Abstract
Objectives:
To assess in vitro the quantitative and qualitative debonding behavior of the AEZ debonding plier, compared to shear debonding force, in debonding orthodontic metal brackets.
Materials and Methods:
Thirty-two extracted premolars bonded with metal brackets were randomly divided into two equal groups according to the type of simulated debonding method; compressive bond strength (CBS) group using AEZ debonding plier (Ormco Corporation, USA) attached to the Instron machine, and shear bond strength (SBS) group using regular Instron attachments. All teeth were subjected to debonding forces, and debonding strength was assessed. The buccal surfaces were then examined, under a stereomicroscope, and adhesive remnants were scored using adhesive remnant index (ARI). Debonding strengths comparison was performed using the independent sample t-test. ARI score comparison was performed using the Mann–Whitney U-test. Correlation between debonding strength and ARI scores was performed using the Spearman correlation.
Results:
There was no significant difference in mean debonding strength between the SBS (M = 6.17 ± 0.77 MPa) and CBS (M = 6.68 ± 1.67 MPa) groups (P > 0.05). The CBS group showed significantly less adhesive remnants than the SBS group (P < 0.05); 62.5% of CBS group had ARI score 1, whereas 68.8% of SBS group had ARI score 3. No significant correlation between ARI and debonding strength was found (P < 0.05).
Conclusion:
SBS was found to produce similar debonding strength to the AEZ debonding plier in vitro. However, the AEZ debonding plier resulted in less adhesive remnant which is of great advantage for reducing chair-time during cleanup after debonding brackets.
Keywords: Adhesive remnants, compressive strength, debonding plier, orthodontic brackets, shear strength
INTRODUCTION
Debonding orthodontic fixed appliances is a critical stage during and at the end of comprehensive fixed orthodontic treatment. Multiple instruments or pliers have been used and assessed for debonding orthodontic brackets. Some clinicians used specialized debonding pliers; straight or angulated.[1,2,3,4,5,6,7,8,9,10,11] Others used instruments that are not manufactured specifically for debonding such as Weingart pliers, Howe pliers, and straight wire cutters.[12,13] Multiple in vitro and some in vivo studies have assessed and compared the effect of such instruments on the debonding strength, enamel surfaces, adhesive remnants, as well as on bracket breakage,[4,7,10,12,13,14,15] with varied results.
The most common type of forces applied at debonding are shear, tension, compression, and torsion (torque). However, many factors have been reported to affect the final debonding strength value. The force application type,[2,3,4,12,16,17,18,19] magnitude,[20] location,[6,16,17,19,21,22,23] direction,[1,7,19] and angulation[23] are some of the major factors affecting the final bond strength value. The in vivo versus in vitro environments have also shown to give different results. The reported bond strength measured in vivo was found to be significantly lower than that measured in vitro.[2,14,24] Multiple finite element analysis highlighted the factor of the nonhomogenous distribution of stresses on the enamel, bracket, adhesive, alveolar bone, as well as on the periodontium with the different debonding forces applied at debonding.[2,3,16,18,21] This could be another added attribute to the great variability of results on debonding strengths reported in the literature.
The debonding pliers, which are specifically designed for debonding orthodontic brackets, are designed to produce shear/peel, compressive, or tensile forces depending on the type of pliers used, direction (occluso-gingival or mesiodistal), and location of force application (at bracket wings or bracket base).[1,4,5,10,12,13,14,17] Su et al., compared in vitro four different methods of debonding using clinically simulated models. They found that applying a debonding force on the brackets in an occluso-gingival direction at the bracket base produced significantly lower bond strength and less adhesive remnants than applying the same force in the same direction but at the bracket wings.[4] Thus, they concluded that force at bracket base in an occluso-gingival direction is the least damaging to enamel when using compressive force.[4] However, they used different pliers for the two latter methods, which makes it difficult to conclude with regards to the best plier or debonding method to be used. Furthermore, Brosh et al. reported the opposite results in debonding strength when assessed the two compressive methods in vivo, with no significant difference in the amount of adhesive remnants.[6]
Prietsch et al., compared three debonding methods; tensile force applied by the Instron machine, shear force applied at bracket base by the Instron machine, and compression force applied in an occluso-gingival direction at the bracket base by a specially designed device. They found that the mean bond strength for shear (7.71 MPa) was statistically higher than for compression (2.98 MPa) and tension (2.69 MPa) with no significant difference between the latter two methods.[17] However, they did not assess the adhesive remnants or enamel fracture. They also did not use a standardized measuring machine for all methods assessed.
