Abstract
Objectives
Early childhood caries (ECC) is rampant among American Indian children, but there has been relatively little study of this problem. This paper reports on risk factors for caries for a group of American Indian children at age 36 months as part of a longitudinal study.
Methods
Pregnant women from a Northern Plains Tribal community were recruited to participate in a longitudinal study of caries and caries risk factors. Standardized dental examinations were completed on children and questionnaires were completed by mothers at baseline and when children were 4, 8, 12, 16, 22, 28 and 36 months of age. Examinations were surface-specific for dental caries, and the questionnaires collected data on demographic, dietary and behavioral factors. Non-parametric bivariate tests and logistic regression models were used to identify risk factors for caries at 36 months, and negative binomial regression was used to identify factors related to caries severity (dmf counts).
Results
Among the 232 children, and caries prevalence for cavitated lesions was 80%, with an additional 15% having only non-cavitated lesions. The mean dmfs was 9.6, and of the total dmfs, nearly 62% of affected surfaces were decayed, 31% were missing, and 7% were filled. Logistic regression identified higher added sugar beverage consumption, younger maternal age at baseline, higher maternal DMFS at baseline, and greater number of people in the household as significant (p<0.05) risk factors. Negative binomial regression found that only maternal DMFS was associated with child dmf counts.
Conclusions
By the age of 36 months, dental caries is nearly universal in this population of American Indian children. Caries risk factors included sugared beverage consumption, greater household size and maternal factors, but further analyses are needed to better understand caries in this population.
Keywords: Dental Caries, Children, Risk factors, Oral health disparities
Introduction
It is well-documented that dental caries prevalence among young American Indian and Alaska Native (AI/AN) children has remained high for many years1–3. At the same time, while there has recently been a slight increase caries prevalence among the youngest U.S. children, there has been a steady decline in caries prevalence among all U.S. children over the past 30+ years4,5. As a result, there is a very large disparity in caries prevalence between AI/AN children and other children. Specifically, decay experience among AI/AN 2- to 5-year old children was 62% as reported in the 2010 Indian Health Service (IHS) Oral Health Survey of Preschool Children1, while caries prevalence was 25% for non-Hispanic white children, 32% for Black children and 42% for Mexican-American children among 2- to 5-year-olds nationally, as reported from NHANES 1999–2004 data4.
While caries prevalence is much higher among AI/AN children, there is virtually no information as to why caries continues to be very prevalent and severe in this population1. NHANES data indicate that children living in poverty (i.e., annual incomes less than 100% of the U.S. federal poverty level for families of a particular size – about $24,000 for a family of four) have substantially higher rates of caries than those not living in poverty4. Moreover, many AI/AN reservations are situated in some of the most impoverished areas in the U.S.6, so that factors associated with poverty undoubtedly play a role in the high caries rates among AI/AN children. However, it remains unclear what specific biological, behavioral and environmental factors contribute to caries in impoverished populations, and particularly in AI/AN populations.
Dietary and oral hygiene factors have been most commonly reported as risk factors for caries among impoverished children7–9, while bacterial10,11 and maternal factors11,12 have also been identified in these populations. Among AI/AN children, only one U.S. and one Canadian study have examined risk factors for caries in these populations13, 14. The U.S. study included 77 children 12- to 36-months of age, and found that prolonged bottle use, falling asleep with a bottle, higher frequency of between-meal snacks and delayed initiation of tooth cleaning were associated with having caries13. A study of 315 First Nations children aged 2 to 6 years in the Northwest Territories of Canada found that children who drank sweetened crystal-based beverages were at higher risk for caries14. The same study found that those from higher income families, those who were breast-fed, those who were in communities with water fluoridation, and those who drank fruit juices and milk were at lower risk for caries14.
In summary, there is ample evidence that dental caries prevalence in young AI/AN children is very high relative to other populations, but there has been little research on factors associated with caries in the AI/AN population. Therefore, the purpose of this study was to assess the risk factors for dental caries among a cohort of American Indian children at age 36 months as part of a longitudinal study in this population.
Methods
This paper reports on factors related to caries among a cohort of children at age 36 months as part of a longitudinal study in a Northern Plains tribal community15. Expectant mothers and those who had recently given birth were recruited into the study over a period of one year beginning in June, 2009, with a recruitment goal of 250 mother-child pairs. Recruitment efforts included a media campaign (posters and radio ads), and presentations made at various community sites and health clinics. Expectant women were also made aware of the study by staff at the local Indian Health Service (IHS) hospital, where nearly all tribal women received prenatal care. Baseline data were collected when children were 1 month of age (±30 days), and included a caries exam of the mother, plaque samples from both mother and child, detailed nutritional data for mother and child, as well as information on childcare, child feeding practices and family demographics. Data regarding plaque microflora and transmission are not included in these analyses; these data will be the focus of future papers.
