Abstract
Conventional orthognathic surgery treatment involves a prolonged period of orthodontic treatment (pre- and post-surgery), making the total treatment period of 3–4 years too exhaustive. Surgery-first orthognathic approach (SFOA) sees orthognathic surgery being carried out first, followed by orthodontic treatment to align the teeth and occlusion. Following orthognathic surgery, a period of rapid metabolic activity within tissues ensues is known as the regional acceleratory phenomenon (RAP). By performing surgery first, RAP can be harnessed to facilitate efficient orthodontic treatment. This phenomenon is believed to be a key factor in the notable reduction in treatment duration using SFOA. This article presents two cases treated with SFOA with emphasis on “case selection, treatment strategy, merits, and limitations” of SFOA. Further, salient features comparison of “conventional orthognathic surgery” and “SFOA” with an overview of author's SFOA treatment protocol is enumerated.
Keywords: Case series, salient features, surgery-first orthognathic surgery
INTRODUCTION
Combined surgical and orthodontic treatment of dentofacial deformity conventionally includes a prolonged period of presurgical orthodontic mechanotherapy (12–24 months) and often lengthy postsurgical orthodontic period resulting in an extended treatment time (3–4 years) which may be exhaustive for the patient to sustain.[1,2,3,4] In addition, the visual impact of unsightly fixed appliances and often worsening or aggravation of the existing deformity at dental and soft-tissue level during the pretreatment period, resulting from decompensatory tooth movements may lead to considerable patient dissatisfaction and may lead the patient to opt-out of treatment.[5] The surgery-first orthognathic approach (SFOA) has been introduced to offset the aforementioned untoward effects of conventional orthognathic surgery (i.e., prolonged treatment period, unsightly long-term braces visibility, worsened facial deformity, etc.,) yet, produce equally excellent results if carefully selected and appropriately managed.[6,7,8]
This article describes the nuances involved in the treatment of Class III skeletal deformity individuals treated with an SFOA. We present two cases treated with SFOA with emphasis on “case selection, treatment strategy, merits, and limitations” of SFOA. Further, salient features comparison of “conventional orthognathic surgery” and “SFOA” with an overview of author's SFOA treatment protocol is enumerated.
CASE REPORTS
Case 1
A 19-year-old male presented with chief complaints of protrusive lower front teeth and a large lower jaw. Extraoral examination reveals a concave profile, increased lower anterior face height, mild hypoplastic maxilla, positive lip step, hyperdivergent skeletal pattern, and a large mandible [Figure 1a-d]. Intraorally, he exhibits a Class III molar and canine relation, mild crowding of upper and lower anterior teeth, dental midlines matching, and reverse overjet of 3 mm [Figure 2a-e]. A cone beam computed tomography scan (CBCT) reveals the absence of skeletal asymmetry and no abnormality of the temporomandibular joint [Figure 3a-c].
Figure 1.
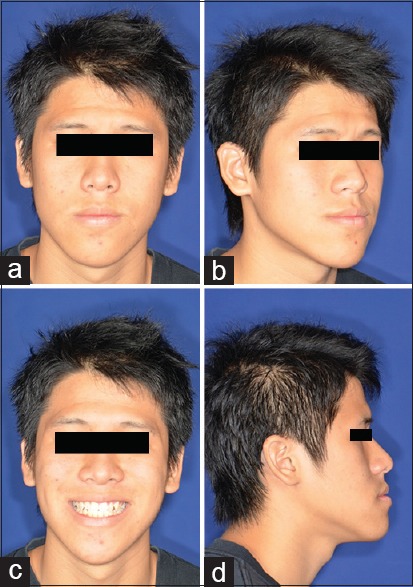
(a-d) Pretreatment extraoral photographs
Figure 2.
