Abstract
Introduction
Trapeziometacarpal osteoarthritis is associated with more pain and restrictions than other hand osteoarthritis due to the functional importance of the thumb. While the effectiveness of surgical and pharmacological interventions has been widely examined, there is a lack of specific evidence about conservative non-pharmacological trapeziometacarpal osteoarthritis therapies. The objective of this systematic review was to provide evidence-based knowledge on the effectiveness of physiotherapy and occupational therapy on pain, function and quality of life.
Methods
A literature search of Medline, CINAHL, PEDro, OTseeker, EMB Dare Cochrane Database of Systematic Reviews and Cochrane CENTRAL was performed. Randomized and quasi-randomized controlled trials and corresponding systematic reviews, observational studies, pragmatic studies and case–control studies were included. The risk of bias was assessed.
Results
Out of 218 studies, 27 were retained. A narrative summary and a series of meta-analyses were performed. Concerning pain reduction, the meta-analysis showed parity of pre-fabricated neoprene and custom-made thermoplastic splints: standardized mean difference (SMD) –0.01 (95%CI −0.43, 0.40) (p=0.95). Multimodal interventions are more effective on pain compared to single interventions: standardized mean difference −3.16 (95%CI −5.56, −0.75) (p = 0.01).
Discussion
Physical and occupational therapy-related interventions, especially multimodal interventions, seem to be effective to treat pain in patients with trapeziometacarpal osteoarthritis. Pre-fabricated neoprene splints and custom-made thermoplastic splints may reduce pain equally. Single interventions seem not to be effective. Significant evidence for effectiveness on function and quality of life could not be found.
Keywords: Review, thumb, physiotherapy, occupational therapy, osteoarthritis
Introduction
The ability to oppose the thumb is made possible primarily by the anatomy and biomechanics of the trapeziometacarpal joint. Its special anatomical shape allows a high degree of mobility, i.e. the freedom to move in all directions. But it may also favor instability which can facilitate osteoarthritis of this joint.1 Depending on the selected diagnostic criterion (radiological or clinical), the prevalence rates of trapeziometacarpal osteoarthritis (TMC OA) may vary between 35.8% (radiological2) to 15% in women and 7% (radiological3) to 1.4%(clinical4) in men. This quantitative discrepancy is explained by the fact that radiological findings do not necessarily correlate with clinical findings.2 The clinical diagnosis-based prevalence may seem low but because of the important functional significance of the thumb, TMC OA causes, in addition to considerable pain, more significant restrictions in work and everyday life compared to osteoarthritis of other fingers.5
The aetiology of TMC OA has yet to be confirmed, and the treatment strategy may be surgical or conservative.6 This decision depends on the patient and their complaints. While the results of surgical procedures have been well studied, gaps remain in research regarding the effectiveness of conservative, occupational and physiotherapy treatment interventions in TMC OA patients.
As Davenport7 stated, hand therapists use a range of treatment modalities whose efficacy and efficiency need to be examined. Many interventions are based on research evidence on osteoarthritis (OA) affecting other joints or on expert opinion, while evidence for treatment modalities of OA in the TMC joint is still lacking. Despite this lack of evidence, conservative treatment seems beneficial. Berggren et al.8 observed a significant reduction in the number of patients requiring surgery after conservative treatment. O'Brien and Giveans9 suggested that assessment and treatment by a non-surgical healthcare provider were associated with a decrease in the rate of surgical interventions, underscoring the importance of conservative hand therapy.
Several systematic reviews have examined conservative treatment modalities of hand OA, regardless of the specific joints.10–13 Two recent systematic reviews have examined specifically TMC OA.14,15 However, Spaans et al.14 included pharmacological interventions and neither examined important physiotherapeutic interventions (e.g. exercise therapy) nor differentiated between different types of splints. Bertozzi et al.15 did not focus solely on treatments for TMC OA but included, in addition, studies on treatment modalities for hand OA in general.15 Further, both systematic reviews included only randomized controlled studies (RCT) and excluded all studies with another research design. Meanwhile, because of the specifics of research in rehabilitation, and to obtain a full picture of the problem, it may be appropriate to include also non-RCT studies in a systematic review.16
Therefore, the aim was to conduct a systematic review and meta-analysis to explore the effectiveness of physical and occupational therapy-related interventions on pain, function and quality of life in patients with TMC OA.
Methods
A research protocol was developed and submitted for registration with PROSPERO (accepted on 30 November 2013; registration number CRD42013006282). All protocol revisions were accepted.