All procedures were reviewed for proper ethical research practices and approved by the Tribal Community’s Human Subjects Review Board, the Aberdeen Area IHS IRB and the University of Iowa Human Subjects Committee.
Much of the same information collected at baseline was also collected at follow-up visits when the children were 4, 8, 12, 16, 22, 28 and 36 months of age (±30 days). Specifically, the follow-up assessments included collection of plaque samples for mother and child, nutritional data for the child, childcare and child feeding practices. Each child also received a dental exam at each follow-up assessment beginning when teeth were first present in the mouth. All data were collected by a study team consisting of a research assistant and one of four dental hygienist/examiners, who were trained by a gold-standard dentist with experience in training examiners for epidemiological examinations. Data were recorded using paper forms, and entered into a web-based database developed for the study.
Nutritional data for mothers and children were collected using a validated beverage frequency questionnaire adapted from the Iowa Fluoride Study16, a 24-hour dietary recall tool, and a food habit questionnaire. These tools were designed to assess overall diet quality and exposure to cariogenic factors including frequency and volume of exposure to fermentable carbohydrate substrates. Nutritional information was gathered for study children at each assessment, while data for mothers was collected only at baseline and at the 36-month assessment.
As described previously15, surface-level dental caries exams were completed using a halogen headlight, a DenLite® illuminated mirror and explorer (Shepherd hook #23 explorer). The teeth were dried with gauze and visually inspected and an explorer was used only to confirm areas of suspected decay and remove debris. In brief, the caries examinations were conducted by one of four trained and calibrated dental hygienist-examiners, and used dmf criteria adapted from those used by NHANES4 and other studies. Training and calibration of examiners was completed by a gold-standard dentist prior to the beginning of the study and subsequently midway through the study period. Reliability of the examiners was high and reported previously15. In addition to the dmf measures, non-cavitated carious lesions were recorded as present or absent at the person level. Children’s caries exams were completed using the knee-to-knee method17, while the permanent dentition exams for the mothers were completed by the same set of examiners and were done under field conditions with the mothers seated in ordinary chairs.
For these analyses baseline demographic and dental data including mother’s age, DMFS, brushing frequency, smoking habits, education level, annual family income, and household size were included and the association of these factors with child caries at 36 months of age was assessed. In addition, child beverage consumption data from the 36-month assessment, which included information on 17 different beverages and beverage consumption categories (e.g., sugar added beverages) were assessed for relationships with caries at 36 months of age.
Data were converted into SAS format for analyses using SAS version 9.3. Bivariate analyses were performed using the chi square and Wilcoxon rank sum tests. Regression modeling was guided by a priori hypotheses that maternal and socio-demographic factors were likely candidate predictors, as well as findings from bivariate analyses. Caries risk models were developed using multivariable logistic regression based on presence or absence of caries at 36 months and were confirmed using both forward and backward selection. The Hosmer-Lemeshow test was used to assess goodness of fit. Counts of decayed, missing or filled surfaces at 36 months were modeled using multivariable negative binomial regression. A 5% significance level was used for all analyses.
Results
A total of 239 children and mother pairs were initially enrolled in the study. By the time of the 36-month examination, 7 were lost to follow-up, leaving 232 subjects in the study. Of these children, 129 were female and 103 were males, with a mean age of 35.4 months. All of the children were American Indian (93%) or American Indian plus another race.
Of the 232 children providing data at the 36-month assessment, 186 (80.2%) had cavitated lesions and an additional 34 subjects (14.7%) had non-cavitated lesions. Prevalence of cavitated lesions in boys was 83.5, while in girls it was 77.5% (p=0.32).
