Abstract
Introduction
Ankle fractures in the osteoporotic patient are challenging injuries to manage, due to a combination of poor soft tissue, peripheral vascular disease and increased bone fragility, often resulting in more complex fracture patterns. I aim to audit current practice and introduce change by producing recommendations to help improve longer-term functional outcomes.
Patients and methods
A retrospective 3-week audit was conducted reviewing results of ankle fracture management in 50 patients aged between 50 and 80 years. Patients admitted for either manipulation under anaesthesia (MUA)/application of cast or open-reduction and internal fixation (ORIF) were considered. Medical notes, including discharge summaries, were used for data extraction.
Results
From the 50 patients included within the cohort, forty-two patients (84%) underwent surgical intervention, with eight patients (16%) managed non-operatively. Malunion (63%) and failed fracture fixation (25%) were more commonly reported in patients managed non-operatively. Surgery performed by trainee surgeons was unlikely to prolong theatre time with no statistical significance observed with the consultant led cohort (p = 0.380). However, incidence of fracture malunion and failed fixation were significantly higher following surgery without consultant supervision in the junior trainee group (p = 0.043).
Conclusions
Poor bone quality and associated co-morbidity can present technical difficulties when managing patients surgically. However, our results have shown considerably improved anatomical reduction rates following internal fixation in eligible patients, irrespective of age or gender.
Keywords: Ankle, Fracture, Elderly
Highlights
-
•
The audit aimed to clarify whether surgical management of ankle fractures in the elderly was favoured.
-
•
Malunion (63%) and failed fracture fixation (25%) were more commonly reported in patients managed non-operatively.
-
•
Our results have shown considerably improved anatomical reduction rates following internal fixation in eligible patients.
1. Introduction
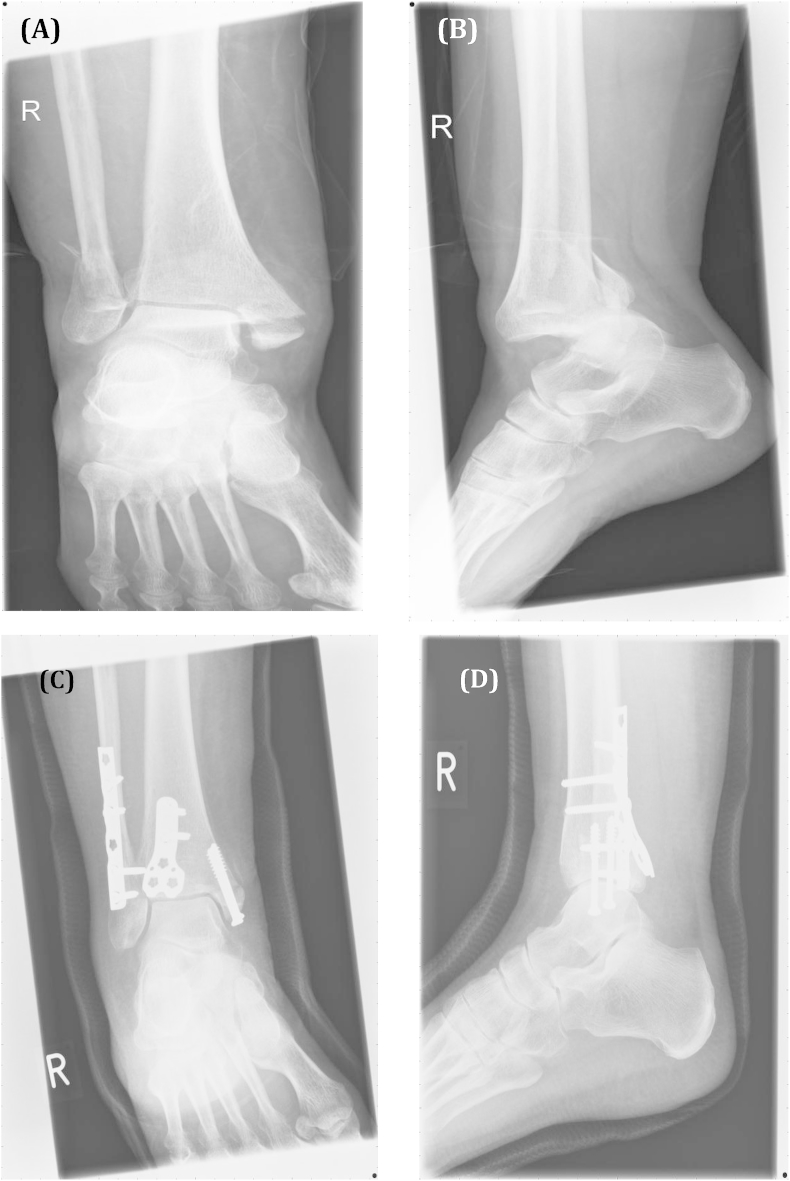
Fragility fractures of the ankle are common, and mainly occur in elderly osteoporotic women. Bi or tri-malleolar fractures together with supra-malleolar fractures of the tibia and fibula are frequently reported [1]. Between 1970 and 2000, a fourfold increase in ankle fragility fractures was observed by Kannus et al. [2], in patients aged over 60 years. Low-energy, trivial trauma often associated with osteoporotic fractures can predispose to more unstable, severe patterns of injury (e.g. Lauge-Hansen supination-eversion stage 4) [1]. Establishing a positive treatment outcome is therefore vital to promote early mobilisation, restore independence, and reduce hospital-associated morbidity (e.g. pressure sores). Despite its high incidence, management remains controversial. Although surgery may be warranted in the majority of younger patients, osteoporotic bone can be associated with poor vascularity, prolonged healing, and failure of fixation [1], [2]. Fixation using hind-foot nailing or locking-plate constructs to preserve vascularity has been documented [3] (see Fig. 1); however, post-operative complications are not unusual. Srinivasan and Moran [4] reported wound edge necrosis and delayed healing in 9% patients aged over 70 years following ORIF ankle. Time to weight bear (TWB) and length of hospital stay (LOS) was also prolonged. This fuels further debate as to whether less invasive methods, including cast application following MUA, should be routinely advocated in the elderly.