Randomized and quasi-randomized controlled trials and corresponding systematic reviews, as well as observational studies, pragmatic studies and case–control studies were eligible for inclusion. Language restriction was set to English, German, French and Dutch. Studies on adults with formal diagnosis of primary TMC OA were eligible for inclusion. Interventions named occupational or physical therapy or physiotherapy were included. Excluded were studies with participants under 18 years of age or suffering from secondary TMC OA or rheumatoid arthritis or any other rheumatologic problem, or any kind of hand surgery or traumatic hand lesions. No date limitation was planned. Control interventions were accepted as presented in the studies. Outcome variables under investigation were pain, function and quality of life. The search strategy contained all relevant terms (Table 1) and was peer-reviewed by an independent researcher with experience in conducting systematic reviews and meta-analyses. The following databases were searched in April 2014: MEDLINE (PubMed), CINAHL, OTseeker, EMB DARE, PEDro, Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL). The reference lists of included articles were screened for further eligible studies. Relevant journals and conference proceedings were searched by hand. An automatic PubMed algorithm continued the search for later updates until August 2015.The other databases were searched monthly until August 2015.
Table 1.
Search terms.
| Key words | MEDLINE pubmed |
|---|---|
| 1. Osteoarthritis | Osteoarthrit* |
| 2. Osteoarthrosis | Osteoarthros* |
| 3. Degenerative arthrosis | – |
| 4. Rhizarthrosis | Rhizarthr* |
| 5. Thumb | Thumb |
| 6. Carpometacarpal joints | Carpometacarpal |
| 7. CMC I | CMC I |
| 8. Trapeziometacarpal joint | Trapeziometacarpal |
| 9. Physical therapy | Physical therapy modalities |
| 10. Physiotherapy | Physiotherapy |
| 11. Occupational therapy | Occupational |
| 12. Exercise | Exercise |
| 13. Exercise therapy | Exercise therapy |
| 14. Manual therapy | Manual therapy |
| 15. Passive movement | Passive movement |
| 16. Active movement | Active movement |
| 17. Passive mobilisation | Passive mobilisation |
| 18. Passive mobilization | Passive mobilization |
| 19. Physical training | – |
| 20. Strengthening | Strength* |
| 21. Thermotherapy | Thermotherapy |
| 22. Heat | Heat therapy |
| 23. Paraffin | – |
| 24. Cryotherapy | Cryotherapy |
| 25. Cold | – |
| 26. Hydrotherapy | Hydrotherapy |
| 27. Electrotherapy | Electrotherapy |
| 28. Ultrasound | Ultrasound therapy |
| 29. TENS | TENS |
| 30. Transcutaneous electrical stimulation | – |
| 31. Splinting | Splint* |
| 32. Orthosis | Ortho* |
| 33. Traction | Traction |
| 34.Patient education | Patient education |
| 35. Pain management | Pain management |
| 36. Joint protection | Joint protection |
| 37. Ergonomics | Ergonomic* |
| 38. Pain | Pain |
| 39. Function | Function |
| 40. Quality of life | Quality of life |
| 41. Intervention | – |
| 42. Strategy | – |
| 43. Rehabilitation | Rehabilitation |
| 44. Randomized controlled trial | – |
| 45. Randomized clinical trial | Randomized clinical trial |
| 46. Systematic review | Systematic review |
| 47. Meta-analysis | Meta-analysis |
| 48. Observational study | Observational |
| 49. Pragmatic study | Pragmatic |
| 50. Case–control study | Case–control |
| 51. Longitudinal study | Longitudinal |
| 52. Prospective | Prospective |
| 53. Cohort | Cohort |
After removing duplicates, two reviewers (BA and SE) independently screened titles and abstracts for studies which did not meet inclusion criteria. Subsequently, the two reviewers extracted all data from the included studies onto a standardized, pre-defined data form. Risk of bias was assessed independently by the same two reviewers by means of the pre-defined RevMan criteria (Review Manager 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).This risk of bias assessment tool can be used for both RCTs and non-RCTs (Cochrane Handbook for Systematic Reviews of Interventions 13.5.2.3). Any disagreement was resolved through discussion.