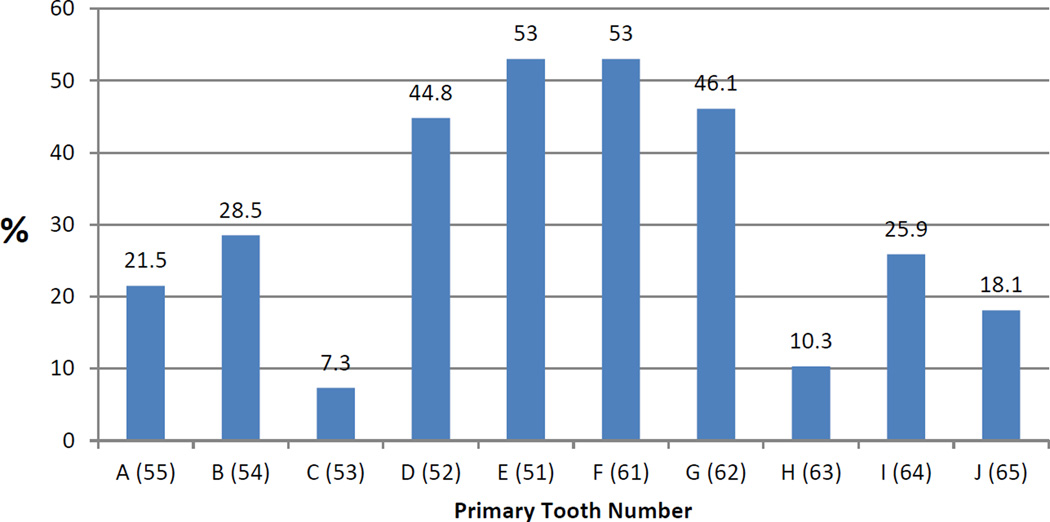
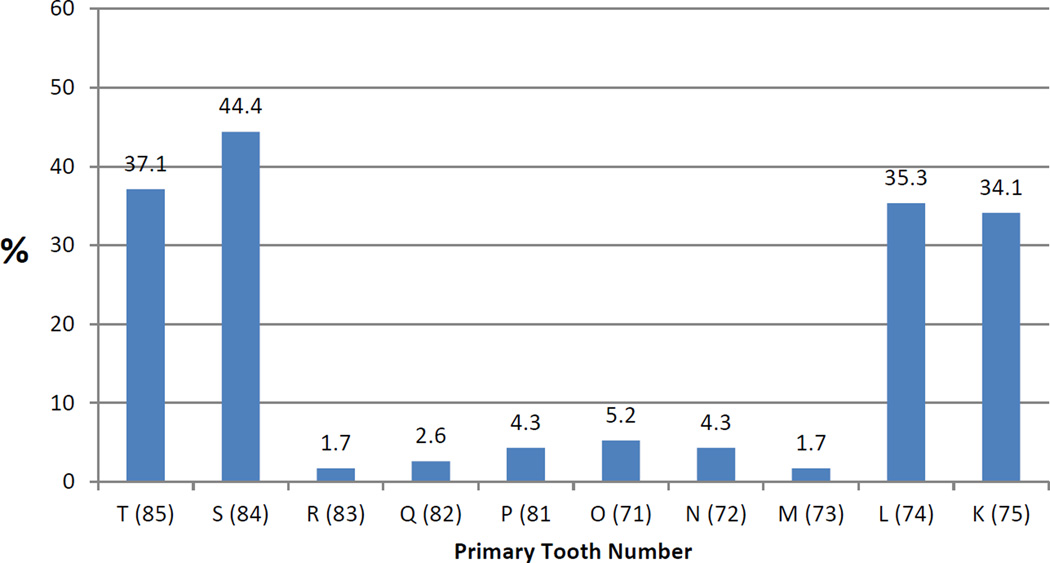
The mean dmfs was 9.6, and was 9.8 in girls and 9.5 in boys (p=0.86). Individual dmfs values ranged from 0 to 42 surfaces. The mean number of erupted surfaces present was 87.7, so that the proportion of all surfaces with dmf was 11.0%. The dmf distribution among affected surfaces was 61.7% decayed, 31.4% missing and 6.9% filled. As seen in Figures 1 & 2, the most commonly affected teeth were the maxillary central incisors with over 50% of these teeth affected.
Figure 1.
Proportion of Maxillary Teeth with dmf Caries
Figure 2.
Proportion of Mandibular Teeth with dmf Caries
Table 1 presents comparison of mean values for selected quantitative demographic and clinical variables by caries status, while Table 2 presents comparisons for categorical variables. Higher maternal caries levels (as measured by DMFS), higher numbers of people per household and lower maternal education level were associated with caries in the primary dentition.
Table 1.
Comparison of mean values for selected quantitative demographic and clinical risk factor variables by caries status in American Indian children.
| Variable | Caries Experience at 36 Months |
N | Mean | Std Dev | P-value |
|---|---|---|---|---|---|
| Child's Age (months) | No | 46 | 35.4 | 0.7 | 0.4852 |
| Yes | 186 | 35.4 | 0.9 | ||
| Total Erupted Teeth | No | 46 | 19. 9 | 0.6 | 0.3999 |
| Yes | 186 | 20.0 | 0.3 | ||
| Maternal Age (years) | No | 46 | 24.2 | 5.7 | 0.4102 |
| Yes | 186 | 23.7 | 5.6 | ||
| Maternal DMFS | No | 46 | 19.4 | 12.7 | 0.0053 |
| Yes | 186 | 29.4 | 22.2 | ||
| Household Size | No | 46 | 6.0 | 1.9 | 0.0046 |
| Yes | 186 | 7.3 | 2.9 |
Table 2.