Fig. 1.
Pre- (A + B) & post-op (C + D) images of an osteoporotic trimalleolar fracture dislocation of the ankle, treated with a modern locking plate system.
Age is an important predictor of functional outcome; however literature explicitly comparing both operative and non-operative management in elderly patients is sparse. There is potential to advocate change with no uniform guideline in place, and this can help reduce in-patient stay, waiting times, encourage early mobilisation, and reduce patient morbidity. Cumulatively, this creates a more cost-effective system which can attract lucrative tertiary recommendations and encourage patient-flow.
The aim of the audit is to assess current management of ankle fragility fractures locally and advocate change in practice to improve longer-term functional outcomes. Several objectives need to be achieved. Firstly, it is important to isolate trends in surgical and non-surgical patients to ensure radiographic outcomes can be compared, including rates of malunion and non-union with talar displacement. Secondly, all patients meeting inclusion criteria will be reviewed for various outcome measures (e.g. LOS). Finally, any recurring trends facilitating better outcomes will be identified and used to propose future improvements in clinical practice. Recommended standards can then be piloted with data collection forms used for stratification (outside scope of this eSSC).
2. Patients and methods
2.1. Patient characteristics
Over a three-week period (dated 9/07/12′–27/07/12′), the clinical audit was conducted on patients admitted with ankle fragility fractures at the Bristol Royal Infirmary (BRI). The fifty most recent hospital admissions aged between 50 and 80 years with ankle fractures formed the cohort for this retrospective audit. Patients were identified through accident and emergency coding. Inclusion criteria involved all patients admitted for application of cast (POP), external-fixation, MUA or ORIF. Patients managed solely by nursing care, ligamentous injury or with complex distal tibial fractures were excluded. For a process-based audit, a target sample of fifty patients was considered adequate by senior clinicians to make recommendations on management quality. Case-notes, including transfer and discharge summaries, as well as X-rays were used for data collection and to confirm diagnosis. Pre-operative details including patient demographics and falls assessment were noted (see Table 1). The operative details included grade of surgeon, duration, previous manipulation, delay to theatre, and category of surgery (e.g. primary, revision, planned delay etc.). Post-operative/non-operative variables included length of stay (LOS), revision, and follow up care. Time for fracture union and mal-union was assessed independently using patient X-rays. Degree of talar shift and fracture classification (using Weber–Danis Classification) was also documented (see Table 2).
Table 1.
Patient demographics, including bone protection strategy.
| Operative (n = 42) | Non-operative (n = 8) | p-Value | |
|---|---|---|---|
| Mean age (range) | 63 (50–80) | 69 (56–80) | 0.127 |
| Male:female ratio (%male) | 13:28 (46%) | 1:2 (50%) | |
| Falls assessment∗(%) | 12 (29%) | 4 (50%) | |
| DEXA scan∗(%) | 3 (7%) | 1 (13%) |
∗Performed.
