Abstract
Objective
To determine the effect of hospital characteristics on failure to rescue after high-risk surgery in Medicare Beneficiaries.
Summary Background Data
Reducing failure to rescue events is a common quality target for U.S. hospitals. Little is known about which hospital characteristics influence this phenomenon and more importantly by how much.
Methods
We identified 1,945,802 Medicare beneficiaries undergoing one of six high-risk general or vascular operations between 2007-10. Using multilevel mixed-effects logistic regression modeling, we evaluated how failure to rescue rates were influenced by specific hospital characteristics previously associated with postsurgical outcomes. We used variance partitioning to determine the relative influence of patient and hospital characteristics on the between-hospital variability in failure to rescue rates.
Results
Failure to rescue rates varied up to 11-fold between very high and very low mortality hospitals. Comparing the highest and lowest mortality hospitals, we observed that teaching status (range: OR 1.08-1.54), high hospital technology (range: OR 1.08-1.58), increasing nurse-to-patient ratio (range: OR 1.02-1.14), and presence of >20 ICU beds (range: OR 1.09-1.62) significantly influenced failure to rescue rates for all procedures. When taken together, hospital and patient characteristics accounted for 12% (lower extremity revascularization) to 57% (esophagectomy) of the observed variation in failure to rescue rates across hospitals.
Conclusions
While several hospital characteristics are associated with lower failure to rescue rates, these macro-system factors explain a small proportion of the variability between hospitals. This suggests that micro-system characteristics, such as hospital culture and safety climate, may play a larger role in improving a hospital's ability to manage postoperative complications.
Introduction
In 2010, the National Quality Forum (NQF) formally endorsed failure to rescue as a quality measure for surgical care. It is now widely accepted as a principal driver of variation in postoperative mortality between hospitals.1, 2 Though its mechanisms are incompletely understood, national and regional surgical quality collaboratives are providing hospitals with their own data on failure to rescue as a means of facilitating safer care practices.3, 4 Reporting within these collaboratives or publicly through efforts such as the Centers for Medicare and Medicaid Services (CMS) Value Based Purchasing Program (VBP) have made hospitals' data on surgical safety more accessible to patient and policymaker scrutiny.
The extent to which specific hospital characteristics influence failure to rescue is unclear. Several factors (e.g. lower nurse to patient ratios) are associated with lower failure to rescue rates in surgical patients.5-9 However, prior work is limited to single-center studies or those confined to specific patient populations.10-12 These current studies fail to answer two important questions. First, it is unclear how hospital characteristics influence outcomes for patients undergoing different operations within the same center. Second, the extent to which hospital characteristics contribute to the wide variation in failure to rescue rates across hospitals is not known. Understanding these issues is critical as hospitals determine whether augmenting available resources will be met with tangible improvements in surgical quality and safety.
Using national Medicare data, we sought to determine the influence of hospital characteristics on failure to rescue following common general and vascular surgery procedures. We then determined the relative effect of hospital characteristics on the between-hospital variation in failure to rescue, after adjusting for patient factors and procedural volume, to assess whether modifying these characteristics would significantly augment postoperative mortality.
Methods
Patient Population and Data Source
We used national data from the Medicare Provider Analysis and Review (MEDPAR) files for the years 2007 thru 2010. The Centers for Medicare & Medicaid Services (CMS) maintains this database using claims submitted by hospitals where Medicare beneficiaries receive care. Patient-level data includes age, sex, race, 29 Elixhauser comorbidities (principal and secondary diagnosis codes), procedural codes, 30-day morbidity and mortality, and information on length of hospital stay.13 We excluded patients under age 65 or those with incomplete clinical data in the registry. We selected patients undergoing six common general or vascular surgical operations using International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes. Specifically, we identified patients undergoing colectomy, pancreatectomy, esophagectomy, abdominal aortic aneurysm repair, lower-extremity revascularization, or lower extremity amputation. We combined general (colectomy, pancreatectomy, esophagectomy) and vascular (AAA repair, LE revascularization, LE amputation) operations in to two groups to improve generalizability of the results.