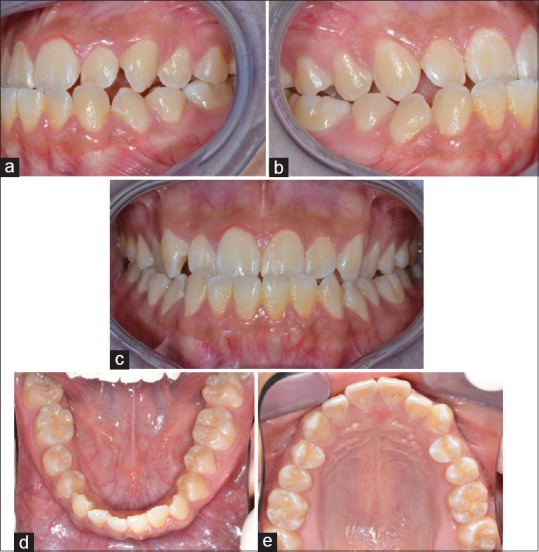
(a-e) Pretreatment intraoral photographs
Figure 3.

(a-c) Pretreatment cone beam computed tomography scan images showing Class III skeletal and dental features
Surgical plan
From the clinical presentation and CBCT scan evaluation, it was apparent that the Class III deformity was primarily due to a prognathic mandible in both vertical and anteroposterior planes. A surgery-first approach was planned to perform a bilateral sagittal split setback osteotomy (BSSO) combined with a vertical reduction genioplasty to correct the vertical mandibular excess. In addition, the mildly hypoplastic maxilla was addressed by an autogenic bone transplant.
Treatment progress
All teeth were bonded with 0.022” preadjusted brackets (Smartclip®, 3M Unitek, St Paul, MN, USA) [Figure 4a-e] and ligated with 0.010 stainless steel ligature wire. A face-bow transfer recorded the relationship of maxilla to the transverse horizontal hinge axis of the mandible [Figure 5]. The patient was subjected to a BSSO set-back and vertical reduction genioplasty of the mandible and autogenic bone transplant of the maxilla. Postsurgically, extraoral images [Figure 6a-d] revealed fulfillment of the surgery objectives. One-week postsurgery, 0.014” NiTi wires were placed in the upper and lower arches [Figure 7a-c], and subsequently, wires were changed to 0.016 × 0.022 NiTi archwires, and the case was finished in 0.017 × 0.025” stainless steel with second-order bends. The overall treatment time was 6 months from start to finish. Treatment results: Six months after surgery, the fixed appliances were removed, and posttreatment photographic images [Figures 8a-d and 9a-e] and CBCT [Figures 10a-c and 11] showed excellent esthetic and occlusal results [Figure 10d]. Pre- and post-treatment superimposition of lateral cephalogram show correction of Class III to Class I skeletal relation.
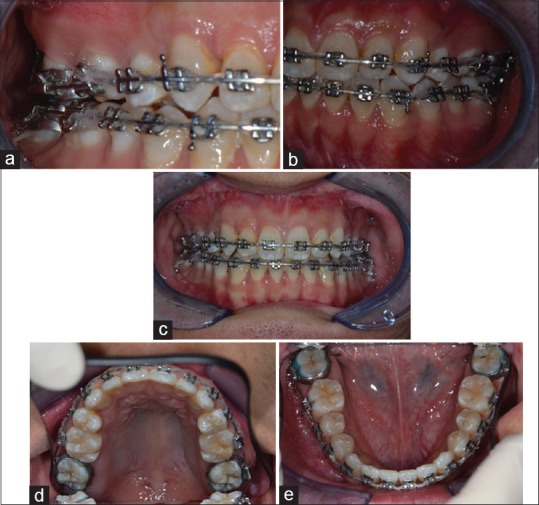
Figure 4.
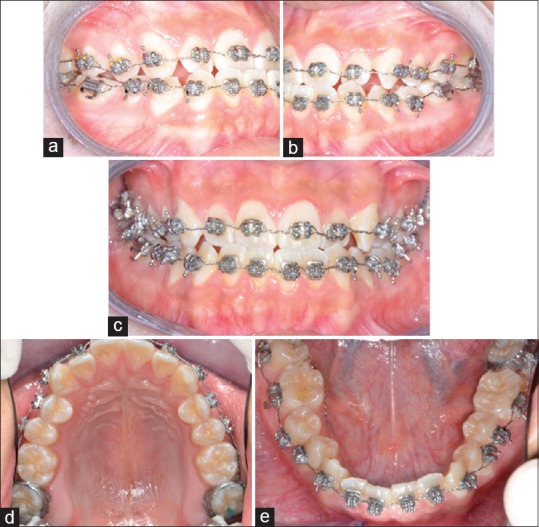
(a-e) Intraoral images showing bonded teeth with 0.022 “preadjusted brackets and ligated with 0.010” ligature wire
Figure 5.

