Abstract
Objectives To identify the prevalence and risk factors for nasal deformities after endoscopic endonasal surgery (EES) of the skull base.
Design Retrospective case series.
Setting Tertiary referral academic center.
Participants EES patients from January 2011 to October 2013.
Main Outcome Measures Surgical approach, method of skull base reconstruction, and postoperative nasal deformities.
Results Of 328 patients, 19 patients (5.8%) had nasal dorsum collapse, 3 (0.9%) with new septal perforations and 2 (0.6%) with septal deviations requiring surgical correction. Postoperative deformities were only found in the setting of nasoseptal flap reconstruction (p = 0.0001) and were most common in patients who had undergone an approach involving more than one anatomical subsite (p = 0.0021). Patients with nasal deformities were on average 6 years younger (p = 0.08) and were more likely to have a malignant pathology (p = 0.08).
Conclusions All deformities were associated with use of a nasoseptal flap for reconstruction and were most common in combined approaches, suggesting that flap size may play a role in the development of nasal deformities. The mechanism of nasal dorsum collapse is unclear but does not appear to be related to septal cartilage necrosis. These findings warrant a prospective analysis to identify risk factors for postoperative nasal deformities and data for counseling of patients.
Keywords: nasoseptal flap, skull base reconstruction
Introduction
As surgeons gain experience with endoscopic endonasal surgery (EES) of the skull base, there is increased attention to the morbidities of these procedures beyond major complications such as cerebrospinal fluid leaks and vascular injury. Although quality-of-life studies have addressed nasal and sinus morbidity, little attention has been paid to the aesthetic complications of EES, specifically nasal deformities such as septal perforations and nasal dorsum collapse (saddle nose deformity).
Over the past decade, the nasoseptal flap and other local vascularized flaps have become the mainstay of skull base reconstruction following EES, and they may contribute to the morbidity of surgery. Postoperative nasal crusting and drainage have been the best documented morbidities following EES, with one study reporting rates of 98% and 46%, respectively.1 Meanwhile, published rates of septal perforations with use of a vascularized flap range from 1.3% to 14.4%.2 3 Soudry et al hypothesized that in cases where a nasoseptal flap was used, a septal perforation could potentially result from an ischemic insult either from mucosal trauma or prolonged pressure on the capillary blood supply to the septal mucosa.2 In the same study, Soudry and colleagues also noted one case of saddle nose deformity in their population of 121 patients.
The senior authors of this paper anecdotally noted an increased incidence of nasal deformities following EES of the skull base including nasal dorsum collapse, some of which required secondary surgical interventions for correction. In light of these findings, this retrospective analysis sought to examine the prevalence and risk factors for external nasal deformities after EES of the skull base.
Methods
After institutional review board approval was obtained, a retrospective search of the senior authors' cases of ESS of the skull base from January 2011 to October 2013 was conducted. After patients were identified, their medical records and postoperative examinations were reviewed for basic patient demographics, type of pathology, intraoperative findings, postoperative complications, reconstructive technique, and nasal deformities. In this series, a nasal deformity was defined as nasal dorsum collapse, septal perforation, or a septal deviation that required secondary surgical correction. Endoscopic endonasal approaches (EEAs) to the skull base were divided into anterior skull base, transsellar, transclival, transpterygoid, and combined approaches. An approach was considered to be combined if it involved more than one of the previously mentioned anatomical subsites or if a cavernous dissection was performed in conjunction with a transsellar approach. The Student t test and Fisher exact test were used to assess statistical significance.
Results
This review identified 328 patients who underwent EES of the skull base. The average age of this cohort was 50.8 years with a sex distribution of 166 women and 162 men. Of these, 19 patients (5.8%) were found to have postoperative nasal dorsum collapse, 3 (0.9%) with new septal perforations and 2 (0.6%) with postoperative septal deviations requiring surgical correction. An example of one instance of postoperative nasal dorsum collapse is shown in Fig. 1. Although not reaching significance (p = 0.08), patients with nasal deformities were on average 6 years younger. There was no significant difference in average body mass index of those patients with nasal deformities compared with those without deformities (p = 0.33) (Table 1). A comparison between patients with benign or malignant pathology trended toward significance with roughly 17% of the cohort with malignancy experiencing postoperative changes compared with 6.5% of the cohort with a benign pathology (p = 0.08) (Table 1). Most of the EEAs in the nondeformity population were either transsellar or a combined approach, accounting for 46.1% and 41.1% of the approaches, respectively. In patients with nasal deformities, 8.3% of the approaches were transsellar compared with 75% involving multiple anatomical subsites (combined approaches). There were no anterior skull base approaches in the patients with external nasal deformities. The frequency of nasal deformities was more common in the setting of a combined approach compared with the sum of nasal deformities in all other approaches (p = 0.0021) (Table 2).