Hospital Characteristics
Using the MEDPAR file claims data; we calculated the annual operative volume of each hospital using hospitals' unique Medicare Provider Identification numbers. Data on hospital structure and resources was derived from the American Hospital Association (AHA) Annual Survey Database. This data included hospital bed size and occupancy, annual inpatient surgical volumes, Council of Teaching Hospital status, intensive care unit (ICU) beds, nurse staffing, and hospital technology. We defined nurse-to-patient ratio as [nursing full-time equivalents (FTE) × 1,768 / adjusted patient days] as has been previously described.9 This method calculates the number of nurse hours per patient day and was treated as a continuous variable in all analyses. We dichotomized the remaining outcomes in the interest of improving generalizability. Hospital bed size greater than 200 beds was used to differentiate hospitals above and below the median for hospitals in our patient population. We calculated percent hospital occupancy as average daily census divided by the hospital bed size. This was dichotomized at greater than 50%.11 Similar to overall bed size, we calculated the total number of ICU beds in each hospital and dichotomized this variable at a median of greater than 20 beds. Finally, we defined hospital technology dichotomously as hospitals performing open heart surgery or solid organ transplantation.14 For all analyses, hospital characteristics and cut-points for dichotomizing were defined a priori.
Outcomes
Our primary outcomes for this analysis were 30-day mortality, major complications, and failure to rescue. Major complications were identified by ICD-9-CM codes for the following occurrence categories: pulmonary failure (518.81, 518.4, 518.5, 518.8), pneumonia (481, 482.0–482.9, 483, 484, 485, 507.0), myocardial infarction (410.00–410.91), deep venous thrombosis/pulmonary embolism (415.1, 451.11, 451.19, 451.2, 451.81, 453.8), renal failure (584), surgical site infection (958.3, 998.3, 998.5, 998.59, 998.51), gastrointestinal bleeding (530.82, 531.00–531.21, 531.40, 531.41, 531.60, 531.61, 532.00–532.21, 532.40, 532.41, 532.60, 532.61, 533.00–533.21, 533.40, 533.41, 533.60, 533.61, 534.00–534.21, 534.40, 534.41, 534.60, 534.61, 535.01, 535.11, 535.21, 535.31, 535.41, 535.51, 535.61, 578.9), and hemorrhage (998.1). This method of identifying complications with administrative data has been previously described and validated.15, 16 Complication rates are consistent with previously published work using similar patient populations and datasets. We defined a failure to rescue as mortality in a patient with at least one major complication.
Statistical Analysis
We compared demographic, comorbidity, and length of stay differences between hospitals with Student's t-test, Chi-squared, Mann-U Whitney test, and analysis of variance (ANOVA) as appropriate. Using multilevel mixed-effects regression modeling, we first grouped hospitals in to quintiles by risk- and reliability-adjusted 30-day mortality. To do this, we used a logistic regression model with 30-day mortality as the primary outcome, including patient characteristics such as age, race, urgency of operation, operative approach (e.g. endovascular) where appropriate, and 29 Elixhauser comorbidities as fixed-effects covariates.13 All estimates were adjusted for clustering of patients within hospitals. We then adjusted our estimates for reliability using empirical Bayes methods in order to reduce random variation attributed to statistical noise that can result from hospitals with small sample size (case volume).17 The c-statistic for all models ranged between 0.77 and 0.92, with good discriminatory power on the basis of Hosmer-Lemeshow test.
Next, we focused our analysis of hospital characteristics on those hospitals in the highest and lowest quintiles of risk- and reliability-adjusted mortality for each procedure. We evaluated the effect of each hospital characteristic individually using logistic regression. Failure to rescue served as our primary outcome and each characteristic was assessed in the model as having a fixed-effect.
For each procedure, we then conducted model testing to determine the relative contribution of patient-level covariates, annual procedure volume, and hospital characteristics to the variation in failure to rescue rates observed between hospitals.18, 19 We first quantified the variance ascribed to hospital level random effects using an empty mixed-effects logistic regression model (xtmelogit in Stata v. 12.1). We generated models with failure to rescue as our primary outcome using patient-level covariates first. We sequentially added hospital volume and hospital characteristics, each time generating a new model. The relative decrease in variance attributed to hospital-level random effects was then calculated to determine each parameters influence on observed variation.