Face-bow transfer was made to ensure the recording of positional relationship of maxillary arch to the temporomandibular joints
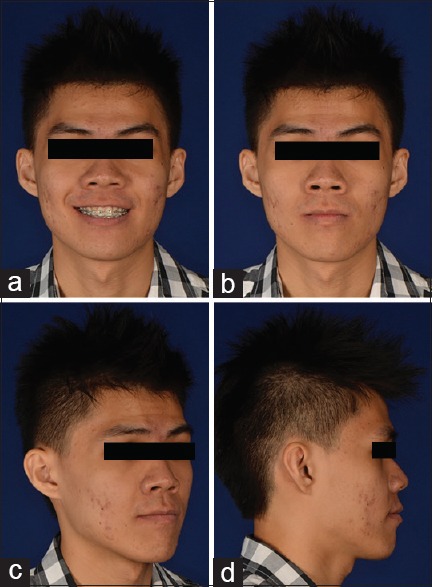
Figure 6.
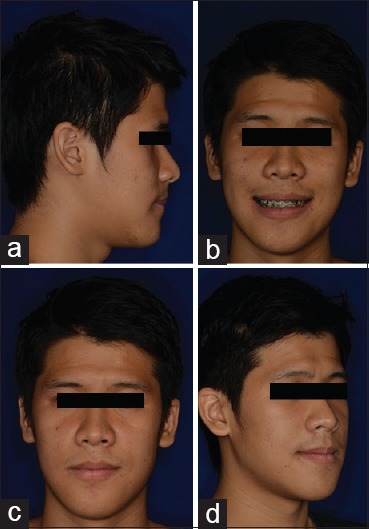
(a-d) Immediate postsurgical extraoral images showing fulfillment of surgical objective
Figure 7.
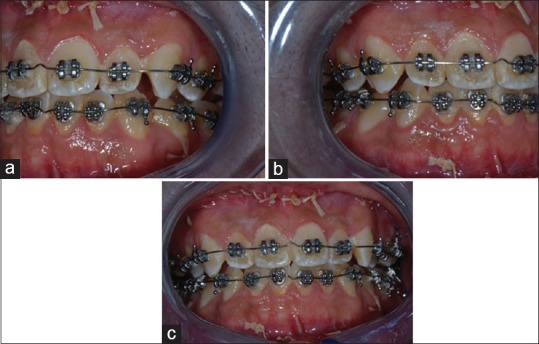
(a-c) Immediate postsurgical intraoral images showing a transitional occlusion wherein the occlusion is set-up such that the skeletal problem is resolved with near normal correction of overjet and overbite
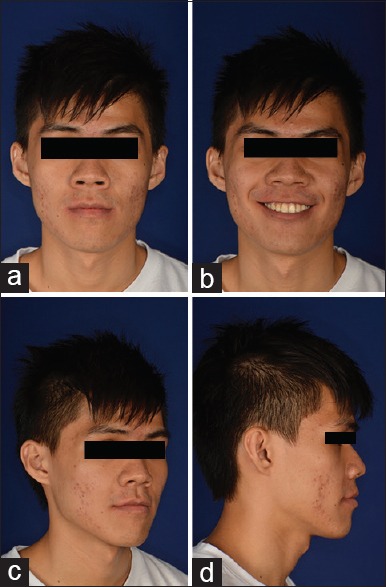
Figure 8.

(a-d) Posttreatment extraoral images showing achievement of orthognathic profile and esthetically pleasing features
Figure 9.