Table 2.
Radiological degree of talar displacement and fracture classification.
| Operative (n = 42) | Non-operative (n = 8) | p-Value | |
|---|---|---|---|
| Degree of talar displacement | |||
| 0–5° | 3 | 1 | 0.478 |
| >5° | 2 | 3 | 0.342 |
| Fracture classification | |||
| Uni-malleolar | 6 | 4 | |
| Bi-malleolar | 20 | 3 | |
| Tri-malleolar | 16 | 1 | |
2.2. Treatment
On day of admission, management was largely dictated by the consultant surgeon on-call. By consensus, severity of injury, degree of swelling and associated co-morbidity helped guide treatment. Management was subdivided into non-operative (MUA/POP) or surgical (ORIF/Ex-Fix followed by POP). A policy of operative treatment was generally favoured by clinicians as the primary mode of intervention. ORIF was performed by senior consultants and/or registrars using a variety of implants specifically designed for osteoporotic bone (e.g. locking plate) in accordance with standard AO principals [8]. Below-knee plaster cast was retained for six weeks post-operation. Follow-up with repeat X-rays was conducted at two and six weeks. The cast was changed at two weeks post-op, with wound inspected for infection. Planned surgical delay was often recommended for patients with extensive swelling. Patients requiring operative intervention following MUA were excluded from non-operative management and assessed under the surgical group.
2.3. Further work
With no best practice recommendations for managing ankle fractures in the elderly, it is difficult to set audit standards and determine compliance. Therefore following data collection, evidence-based guidelines may be drawn up (after discussion with the surgical team) to identify acceptable standards and define criteria. Published guidelines can then be implemented locally, with further data collection carried out on all patients prospectively to detect significant changes in functional outcome. Re-audit falls outside the scope of this eSSC period.
The Mann–Whitney U-test was used to analyse recorded data. A p-value <0.05 was considered statistically significant.
3. Results
Fifty patients aged between 50 and 80 years formed the patient cohort, of which 34 females (68%) and 16 males (32%) met the inclusion criteria. The average age was 64 years (50–80 years), with no significant difference in mean age between both groups (p = 0.768). No association between age and type of fracture was noted. However, increasing age was associated with non-operative management, particularly over 60 years (mean average: 69 (SD 8.77). Patients distinct from this trend (22%) were often ineligible for surgery (e.g. severe co-morbidity).
3.1. Bone protection
A formal bone protection strategy was performed on only three patients (6%) in both operative and non-operative groups. This included a comprehensive falls history taken on admission and DEXA scan result. Furthermore, only 3 patients (14%) aged over 65 years had received a DEXA scan, inconsistent with recommendations made by NICE (2011) [10] on osteoporosis screening and management.
3.2. Inpatient stay
Patients managed non-operatively had a mean LOS of 7.44 days (SD 8.78), compared with 9.50 days (SD 8.88) in the surgical group (e.g. ORIF, ex-fix). This was not statistically significant (p = 0.533). Planned surgical delay (≥7 days) was scheduled for ten patients (24% surgical patients), due to medical co-morbidity (e.g. extensive swelling) that needed to be optimised. Four patients required further revision following failed MUA. The remaining 28 patients (67%) were operated on before 7 days. However, this had no significant influence on total inpatient stay (p = 0.740).
3.3. Fracture classification
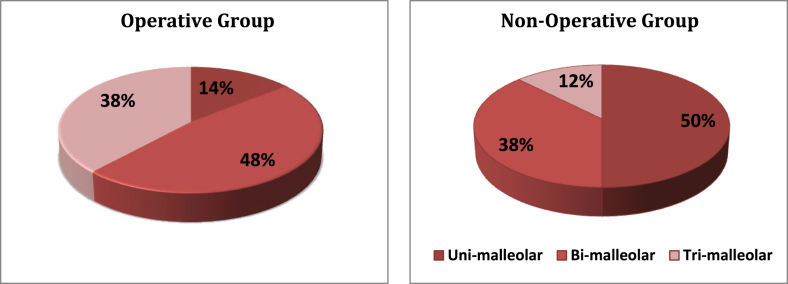
Majority of ankle fractures (98%) were closed, with only one Grade II open fractures (2%). Delayed primary closure was used to treat all open fractures. Thirty-nine fractures (78%) were classed as Weber B (at the level of the syndesmosis), 9 fractures (18%) classed Weber C (above the level of the syndesmosis), and 2 fractures (4%) Weber A. Forty-four of these fractures (92%) were associated with low energy trauma (e.g. simple falls), and 4 fractures (8%) associated with high-energy trauma (e.g. road traffic accidents). Weber B fractures were most commonly associated with ankle dislocation (76%). This contributed to overt antero-posterior joint instability, requiring fixation with locking-plate constructs. Bimalleolar fractures were most likely to undergo surgical management, followed by trimalleolar, and unimalleolar fragility fractures (see Fig. 2).