A significance level of α=0.05 was used. All statistical analyses were performed using Stata statistical software version 12.1 (College Station, Texas). This study was approved by the University of Michigan Institutional Review Board.
Results
Patient Characteristics
For all procedures, patient characteristics were similar across quintiles of hospital mortality. (Table 1) There were no differences in median age, gender distribution, or overall comorbid disease burden between hospitals for all procedures. There were significant differences in the percentage of patients of non-white race for all procedures – with an overall higher proportion of non-white patients being treated at high mortality hospitals (10-34%) compared to low mortality hospitals (8-30%). There were also statistically significant differences in overall hospital length of stay across hospitals for each procedure. The number of hospitals included in this study ranged from 1,681 for esophagectomy to 3,827 for colectomy.
Table 1. Patient Characteristics by Procedure and Hospital Quintiles of Mortality.
| Quintile of Hospital Mortality | |||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Very Low | Low | Medium | High | Very High | p-valuea | |
| Colectomy | |||||||
| n | 98,860 | 98,685 | 98,636 | 98,728 | 98,715 | - | |
| Median age, y (IQR) | 75 (13) | 75 (12) | 75 (12) | 75 (13) | 74 (13) | 0.67 | |
| Male sex, % | 42% | 42% | 42% | 43% | 43% | 0.29 | |
| Non-white race, % | 12% | 14% | 13% | 14% | 15% | <0.01 | |
| Mean number comorbidities | 2 | 2 | 2 | 2 | 2 | 0.35 | |
| Median length of stay, d (IQR) | 8 (8) | 8 (9) | 8 (9) | 8 (9) | 8 (9) | <0.01 | |
| Pancreatectomy | |||||||
| n | 3,522 | 3,524 | 3,415 | 3,484 | 3,483 | - | |
| Median age, y (IQR) | 73 (9) | 73 (10) | 73 (10) | 73 (10) | 73 (10) | 0.88 | |
| Male sex, % | 51% | 50% | 49% | 51% | 50% | 0.61 | |
| Non-white race, % | 10% | 13% | 14% | 17% | 15% | <0.01 | |
| Mean number comorbidities | 2 | 2 | 2 | 2 | 2 | 0.44 | |
| Median length of stay, d (IQR) | 10 (8) | 11 (9) | 12 (11) | 12 (11) | 12 (12) | <0.01 | |
| Esophagectomy | |||||||
| n | 2,796 | 2,551 | 2,674 | 2,675 | 2,665 | - | |
| Median age, y (IQR) | 72 (9) | 72 (10) | 72 (9) | 72 (10) | 72 (9) | 0.93 | |
| Male sex, % | 75% | 75% | 72% | 73% | 74% | 0.16 | |
| Non-white race, % | 8% | 10% | 14% | 15% | 13% | <0.01 | |
| Mean number comorbidities | 2 | 2 | 2 | 2 | 2 | 0.34 | |
| Median length of stay, d (IQR) | 11 (11) | 11 (11) | 13 (12) | 12 (9) | 13 (11) | <0.01 | |
| Abdominal Aortic Aneurysm Repair | |||||||
| n | 37,883 | 37,746 | 37,699 | 38,030 | 37,491 | - | |
| Median age, y (IQR) | 75 (11) | 75 (11) | 75 (11) | 74 (11) | 74 (11) | 0.15 | |
| Male sex, % | 72% | 72% | 72% | 72% | 71% | 0.44 | |
| Non-white race, % | 8% | 9% | 11% | 10% | 10% | <0.01 | |
| Mean number comorbidities | 2 | 2 | 2 | 2 | 2 | 0.19 | |
| Median length of stay, d (IQR) | 5 (7) | 4 (6) | 4 (6) | 4 (6) | 4 (6) | <0.01 | |
| Lower Extremity Revascularization | |||||||
| n | 136,578 | 135,925 | 137,053 | 135,771 | 135,751 | - | |
| Median age, y (IQR) | 72 (15) | 72 (15) | 71 (14) | 71 (14) | 70 (14) | 0.35 | |
| Male sex, % | 53% | 53% | 54% | 53% | 53% | 0.73 | |
| Non-white race, % | 23% | 21% | 23% | 24% | 24% | 0.02 | |
| Mean number comorbidities | 3 | 3 | 3 | 3 | 3 | 0.49 | |
| Median length of stay, d (IQR) | 4 (7) | 4 (8) | 4 (7) | 4 (7) | 5 (7) | <0.01 | |
| Lower Extremity Amputation | |||||||
| n | 136,689 | 136,322 | 141,769 | 138,259 | 136,609 | - | |
| Median age, y (IQR) | 69 (18) | 69 (17) | 68 (16) | 69 (17) | 67 (16) | 0.81 | |
| Male sex, % | 63% | 61% | 64% | 61% | 62% | 0.91 | |
| Non-white race, % | 30% | 28% | 36% | 33% | 34% | 0.04 | |
| Mean number comorbidities | 3 | 3 | 3 | 3 | 3 | 0.28 | |
| Median length of stay, d (IQR) | 10 (10) | 10 (11) | 9 (11) | 10 (10) | 9 (10) | <0.01 | |
p-values indicate the difference in trend across all quintiles of hospital mortality. Results were similar when comparing very high to very low mortality quintiles alone.