(a-e) Posttreatment intraoral images showing achievement of normal overjet and overbite
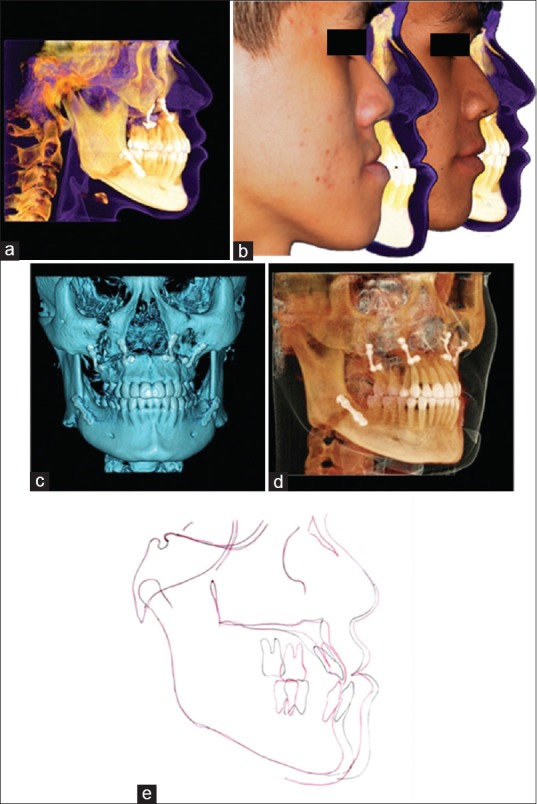
Figure 10.
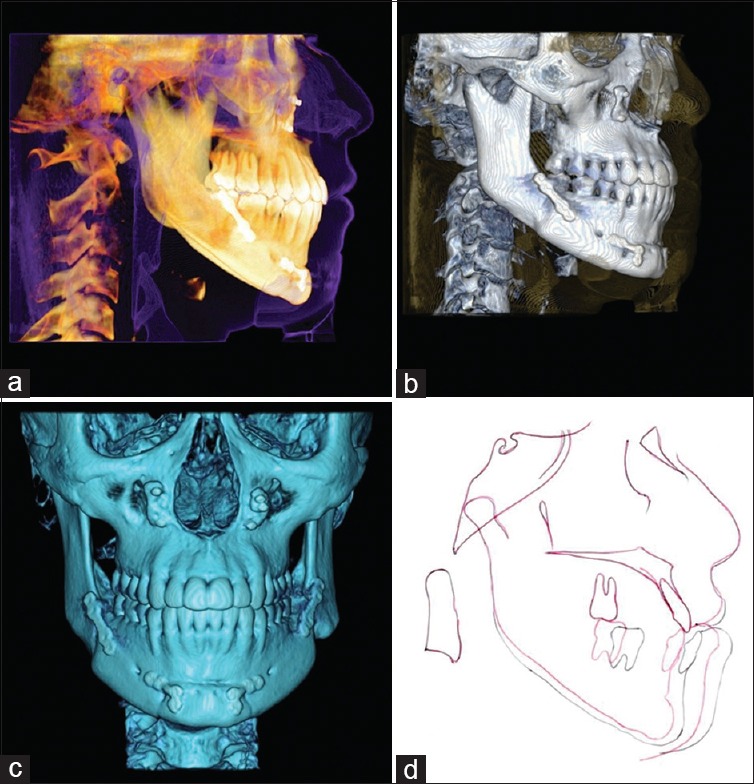
(a-d) Posttreatment cone beam computed tomography scan images showing orthognathic skeletal relationship with normal occlusion. Superimposition of pre (black) and posttreatment (red) lateral cephalometric tracings
Figure 11.
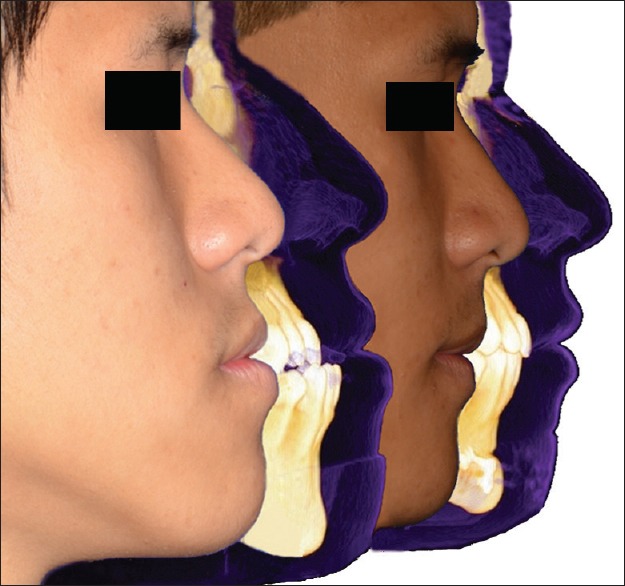
Profile views of pre- and post-treatment images superimposed to show the amount of correction
Case 2
A 21-year-old male reported to the orthodontic clinic with chief complaint of protrusive lower front teeth and large lower jaw. On examination, CBCT scan and extraoral images revealed a severe Class III profile with increased lower anterior face height, shallow mentolabial sulcus, positive lip step, and maxillary hypoplasia with no temporomandibular joint abnormality [Figure 12a-g].