Bivariate analyses of selected categorical demographic and clinical risk factors by caries status in American Indian children at 36 months of age.
| Variable (n) | Caries Experience at 36 Months |
P-value | |
|---|---|---|---|
| Yes (%) | No (%) | ||
| Mother’s Brushing Frequency | 0.0522 | ||
| More than once/day (143) | 83.9 | 16.1 | |
| Daily (72) | 70.8 | 29.2 | |
| Less than once/day ((17) | 88.3 | 11.7 | |
| Cigarette Smoking | 0.7294 | ||
| No (136) | 79.4 | 20.6 | |
| Yes (96) | 81.3 | 18.7 | |
| Mother’s Education Level | 0.0229 | ||
| Less than High School (104) | 87.5 | 12.5 | |
| High School or GED (48) | 79.2 | 20.8 | |
| Attended College (80) | 71.3 | 28.7 | |
| Annual Family Income | 0.1243 | ||
| $10,000 or less (93) | 83.9 | 16.1 | |
| $10,001 to $40,000 (62) | 77.4 | 22.6 | |
| More than $40,000 (11) | 54.6 | 45.4 | |
| Refused/Don’t know (66) | 81.8 | 18.2 | |
Table 3 presents comparison of mean proportion of total beverage from individual intake sources between those with cavitated caries and those with no cavitated caries. Among the beverages considered, added sugar beverage consumption (which included juice drinks, flavored water, sugared drinks from powder, regular pop, sports drinks, energy drinks, and other sugared drinks) was significantly higher among children with caries than for children with no caries. In addition, those with caries experience had lower mean consumption of sugar-free beverages than those who had no caries experience.
Table 3.
Bivariate analyses of beverage category as a percentage of total beverage intake and caries status in 36-month old American Indian children.
| Category | Caries Experience at 36 Months |
Mean Percentage of Total Beverage Intake |
Std Dev |
Minimum | Maximum | P-value |
|---|---|---|---|---|---|---|
| Milk1 | No | 31.2 | 19.9 | 2.5 | 100.0 | 0.2382 |
| Yes | 27.0 | 15.6 | 0.0 | 78.8 | ||