Fig. 2.
Fracture classification.
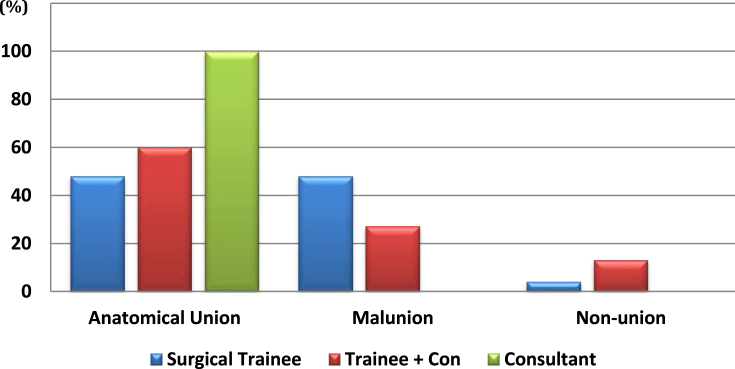
3.4. Grade of surgeon
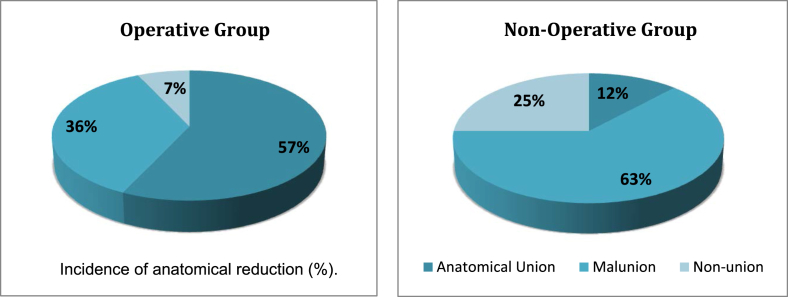
The total time for surgery was shorter when performed by a senior registrar without supervision (mean average: 107.83 min), as opposed to a consultant supervising a registrar (mean average: 126.19 min). Surgery performed by a lone consultant resulted in the shortest time in theatre (mean average: 92.50 min). However, this was not statistically significant (p = 0.380). Incidence of fracture malunion (48%) was significantly higher following surgery without consultant supervision (p = 0.043). Similar failure rates were not reproducible following surgery performed by a consultant lead (see Fig. 3) (see Fig. 4).
Fig. 3.
Influence of grade of surgeon on anatomical reduction (%).
Fig. 4.
Incidence of anatomical reduction (%).
3.5. Radiological results
Following radiological confirmation, average time for fracture union was similar in patients treated by either non-operative (mean average: 9.83 weeks, SD 0.75) or operative (mean average: 9.97 weeks, SD 11.41) approaches (p = 0.976). However, at 6 weeks post-treatment, fracture union was incomplete in all patients managed non-operatively as opposed to 23 post-surgical cases. No significant difference in fracture non-union was noted between age groups, fracture class, or male-to-female ratio. Majority of fractures united radiologically by 12 weeks (93%). Malunion (63%) and failed fracture fixation (25%) was more commonly reported in patients managed non-operatively. No significant difference in degree of talar displacement was recorded following operative and non-operative management (p = 0.342) (see Table 2).
4. Discussion
Achieving anatomical union and reducing inpatient stay are crucial in encouraging early mobilisation and facilitating patient-flow. Poor bone quality, increasing age, and associated co-morbidity have been cited as potential reasons to favour non-operative management, particularly in elderly women [9]. However, authors have only reviewed 86 patients clinically (as opposed to 126 radiologically) with no scoring system in place to verify results. Internal-fixation has been shown to promote fracture union and functional outcome, with a reduced rate of failure [11].