Pithon et al., in their in vivo study, used a lift-off debonding instrument, straight cutter plier, how plier, and the conventional bracket removal plier. The latter instrument was used to apply a squeezing force at the bracket base in a mesiodistal direction. They found that the conventional bracket removal plier as used in their study seemed to result in a lot of adhesive remnants after debonding.[12] The objective of the current study was to assess and compare in vitro; the quantitative and qualitative differences in debonding behavior between compressive strengths produced by an AEZ debonding plier at bracket base in an occluso-gingival direction and shear bond strengths (SBSs) at bracket base produced by the Instron machine in debonding orthodontic metal brackets.
MATERIALS AND METHODS
In this in vitro study, two different debonding methods were assessed and compared quantitatively and qualitatively. The first method was the regular laboratory method that produced SBSs by a load applied at bracket base by the blades of an Instron Universal Testing Machine (ElectroPlus E1000, Instron, Canton, MA, USA) and directed from gingival to occlusal [Figure 1]. The second method simulated the clinical situation where a compressive load at bracket base in an occluso-gingival direction was applied by an AEZ narrow blade debonding plier mounted on an Instron machine, as proposed by Bishara et al.[8,9] and Horiuchi et al. [Figure 2].[25]
Figure 1.
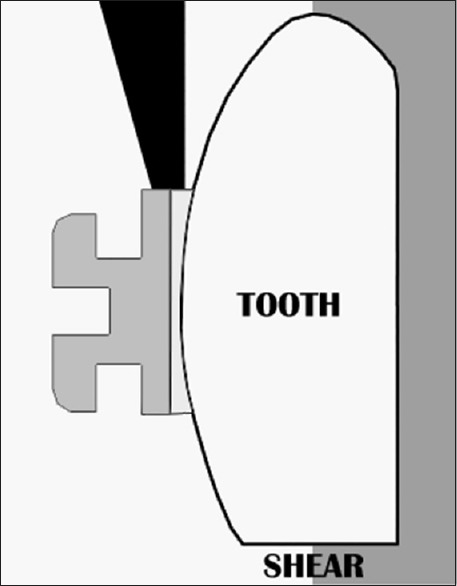
Diagram showing the shear debonding force applied by the Instron blades from gingival to occlusal direction at debonding
Figure 2.
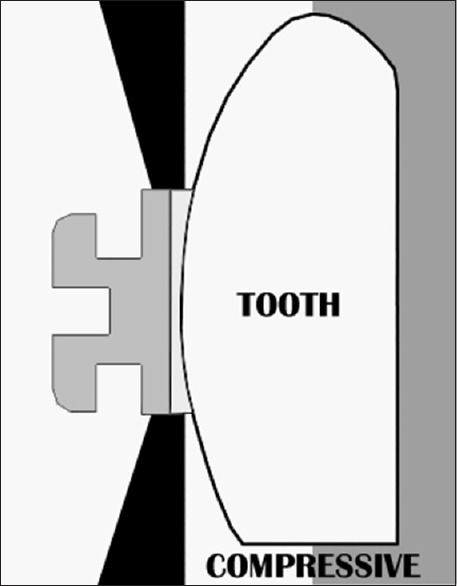
Diagram showing the compressive debonding force applied by the AEZ narrow blade debonding plier in an occluso-gingival direction at debonding
Sample Preparation
Based on 80% power of the test, 32 sound extracted premolars, with no obvious enamel cracks, were collected and stored in distilled water. Teeth were then cleaned, polished with nonfluoridated pumice and rubber prophylactic cups for 15 s, rinsed with water spray for 10 s, and dried with oil-free compressed air for 10 s. The buccal surfaces were etched with 37% phosphoric acid solution for 30 s according to the manufacturer's instructions, rinsed with water spray for 20 s, and then dried with oil-free compressed air for 20 s. All teeth were bonded with metal brackets (Gemini series, 3M Unitek, USA) using Transbond XT light-cured composite resin (3M, St. Paul, MN, USA), and applied according to manufacturer instructions. Excess composite was removed from around the bracket margins with the tip of a probe and then photo-polymerized from five directions: Above the bracket, cervical, occlusal, mesial, and distal for 20 s each (Ortholux, 3M Unitek, Monrovia, CA, USA) (light output, 430–480 nm). Teeth were then stored in distilled water at 37°C in an incubator for 1 week to ensure complete polymerization of the adhesive resin. Each tooth was then embedded in an acrylic block so that only the buccal surfaces are exposed for testing. The sides of the blocks were trimmed straight to act as a flat surface at which the blocks were screwed on the attachments of the Instron testing machine. This method was designed to help properly align the blades of the testing device parallel to the enamel surface and secure it in place for standardization. All teeth were then randomly divided into two groups (n = 16 each); compressive bond strength (CBS) and SBS groups.