| 100% Juice | No | 21.9 | 13.5 | 0.0 | 51.6 | 0.1259 |
| Yes | 18.7 | 11.6 | 0.0 | 64.9 | ||
| Added Sugar Beverages 2 | No | 45.5 | 20.6 | 0.0 | 94.1 | 0.0158 |
| Yes | 52.8 | 18.5 | 5.5 | 91.3 | ||
| Water | No | 29.6 | 17.7 | 0.0 | 94.1 | 0.7696 |
| Yes | 30.4 | 16.4 | 0.0 | 83.5 | ||
| Sugar-free Beverages3 | No | 3.6 | 8.9 | 0.0 | 50.0 | 0.0424 |
| Yes | 2.5 | 6.2 | 0.0 | 56.8 | ||
| Non-sugar Beverages4 | No | 33.2 | 19.0 | 0.0 | 94.1 | 0.9102 |
| Yes | 32.9 | 16.8 | 3.5 | 83.5 | ||
| Sugared Beverages5 | No | 35.6 | 17.6 | 0.0 | 74.2 | 0.2291 |
| Yes | 40.1 | 18.6 | 1.8 | 91.3 |
Milk included infant formula, breast milk, cow’s milk, milk-based beverages & soy milk
Added sugar beverages included juice drinks, flavored water, sugared drinks from powder (e.g., Kool Aid), regular soda pop, sports drinks, energy drinks, other sugared drinks (e.g., lemonade or sweet tea)
Sugar-free beverages included sugar-free drinks from powder, diet soda pop, other sugar-free beverages (e.g., plain iced tea)
Non-sugar beverages included “sugar-free beverages” plus water
Sugared beverages included “added sugar beverages” plus 100% juice
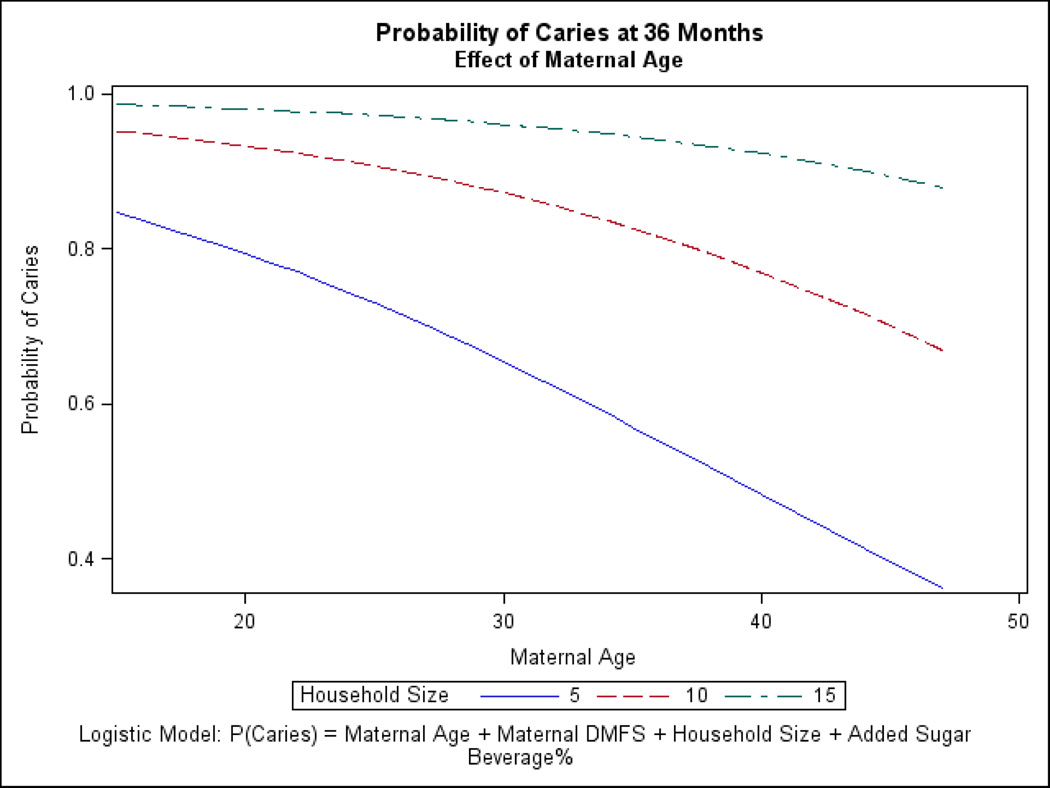
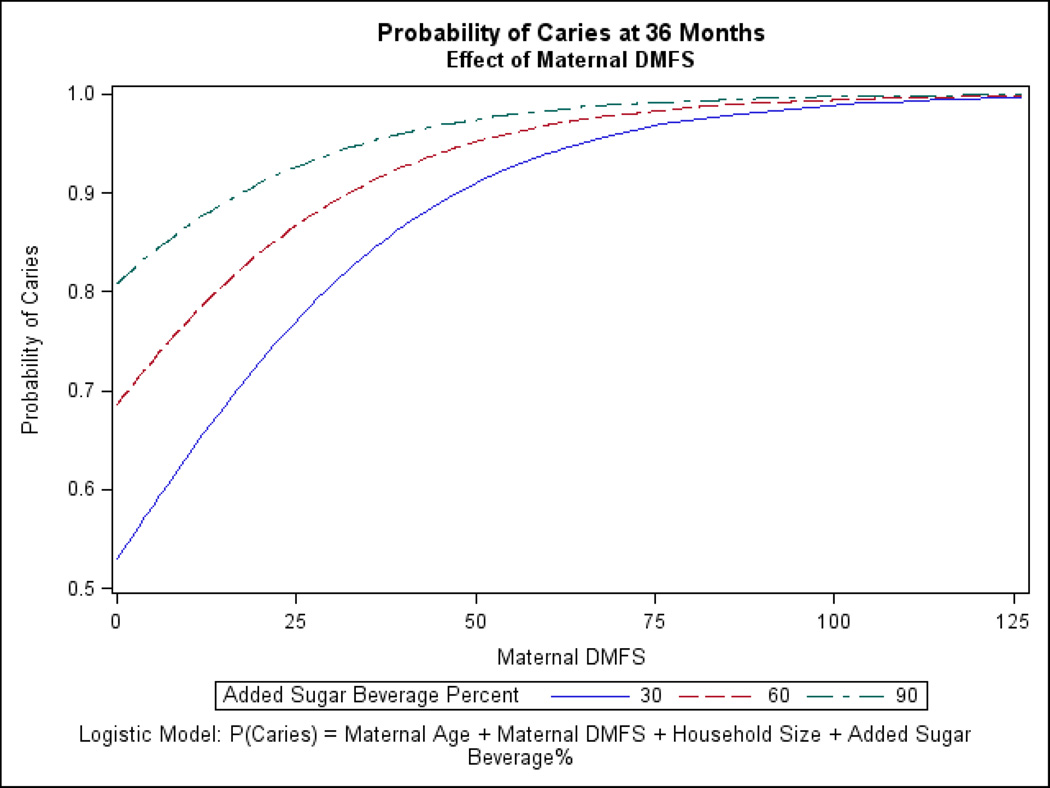
Logistic regression analyses were used to assess variables contributing to caries in children, and as presented in Table 4, cavitated caries was associated with younger maternal age, higher maternal DMFS, higher number of people in the household, and a higher proportion of added sugar beverages consumed. Figures 3 and 4 illustrate the relationships among selected variables in the regression model. Figure 3 demonstrates that younger maternal age and greater household size are associated with higher probability of caries in children, while Figure 4 shows how maternal DMFS and added sugar beverage consumption influence the probability of caries in children.