As a first step, a narrative review was carried out. For each study, we assigned symbols (+ = positive effect/− = no positive effect) for the outcome of an intervention as reported in the authors' conclusions. Where different time points were available, we chose the outcome closest to the end of the intervention. Then, in an attempt to quantify objectively the narrative summary, different meta-analyses were conducted. For the studies included in the meta-analyses, effect sizes have been calculated. These meta-analyses were computed only when the key elements were comparable (population, intervention and outcome). For pragmatic reasons, a certain amount of heterogeneity and risk of bias were accepted. The standardized mean difference (SMD) to express individual studies' effect sizes and a random effects model were chosen a priori. Hedge's g was used to correct for possible small sample bias. It is implemented in RevMan 5.3 algorithms. Weights of the individual studies were based on the inverse variance method. RevMan 5 in the non-Cochrane Mode was used for the calculations. Cohen's d benchmarking was used to allow a clinical interpretation of the observed overall weighted mean effect sizes.17
Results
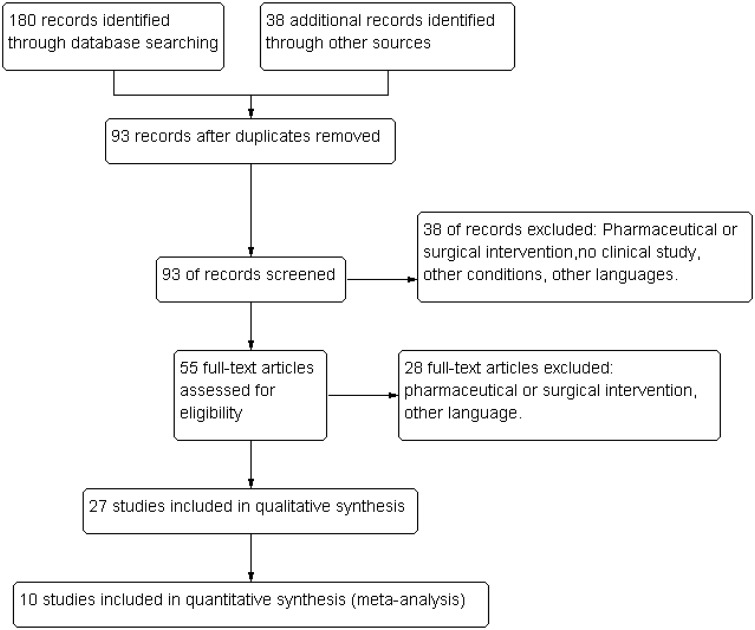
Two hundred and eighteen studies were found initially and assessed for eligibility. After removing duplicates, 93 studies remained. After screening of titles and abstracts, 38 studies were excluded. Reasons for exclusion were studies being related to drugs, surgery, non-clinical study, other condition and other language. The full texts of the remaining 55 studies were read leading to the exclusion of another 28 studies (for reasons of other language, surgery and drugs). Twenty-seven studies totaling 1179 patients could be included for analysis: 10 RCTs with sham intervention or usual care for the control group, seven parallel group studies without control group, five cross-sectional design studies, three observational studies and two retrospective studies (Figure 1). The outcome time frame presents a very wide range, from 1 week to 7 years, for most studies from 2 weeks to 3 or 4 months. Risk of bias was assessed for seven criteria (online supplementary tables 2 and 3). All studies presented at least one high or unclear risk of performance bias (blinding of participants and personnel). Furthermore, 11 studies had a high risk in two or more out of seven criteria. Only eight studies had no high risk of bias, despite presenting at least two unclear risk assessments."]
Figure 1.
Flow chart.
The online supplementary table 1 depicts an overview of the study characteristics. Forty-two interventions were compared. The different interventions observed in the studies are summarized in Table 2. Table 3 presents the effects on the outcomes. While no study evaluated quality of life, all but two studies examined at least one of the two other outcomes (pain or function).8,18
Table 2.
Interventions (numbers refer to frequency with which an intervention was examined).
| List of interventions in included studies: | ||
| Pre-fabricated neoprene splint | 7 | |
| Custom-made thermoplastic splint | 13 | |
| Laser or nettle sting or acupuncture | 1 | |
| Advice | 1 | |
| Advice + technical accessoires | 1 | |
| Advice + technical accessories + splint | 2 | |
| Joint protection (JP) | 1 | |
| JP + splint + hot pack + exercises | 1 | |
| Specific exercises | 1 | |
| General exercises | 2 | |
| Exercises + splint | 3 | |
| Heat + exercises + splint + JP | 1 | |
| Exercises + splint + JP | 1 | |
| Neurodynamic mobilization | 2 | |
| Manual therapy | 2 | |
| Manual therapy + neurodynamic mobilization + exercises | 1 | |
| Summary of interventions: | ||
| Splint only | 20 | 47.6% |
| Multimodal | 6 | 14.3% |
| Single interventions | 3 | 7.1% |
| Exercises + splint | 3 | 7.1% |
| Exercices only | 3 | 7.1% |
| Advice or joint protection or technical accessories | 3 | 7.1% |
| Neurodynamic mobilization | 2 | 4.8% |
| Manual therapy | 2 | 4.8% |
Table 3.
Effects on outcomes.