Figure 12.
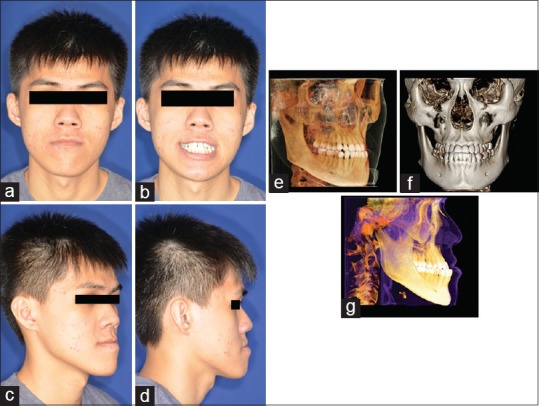
(a-g) Pretreatment extraoral photographs. Pretreatment cone beam computed tomography scan images showing Class III skeletal and dental features
Intraoral images revealed a full cusp Class III molar with Class III canine, midline diastema, upper incisor proclination, moderate upper and lower crowding, and reverse overjet of 6 mm [Figure 13a-e].
Figure 13.

(a-e) Pretreatment intraoral photographs
Surgical plan
Bimaxillary surgery with surgery-first approach was planned, wherein a BSSO mandibular setback and Lefort I maxillary advancement would be performed to address the Class III skeletal discrepancy.
Treatment progress
All teeth were bonded with 0.022” preadjusted brackets (Gemini®, 3M Unitek, St Paul, MN, USA). 0.014Ψ NiTi wire were placed in the upper and lower arches [Figure 14a-e] before a BSSO and Lefort I osteotomy of the mandible and maxilla, respectively, and upper bilateral second premolars were extracted. One-month postsurgically, 0.014” NiTi wire was placed. Bilateral upper first premolars were extracted to correct the proclination of upper anterior teeth. Subsequently, the initial wires were replaced by 0.016 × 0.022” NiTi upper and lower arches [Figure 15a-e]. Extraoral photographs at 2 months postsurgery showed good improvement [Figure 16a-d]. Subsequently, the case was finished with 0.017 × 0.025 TMA archwires having second-order bends. The overall treatment time took 9 months from start to finish. Treatment results: Posttreatment photographic images [Figures 17a-d and 18a-e] and CBCT showed great improvements in the profile. Class III facial pattern was changed to Class I profile with pleasing esthetics and good occlusion [Figure 19a-e].
Figure 14.

(a-e) Intraoral images showing bonded teeth with 0.022 “preadjusted brackets and placement of 0.014 ” upper and lower archwires
Figure 15.
(a-e) 0.016 × 0.022” NiTi upper and lower arches were placed 1-month postsurgery
Figure 16.
(a-d) Extraoral photographs at 2 months postsurgery showed achievement of promulgated objective
Figure 17.
(a-d) Posttreatment extraoral images
Figure 18.

(a-e) Posttreatment intraoral images
Figure 19.
(a-e) Posttreatment cone beam computed tomography scan images showing orthognathic skeletal relationship with normal occlusion. Profile views of pre- and post-treatment images superimposed to show the amount of correction. Posttreatment cone beam computed tomography scan images showing orthognathic skeletal relationship with normal occlusion. Superimposition of pre- (black) and post-treatment (red) lateral cephalometric tracing
DISCUSSION
Previously, authors who have reported treatment with the surgery-first technique have suggested several ways of securing brackets such as, use of rigid wires, passive NiTi wires, and passive ligation of brackets with stainless steel ligature wires conforming to malocclusion before surgery.[6,7,8,9] The authors of this article have used all the methods and conclude that any of the methods can be used prior to surgery; however, the most important factor to consider is the immediate movement of the teeth (approximately 1 week postsurgery) such that the regional acceleratory phenomenon (RAP) is utilized which begins immediately after surgery and lasts for approximately 3-month postsurgery.[9,10] Hence, irrespective of the bracket securing methods, the orthodontist has to move the teeth within the stipulated period of time such that RAP is utilized. RAP is the primary reason for entailing SFOA to significantly shorten treatment duration with fewer treatment stages, in comparison to conventional orthognathic treatment, along with the possibility of immediate correction of the problem.[9,11]
Several authors have enumerated advantages of SFOA, such as early correction of dentofacial deformities, rapid correction of malocclusion postsurgery, immediate gratification, significant decrease of total treatment time, and no presurgical orthodontics.[5,6,7,8,9,10] However, SFOA can be a successful modality of treatment, only if the case selection is carried out meticulously.