A lower rate of complications was noted in patients following ORIF as opposed to MUA or POP. This has helped answer several key learning objectives stated at the start of the audit. Although no significant difference was identified in time for fracture union, achieving anatomical restoration after non-operative management was difficult. Sixty-three percent patients lost anatomical congruity following non-operative management (e.g. externally rotated fibula) with 8% requiring further surgical intervention. Previous reports [9], [11], [12] have found rates of remanipulation can reach 50% following non-operative treatment. Similar failure rates could not be reproduced following internal-fixation, with only three surgical patients requiring subsequent revision. On the contrary, 36% of patients lost anatomical reduction following surgery, generally inconsistent with reported results [11], [12]. However, several clinical trials have employed strict exclusion criteria, rejecting patients with poor mobility [12]. This limits their overall generalisability to the audit as patients with poor mobility are more likely to sustain fragility fractures.
As highlighted through the audit, low-energy trauma commonly associated with fragility fracture can result in two distinct patterns of injury. The majority of patients (78%) sustained fractures at the level of the syndesmosis, with 18% just above. Prospective cohorts [1] have reported similar outcomes, resulting in displaced and inherently unstable fractures, with associated subluxation of the subtalar joint. Seventy-six percent of Weber B fractures were associated with subluxation/dislocation, with internal-fixation the preferred mode of treatment. Manipulation and POP for similar patterns of injury have been shown to promote malunion or non-union, with a significant number requiring surgical revision [11], [12]. Although only 8% of the patient cohort required internal-fixation following failed MUA, failed fracture fixation was reported in 25% patients managed solely with MUA or POP. Unimalleolar fractures with minimal ligamentous injury are less prone to rotational misalignment, advocating the use of non-operative treatment (50%). Previous reports have shown how stable fractures managed solely with a functional brace can promote cost-benefit and functional outcome [13]. However, the report employed a smaller sample size (n = 45) and younger cohort (mean average: 45.7 years). Therefore assumptions on statistical significance and generalisability need to be approached with caution.
No significant difference in mean LOS (p = 0.533) was noted between either treatment arm. Furthermore, total inpatient stay was not significantly influenced by delayed surgery, aimed at optimising patient co-morbidity (e.g. reduce extensive swelling). This correlates poorly with previous reports showing a mean average increase of 4.1 days in surgical patients delayed due to overrun theatre list or patient co-morbidity [14]. Intensive physiotherapy and early-facilitated discharge in surgical patients may validate this trend, with significant cost-saving implications [15]. As was expected, surgery performed by a lone consultant resulted in the shortest time to theatre (mean average-92.50 min). Although no significant difference was noted when compared with registrar-led surgery, rates of fracture malunion and failed fixation were significantly higher in the latter group. This was more commonly reported following trimalleolar and bimalleolar repair without consultant supervision (80% of fracture malunion). This was largely expected given the lower levels of surgical experience and level of training held by registrars.
Following data collection, a number of key recommendations can be made towards prospective re-audit and current practice. Firstly, primary prevention should involve screening all patients over the age of 65 for reduced bone mineral density, using DEXA scanning. Hence, at risk patients can be identified early and treated with combination bone protection therapy if required. Such recommendations are consistent with national guidelines produced by NICE (2011) [10]. Secondly, failed anatomical reduction following internal fixation of complex ankle fractures (e.g. bi- or trimalleolar) was more likely when performed by registrars without supervision. Therefore, all surgical fixation performed on either bi- or trimalleolar fractures should be supervised or performed by a lead consultant. Finally, as incidence of fracture malunion and failed fixation was approximately half the failure rate associated with non-operative management, internal-fixation or hind-foot nail should be the preferred mode of treatment. This is provided patients are medically fit and eligible for surgery. Following implementation of these recommendations, a prospective re-audit can be devised to assess for marked changes in radiological non-union.
Limitations of the present study should be recognised. Given the small sample size, reasonable assumptions cannot be made about the statistical significance of the data set. The audit is insufficiently powered to detect rare treatment outcomes (e.g. malunion and failed fixation), particularly as only nine patients were managed non-operatively across the cohort. Therefore, to avoid type-II statistical error a reasonable sample size of at least 216 patients in each treatment arm, at 80%-power is required. This is provided the mean levels of failed reduction are 63.0% and 36.0% in non-operative and operatively managed groups respectively (mean averages taken from current study). Given this is a retrospective audit, the included cohort are prone to selection bias. Allocation of patients to either treatment arm was based on clinical condition, in the absence of a randomised system. This tailored selection criteria may not be reproducible universally. However, following implementation of clinical recommendations, data-collection following re-audit will be in prospective format. Selection and measurement bias can therefore be controlled. Finally, no prolonged follow-up protocol or information on pre-injury mobility was used. This would help quantify limitations in physical activity for patients following treatment.