| Outcome | Intervention | Results according to authors conclusions + = positive effect − = no positive effect | Study |
|---|---|---|---|
| Pain | Pre-fabricated neoprene splint | + | Bani 2013, Bani 2013a,28 Bani 2014,29 Becker 2013,30 Buurke 1999,31 Sillem 2011,32 Weiss 200433 |
| Custom-made thermo splint | + | Bani 2013,27 Bani 2013a,28 Bani 2014,29 Becker 2013,30 Buurke 1999,31 Carreira20, McKee 2006,34 Sillem 2011,32 Swigart et al.18, Weiss22, Weiss 200433 | |
| Custom-made neoprene splint + usual care | + | Rannou 200935 | |
| Laser | − | Basford et al.19 | |
| Joint protection (JP) | + (only for pain in motion) | Boustedt et al.21 | |
| JP + splint + hot pack + exercises | + | Boustedt et al.21 | |
| Soft splint + general exercises | + | Hermann 201436 | |
| Thermoplast CMC splint + abduction exercises | + | Wajon 200537 | |
| Thermoplast short splint + pinch exercises | + | Wajon 200537 | |
| Heat + exercises + splints + JP | + | Merrit 201238 | |
| Exercises + splints + JP | + | O'Brien and Giveans9 | |
| Passive mobilization + neurodynamic mobilization + exercises | + | Villafane 201339 | |
| Specific exercises | + | Davenport 201240 | |
| General exercises | + | Davenport 2012;40 Hermann 201436 | |
| Acupuncture | + | Dickens 198941 | |
| Nettle sting | + | Randall 200042 | |
| Median nerve mobilization | + | Villafane 201143 | |
| Radial nerve mobilization | + | Villafane 201244 | |
| Kaltenborn manual mobilization | + | Villafane 201145 | |
| Maitland mobilization | + | Villafane 2012a46 | |
| Function/DASH/QuickDASH | Pre-fabricated neoprene splint | + | Bani 2013,27 Bani 2014,29 Becker 201330 |
| Custom-made thermoplastic splint | + − | Bani 2013,27 Bani 2013a,28 Becker 201330 Carreira et al.20 | |
| Joint protection (JP) | − | Boustedt et al.21 | |
| JP + splint + hot pack + exercises | + | Boustedt et al.21 | |
| Specific exercises | + | Davenport 201240 | |
| General exercises | + | Davenport 201240 | |
| Multimodal (exercises + splint + JP) | + | O'Brien 20139 | |
| Function/Green test | Different splints | + | Buurke 199931 |
| Function/AUSCAN | Exercises + soft splint | + | Hermann 201436 |
| Exercises | + | Hermann 201436 | |
| Multimodal (heat + exercises + splint + JP) | + | Merrit 201238 | |
| Pre-fabricated neoprene splint | + | Sillem 201132 | |
| Custom-made hybrid splint | + | Sillem 201132 | |
| Function/PRWHE 10 point | Splint with mcp | + | McKee 200634 |
| Splint without mcp | + | MecKee 200634 | |
| Function/Stanford Health assessment questionnaire | Nettle sting | + | Randall 200042 |
| Function/Cochin hand function scale | Custom-made neoprene splint + usual care | + | Rannou 200935 |
| Function/Sollerman test of hand function | Thumb base splint + abduction exercises | + | Wajon 200537 |
| Short opponens splint + pinch exercises | + | Wajon 200537 | |
| Function/ADL self-rating scale | Custom-made short splint | + | Weiss22 |
| Custom-made long splint | − | Weiss22 | |
| Pre-fabricated long neoprene splint | + | Weiss 200433 | |
| Custom-made short thermoplast splint | + | Weiss 200433 | |
| Strength/pinch + grip | Prefabricated neoprene splint | + − grip | Bani 2013,27 Becker 2013,30 Sillem 201132 Bani 201327 |
| Custom-made thermos plastic | + − | Bani 2013,27 Bani 2013a,28 Bani 2014,29 Becker 2013,30 Sillem 201132 Carreira 2010,20 Weiss 200022 | |
| Splint with CMC | + | McKee 200634 | |
| Splint with CMC + mcp | + pinch − grip | McKee 200634 | |
| Joint protection | − | Boustedt 200921 | |
| Multimodal (heat + exercises + splints + JP) | − | Merrit 201238 (pinch only) | |
| Multimodal (JP + splint + hot pack + exercise) | + | Boustedt et al.21 | |
| Multimodal (joint mobilization + neurodynamic mobilization + exercises) | − | Villafane 201339 | |
| Specific exercises | + | Davenport 201240 (pinch only) | |
| General exercises | + | Davenport 201240 (pinch only), Hermann 201436 | |
| Exercises + splint | + | Hermann 201436 | |
| Thumb base splint + abduction exercises | + | Wajon 200537 | |
| Short opponens splint + pinch exercises | + | Wajon 200537 | |
| Acupuncture | − | Dickens 198941 (pinch only) | |
| Median nerve mobilization | − pinch + grip | Villafane 201143 | |
| Kaltenborn mobilization | − | Villafane 201145 | |
| Radial nerve mobilization | + | Villafane 201244 | |
| Maitland mobilization | − | Villafane 2012a46 |
Pain was reduced by all but one intervention.19 Function was improved in all but three studies (custom-made thermoplastic splint,20 joint protection21 and custom-made thermoplastic long splint22). Analyzing the interventions, we found that all splints seem to bring a positive result for pain regardless of their make and design. Likewise, all splint studies except two report improvement of function. The exceptions are Carreira20 for custom-made thermoplastic splint and Weiss22 for long custom-made thermoplastic splint. All multimodal interventions improved pain and function. Interventions consisting of exercises with or without splint improved all outcomes. The exercise regimens consisted of stabilization, standardized range of motion, general strengthening, abduction, pinch and thumb web exercises and were different in each study. Joint protection solely improved pain but not function. Neurodynamic mobilization (mobilization of median or radial nerve) and manual therapy (Kaltenborn passive posterior-anterior gliding) improved pain. Laser was tested only for pain without positive effect. Acupuncture was tested positively for pain. Nettle sting showed positive results for pain and function. Basford et al.19 could not confirm a pain reducing effect of laser therapy in TMC OA patients. This narrative summary showed a positive overall effect of physiotherapy and occupational therapy-related interventions on pain and function in patients with TMC OA.