Bond Strength Assessment (Quantitative)
All teeth were debonded using an Instron Universal Testing Machine with a crosshead speed of 0.5 mm/min and a 50-kg load cell. However, each group received a different method of force loading. The SBS group was subjected to a shear force produces by the blades of the Instron machine. The force was applied by the blades on the bracket base and directed from gingival to occlusal until bond failure occurred. The CBS group was debonded with a custom-made attachment that was composed of a regular narrow blade orthodontic debonding plier (AEZ Debonding Orthodontic Plier, Ormco Corporation, USA) mounted on the Instron machine. Forces exerted by the stainless steel blades of the pliers were applied at the bracket base with a squeezing action in an occluso-gingival direction until bond failure occurred.
The force at failure, in Newtons (N), was recorded in both groups. The debonding strength, in megapascal (MPa), was then calculated as follows:
For the SBS group, the SBS was calculated using the formula F/A, where A is the surface area of the bracket base
For the CBS group, the debonding force by the Instron was applied at a predetermined constant distance on the arms of the plier. Thus, the actual compressive debonding strength was calculated using the formula;
(the actual debonding strength = recorded force [by the Instron machine] × [b/a]).
Where a is the distance between the blades of the plier at the bracket base and the fulcrum of the plier, while b is the distance from the fulcrum of the plier to where the force is applied on the plier's arms by the Instron machine [Figure 3]. The conversion factor (b/a) used in this study was calculated to be 0.55.
Figure 3.
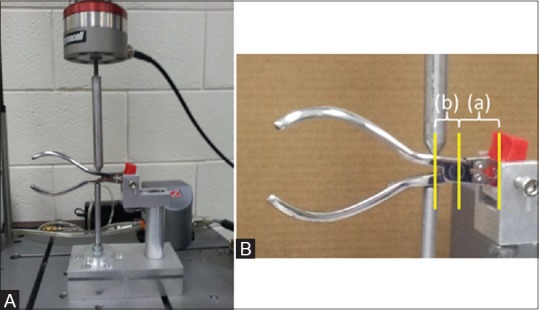
Diagram showing (A) the design of the AEZ debonding plier mounted on the Instron machine, and (B) how the distances (a) and (b) used to calculate the actual debonding force are measured
Adhesive Remnant Assessment (Qualitative)
All teeth were examined under a stereomicroscope at ×10, and ×20 magnifications for the residual adhesives remaining on the buccal enamel surfaces. The amount of adhesive remnant was then scored using the modified adhesive remnant index (ARI)[25] as follows:
Score 0: No retained resin (0%)
Score 1: ≤50% retained resin on the enamel surface (>0–≤50%)
Score 2: >50% retained resin on the enamel surface (>50–<100%)
Score 3: All resin retained on the enamel surface with bracket imprint (100%).
Statistical Analysis
Data were analyzed using descriptive statistics to report the means and standard deviations for the debonding strengths (MPa) of the two groups assessed, as well as the number and percentages of teeth for each ARI score. Inferential statistics for mean comparison in debonding strength values was conducted using independent sample t-test. Mann–Whitney U-test was conducted for ARI score comparison between the groups. Spearman correlation test was used to examine the correlation between the debonding strength and the ARI scores. All data were analyzed using SPSS statistical analysis software program (version 16.0, SPSS Inc., Chicago, USA). Significance level was set at (P < 0.05).
RESULTS
Debonding Strength
No significant difference in the mean debonding strength was reported between the SBS and CBS groups (P > 0.05). The mean debonding strength for the SBS group was 6.17 ± 0.77 MPa, and for the CBS was 6.68 ± 1.67 MPa [Figure 4].
Figure 4.