Case Selection for Surgery-first Orthognathic Approach
To begin with, cases with minimal dental discrepancies, in sagittal, vertical, and transverse planes could be assigned for surgery first, such as, in sagittal plane, mild proclination or retroclination of teeth; in the transverse plane, no posterior crossbite or collapsed bite; in the vertical plane, mild curve of Spee with no significant deep bite or open bite. However, more complex cases can be assigned for SFOA; several factors are to be taken into consideration, such as presurgical complexities (skeletal, dental and soft-tissue), orthodontic treatment mechanics (pre- and post-surgical), and transitional occlusion.
Vertical Discrepancy
Curve of Spee is given primary importance while correcting the vertical discrepancy. Curve of Spee can be leveled either by orthodontic treatment prior to surgery or by segmental osteotomy at the time of surgery. Several orthodontic treatment mechanics can be employed for correction of curve of Spee such as cantilever arm mechanics for intrusion of lower anterior teeth; skeletal anchorage placed in the anterior region of lower jaw for anterior teeth intrusion. Lower jaw segmental osteotomy may also be planned during surgery for the correction of curve of Spee.
Sagittal Discrepancy
The anteroposterior discrepancies such as maxillary dental proclination can be corrected by maxillary first premolar extraction or anterior segmental osteotomy. In the second case, extraction in the upper arch was carried out to correct the maxillary dental proclination, facilitated by the RAP that ensued immediately after surgery. This phenomenon, which generally lasts for 3 months postsurgery, can be utilized to correct any dental malocclusion.[7] In addition, a chin cap can be used postsurgically to retain the surgical correction of Class III skeletal discrepancies defined by a large mandible. A chin cap essentially prevents muscular and skeletal relapse and is usually indicated for 3–4 months postsurgery.
In the transverse plane, crossbite correction can be either corrected by orthodontic mechanics or during surgery. A transpalatal arch (0.032-inch TMA wire) is placed across the maxillary first molars and constricted so that a molar crossbite is corrected postsurgically with utilization of RAP. Alternatively, a narrow maxilla can be corrected either by maxillary osteotomy or by surgically assisted rapid palatal expansion (SARPE). A maxillary osteotomy needs careful evaluation and follow-up as it involves a complex surgical procedure requiring extended hospitalization which might increase the burden of care and financial costs. In addition, decreased blood flow to the osteotomy site might lead to avascular necrosis and pseudo-bone fusion. SARPE could be the treatment of choice in a severely collapsed maxillary arch as it allows constricted maxillary arch correction without untoward effects brought by orthodontic expansion such as buccal alveolar bone dehiscence and maxillary posterior tooth root resorption.[12,13,14]
Setting Up “Transitional Occlusion”
In the traditional orthognathic surgery approach, a presurgical orthodontic treatment is performed such that the dental component is decompensated to reveal the true skeletal discrepancy. The presurgical orthodontics ensures fabrication of a “surgical splint” such that the maxilla and mandible are placed in a “concrete occlusion” ensuring little or no postsurgical relapse. Unlike conventional orthognathic surgery, in SFOA, as teeth are malpositioned and lack proper occlusal antagonists in either arch, a “transitional occlusion” has to be set-up postsurgically. Some key elements must be considered for setting up a “transitional occlusion” during model surgery to emulate the actual surgical outcome, and they are as follows:
-
Sagittal plane:
- For minimal or moderate crowding cases: Establishing positive overjet or at least a “three point contact” with “two point” contacting at the posterior teeth preferably at bilateral molars, and “one point” at the anterior teeth such that a “tripod effect” is created
- For severely retroclined or crowded lower anterior teeth and proclined upper anterior teeth cases: Creation of larger positive overjet such that the large overjet can be utilized for lower incisors uprighting or decrowding, and retraction of proclined upper incisors.