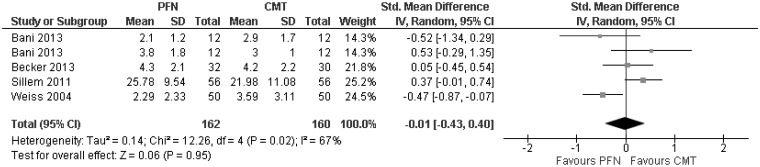
Two meta-analyses on the main outcome of pain could be performed. The first meta-analysis compared the pain reducing effect of pre-fabricated neoprene splint versus custom-made thermoplastic splint in five studies totaling 332 patients. This analysis found no difference between the study groups. The overall weighted mean effect size expressed as SMD was −0.01 (95%CI = −0.43, 0.40) (p = 0.95) (Figure 2).
Figure 2.
PFN vs. CMT/pain.
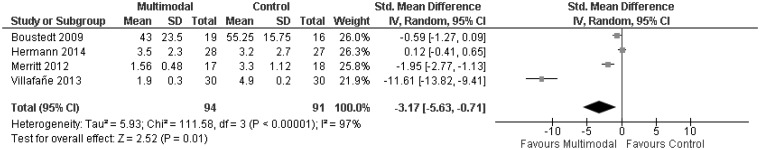
A second meta-analysis including four studies and 175 patients compared multimodal interventions to reduce pain versus control in TMC OA patients. This analysis showed a very high effect size favoring the multimodal interventions: SMD = −3.16 (95%CI = −5.56, −0.75) (p = 0.01) (Figure 3).
Figure 3.
Multimodal vs. control/pain.
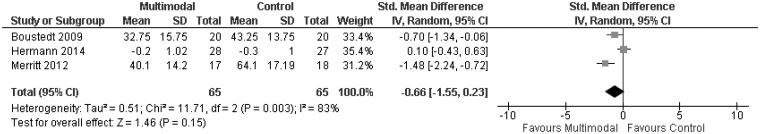
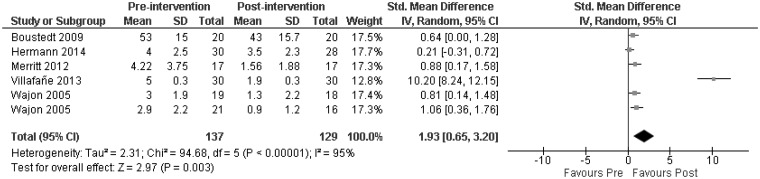
A third meta-analysis was conducted to compare the effect of multi-modal interventions on function in TMC OA patients versus control. The overall weighted effect size expressed as SMD was high: SMD = −0.66 (95%CI = −1.55, 0.23) (p = 0.15) (Figure 4), but without statistical significance. A last meta-analysis was conducted to explore the before and after effect of multimodal interventions on pain (no controls) including six studies totaling 266 patients. The overall weighted mean effect size was very high: SMD = 1.93 (95%CI = 0.65, 3.20) (p = 0.003) (Figure 5).
Figure 4.
Multimodal vs. control/function.
Figure 5.
Multimodal pre–post/pain.
Discussion
Summary of evidence
This review including a systematic review and meta-analyses explored the effectiveness of physical and occupational therapy related interventions on pain and function in patients with TMC OA. The main finding was that there is moderate to high evidence that multimodal physiotherapy and occupational therapy related interventions have beneficial effects on pain. Concerning improvement of function, there is only narrative but no statistical evidence. Interestingly, quality of life was not examined by any of the studies. It can be assumed that absence of symptoms (e.g. pain and functional disorder) is associated with a higher quality of life.18 If this assumption holds, then the results of this review suggest that most physiotherapy or occupational therapy related interventions also improve quality of life. Valdes et al.11 referred to different studies which underscore the relation between pain reduction and improved hand functioning and global rating of disease in patients with hand OA. Frouzakis et al.23 confirm that most patients seek treatment to reduce pain and not to improve function or activities of daily living (ADL).
Despite major differences in design or outcomes, three studies (need for surgery;8 retrospective chart review;9 retrospective cohort study18) were included in this systematic review because of their clinical interest.
The narrative interpretation of the results, based on the conclusions of the individual studies, suggested that pain was improved with all intervention modalities except for laser therapy.19 However, on many occasions in this overview, a certain discrepancy between the authors' conclusions and the reported data was observed. In some of the studies, data were missing or even contradictory to the conclusions. Some conclusions were based on selected time points, while other time points with other results were not further mentioned, indicating a high risk for reporting bias.
As Marks et al.24 already highlighted, all studies had in common a wide variety of measurement methods for all outcomes, e.g. for pain: pain in the most recent week, pain during motion, pain at rest, pain during or after strength measurement, and so on. Moreover, the scales used in the included studies varied widely. For pain VAS, NRS, AUSCAN pain subscale, 10-point scale or verbal rating scale. For function, DASH, Quick DASH, AUSCAN, Green Test, Cochin hand function scale, Stanford Health Assessment, 10-point PRWHE scale and others.