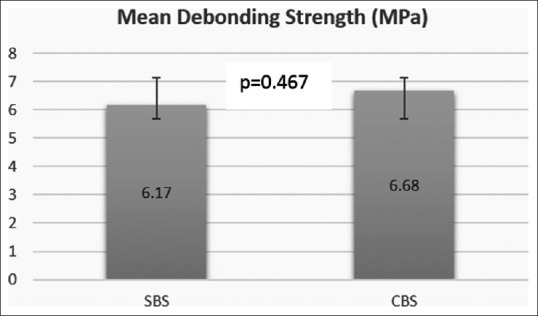
Mean and standard deviation of the debonding strength values (MPa) for the two groups assessed. Using independent sample t-test; no significant difference was found at P < 0.05
Adhesive Remnants
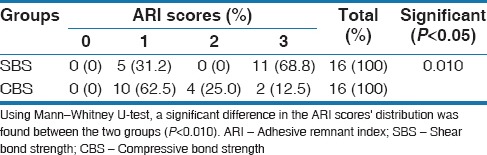
Mann–Whitney U-test revealed a significant difference in the adhesive remnant scores after debonding between the two groups assessed (P < 0.05). More than 60% of the sample in the SBS group had ARI score 3 (all resin retained on the enamel surface with bracket imprint [100%]). On the other hand, 60% of the CBS group had ARI score of 1 (≤50% retained resin on the enamel surface). Concomitantly, none of the samples had ARI score (0) where no adhesive remained after debonding [Table 1].
Table 1.
Number and percentages of teeth under each adhesive remnant index score for the two groups assessed
Correlations
No significant correlation was found between the debonding strength and the ARI scores in both the SBS (r = −0.282) and CBS (r = 0.577) groups (P > 0.05).
DISCUSSION
The force direction and location applied in the current study using an AEZ narrow blade debonding plier was similar to the method developed by Bishara and Fehr,[8] in which force was applied at the bracket base on both sides of the bracket simultaneously (bilateral load) in an occluso-gingival direction. Bishara and Fehr described such type of force as being similar to the force applied during a diametral compression test for tension. They also proposed that such method is an indirect way of measuring the tensile strength of materials that exhibited very limited plastic deformation such as ceramics, composites, and enamel.[8] Such method was further assessed by Bishara et al. in 1994 for debonding ceramic brackets.[9] They found that debonding with pliers required the application of 30% less force to the enamel surface than debonding with shear forces as tested in the laboratory, with no significant differences in the ARI.[9] Thus, they hypothesized that applying the load to the two sides of the bracket increased the chances of starting a crack and propagating it in the brittle adhesive causing debonding to occur at a lower debonding force.[9] Horiuch et al. also adopted such method as a clinically representative laboratory method.[26] However, they used it to assess the bond strength between different types of adhesives but did not use it for assessing debonding strengths.
Contrary to the findings of Prietsch et al.[17] and Bishara et al.,[9] the current study reported no significant differences in the debonding strength between shear and compressive forces when applied at the bracket base. However, a significant reduction in the amount of adhesive remnants was found in the current study with the compressive group. The latter indicates that the site of bond failure was more toward the enamel-adhesive interface than the bracket-adhesive interface. It also shows that the debonding behavior of metal brackets using the current settings differs than that of ceramic brackets as reported by Bishara et al.[9]
Similar to the findings of Brosh et al.,[6] no significant correlation was found between the debonding strength and the ARI scores in both groups. Thus, the debonding force cannot be used as a predictor to the bond failure site or enamel fracture.
Holberg et al. in his finite element analysis studies assessed four directions and locations of forces applied by pliers.[2,3] He found that the least amount of stress on enamel occurred when applying lateral rotation force, which is a compressive force in an occluso-gingival direction but at bracket wings.[2] However, he also found this method resulted in a significantly high stress on the periodontium.[3] In contrast, he found that applying compressive loads in a mesiodistal direction at bracket wings produced a moderate maximum stress values on the enamel and alveolar bone,[2] but with a negligible effect on the periodontium.[3] The latter method of force application was also found to result in a bond failure that is at or just close to the enamel-adhesive interface in vitro[1] which could explain the results of the finite element analysis. Thus, Holberg et al. recommended that lateral rotation force is the best method to be used for debonding orthodontic brackets in a healthy periodontium, while compressive force is the best to be used in a compromised periodontium.[3] However, Holberg did not assess the compressive force in an occluso-gingival direction at bracket base, which makes it difficult to compare with the findings of the current study.