Table 4.
Results of logistic regression analyses of factors associated with caries experience in 36-month-old American Indian children.
| Variable | Odds Ratio | 95% CI | P-value | |
|---|---|---|---|---|
| Maternal Age | 0.931 | 0.871 | 0.996 | 0.0381 |
| Maternal DMFS | 1.045 | 1.018 | 1.072 | 0.0008 |
| Household Size | 1.291 | 1.091 | 1.526 | 0.0029 |
| Added Sugar Beverage Intake as a Proportion of Total | 1.022 | 1.004 | 1.041 | 0.0175 |
Figure 3.
Effects of Maternal Age and Household Size on Probability of Caries in Children
Figure 4.
Effects of Maternal DMFS and Child Added Sugar Beverage Consumption on Probability of Caries in Children
Table 5 presents the results of negative binomial regression analyses of factors associated with dmf counts at 36 months of age. Of all the factors considered (see Table 5), only maternal DMFS was associated with child dmf levels.
Table 5.
Results of negative binomial regression analyses of factors associated with dmfs in 36-month-old American Indian Children.
| Parameter | Coefficient* | 95% CI* | P-value | ||
|---|---|---|---|---|---|
| Total Erupted Teeth | 1.0895 | 0.6616 | 1.7943 | 0.7362 | |
| Male vs Female | 1.0044 | 0.7335 | 1.3753 | 0.9783 | |
| Household Size | 1.0133 | 0.9585 | 1.0713 | 0.6413 | |
| Mother's Age | 0.9908 | 0.9585 | 1.0244 | 0.5894 | |
| Maternal DMFS | 1.0110 | 1.0027 | 1.0192 | 0.0093† | |
| Smokes Cigarettes vs Does Not Smoke | 1.0122 | 0.7357 | 1.3925 | 0.9409 | |
| Added Sugar Beverage Intake as a Proportion of Total | 1.0042 | 0.9940 | 1.0144 | 0.4211 | |
| Pure Juice Beverage Intake as a Proportion of Total | 0.9969 | 0.9803 | 1.0138 | 0.7179 | |
| Maternal Brushing: At Least Once per Day vs Less Than Once per Day | 0.7989 | 0.4278 | 1.4918 | 0.481 | |
| Annual Family Income | 0.4554 | ||||
| $10,000 or Less | 1.0000 | Reference Category | |||
| $10,000 to $40,000 | 1.0207 | 0.6783 | 1.5360 | 0.9216 | |
| More Than $40,000 | 0.5015 | 0.2217 | 1.1345 | 0.0975 | |
| Refused/Don't Know | 1.0286 | 0.6971 | 1.5177 | 0.8871 | |
| Mother's Education | 0.5967 | ||||
| Less than High School | 1.1818 | 0.8039 | 1.7371 | 0.3956 | |
| High School or GED | 1.2276 | 0.7855 | 1.9186 | 0.3679 | |
| Attended College | 1.0000 | Reference Category | |||
Coefficients are exponentiated allowing for direct interpretation based on children's dmfs
Statistically significant result at the 5% level of significance.
Discussion
This study found that over 80% of children had cavitated (dmf) caries by the time of their 3rd birthday. This finding of high prevalence of caries exist in a population of young U.S. children is alarming; however, it is not very surprising, as the prevalence reported in a recent Indian Health Service survey was 61% among 3-year-olds1. Nonetheless, the prevalence and mean dmfs were very much higher than those in in the U.S. general population as reported by the NHANES data4, and suggest that perhaps some extraordinary factors play important roles in the caries etiology of this population.