Taken together, most studies showed poor quality and the across study heterogeneity was high, making pooling of the data to assess a true effect on population level difficult. Therefore, the reader would be reduced to pure vote-counting, which can lead to erroneous conclusions. To counter this risk, we decided to add meta-analyses for the studies presenting enough homogeneity in the key factors. This procedure is acceptable in the context of the chosen goal.25 Based on the findings of Marks et al.,24 we decided a priori to calculate the SMD instead of the mean difference.
Neither the narrative summary nor the meta-analyses showed a difference between pre-fabricated neoprene splints and custom-made thermoplastic splints, while there is moderate to high evidence that multimodal interventions may be efficient forms of treatment in patients with TMC OA. This finding is confirmed by Berggren et al.8 and O'Brien and Giveans.9 The SMDs found in the two meta-analyses for multimodal interventions (−3.17 and 1.93) have clinical significance.26
There is not enough evidence to support single interventions such as exercises, joint protection, neurodynamic mobilization, manual therapy, laser, nettle sting or acupuncture.
This review showed evidence that a multimodal physical or occupational therapy may be effective in the treatment of patients with TMC OA. Such multimodal approach could consist of splint application combined with an exercise program, patient education on joint protection, advice about technical accessories (e.g. ergonomic bottle openers or key holders) and techniques to increase the local metabolism (heat, deep frictions, ultrasound and others). Based on the evidence, the type of exercises (specific or general) integrated into a multimodal intervention seems to be irrelevant. The parity of splints concerning pain reduction has been shown. Therefore, the choice of the best splint has to be checked individually. The chosen splints should be adapted to the type of activity (hard work = thermoplastic splint, normal ADL and sleep = soft splint).
Strengths
This review included not only RCTs, but also studies with other designs, allowing a broader analysis of the effectiveness of physiotherapy or occupational therapy-related interventions on patients with TMC OA. The inclusion of the studies in the meta-analyses was done on the assumption of clinical value and based on clinical expertise.
This review may have clear clinical relevance. While there is no evidence to support single interventions, there seems to be moderate to high evidence that multimodal physical or occupational therapy related interventions may be effective in the treatment of pain and function of the hand in patients with TMC OA.
Limitations
Overall, the included studies present a moderate to high risk of bias. While the risk for performance bias through lack of blinding of participants and personnel is inherent in physical rehabilitation studies, other risks could theoretically be avoided. This elevated level of risk of bias asks for a conservative interpretation of the results. Another limitation of some studies is the lack of indication whether the participants had only isolated TMC OA or not. It may well be that patients with OA in several finger joints react differently to interventions and at measurements.
A number of other limitations of this review are recognized. First, non-published trials were not systematically searched for and this exclusion may have resulted in a biased selection of trials which were more likely to include positive trials. Second, other language publications were only included if they had an accompanying English abstract which summarized sufficient details of the trial report. Third, the procedure to include the studies in the meta-analyses was based on subjective clinical values and expertise of the authors after a consensus meeting. And finally, the number of the studies and patients included in the pooling was low.
Conclusions
This review included a systematic review with a narrative summary and a series of meta-analyses. Physical and occupational therapy-related interventions, especially multimodal interventions, seem to be effective to treat pain in patients with TMC OA. The use of pre-fabricated neoprene splints and custom-made thermoplastic splints may result in similar pain reduction. There is only narrative but not statistical evidence for effectiveness of single interventions on pain. The same has been found for improvement of function.
Multimodal interventions may need more resources. Therefore, more large and high quality studies, with embedded economic analyses are needed to further strengthen the evidence and cost-effectiveness of different types of multimodal physiotherapy or occupational therapy related interventions in patients with TMC OA.
Supplementary Material
Acknowledgements
The authors thank Roger Hilfiker for peer-reviewing the search strategy, Anne-Kathrin Rausch-Osthoff for peer-reviewing the manuscript and Daniel Fooder for the English editing and proof-reading.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received financial support from the Swiss Society for Hand Rehabilitation SGHR and the Swiss Physiotherapy Association physioswiss.
