Abstract
Since 2000, the Children with Special Health Care Needs (CSHCN) Screener (CS) has been widely used nationally, by states, and locally as a standardized and brief survey-based method to identify populations of children who experience chronic physical, mental, behavioral, or other conditions and who also require types and amounts of health and related services beyond those routinely used by children. Common questions about the CS include those related to its development and uses; its conceptual framework and potential for under- or over-identification; its ability to stratify CSHCN by complexity of service needs and daily life impacts; and its potential application in clinical settings and comparisons with other identification approaches. This review recaps the development, design, and findings from the use of the CS and synthesizes findings from studies conducted over the past 13 years as well as updated findings on the CS to briefly address the 12 most common questions asked about this tool through technical assistance provided regarding the CS since 2001. Across a range of analyses, the CS consistently identifies a subset of children with chronic conditions who need or use more than a routine type or amount of medical- and health-related services and who share common needs for health care, including care coordination, access to specialized and community-based services, and enhanced family engagement. Scoring algorithms exist to stratify CSHCN by complexity of needs and higher costs of care. Combining CS data with clinical diagnostic code algorithms may enhance capacity to further identify meaningful subgroups. Clinical application is most suited for identifying and characterizing populations of patients and assessing quality and system improvement impacts for children with a broad range of chronic conditions. Other clinical applications require further implementation research. Use of the CS in clinical settings is limited because integration of standardized patient-reported health information is not yet common practice in most settings or in electronic health records. The CS continues to demonstrate validity as a non-condition-specific, population-based tool that addresses many of the limits of condition or diagnosis checklists, including the relatively low prevalence of many individual conditions and substantial within-diagnosis variations and across-diagnoses similarities in health service needs, functioning, and quality of care.
Keywords: children with special health care needs, children with chronic conditions, complex CSHCN, National Survey of Children With Special Health Care Needs, National Survey of Children’s Health, Medical Expenditures Panel Survey
Background
Since 1998, legislative mandates have required the Maternal and Child Health Bureau (MCHB) to monitor system performance for US children with special health care needs (CSHCN), a process that requires population-based identification of CSHCN. For this purpose, CSHCN are broadly defined as those who “have or who are at increased risk of having a physical, mental, emotional or other type of health condition requiring a type or amount of health and related services beyond that required by children generally.”1 More recent national legislation requires health systems and/or providers to identify CSHCN to assess accessibility and quality of health care services for this growing population of children.2–8 Specifically, the Children’s Health Insurance Plan Reauthorization Act (CHIPRA) and the Patient Protection and Affordable Care Act (ACA) require quality measures to be reported separately for CSHCN.6–8 ACA-related initiatives to incentivize the development of primary care medical homes include similar requirements, and the Centers for Medicare and Medicaid Services (CMS) has issued a set of administrative data-based diagnostic codes to assist in doing so.4,9
The CSHCN Screener (CS) has been widely used as a method to identify CSHCN based primarily on the MCHB definition. This 5-item, parent-reported screening instrument requires an average of 1 minute for parents to complete and identifies 15% to 20% of US children, depending on their health and service needs and the presence of any kind of chronic condition.10 Nationally, data on the CS for over 1.5 million children have been collected through the 2001, 2005–2006, and 2009–2010 National Survey of CSHCN (NS-CSHCN; n = 1,106,974); the 2003, 2007, and 2011–2012 National Survey of Children’s Health (NSCH; n = 289,672); and the Medical Expenditure Panel Survey (MEPS) since the year 2000 (n = 113,729).
In response to the persistent and growing need to identify CSHCN for population health and quality measurement and improvement purposes, we recap the development, design features, and population prevalence findings using the CS since 2000, and we briefly address commonly posed questions about its conceptual framework, potential for under- and over-identification, ability to stratify children once identified, and application in clinical settings and in combination with administrative data approaches.