Fig. 1.

Patient with postoperative nasal dorsum collapse.
Table 1. Patient demographics and type of skull base pathology.
| Pathology | No. of patients without deformity | % | No. of patients with deformity | % | p value |
|---|---|---|---|---|---|
| Age, y | 51.27 | 44.73 | 0.08 | ||
| Sex | |||||
| Female | 153 | 13 | 0.83 | ||
| Male | 151 | 11 | |||
| BMI | 29.72 | 28.32 | 0.33 | ||
| Nasoseptal flap usage | 128.00 | 42.1 | 24.00 | 100 | 0.0001a |
| Benign pathology | 285 | 93.75 | 20 | 83.33 | 0.08b |
| Pituitary adenoma | 196 | 64.47 | 12 | 50.00 | |
| Rathke cleft cyst | 24 | 7.89 | 0 | 0.00 | |
| Meningioma | 15 | 4.93 | 4 | 16.67 | |
| Craniopharyngioma | 10 | 3.29 | 2 | 8.33 | |
| Spontaneous CSF leak | 11 | 3.62 | 0 | 0.00 | |
| Meningocele/Encephalocele | 9 | 2.96 | 1 | 4.17 | |
| Inverted papilloma | 4 | 1.32 | 0 | 0.00 | |
| Benign lesion NOS | 14 | 4.61 | 1 | 4.17 | |
| Infectious | 2 | 0.66 | 0 | 0.00 | |
| Malignant pathology | 19 | 6.25 | 4 | 16.67 | |
| Sinonasal malignancy | 11 | 3.62 | 2 | 8.33 | |
| Chordoma | 7 | 2.30 | 2 | 8.33 | |
| SNUC | 1 | 0.33 | 0 | 0.00 |
Abbreviations: BMI, body mass index; CSF, cerebrospinal fluid; NOS, not otherwise specified; SNUC, sinonasal undifferentiated carcinoma.
Indicates statistical significance.
Indicates comparison between benign and malignant pathology.
Table 2. Comparison of endoscopic endonasal approaches to the skull base between patients with and without nasal deformities.
| No. of patients without deformity | % | No. of patients with deformity | % | p value | |
|---|---|---|---|---|---|
| Anterior skull base | 23 | 7.57 | 0 | 0 | |
| Transsellar | 140 | 46.05 | 2 | 8.33 | |
| Transclival | 16 | 5.26 | 4 | 16.67 | |
| Combined | 125 | 41.12 | 18 | 75 | 0.0021a b |
Indicates statistical significance.
Indicates comparison between combined and all other approaches.
Regarding the methods of reconstruction, 152 patients (46%) underwent nasoseptal flap reconstruction in this total series. Only patients with a nasoseptal flap experienced postoperative deformities. Of the 152 patients with nasoseptal reconstruction, 24 (15.8%) experienced postoperative nasal deformities; there were no deformities in the remaining 176 patients (p = 0.0001) (Table 1). The rates of nasal dorsum collapse and septal perforations in patients with nasoseptal flap reconstruction were 12.5% and 1.3%, respectively. The time to presentation of these postoperative deformities was variable, with a range of 41 days to > 2 years.
Discussion
This study demonstrates an association of postoperative nasal deformities with nasoseptal flap reconstruction of the skull base as well as the extent of the surgical approach to the skull base. Nasoseptal flap reconstruction of the skull base may play a critical role in the formation of postoperative nasal deformities because only patients with nasoseptal flaps were found to have postoperative changes. Moreover, the extent of the approach to the skull base appears to be of importance because 75% of the patients with nasal deformities underwent combined approaches involving multiple anatomical subsites compared with less than half (41.1%) of the group without nasal deformities. Both of these comparisons were found to be statistically significant. This suggests that not only is the use of a nasoseptal flap a risk factor for postoperative nasal deformities, but it may also indicate that the size of the flap required for the reconstruction may play a role in the development of nasal deformities.
Although the advantages of nasoseptal flaps and other vascularized reconstruction techniques to prevent major postoperative complications are well documented, there are limited reports of nasal deformities associated with nasoseptal flap usage for reconstruction of the skull base. A recent retrospective review by Soudry et al noted a 14.4% rate of septal perforations and a < 1% rate of nasal dorsum collapse in their experience with nasoseptal flap reconstruction.2 These authors hypothesized that the underlying cause of septal perforations was an intraoperative ischemic insult. Interestingly, their one case of nasal dorsum collapse was not accompanied by a septal perforation. Another retrospective review of 152 patients with vascularized flaps for reconstruction by Thorp et al revealed a rate of septal perforations of 1.3% and did not mention the prevalence of nasal dorsum collapse.3 In our study, the rate of septal perforations was identical to that reported by Thorp and colleagues. Given the dramatic difference in incidence between septal perforations and dorsum collapse both in this study and the report by Soudry et al, it is unlikely that dorsal collapse is due to loss of septal cartilage anteriorly.