Online only supplementary tables are available at http://hth.sagepub.com/content/early/recent
References
- 1.Hunter DJ, Zhang Y, Sokolve J, et al. Trapeziometacarpal subluxation predisposes to incident trapeziometacarpal osteoarthritis (OA): the Framingham study. Osteoarthr Cartil 2005; 13: 953–957. [DOI] [PubMed] [Google Scholar]
- 2.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, et al. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (The Rotterdam Study). Ann Rheum Dis 2005; 64: 682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haara MM, Arokoski JP, Kroger H, et al. Association of radiological hand osteoarthritis with bone mineral mass: a population study. Rheumatology 2005; 44: 1549–1554. [DOI] [PubMed] [Google Scholar]
- 4.Wolf J, Turkiewicz A, Atroshi I, et al. Prevalence of doctor-diagnosed thumb carpometacarpal joint osteoarthritis: analysis of Swedish health care. Arthritis Care Res 2013; 66: 961–965. [DOI] [PubMed] [Google Scholar]
- 5.Bijsterbosch J, Visser W, Kroon H, et al. Thumb base involvement in symptomatic osteoarthritis is associated with more pain and functional disability. Ann Rheum Dis 2010; 69: 585. [DOI] [PubMed] [Google Scholar]
- 6.Hamann N. Stabilization effectiveness and functionality of different thumb orthoses in female patients with first carpometacarpal joint osteoarthritis. Clin Biomech 2014; 29: 1170–1176. [DOI] [PubMed] [Google Scholar]
- 7.Davenport BJ. An investigation into therapist's management of osetoarthritis of the carpometacarpal joint of the thumb in the UK. Hand Ther 2009; 14: 2–9. [Google Scholar]
- 8.Berggren M, Joost-Davidsson A, Lindstrand J, et al. Reduction in the need for operation after conservative treatment of osteoarthritis of the first carpometacarpal joint: a seven year prospective study. Scand J Plast Reconstr Surg Hand Surg 2001; 35: 415–417. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien VH, Giveans MR. Effects of a dynamic stability approach in conservative intervention of the carpometacarpal joint of the thumb: a retrospective study. J Hand Ther 2012; 26: 44–51. [DOI] [PubMed] [Google Scholar]
- 10.Ye L, Kalichman L, Spittle A, et al. Effects of rehabilitative interventions on pain, function and physical impairments in people with hand osteoarthritis: a systematic review. Arthritis Res Ther 2011; 13: R28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther 2009; 23: 334–350. [DOI] [PubMed] [Google Scholar]
- 12.Moe RH, Kjeken I, Uhlig T, et al. There is inadequate evidence to determine the effectiveness of nonpharmacological and nonsurgical interventions for hand osteoarthritis: an overview of high-quality systematic reviews. Phys Ther 2009; 89: 1363–1370. [DOI] [PubMed] [Google Scholar]
- 13.Towheed TE. Systematic review of therapies for osteoarthritis of the hand. Osteoarthritis Cartilage 2005; 13: 455–462. [DOI] [PubMed] [Google Scholar]
- 14.Spaans AJ, van Minnen LP, Kon M, et al. Conservative treatment of thumb base osteoarthritis: a systematic review. J Hand Surg Am 2015; 40: 16–21. [DOI] [PubMed] [Google Scholar]
- 15.Bertozzi L, Valdes K, Vanti C, et al. Investigation of the effect of conservative interventions in thumb carpometacarpal osteoarthritis: systematic review and meta-analysis. Disabil Rehabil 2015; 37: 2025–2043. [DOI] [PubMed] [Google Scholar]
- 16.Brown P, Harniss MK, Schomer KG, et al. Conducting systematic evidence reviews: core concepts and lessons learned. Arch Phys Med Rehabil 2012; 93: S177–S184. [DOI] [PubMed] [Google Scholar]
- 17.Streiner DL, Norman GR. Health measurment scales – a practical guide to their development and use, 4th ed Oxford: Oxford University Press, 2008, pp. 153. [Google Scholar]
- 18.Swigart CR, Eaton RG, Glickel SZ, et al. Splinting in the treatment of arthritis of the first carpometacarpal joint. J Hand Surg Am 1999; 24: 86–91. [DOI] [PubMed] [Google Scholar]
- 19.Basford JR, Sheffield CG, Mair SD, et al. Low-energy helium neon laser treatment of thumb osteoarthritis. Arch Phys Med Rehab 1987; 68: 794–797. [PubMed] [Google Scholar]
- 20.Carreira GAC, Jones A, Natour J. Assessment of the effectiveness of a functional splint for osteoarthritis of the trapeziometacarpal joint on the dominant hand: a randomized controlled study. J Rehabil Med 2010; 42: 469–474. [DOI] [PubMed] [Google Scholar]
- 21.Boustedt C, Nordenskiold U, Nilsson LA. Effects of a hand-joint protection programme with an addition of splinting and exercise: one year follow-up. Clin Rheumatol 2009; 28: 793–799. [DOI] [PubMed] [Google Scholar]
- 22.Weiss S. Prospective analysis of splinting the first carpometacarpal joint: an objective, subjective, and radiographic assessment. J Hand Ther 2000; 13: 218–226. [DOI] [PubMed] [Google Scholar]
- 23.Frouzakis R, Herren DB, Marks M. Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis. J Hand Surg Am 2015; 40: 483–490. [DOI] [PubMed] [Google Scholar]
- 24.Marks M, Schoones JW, Kolling C, et al. Outcome measures and their measurement properties for trapeziometacarpal osteoarthritis: a systematic literature review. J Hand Surg Eur 2013; 38: 822–38. [DOI] [PubMed] [Google Scholar]
- 25.Borenstein M, Hedges LV, Higgins JPT, et al. Introduction to meta-analysis, Hoboken: Wiley & Sons, 2009, pp. 357–364. [Google Scholar]
- 26.Oesch P, Hilfiker R, Keller S et al. Assessments in der rehabilitation. Band 2: Bewegungsapparat. Bern: Verlag Hans Huber, 2011. pp.305–310.