The study found that younger maternal age, higher added-sugar beverage consumption, higher maternal caries levels, and a higher number of people in the household were associated with caries in this population. Younger maternal age and higher added-sugar beverages have been identified as risk factors in many populations7, 8, 18–20, and thus are not unique, but seem unlikely to fully explain the high prevalence of caries in this population. Higher maternal caries experience has also been found to be a risk factor in other studies11, 12, 19, 21, and the results of the negative binomial regression analyses found that maternal DMFS was associated with children’s dmf levels. The use of continuous variables in the negative binomial regression analyses of the present study limits the comparability to previous studies12, 21, which used categorical or dichotomous measures of maternal untreated decay; nonetheless, the findings of a significant relationship are consistent between the present study and previous ones.
A large majority (88% - data not shown) of mothers had untreated decay in the present study, so that extensive caries is characteristic in this population. Access to dental care is limited in many AI/AN communities because there are few private providers in the remote areas where they are located and the Indian Health Service, which provides free dental care to tribal community members, is often under-staffed and cannot meet the extensive needs of the community. In addition, tribal community members often have to travel great distances to receive dental care, and many lack reliable transportation. As a result, most of the decay seen in children and adults remains untreated – often for long periods of time. As a result, mothers in this study may have had very high loads of mutans streptococci that were harbored in areas of decay and were readily passed on to their children at a very early age. Given that maternal DMFS was significantly related to child dmf, other maternal factors that likely contribute to high DMFS levels, such as poor diet and lack of oral hygiene, may be reflected in mothers’ child-care practices and thereby increased caries risk for the children.
The other caries risk factor identified in this study was that children with caries had a higher mean number of people residing in their households than did those without caries, which may be related to the patterns of bacterial transmission as mentioned above, but may also be a marker for the high levels of poverty in this population. The tribal community in this study is located in one of the poorest counties in the United States, where over 50% of people live below the federal poverty level and the median annual household income is only $28,512 annually6, compared to the U.S. national poverty rate of 15.3% and the U.S. average median annual household income of $50,0466. However, while the relationship between poverty and higher caries prevalence is well-known, it is not clear what specific conditions associated with poverty contribute to dental caries. The finding that higher numbers of people in the household is a risk factor for caries in this impoverished population suggest that crowded housing may play a role. From a bacterial transmission perspective, crowded housing may allow for more sources of transmission for cariogenic bacteria, and more importantly, increased opportunity for earlier colonization and colonization by more virulent species. In addition, crowded housing may foster an atmosphere for more exposure to cariogenic substrates, specifically a perceived need to pacify young children with sweetened beverages. Also, crowded housing may result in less consistent parenting practices and less consistent oral care for children due to having a variety of caregivers, or overly-fatigued parents. Clearly, these issues warrant further research, including further analyses of the present study’s data.
While this longitudinal study of dental caries among very young children in an AI population was unique, and the loss to follow-up was low, there were limitations. The study sample was drawn from a single tribal community and may not be representative of other American Indian communities, so that generalizing the findings to other American Indian populations must be done with caution. Moreover, due to the widespread prevalence of disease, the number of children without caries was modest, which imposed limitations on logistic modeling. In addition, due to the longitudinal design, the final sample which remained in the study for 3 years may represent a more compliant group than the general population, and may have altered their behavior as part of being in the study (i.e., the Hawthorne effect). Lastly, the scope of the analyses was limited with some potentially important data, such as longitudinal dietary and tooth eruption data, not included.
In conclusion, this study found extremely high levels of dental caries in the sample of American Indian children by the time of their third birthday. Risk factors significantly associated with caries included higher sugar-added beverage consumption, younger maternal age, higher maternal DMFS, and a greater number of people living in the household. Negative binomial regression found maternal DMFS to be associated with child dmf. These factors may reflect the extreme poverty in this population including the high DMFS levels in mothers and suggest that social conditions may have a large impact on caries development in young children.
Acknowledgement
This study was supported by NIH Grant RO1-DE017736. The authors also wish to acknowledge the work of our great study staff and the participation of our study families.
References
- 1.Phipps KR, Ricks TL, Manz MC, Blahut P. Prevalence and severity of dental caries among American Indian and Alaska Native preschool children. J Public Health Dent. 2012;72:208–215. doi: 10.1111/j.1752-7325.2012.00331.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Dental caries in American Indian and Alaska native children. MMWR Morbidity Mortal Weekly Rep. 1985;34:400–401. [PubMed] [Google Scholar]
- 3.Niendorff WJ, Jones CM. Prevalence and severity of dental caries among American Indians and Alaska natives. J Public Health Dent. 2000;60:243–249. doi: 10.1111/j.1752-7325.2000.tb04069.x. [DOI] [PubMed] [Google Scholar]
- 4.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, Beltran-Aguilar ED, Horowitz AM, Li CH. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;248:1–92. [PubMed] [Google Scholar]
- 5.Hicks MJ, Flaitz CM. Epidemiology of dental caries in the pediatric and adolescent population: a review of past and current trends. J Clin Ped Dent. 1993;18:43–49. [PubMed] [Google Scholar]
- 6.U.S. Census Bureau. Small Area Income and Poverty Estimates 2010. http://www.census.gov/did/www/saipe/data/highlights/2010.html.