Hospital Mortality, Major Complications, and Failure to Rescue
Comparing very low and very high mortality centers, hospital mortality varied between 1.4-fold following lower extremity amputation to 7-fold following pancreatectomy. (Table 2) There was a significant difference in the incidence of major complications between very low and very high mortality hospitals following colectomy (OR 1.2, 95% CI 1.2 to 1.3), pancreatectomy (OR 2.0, 95% CI 1.7 to 2.3, esophagectomy (OR 2.1, 95% CI 1.8 to 2.4), and lower extremity revascularization (OR 1.2, 95% CI 1.1 to 1.2). No significant differences in the incidence of major complications were observed following abdominal aortic aneurysm repair (OR 1.0, 95% CI 0.9 to 1.1) or lower extremity amputation (OR 1.0, 95% CI 0.9 to 1.1). There were statistically significant differences in failure to rescue rates between very low and very high mortality hospitals for all procedures. Patients treated at very low compared to very high mortality hospitals had an increased odds of dying after a major complication – ranging from 1.9 (95% CI 1.8 to 2.0) after lower extremity revascularization to 18.2 (95% CI 11.4 to 21.4) after esophagectomy.
Table 2. Rates of Major Complications, Mortality, and Failure to Rescue by Procedure and Quintiles of Hospital Mortality.
| Quintile of Hospital Mortality | |||||||
|---|---|---|---|---|---|---|---|
| Procedure | Very Low | Low | Medium | High | Very High | Odds Ratio, Very Low v. Very High (95% CI) | |
| Colectomy | |||||||
| Major complications | 28.2% | 28.8% | 29.7% | 30.6% | 32.5% | 1.2 (1.2-1.3) | |
| Mortality | 6.6% | 7.8% | 8.6% | 9.5% | 11.3% | 2.4 (2.3-2.5) | |
| Failure to Rescue | 15.6% | 18.8% | 21.7% | 25.2% | 30.1% | 2.3 (2.2-2.4) | |
| Pancreatectomy | |||||||
| Major complications | 24.1% | 30.7% | 31.4% | 32.6% | 38.9% | 2.0 (1.7-2.3) | |
| Mortality | 2.1% | 3.0% | 4.1% | 5.9% | 14.1% | 7.6 (5.9-9.7) | |
| Failure to Rescue | 4.0% | 4.7% | 8.2% | 11.7% | 35.5% | 13.2 (8.2-21.4) | |
| Esophagectomy | |||||||
| Major complications | 33.5% | 37.8% | 41.1% | 37.8% | 50.9% | 2.1 (1.8-2.4) | |
| Mortality | 3.4% | 4.7% | 6.1% | 9.1% | 20.6% | 7.4 (5.9-9.3) | |
| Failure to Rescue | 6.8% | 7.3% | 9.4% | 16.1% | 41.8% | 18.2 (11.4-29.1) | |
| Abdominal Aortic Aneurysm Repair | |||||||
| Major complications | 26.2% | 24.2% | 25.0% | 25.3% | 25.9% | 1.0 (0.9-1.1) | |