- 27.Bani MA, Arazpour M, Kashani RV, et al. Comparison of custom-made and prefabricated neoprene splinting in patients with the first carpometacarpal joint osteoarthritis. Disabil Rehabil Assist Technol 2012; 8(3): 232–237. [DOI] [PubMed]
- 28.Bani MA, Arazpour M, Kashani RV, et al. The effect of custom-made splints in patients with the first carpometacarpal joint osteoarthritis. Prosthet Orthot Int 2012; 37(2): 139–144. [DOI] [PubMed]
- 29.Bani AA. A custom-made neoprene thumb carpometacarpal orthosis with thermoplastic stabilization: An orthosis that promotes function and improvement in patients with the first carpometacarpal joint osteoarthritis. Prosthet Orthot Int 2014; 38(1): 79–82. [DOI] [PubMed]
- 30.Becker SJ, Bot AG, Curley SE, et al. A prospective randomized comparison of neoprene vs thermoplast hand-based thumb spica splinting for trapeziometacarpal arthrosis. Osteoarthr Cartil 2013; 21(5): 668–75. [DOI] [PubMed]
- 31.Buurke JH, Grady JH, de Vries J, et al. Usability of thenar eminence orthoses: report of a comparative study. Clin Rehabil 1999; 13(4): 288–294. [DOI] [PubMed]
- 32.Sillem CLB, Miller WC, Li LC, et al. Comparison of two carpometacarpal stabilizing splints for individuals with thumb osteoarthritis. J Hand Ther 2011; 24(3): 216–225. [DOI] [PubMed]
- 33.Weiss S, Lastayo P, Mills A, et al. Splinting the degenerative basal joint: custom-made or prefabricated neoprene? J Hand Ther 2004; v17(4): v401–v406. [PubMed]
- 34.McKee P, Rivard A. Orthoses as enablers of occupation: client-centred splinting for better outcomes. Can J Occup Ther 2005; 71(5): v306–v314. [DOI] [PubMed]
- 35.Rannou F, Dimet J, Boutron I, et al. Splint for base-of-thumb osteoarthritis: a randomized trial. Ann Intern Med 2009; 150(10): 661–669. [DOI] [PubMed]
- 36.Hermann M, Nilsen T, Eriksen CS, et al. Effects of a soft prefabricated thumb orthosis in carpometacarpal osteoarthritis. Scand J Occup Ther 2013; 21(1): 31–39. [DOI] [PubMed]
- 37.Wajon A and Ada L. No difference between two splint and exercise regimens for people with osteoarthritis of the thumb: a randomised controlled trial. Aust J Physiother 2005; 51(4): 245–249. [DOI] [PubMed]
- 38.Merrit M. Comparison of hand therapy to placebo in the treatment of thumb carpometacarpal osteoarthritis. PhD Thesis, Texas Women's University, Denton, Texas, 2012.
- 39.Villafañe JH, Cleland J and Fernández-de-Las-Peñas C. The effectiveness of a manual therapy and exercise protocol in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther 2013; 43(4): 204–213. [DOI] [PubMed]
- 40.Davenport BJ, Jansen V and Yeandle N. Pilot randomized controlled trial comparing specific dynamic stability exercises with general exercises for thumb carpometacarpal joint osteoarthritis. Hand Therapy 2012; 17: 60–67.
- 41.Dickens W. A single-blind controlled randomized controlled trial to evaluate the effect of acupuncture of trapeziometacarpal osteoarthritis. Complement Med Res 1989; 3(2): 5--8.
- 42.Randall C, Randall H, Dobbs F, et al. Randomized controlled trial of nettle sting for treatment of base-of-thumb pain. J R Soc Med 2000; 93(6): 305–309. [DOI] [PMC free article] [PubMed]
- 43.Villafane J, Silva B and Fernandez-Carnero J. Short-term effects of neurodynamic mobilization in 15 patients with secondary thumb carpometacarpal osteoarthritis. J Manip Physiol Ther 2011; 34(7): 449–456. [DOI] [PubMed]
- 44.Villafañe J, Silva G, Bishop M, et al. Radial nerve mobilization decreases pain sensitivity and improves motor performance in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial. Arch Physi Med Rehabil 2012; 93(3): 396–403. [DOI] [PubMed]
- 45.Villafañe J , Silva G, Diaz S, et al. Hypoalgesic and motor effects of kaltenborn mobilization on elderly patients with secondary thumb carpometacarpal osteoarthritis: a randomized controlled trial. J Manip Physiol Ther 2011; 34(8): 547–556. [DOI] [PubMed]
- 46.Villafañe J, Silva G, Fernandez-Carnero J. Effect of thumb joint mobilization on pressure pain threshold in elderly patients with thumb carpometacarpal osteoarthritis. J Manip Physiol Ther 2012; 35(2): 110–120. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.