-
Transverse plane:
- Intercanine and intermolar width of upper and lower dentition are maintained
- Crossbite not more than one buccal cusp width of maxillary molar.
-
Vertical plane:
- For hypodivergent skeletal pattern with deep curve of Spee: Edge to edge anterior teeth with no occlusion in the posterior teeth such that posterior teeth can be extruded postsurgically
- For hyperdivergent skeletal pattern with anterior open bite: Positive overjet with clockwise rotation of maxilla and anticlockwise rotation of mandible to counter postsurgical relapse of open bite.
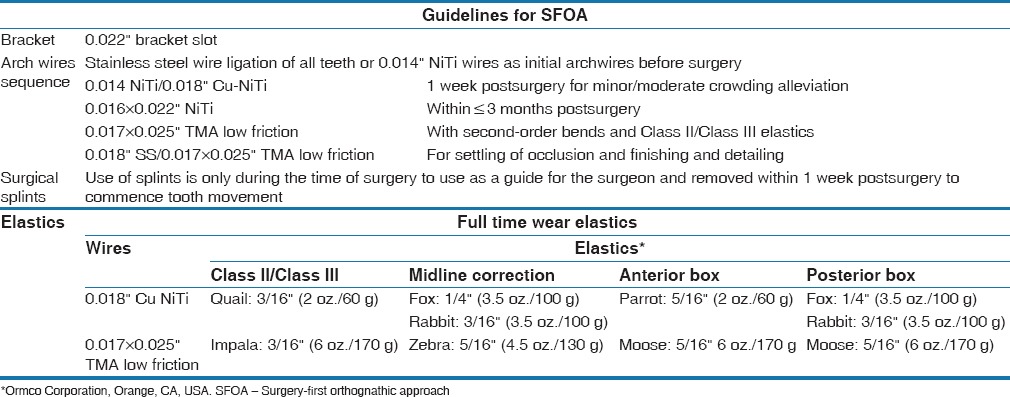
A full comparison of the salient features of SFOA and conventional orthognathic surgery is outlined in Table 1. The proposed treatment protocols for SFOA involving brackets, archwire sequence, surgical splints, and type of elastics are explained in Table 2.
Table 1.
Comparing salient features of “conventional orthognathic surgery” and Ysurgery-first orthognathic approach“

Table 2.
Author's treatment protocol for surgery first orthognathic approach involving brackets, archwire sequence, surgical splints, and type of elastics
One Patient Two Problems Concept
The authors endorse the fact that the SFOA is a “one patient two problem concept;” wherein, skeletal and dental are two separate problems which need to be addressed in one patient. Hence, in SFOA, first, the skeletal complexities are corrected by performing surgery and a “transitional occlusion” is set-up such that the second problem, which is the dental problem, is taken care off with regular orthodontic treatment utilizing RAP.