| Mortality | 4.4% | 5.5% | 6.2% | 6.9% | 8.4% | 2.6 (2.5-2.8) | |
| Failure to Rescue | 12.2% | 13.8% | 16.7% | 21.6% | 28.2% | 2.8 (2.6-3.0) | |
| Lower Extremity Revascularization | |||||||
| Major complications | 25.9% | 26.5% | 27.7% | 28.7% | 29.7% | 1.2 (1.1-1.2) | |
| Mortality | 3.8% | 4.6% | 5.1% | 5.6% | 6.6% | 2.3 (2.2-2.4) | |
| Failure to Rescue | 9.2% | 10.4% | 11.4% | 13.6% | 16.1% | 1.9 (1.8-2.0) | |
| Lower Extremity Amputation | |||||||
| Major complications | 35.2% | 34.0% | 32.6% | 33.9% | 34.3% | 1.0 (0.9-1.1) | |
| Mortality | 8.5% | 9.5% | 10.1% | 10.7% | 12.0% | 2.5 (2.4-2.7) | |
| Failure to Rescue | 11.3% | 13.7% | 16.3% | 21.0% | 25.3% | 2.7 (2.5-2.8) | |
Hospital Characteristics Associated with Failure to Rescue
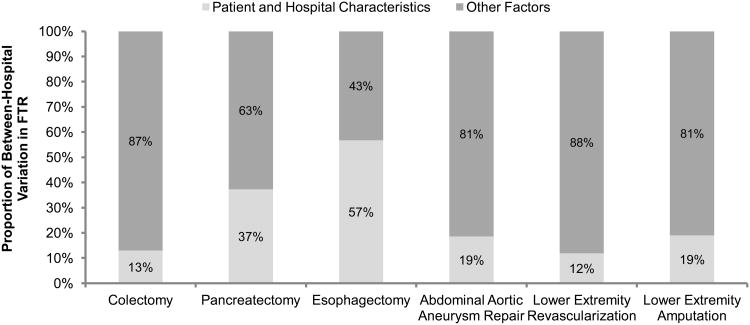
When comparing very low and very high mortality hospitals, teaching status (range: OR 1.08 to 1.54), high hospital technology (range: OR 1.08 to 1.58), increasing nurse-to-patient ratio (range: OR 1.02 to 1.14), and presence of an ICU >20 beds (range: OR 1.09 to 1.62) significantly influenced failure to rescue rates for all procedures. (Table 3) Hospital size greater than 200 beds was associated with failure to rescue (range: OR 1.15 to 1.93) for all procedures, except abdominal aortic aneurysm repair. Hospital occupancy greater than 50% was associated with failure to rescue (range: OR 1.14 to 1.76) for colectomy, pancreatectomy, and abdominal aortic aneurysm repair only. For each procedure, there was variability in influence of hospital characteristics on failure to rescue between very low and very high mortality hospitals. For example, following colectomy, hospital bed size had the largest influence on failure to rescue (OR 1.18, 95% CI 1.10 to 1.36). In contrast, following abdominal aortic aneurysm repair, hospital occupancy had the largest influence (OR 1.32, 95% CI 1.20 to 1.43). Taken together, patient and procedural characteristics, procedure volume, and hospital characteristics accounted for 12% (lower extremity revascularization) to 57% (esophagectomy) of the variability in failure to rescue between hospitals. (Figure 1) Relative to the total amount of variation explained by all factors considered– hospital characteristics explained between 36% (abdominal aortic aneurysm repair) and 80% (esophagectomy) of the observed variation.