- 7.Kolker JL, Yuan Y, Burt BA, Sandretto AM, Sohn W, Lang SW, Ismail AI. Dental caries and dietary patterns in low income African American children. Pediatr Dent. 2007;29:457–464. [PubMed] [Google Scholar]
- 8.Warren JJ, Weber-Gasparoni K, Marshall TA, Drake DR, Dehkordi-Vakil F, Dawson DV, Tharp KM. A longitudinal study of dental caries risk among very young low SES children. Community Dent Oral Epidemiol. 2008;37:116–122. doi: 10.1111/j.1600-0528.2008.00447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nair R, Weber-Gasparoni K, Marshall TA, Warren JJ, Levy SM. Factors affecting early childhood caries among WIC-enrolled children in Linn County, Iowa. J Dent Child. 2010;77:158–165. [PubMed] [Google Scholar]
- 10.Ramos-Gomez FJ, Weintraub JA, Gansky SA, Hoover CI, Featherstone JDB. Bacterial, behavioral and environmental factors associated with early childhood caries. J Clin Pediatr Dent. 2002;26:165–173. doi: 10.17796/jcpd.26.2.t6601j3618675326. [DOI] [PubMed] [Google Scholar]
- 11.Smith RE, Badner VM, Morse DE, Freeman K. Maternal risk indicators for childhood caries in an inner city population. Community Dent Oral Epidemiol. 2002;30:176–181. doi: 10.1034/j.1600-0528.2002.300303.x. [DOI] [PubMed] [Google Scholar]
- 12.Weintraub JA, Prakash P, Shain SG, Laccabue M, Gansky SA. Mothers’ caries increases odds of children’s caries. J Dent Res. 2010;89:954–958. doi: 10.1177/0022034510372891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsubouchi J, Tsubouchi M, Maynard RJ, Domoto PK, Weinstein P. A study of dental caries and risk factors among Native American infants. ASDC J Dent Child. 1995;62:283–287. [PubMed] [Google Scholar]
- 14.Leake J, Jozzy S, Uswak G. Severe dental caries, impacts and determinants among children 2–6 years of age in Inuvik Region, Northwest Territories, Canada. J Canad Dent Assoc. 2008;74:519a-f. [PubMed] [Google Scholar]
- 15.Warren JJ, Kramer KWO, Phipps K, Starr D, Dawson DV, Marshall T, Drake D. Dental caries in a cohort of very young American Indian children. J Public Health Dent. 2012;72:265–268. doi: 10.1111/j.1752-7325.2012.00372.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall TA, Eichenberger-Gilmore JM, Broffitt B, Levy SM, Stumbo PJ. Relative validation of a beverage frequency questionnaire in children ages 6 months through 5 years using 3-day food and beverage diaries. J Am Diet Assoc. 2003;103:714–720. doi: 10.1053/jada.2003.50137. [DOI] [PubMed] [Google Scholar]
- 17.Nowak AJ, Warren JJ. Infant oral health and oral habits. Pediatr Clin N America. 2000;47:1043–1066. doi: 10.1016/s0031-3955(05)70257-1. [DOI] [PubMed] [Google Scholar]
- 18.Mattila M-L, Rautava P, Sillanpää M, Paunio P. Caries in five-year-old children and associations with family-related factors. J Dent Res. 2000;79:875–881. doi: 10.1177/00220345000790031501. [DOI] [PubMed] [Google Scholar]
- 19.Thitasomakul S, Piwat S, Thearmontree A, Chankanka O, Pithpornchaiyakul W, Madyusoh S. Risk for early childhood caries analyzed by negative binomial models. J Dent Res. 2009;88:137–141. doi: 10.1177/0022034508328629. [DOI] [PubMed] [Google Scholar]
- 20.Tsai AI, Chen C-Y, Li L-A, Hsaing C-L, Hsu K-H. Risk indicators for early childhood caries in Taiwan. Community Dent Oral Epidemiol. 2006;34:437–445. doi: 10.1111/j.1600-0528.2006.00293.x. [DOI] [PubMed] [Google Scholar]
- 21.Dye BA, Vargas CM, Lee JL, Magder L, Tinanoff N. Assessing the relationship between children’s oral health status and that of their mothers. J American Dent Assoc. 2011;142:173–183. doi: 10.14219/jada.archive.2011.0061. [DOI] [PubMed] [Google Scholar]