Although these nasal deformities are obviously a result of an insult to the structural integrity of the nasal framework, specifically the nasal septal cartilage, we suspect that an ischemic insult is an unlikely cause. Shin and colleagues indirectly tested this hypothesis in a report of 67 patients in which the authors raised bilateral nasoseptal flaps for transsellar approaches, theoretically inducing a transient ischemic event of the nasal septum similar to that which would be incurred by intraoperative compression of the septal blood supply by surgical instrumentation. The authors reported only one septal perforation and did not mention the incidence of nasal dorsum collapse.4 This equates to a rate of septal perforation of ∼ 1.5%, which is again similar both to the rate in our data and that reported by Thorp et al.
Given the retrospective nature of this review and the paucity of reports concerning postoperative nasal changes in these operations, it is difficult to ascertain which of the many insults to the nasal structure represents the exact etiology of these deformities in our patient population. According to Menick, nasal dorsum collapse may be categorized into four possible etiologies: iatrogenic injury (e.g., overaggressive rhinoplasty), trauma, loss of intranasal lining, or congenital insults.5 Certainly, EES may induce iatrogenic injury, trauma, or loss of intranasal lining. As Boccieri comments, delayed appearance of a crooked nose following nasal surgery may be a result of forces exerted on the nasal septum from the upper lateral cartilages or from those generated by the ligamentous connections to the bony septum. He further notes that prior trauma is capable of altering the integrity and ultrastructure of the cartilaginous septum itself.6 Capone and Papel reinforce that the cartilaginous vault is critical in the maintenance of dorsal height and tip projection.7 The association of dorsum collapse in our study with a combined approach may implicate that use of the four-handed surgical technique puts undue strain on the previously mentioned supportive structures, with traumatic disruption of the cartilaginous attachments to the nasal septum or direct trauma to the cartilaginous septal structure itself. Alternatively, the loss of posterior septal support (rostrum of sphenoid) may disrupt the vectors of septal support. Disruption or weakening of any of the numerous attachments to the septum may modify its appearance (Fig. 2).
Fig. 2.
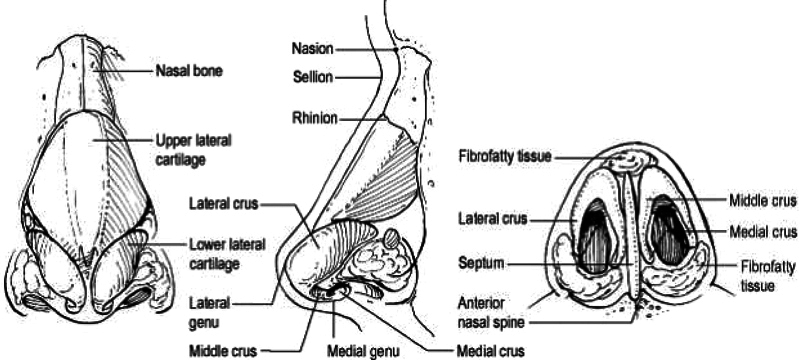
Numerous cartilaginous and ligamentous attachments that may play a role in postoperative nasal deformities if disrupted (reprinted with permission from the publisher of reference 5).
Regarding the loss of intranasal lining, it is well established that overdesiccation of the nasal cavity with subsequent necrosis of septal cartilage may lead to the saddle nose deformity associated with cocaine use, granulomatosis with polyangiitis (Wegener's), and other autoimmune or infectious causes.8 Although the use of a nasoseptal flap does lead to significant septal crusting postoperatively, de Almeida et al failed to demonstrate a difference in time to resolution of nasal crusting in patients with nasoseptal flap reconstruction and those without.1 Additionally, the characteristic progressive changes and necrosis of the nasal lining that accompanies this cause of dorsum collapse are fairly obvious on intranasal examination8 and not readily apparent in our patient population. The use of electrocautery for incision of the flap as well as the proximity of the incision to the nasal dorsum may be contributory factors due to soft tissue injury with scar contraction. Furthermore, although the comparison of the frequency of nasal deformities between benign and malignant pathologies only trended toward statistical significance, this may indicate a loss of intrinsic septal strength as a potential cause because most patients with malignant pathologies underwent irradiation.