Table 3. Hospital Characteristics Associated with Failure to Rescue Between Very High and Very Low Mortality Hospitals.
| Colectomy | Pancreatectomy | Esophagectomy | Abdominal Aortic Aneurysm Repair | Lower Extremity Revascularization | Lower Extremity Amputation | |
|---|---|---|---|---|---|---|
| Hospital Characteristic | Odds Ratio of Failure to Rescue (95% CI) | |||||
| Hospital bed size <200 | 1.18 (1.10-1.36) | 1.77 (1.22-1.93) | 1.93 (1.45-1.99) | 1.02 (0.77-1.23) | 1.15 (1.02-1.25) | 1.28 (1.12-1.42) |
| Decreasing nurse-patient ratio | 1.02 (1.01-0.03) | 1.14 (1.08-1.20) | 1.08 (1.02-1.14) | 1.02 (1.01-1.04) | 1.02 (1.01-1.03) | 1.02 (1.01-1.03) |
| Hospital occupancy <50% | 1.14 (1.08-1.19) | 1.76 (1.50-1.88) | 1.33 (0.83-1.61) | 1.32 (1.20-1.43) | 1.08 (1.00-1.15) | 1.10 (0.99-1.21) |
| No teaching status (COTHa) | 1.08 (1.05-1.12) | 1.32 (1.09-1.49) | 1.54 (1.39-1.66) | 1.16 (1.09-1.22) | 1.09 (1.05-1.13) | 1.08 (1.02-1.14) |
| Intensive care beds <20 | 1.09 (1.05-1.12) | 1.58 (1.38-1.71) | 1.62 (1.46-1.73) | 1.18 (1.11-1.25) | 1.13 (1.03-1.16) | 1.14 (1.08-1.19) |
| Absence of high hospital technology | 1.08 (1.05-1.12) | 1.48 (1.27-1.63) | 1.58 (1.41-1.69) | 1.25 (1.18-1.31) | 1.13 (1.08-1.17) | 1.15 (1.09-1.21) |
Council of teaching hospitals (COTH)
Figure 1.
Identifying sources of between-hospital variation in failure to rescue rates. Patient characteristics, procedural volume, and hospital characteristics were compiled in aggregate. The remaining variation is explained by other factors.
Discussion
Safe and efficient surgical care is a clinical imperative for hospitals that perform major surgery. We used data from six common, high-risk, surgical procedures in the national Medicare population to examine the influence of hospital characteristics on failure to rescue. As previously observed, failure to rescue rates varied widely across hospitals for all procedures and were highly correlated with postoperative mortality. Hospital bed size, ICU availability, technology, nurse staffing, occupancy, and teaching status were all associated with differences in failure to rescue between very low and very high mortality hospitals. Despite the association with failure to rescue, these factors along with patient characteristics and surgical volume explain only a small proportion of the variability in failure to rescue that exists between hospitals in the United States.
Interest in the relationship between hospital characteristics and patient safety is not new.20 Within the surgical literature, the emergence of failure to rescue as a quality metric has increased interest in understanding what factors influence quality and safety. Prior work studying failure to rescue in patients undergoing pancreatic or colorectal resections identified the importance of macro-system hospital characteristics such as bed size, ICU availability, and teaching status.10, 11 The nursing literature represents the most active attempts to understand the relationship between the presence and utilization resources and failure to rescue.5, 6, 21, 22 Not only is the presence of lower nurse-to-patient ratios important in complication rescue, but also it appears that nurses physical time with the patient is associated with improved outcomes.23 On a broader scale, hospital credentialing is another example of an attempt to improve care through concentration of hospital resources. Steering patients towards certain centers for bariatric (Centers of Excellence) or oncologic (Comprehensive Cancer Centers) procedures, for example, all attempt to consolidate care where hospital resources and characteristics are most appropriate to deliver safe and effective care.24, 25 The efficacy of efforts such as these are debated widely.