Findings of this study highlight two issues; the first is that any findings in vitro on SBS using the Instron blades in an occlusal to the gingival direction at bracket base with similar laboratory conditions as our study can be generalized to represent the clinical situation of using AEZ debonding plier in an occluso-gingival direction at bracket base. The second issue is that using the AEZ debonding plier resulted in minimal adhesive remnant and thus less chair-time for cleanup after debonding, thus giving it an extra advantage over using SBS.
Further studies are needed to assess the debonding behavior of the AEZ debonding pliers using different forces, methods of applications, as well as comparing in vivo, in vitro, and finite element analysis. Furthermore, with the current advances in technology and science, a standardized protocol needs to be developed for assessing the debonding problems in orthodontics to solve the big variability in debonding results in the literature, hence, aid in reaching comparable findings for conclusive meanings. As observed, but not investigated in this study, the AEZ pliers have thick beaks that might not always guaranteed that the pliers are applied at the enamel-adhesive interface. Thus, debonding pliers with thin beaks are recommended.
CONCLUSION
Within the limitations of this study, in vitro testing of SBS by the Instron blades in an occlusal to gingival direction was found to produce similar debonding strength as applying the AEZ debonding plier in a similar direction at bracket base. However, the AEZ debonding plier resulted in less adhesive remnant which is of great advantage for reducing chair-time during cleanup after debonding brackets.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Choudhary G, Gill V, Reddy YN, Sanadhya S, Aapaliya P, Sharma N. Comparison of the debonding characteristics of conventional and new debonding instrument used for ceramic, composite and metallic brackets - An in vitro study. J Clin Diagn Res. 2014;8:ZC53–5. doi: 10.7860/JCDR/2014/9370.4617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holberg C, Winterhalder P, Holberg N, Wichelhaus A, Rudzki-Janson I. Orthodontic bracket debonding: Risk of enamel fracture. Clin Oral Investig. 2014;18:327–34. doi: 10.1007/s00784-013-0969-4. [DOI] [PubMed] [Google Scholar]
- 3.Holberg C, Rudzki-Janson I, Wichelhaus A, Winterhalder P. Periodontal ligament strain induced by different orthodontic bracket removal techniques: Nonlinear finite-element comparison study. J Orofac Orthop. 2014;75:287–98. doi: 10.1007/s00056-014-0219-7. [DOI] [PubMed] [Google Scholar]
- 4.Su MZ, Lai EH, Chang JZ, Chen HJ, Chang FH, Chiang YC, et al. Effect of simulated debracketing on enamel damage. J Formos Med Assoc. 2012;111:560–6. doi: 10.1016/j.jfma.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Pont HB, Özcan M, Bagis B, Ren Y. Loss of surface enamel after bracket debonding: An in-vivo and ex-vivo evaluation. Am J Orthod Dentofacial Orthop. 2010;138:387.e1–9. doi: 10.1016/j.ajodo.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 6.Brosh T, Kaufman A, Balabanovsky A, Vardimon AD. In vivo debonding strength and enamel damage in two orthodontic debonding methods. J Biomech. 2005;38:1107–13. doi: 10.1016/j.jbiomech.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 7.Pickett KL, Sadowsky PL, Jacobson A, Lacefield W. Orthodontic in vivo bond strength: Comparison with in vitro results. Angle Orthod. 2001;71:141–8. doi: 10.1043/0003-3219(2001)071<0141:OIVBSC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Bishara SE, Fehr DE. Comparisons of the effectiveness of pliers with narrow and wide blades in debonding ceramic brackets. Am J Orthod Dentofacial Orthop. 1993;103:253–7. doi: 10.1016/0889-5406(93)70006-A. [DOI] [PubMed] [Google Scholar]
- 9.Bishara SE, Forrseca JM, Fehr DE, Boyer DB. Debonding forces applied to ceramic brackets simulating clinical conditions. Angle Orthod. 1994;64:277–82. doi: 10.1043/0003-3219(1994)064<0277:DFATCB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Bishara SE, Ostby AW, Laffoon J, Warren JJ. Enamel cracks and ceramic bracket failure during debonding in vitro . Angle Orthod. 2008;78:1078–83. doi: 10.2319/112007-540.1. [DOI] [PubMed] [Google Scholar]