Most patients have elected not to have correction of the nasal deformity. At least three of the patients in this study have undergone surgical correction of their external nasal deformities. In one case, a functional septorhinoplasty using an auricular cartilage graft to bolster the dorsal height was required. Given the nature of a tertiary referral center, many of these patients with acquired nasal deformities received follow-up at other institutions closer to home. This fact and the retrospective nature of this review may account for the variable time in presentation of nasal deformities. The actual incidence of nasal dorsum collapse may be underestimated by a retrospective review and patient variations in nasal structure (size and thickness of cartilage, thickness of skin, etc.). One hypothesis as to why there was a trend toward younger patients in the nasal deformity group is that these postoperative changes may be more noticeable in a younger population compared with the natural changes of the aging nose that may mask similar changes in older patients.
Because the exact etiology of these postoperative nasal deformities is unknown, further prospective analysis of this topic is required. One author recommends evaluating nasal dorsum collapse with a septal support test in which one places digital pressure on the nasal tip to assess the integrity of the septum itself as well as the components of the septal support system.9 Implementation of this assessment or similar examination techniques combined with a systematic method of classification of the deformity, such as that created by Durbec and Disant, may indicate a structural cause of the deformity.10 Prospective analysis with photo documentation will allow for both a more qualitative assessment of these deformities and a more accurate representation of when these occur. Analysis of other factors such as case duration and the design of the nasoseptal flap may help identify the risk factors for postoperative deformities.
In conclusion, although reconstruction of skull base defects with vascularized nasoseptal flaps has led to a significant reduction in major postoperative complications, there appear to be aesthetic complications associated with its use that have not been well documented. Based on these data, use of nasoseptal flap reconstruction alone is a risk factor for postoperative nasal deformities, most notably nasal dorsum collapse. Additionally, type and extent of the EEA to the skull base may also play a role in the development of these deformities. These findings warrant prospective analysis to identify risk factors for postoperative nasal deformities and provide data for the counseling of patients.
References
- 1.de Almeida J R, Snyderman C H, Gardner P A, Carrau R L, Vescan A D. Nasal morbidity following endoscopic skull base surgery: a prospective cohort study. Head Neck. 2011;33(4):547–551. doi: 10.1002/hed.21483. [DOI] [PubMed] [Google Scholar]
- 2.Soudry E, Psaltis A J, Lee K H, Vaezafshar R, Nayak J V, Hwang P H. Complications associated with the pedicled nasoseptal flap for skull base reconstruction. Laryngoscope. 2015;125(1):80–85. doi: 10.1002/lary.24863. [DOI] [PubMed] [Google Scholar]
- 3.Thorp B D, Sreenath S B, Ebert C S, Zanation A M. Endoscopic skull base reconstruction: a review and clinical case series of 152 vascularized flaps used for surgical skull base defects in the setting of intraoperative cerebrospinal fluid leak. Neurosurg Focus. 2014;37(4):E4. doi: 10.3171/2014.7.FOCUS14350. [DOI] [PubMed] [Google Scholar]
- 4.Shin J H, Kang S G, Kim S W. et al. Bilateral nasoseptal flaps for endoscopic endonasal transsphenoidal approach. J Craniofac Surg. 2013;24(5):1569–1572. doi: 10.1097/SCS.0b013e31829a8105. [DOI] [PubMed] [Google Scholar]
- 5.Menick F J. Philadelphia, PA: Saunders Elsevier; 2009. The interface of cosmetic and reconstructive rhinoplasty: the crucified tip, the saddlenose and the continuum of reconstruction and cosmesis. [Google Scholar]
- 6.Boccieri A. The crooked nose. Acta Otorhinolaryngol Ital. 2013;33(3):163–168. [PMC free article] [PubMed] [Google Scholar]
- 7.Capone R B, Papel I D. Baltimore, MD: Lippincott Williams & Wilkins; 2014. The nasal dorsum: management of the upper two-thirds of the nose. [Google Scholar]
- 8.Menick F J, Salibian A. Primary intranasal lining injury cause, deformities, and treatment plan. Plast Reconstr Surg. 2014;134(5):1045–1056. doi: 10.1097/PRS.0000000000000694. [DOI] [PubMed] [Google Scholar]
- 9.Daniel R K. Rhinoplasty: septal saddle nose deformity and composite reconstruction. Plast Reconstr Surg. 2007;119(3):1029–1043. doi: 10.1097/01.prs.0000252503.30804.5e. [DOI] [PubMed] [Google Scholar]
- 10.Durbec M, Disant F. Saddle nose: classification and therapeutic management. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131(2):99–106. doi: 10.1016/j.anorl.2013.01.006. [DOI] [PubMed] [Google Scholar]