Since it was first described by Silber and colleagues, failure to rescue has been largely regarded as a hospital-level phenomenon – thereby necessitating some association with hospital characteristics.2 However, the relationship between fixed aspects of a hospital and the management of postoperative complications is complex. Surgeon and hospital experience are also intimately associated with outcomes.26, 27 The mechanism by which these factors work in conjunction with hospital resources to augment failure to rescue are not well understood.28 Our results suggest that hospital size, occupancy, ICU availability, teaching status, and technology offer a survival advantage to patients undergoing major surgery. While significant, these factors are not easily remediable and likely serve as proxies for an overall pedigree of hospital with sufficient resources to manage the complexity of high-risk surgical patients and their complications. While nurse staffing may be more readily augmented, the exact mechanism by which lower nurse-to-patient ratios reduce failure to rescue events is unknown. It is plausible that this characteristic also serves as a surrogate for a hospital's preparedness to perform high-risk operations. Despite these associations, hospital characteristics, patient factors, and operative volume explain a small proportion of the variation in failure to rescue rates that exist across hospitals. Potentially these factors act more as threshold barriers to safety when performing complex surgeries. There is emerging evidence to suggest that caregiver attitudes, safety culture, and care process adherence may be more actionable means of improving surgical care.29, 30
This study has numerous limitations and it is important to note that this work does not suggest causation. The use of Medicare data restricts this study to a particular patient population, which may reduce generalizability. The use of administrative data also imposes limitation on adequate risk-adjustment, though our approach using the Elixhauser method is widely accepted.31 We attempted to address possible inaccuracies in identification of complications by restricting our analysis to a validated subset of events known to have high sensitivity and specificity.15 Our results may not be generalizable to other procedures. We attempted to select a group of procedures that represent a spectrum of major general and vascular surgery. Further, all analyses were carried out for each procedure individually. There may be an element of information bias in using the AHA Annual Hospital Survey data to identify hospital characteristics given that this information is self-reported by each hospital. Finally, operative mortality is a rare event and issues of data reliability are real. We have attempted to address this in all analyses using empirical Bayes methods as previously described.17
The exact relationship between hospital characteristics and failure to rescue after major surgery is unknown. Though significant associations exist, these factors do not explain the wide variation in outcomes observed between U.S. hospitals. There were some exceptions to this observation, especially for pancreatectomy and esophagectomy. This observation may be due to the fact that many centers perform only a handful of these operations annually. The majority cluster at hospitals with substantial experience. These centers tend to be larger and resource-rich. Some baseline structural composition of acute care hospitals is likely necessary to perform high-risk surgeries. However, augmentation of hospital characteristics alone will likely be of marginal benefit. Emerging efforts to improve hospitals' effectiveness in responding to patients in crisis may address the quality targets sought by hospitals and described in this study.32 This involves a more complex understanding of the hospital system, caregivers, and available resources. Implementing process methods developed and popularized by industry may allow hospitals to effectively learn from failure to rescue events (e.g. root cause analysis).33 Hospital process analysis is demanding of both manpower and capital. However, coordinated and deliberate efforts to understand failure to rescue may be necessary to facilitate the cultural changes that lead to safer patient care.
Acknowledgments
This work was funded NIH/NIA R01 AG042340-01 and K08HS023621 issued to Amir A. Ghaferi.
Footnotes
KHS no conflicts of interest.
JBD reports having equity in Arbor Metrix. The company had no role in this study.
AAG no conflicts of interest.
References
- 1.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 2.Silber JH, Williams SV, Krakauer H, et al. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care. 1992;30:615–29. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Sheetz KH, Waits SA, Krell RW, et al. Improving mortality following emergent surgery in older patients requires focus on complication rescue. Ann Surg. 2013;258:614–7. doi: 10.1097/SLA.0b013e3182a5021d. discussion 617-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wakeam E, Hyder JA, Tsai TC, et al. J Surg Res. 2014. Complication timing and association with mortality in the American College of Surgeons' National Surgical Quality Improvement Program database. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Harless DW, Mark BA. Nurse staffing and quality of care with direct measurement of inpatient staffing. Med Care. 2010;48:659–63. doi: 10.1097/MLR.0b013e3181dbe200. [DOI] [PubMed] [Google Scholar]