Skeletal anchorage, such as placement of miniplates, has been recommended to assist in challenging postsurgical movements as it provides three-dimensional control for correction of any relapse tendencies, or minor discrepancies ensued in comparison to actual planned surgical outcomes. Furthermore, skeletal anchorage system limits the excessive relying on usage of elastics.[11,15,16,17,18]
CONCLUSION
This paper describes dentofacial deformities treated with surgery-first approach and compare salient features of conventional surgery with SFOA. In addition, authors describe their SFOA-guidelines in bracket selection, archwire sequencing, surgical splint duration and elastics use. Although many advantages are evident with the SFOA, several factors have to be taken into account for the successful management of SFOA cases without compromising on the final outcome. The phenomenon of regional acceleration could be utilized to enhance faster tooth movement which considerably reduces treatment duration and may also present difficulties associated with tooth movement. It is imperative that the orthodontist and surgeon involved in SFOA should closely not only follow the orthognathic surgery principles but also understand the limitations of orthodontic teeth movement and the surgery-first approach. Meticulous treatment planning is deemed essential such that all the aspects of orthognathic surgery are carefully evaluated preoperatively and the necessary amount of dental correction (pre- or post-surgical), arch coordination, incisor decompensation taken into account. The surgeon should exhibit the ability to plan and perform surgery on malaligned, nondecompensated dental arches, according to the treatment plan. Finally, long-term studies comparing primary predictors of orthognathic surgery and surgery-first approaches outcomes are required so that additional clinical evidence may be established to support the surgery-first approach.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Proffit WR, White RP, Sarver DM, editors. Contemporary Treatment of Dentofacial Deformity. St. Louis, MO: Mosby; 2003. Combining surgery and orthognathics: Who does what, when? pp. 245–67. [Google Scholar]
- 2.Epker BN, Fish L. Surgical-orthodontic correction of open-bite deformity. Am J Orthod. 1977;71:278–99. doi: 10.1016/0002-9416(77)90188-9. [DOI] [PubMed] [Google Scholar]
- 3.Thornhill R, Gangestad SW. Facial attractiveness. Trends Cogn Sci. 1999;3:452–460. doi: 10.1016/s1364-6613(99)01403-5. [DOI] [PubMed] [Google Scholar]
- 4.Keim RG. Surgery-first orthognathics. J Clin Orthod. 2009;43:77–8. [PubMed] [Google Scholar]
- 5.Yu CC, Chen PH, Liou EJ, Huang CS, Chen YR. A Surgery-first approach in surgical-orthodontic treatment of mandibular prognathism – A case report. Chang Gung Med J. 2010;33:699–705. [PubMed] [Google Scholar]
- 6.Hernández-Alfaro F, Guijarro-Martínez R, Molina-Coral A, Badía-Escriche C. “Surgery first” in bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 2011;69:e201–7. doi: 10.1016/j.joms.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Liou EJ, Chen PH, Wang YC, Yu CC, Huang CS, Chen YR. Surgery-first accelerated orthognathic surgery: Postoperative rapid orthodontic tooth movement. J Oral Maxillofac Surg. 2011;69:781–5. doi: 10.1016/j.joms.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 8.Gandedkar NH. Surgery-first orthognathic approach: A KKH perspective. Spec Deliv. 2014;62:8–9. [Google Scholar]
- 9.Villegas C, Uribe F, Sugawara J. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44:97. [PubMed] [Google Scholar]
- 10.Frost HM. The biology of fracture healing. An overview for clinicians. Part II. Clin Orthop Relat Res. 1989;248:294–309. [PubMed] [Google Scholar]
- 11.Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery first” skeletal class III correction using the skeletal anchorage system. J Clin Orthod. 2009;43:97–105. [PubMed] [Google Scholar]
- 12.Nicholson PT, Plint DA. A long-term study of rapid maxillary expansion and bone grafting in cleft lip and palate patients. Eur J Orthod. 1989;11:186–92. doi: 10.1093/oxfordjournals.ejo.a035982. [DOI] [PubMed] [Google Scholar]
- 13.Alpern MC, Yurosko JJ. Rapid palatal expansion in adults with and without surgery. Angle Orthod. 1987;57:245–63. doi: 10.1043/0003-3219(1987)057<0245:RPEIA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Bishara SE, Staley RN. Maxillary expansion: Clinical implications. Am J Orthod Dentofacial Orthop. 1987;91:3–14. doi: 10.1016/0889-5406(87)90202-2. [DOI] [PubMed] [Google Scholar]
- 15.Sugawara J. Dr. Junji Sugawara on the skeletal anchorage system. Interview by Dr. Larry W. White. J Clin Orthod. 1999;33:689–96. [PubMed] [Google Scholar]
- 16.Umemori M, Sugawara J, Mitani H, Nagasaka H, Kawamura H. Skeletal anchorage system for open-bite correction. Am J Orthod Dentofacial Orthop. 1999;115:166–74. doi: 10.1016/S0889-5406(99)70345-8. [DOI] [PubMed] [Google Scholar]
- 17.Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44:97–103. [PubMed] [Google Scholar]
- 18.Sugawara J, Aymach Z, Nagasaka DH, Kawamura H, Nanda R. “Surgery first” orthognathics to correct a skeletal class II malocclusion with an impinging bite. J Clin Orthod. 2010;44:429–38. [PubMed] [Google Scholar]


