a possibility that detected cases would not become fatal. Taken together, our descriptive analysis suggests the possibility of overdiagnosis, though evaluation including individual-level analysis is required to further clarify the contribution of underlying factors.
Our estimates have several uncertainties. Firstly, although the overall screening rate was high (81.7%), there was variation with age at disaster (0–5 years: 85.7%; 6–10 years: 95.8%; 11–15 years: 83.1%; 16–18 years: 52.7%) (4). Given that the oldest age group had a low participation rate, we conducted a sensitivity analysis excluding the oldest age group (limiting to attained age of 18 years or younger). O/E ratio was 32.1 (95% CI: 25.6, 39.5), almost the same as the overall result (30.8; see Table 1). Secondly, to ensure data stability, we calculated the expected prevalence of thyroid cancer in Fukushima Prefecture using the national estimate of thyroid cancer incidence rate. A population-based cancer registry was started in Fukushima Prefecture in 2010: incidence rates of thyroid cancer among juveniles in 2011 were similar to the national estimates: 0.0 vs. 0.9 for 15–19 years old and 4.6 vs. 4.7 for 20–24 years old (per 100 000 population). Finally, we did not have information to distinguish cancers which could be ascertained even in the absence of screening programme and the cancers which could be detected only when screening programme was conducted.
In summary, during the first 3 years after the nuclear disaster in Fukushima, Japan, the Thyroid Screening Program targeting juveniles has identified 20–30 times more thyroid cancer cases than would be expected if the programme had not been implemented. The estimated cumulative number of thyroid cancer deaths in Fukushima (annual average in 2009–13) was 0.6 under age 40. Combined with the existing knowledge about radiation effect on thyroid cancer, our descriptive analysis suggests the possibility of overdiagnosis. Evaluation including individual-level analysis is required to further clarify the contribution of underlying factors.
Author's contributions
K.K.: Conception and design of the study, analysis, interpretation of data and drafting of the paper. K.-i.K.: analysis and revision of the paper for critical intellectual content. S.T.: conception and design of the study, and revision of the paper.
Funding
This work was supported by Grants-in-aid for the Cancer Control Policy from the Ministry of Health, Labour and Welfare, Japan (H26-Ganseisaku-Shitei-002, H26-Ganseisaku-Ippan-013). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Funding to pay the Open Access publication charges for this article was provided by the former grant (H26-Ganseisaku-Shitei-002).
Conflict of interest statement
S.T. is a member of the Prefectural Oversight Committee for Fukushima Health Management Survey.
Acknowledgements
The authors sincerely thank Dr Megumi Hori at the National Cancer Center, Japan, for her technical assistance in this study.
References
- 1.Yasumura S, Hosoya M, Yamashita S, Kamiya K, Abe M, Akashi M et al. . Study protocol for the Fukushima Health Management Survey. J Epidemiol 2012;22:375–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thyroid Ultrasound Examination (Full-scale Thyroid Screening Program). http://fmu-global.jp/survey/proceedings-of-the-18th-prefectural-oversight-committee-meeting-for-fukushima-health-management-survey/ (9 September 2015, date last accessed).
- 3.Interim Report of Thyroid Ultrasound Examination (Initial Screening): Fukushima Medical University. http://fmu-global.jp/survey/proceedings-of-the-18th-prefectural-oversight-committee-meeting-for-fukushima-health-management-survey/ (9 September 2015, date last accessed).
- 4.Final Report of Thyroid Ultrasound Examination (Initial Screening): Fukushima Medical University. http://fmu-global.jp/survey/the-20th-prefectural-oversight-committee-meeting-for-fukushima-health-management-survey/ (9 September 2015, date last accessed).
- 5.Katanoda K, Kamo KI, Hori M, Tsugane S. Estimated prevalence of thyroid cancer in Fukushima prior to the Fukushima Daiichi nuclear disaster. http://www.bmj.com/content/346/bmj.f1271/rr (25 February 2015, date last accessed).
- 6.Document 5 Estimated prevalence of thyroid cancer in Fukushima: Fukushima Medical University. http://www.pref.fukushima.lg.jp/sec/21045b/kenkocyosa-kentoiinkai-b4.html (22 October 2015, date last accessed) [Japanese].
- 7.Wun LM, Merrill RM, Feuer EJ. Estimating lifetime and age-conditional probabilities of developing cancer. Lifetime Data Anal 1998;4:169–86. [DOI] [PubMed] [Google Scholar]
- 8.Kamo K, Katanoda K, Matsuda T, Marugame T, Ajiki W, Sobue T. Lifetime and age-conditional probabilities of developing or dying of cancer in Japan. Jpn J Clin Oncol 2008;38:571–6. [DOI] [PubMed] [Google Scholar]
- 9.Katanoda K, Hori M, Matsuda T, Shibata A, Nishino Y, Hattori M et al. . An updated report on the trends in cancer incidence and mortality in Japan, 1958–2013. Jpn J Clin Oncol 2015;45:390–401. [DOI] [PubMed] [Google Scholar]
- 10.Jacob P, Kaiser JC, Ulanovsky A. Ultrasonography survey and thyroid cancer in the Fukushima Prefecture. Radiat Environ Biophys 2014;53:391–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heidenreich WF, Kenigsberg J, Jacob P, Buglova E, Goulko G, Paretzke HG et al. . Time trends of thyroid cancer incidence in Belarus after the Chernobyl accident. Radiat Res 1999;151:617–25. [PubMed] [Google Scholar]
- 12.Ionizing Radiation, Part 1: X- and Gamma-radiation, and Neutrons. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Lyon, France: World Health Organization International Agency for Research on Cancer, 2000. [Google Scholar]
- 13.Tronko MD, Howe GR, Bogdanova TI, Bouville AC, Epstein OV, Brill AB et al. . A cohort study of thyroid cancer and other thyroid diseases after the chornobyl accident: Thyroid cancer in Ukraine detected during first screening. J Natl Cancer Inst 2006;98:897–903. [DOI] [PubMed] [Google Scholar]