- 6.Aiken LH, Cimiotti JP, Sloane DM, et al. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care. 2011;49:1047–53. doi: 10.1097/MLR.0b013e3182330b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hammer JA, Jones TL, Brown SA. Rapid response teams and failure to rescue: one community's experience. J Nurs Care Qual. 2012;27:352–8. doi: 10.1097/NCQ.0b013e31825a8e2f. [DOI] [PubMed] [Google Scholar]
- 8.Mark BA, Harless DW, Spetz J, et al. California's minimum nurse staffing legislation: results from a natural experiment. Health Serv Res. 2013;48:435–54. doi: 10.1111/j.1475-6773.2012.01465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spetz J, Donaldson N, Aydin C, et al. How many nurses per patient? Measurements of nurse staffing in health services research. Health Serv Res. 2008;43:1674–92. doi: 10.1111/j.1475-6773.2008.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henneman D, van Leersum NJ, Ten Berge M, et al. Ann Surg Oncol. 2013. Failure-to-Rescue After Colorectal Cancer Surgery and the Association with Three Structural Hospital Factors. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.Ghaferi AA, Osborne NH, Birkmeyer JD, et al. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–30. doi: 10.1016/j.jamcollsurg.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Tan HJ, Wolf JS, Jr, Ye Z, et al. Complications and failure to rescue after laparoscopic versus open radical nephrectomy. J Urol. 2011;186:1254–60. doi: 10.1016/j.juro.2011.05.074. [DOI] [PubMed] [Google Scholar]
- 13.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45:918–25. doi: 10.1097/MLR.0b013e31812e01cc. [DOI] [PubMed] [Google Scholar]
- 15.Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care. 1994;32:700–15. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Weingart SN, Iezzoni LI, Davis RB, et al. Use of administrative data to find substandard care: validation of the complications screening program. Med Care. 2000;38:796–806. doi: 10.1097/00005650-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Dimick JB, Ghaferi AA, Osborne NH, et al. Reliability adjustment for reporting hospital outcomes with surgery. Ann Surg. 2012;255:703–7. doi: 10.1097/SLA.0b013e31824b46ff. [DOI] [PubMed] [Google Scholar]
- 18.Birkmeyer NJ, Dimick JB, Share D, et al. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010;304:435–42. doi: 10.1001/jama.2010.1034. [DOI] [PubMed] [Google Scholar]
- 19.Sheetz KH, Dimick JB, Ghaferi AA. The association between hospital care intensity and surgical outcomes in medicare patients. JAMA Surg. 2014;149:1254–9. doi: 10.1001/jamasurg.2014.552. [DOI] [PubMed] [Google Scholar]
- 20.Hartz AJ, Krakauer H, Kuhn EM, et al. Hospital characteristics and mortality rates. N Engl J Med. 1989;321:1720–5. doi: 10.1056/NEJM198912213212506. [DOI] [PubMed] [Google Scholar]
- 21.Aiken LH, Sochalski J, Anderson GF. Downsizing the hospital nursing workforce. Health Aff (Millwood) 1996;15:88–92. doi: 10.1377/hlthaff.15.4.88. [DOI] [PubMed] [Google Scholar]
- 22.McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Res Nurs Health. 2012;35:566–75. doi: 10.1002/nur.21503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seago JA, Williamson A, Atwood C. Longitudinal analyses of nurse staffing and patient outcomes: more about failure to rescue. J Nurs Adm. 2006;36:13–21. doi: 10.1097/00005110-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Hollenbeak CS, Rogers AM, Barrus B, et al. Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery. 2008;144:736–43. doi: 10.1016/j.surg.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 25.Friese CR, Earle CC, Silber JH, et al. Hospital characteristics, clinical severity, and outcomes for surgical oncology patients. Surgery. 2010;147:602–9. doi: 10.1016/j.surg.2009.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 27.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–37. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]
- 29.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 30.Birkmeyer NJ, Finks JF, Greenberg CK, et al. Safety culture and complications after bariatric surgery. Ann Surg. 2013;257:260–5. doi: 10.1097/SLA.0b013e31826c0085. [DOI] [PubMed] [Google Scholar]
- 31.Dubois RW, Rogers WH, Moxley JH, 3rd, et al. Hospital inpatient mortality. Is it a predictor of quality? N Engl J Med. 1987;317:1674–80. doi: 10.1056/NEJM198712243172626. [DOI] [PubMed] [Google Scholar]
- 32.Pronovost PJ, Berenholtz SM, Goeschel CA, et al. Creating high reliability in health care organizations. Health Serv Res. 2006;41:1599–617. doi: 10.1111/j.1475-6773.2006.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghaferi AA, Dimick JB. Understanding Failure to Rescue and Improving Safety Culture. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001135. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]