- 11.Lin CL, Huang SF, Tsai HC, Chang WJ. Finite element sub-modeling analyses of damage to enamel at the incisor enamel/adhesive interface upon de-bonding for different orthodontic bracket bases. J Biomech. 2011;44:134–42. doi: 10.1016/j.jbiomech.2010.08.038. [DOI] [PubMed] [Google Scholar]
- 12.Pithon MM, Santos Fonseca Figueiredo D, Oliveira DD, Coqueiro Rda S. What is the best method for debonding metallic brackets from the patient's perspective? Prog Orthod. 2015;16:17. doi: 10.1186/s40510-015-0088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumbryte I, Linkeviciene L, Malinauskas M, Linkevicius T, Peciuliene V, Tikuisis K. Evaluation of enamel micro-cracks characteristics after removal of metal brackets in adult patients. Eur J Orthod. 2013;35:317–22. doi: 10.1093/ejo/cjr137. [DOI] [PubMed] [Google Scholar]
- 14.Hajrassie MK, Khier SE. In-vivo and in-vitro comparison of bond strengths of orthodontic brackets bonded to enamel and debonded at various times. Am J Orthod Dentofacial Orthop. 2007;131:384–90. doi: 10.1016/j.ajodo.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 15.Parrish BC, Katona TR, Isikbay SC, Stewart KT, Kula KS. The effects of application time of a self-etching primer and debonding methods on bracket bond strength. Angle Orthod. 2012;82:131–6. doi: 10.2319/020411-82.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katona TR. A comparison of the stresses developed in tension, shear peel, and torsion strength testing of direct bonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 1997;112:244–51. doi: 10.1016/S0889-5406(97)70251-8. [DOI] [PubMed] [Google Scholar]
- 17.Prietsch JR, Spohr AM, Lima da Silva IN, Pinheiro Beck JC, Silva Oshima HM. Development of a device to measure bracket debonding force in vivo . Eur J Orthod. 2007;29:564–70. doi: 10.1093/ejo/cjm069. [DOI] [PubMed] [Google Scholar]
- 18.Chen CS, Hsu ML, Chang KD, Kuang SH, Chen PT, Gung YW. Failure analysis: Enamel fracture after debonding orthodontic brackets. Angle Orthod. 2008;78:1071–7. doi: 10.2319/091907-449.1. [DOI] [PubMed] [Google Scholar]
- 19.Algera TJ, Feilzer AJ, Prahl-Andersen B, Kleverlaan CJ. A comparison of finite element analysis with in vitro bond strength tests of the bracket-cement-enamel system. Eur J Orthod. 2011;33:608–12. doi: 10.1093/ejo/cjq112. [DOI] [PubMed] [Google Scholar]
- 20.Finnema KJ, Ozcan M, Post WJ, Ren Y, Dijkstra PU. In-vitro orthodontic bond strength testing: A systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2010;137:615–622.e3. doi: 10.1016/j.ajodo.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 21.Katona TR. The effects of load location and misalignment on shear/peel testing of direct bonded orthodontic brackets – A finite element model. Am J Orthod Dentofacial Orthop. 1994;106:395–402. doi: 10.1016/S0889-5406(94)70061-3. [DOI] [PubMed] [Google Scholar]
- 22.Klocke A, Kahl-Nieke B. Influence of force location in orthodontic shear bond strength testing. Dent Mater. 2005;21:391–6. doi: 10.1016/j.dental.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Klocke A, Kahl-Nieke B. Effect of debonding force direction on orthodontic shear bond strength. Am J Orthod Dentofacial Orthop. 2006;129:261–5. doi: 10.1016/j.ajodo.2004.07.048. [DOI] [PubMed] [Google Scholar]
- 24.Murray SD, Hobson RS. Comparison of in vivo and in vitro shear bond strength. Am J Orthod Dentofacial Orthop. 2003;123:2–9. doi: 10.1067/mod.2003.49. [DOI] [PubMed] [Google Scholar]
- 25.Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am J Orthod. 1984;85:333–40. doi: 10.1016/0002-9416(84)90190-8. [DOI] [PubMed] [Google Scholar]
- 26.Horiuch S, Kaneko K, Mori H, Kawakami E, Tsukahara T, Yamamoto K, et al. Enamel bonding of self-etching and phosphoric acid-etching orthodontic adhesives in simulated clinical conditions: Debonding force and enamel surface. Dent Mater J. 2009;28:419–25. doi: 10.4012/dmj.28.419. [DOI] [PubMed] [Google Scholar]