5. Conclusions
Inherently unstable fractures coupled with poor bone quality and healing capacity in geriatric patients has fuelled further debate on the optimal management strategy. Significant ambiguity persists; however our results have shown considerably better treatment outcomes following operative management (including superior anatomical reduction rates) when compared to non-operative treatment.
Ethical approval
Nothing to declare.
Funding
Nothing to declare.
Consent
Nothing to declare.
Author contribution
Dr. Langhit Kurar (Audit lead).
Mr. Steven Mitchell (assisted with data collection).
Mr. Steven Metcalfe (assisted with data analysis).
Conflict of interest
Nothing to declare.
Registration of Research Studies
Assigned Unique Identifying Number (UIN) from the Research Registry: researchregistry548.
Guarantor
Dr. Langhit Kurar.
Acknowledgements
I would like to thank Mr. Steve Mitchell for supervising the audit and providing radiographs as well as Mr. Stuart Metcalfe for assisting in data collection.
Footnotes
This project is all my own work unless otherwise stated. All text, figures, tables, data or results which are not my own work are indicated and the sources acknowledged.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.amsu.2015.12.061.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Lemon H., Somayaji H.S., Khaleel A., Elliot D.S. Fragility fractures of the ankle: stabilisation with an expandable calcaneotalotibial nail. J. Bone Jt. Surg. 2005;87-B:809–813. doi: 10.1302/0301-620X.87B6.16146. [DOI] [PubMed] [Google Scholar]
- 2.Kannus P., Palvanen M., Niemi S., Parkkari J., Jarvinen M. Increasing number and incidence of low-trauma ankle fractures in elderly people: finnish statistics during 1970–2000 and projections for the future. Bone. 2002;31:430–433. doi: 10.1016/s8756-3282(02)00832-3. [DOI] [PubMed] [Google Scholar]
- 3.Wagner M. General principles for the clinical use of the LCP. Injury. 2003;34(Suppl. 2):B31–B42. doi: 10.1016/j.injury.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan C.M., Moran C.G. Internal fixation of ankle fractures in the very elderly. Injury. 2001;32:559–563. doi: 10.1016/s0020-1383(01)00034-1. [DOI] [PubMed] [Google Scholar]
- 8.Müller M.E., Allgöwer M., Schneider R., Willenegger H. second ed. Springer-Verlag; Berlin: 1979. Manual of Internal Fixation: Techniques Recommended by the AO Group. [Google Scholar]
- 9.Beauchamp C.G., Clay N.R., Thaxton P.W. Displaced ankle fractures in patients over 50 years of age. J. Bone Jt. Surg. 1983;65B:329–334. doi: 10.1302/0301-620X.65B3.6404905. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Clinical Excellence . NICE; London: 2011. Guidelines on the Primary Prevention of Osteoporotic Fragility Fractures in Postmenopausal Women. (amended) [Google Scholar]
- 11.Anand N., Klenerman L. Ankle fractures in the elderly: MUA versus ORIF. Injury. 1993;24:116–120. doi: 10.1016/0020-1383(93)90202-h. [DOI] [PubMed] [Google Scholar]
- 12.Ali M.S., McLaren C.A.N., Rouholamin E., O'Connor B.T. Ankle fractures in the elderly: nonoperative or operative treatment. J. Orthop. Trauma. 1987;1:275–280. doi: 10.1097/00005131-198701040-00002. [DOI] [PubMed] [Google Scholar]
- 13.Jain N., Symes T., Doorgakant A., Dawson M. Clinical audit of the management of stable ankle fractures. Ann. R. Coll. Surg. Engl. 2008;90(6):483–487. doi: 10.1308/003588408X301145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pietzik P., Qureshi I., Langdon J., Molloy S., Solan M. Cost benefit with early operative fixation of unstable ankle fractures. Ann. R. Coll. Surg. Engl. 2006;88:405–407. doi: 10.1308/003588406X106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James L.A., Sookhan N., Subar D. Timing of operative intervention in the management of acutely fractured ankles and the cost implications. Injury. 2001;32:469–472. doi: 10.1016/s0020-1383(00)00254-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.