Review of CS Development, Design, and Prevalence Findings
The CS was designed during 1998–2000 through a national collaborative led by the Child and Adolescent Health Measurement Initiative (CAHMI) and supported by the David and Lucile Packard Foundation and Agency for Healthcare Research and Quality.11–13 It was initially designed to identify a robust and sufficiently large group of children for measuring quality of care for CSHCN across health plans in the Consumer Assessment of Health Plans Survey for Children with Chronic Condition (CAHPS-CCC). Subsequently, it was validated as a population-based tool for estimating the prevalence of CSHCN and for comparing needs and health care system performance across states and population subgroups in the NS-CSHCN.13
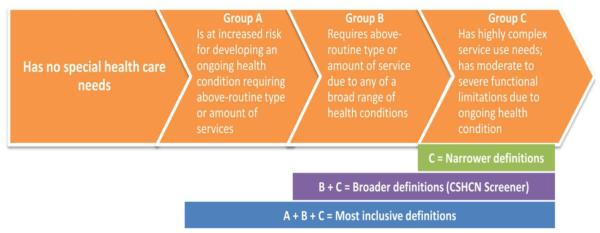
CSHCN can be characterized along a continuum according to the types of chronic health conditions experienced and the frequency, consistency, scope, and intensity of services required (Fig. 1). With a focus on quality measurement and system performance measurement, the national collaboration assembled to develop the CS agreed to not include children at risk for special health care needs (SHCN) but instead to focus on identifying children with existing SHCN who are most vulnerable to weakness in quality and system performance. They also agreed to target identification of a broad range of children, requiring only that the child experience any type of ongoing health condition that results in a need for an above-routine type or amount of health and related services.
Figure 1.
Continuum for defining a consequences-based, non-categorical, non-condition-specific MCHB definition of CSHCN.
After careful review of a range of conceptual models, including administrative data–based methods, the conceptual and empirical foundation from the Questionnaire to Identify Children With Chronic Conditions (QuICCC)14 and the Questionnaire for Identifying Children with Chronic Conditions—Revised (QuICCC-R)15 was selected as the framework for the CS. Key features include: 1) a non-categorical definition that is not dependent upon diagnostic lists; 2) the use of service need and/or functional consequences of ongoing conditions as the method of identifying children; and 3) confirmation of eligibility based on the presence of any type of chronic condition and duration of at least 12 months.12–20 Exhibit A and Exhibit B (available online at http://www. academicpedsjnl.net) provide a synthesis of the specific questions and key design parameters considered during the 2-year collaborative development of the CSHCN Screener (CS) survey-based tool.
As a result of response rate concerns and costs of measurement for the CAHPS and NS-CSHCN, brevity was essential for the survey-based CS. Starting with over 39 candidate items largely adapted from the QuICCC,17 and based on iteratively evaluated results of qualitative and quantitative analyses, 5 parent-reported stem items were selected for inclusion in the CS, each including 1 or 2 follow-up items to discern CSHCN classification. The 5 stem items assess: 1) need or use of prescription medication; 2) above-routine use of medical, mental health, or educational services compared to other children of the same age; 3) activity limitations in day-to-day life compared to similar age children; 4) need or use of specialized therapies; and 5) need or use of treatment or counseling for an emotional, behavioral, or developmental condition. As in the QuICCC, follow-up items are used to confirm that affirmative responses to each stem item are due to a physical, mental, behavioral, or other health condition that has or is expected to last at least 12 months. Although CSHCN experience many more consequences than those directly evaluated in the CS, the 5 stem items in the CS were selected to capture the health service and health-related consequences experienced by virtually all children identified as CSHCN using the longer set of survey items.
Recent data from the 2011–2012 NSCH show that 30.1% of US children have parents who gave an affirmative response to 1 or more of the 5 consequences-based CS stem items, and 59.2% to 83.4% of children (across items) have parents who indicated that these consequences were “due to a condition.” Even though repeated testing shows that parents largely interpret the word condition to indicate an ongoing health problem, a final follow-up question asks whether the child’s condition has lasted or is expected to last at least 12 months to ensure that the condition is a chronic condition. Most of those with affirmative responses to the first “due to a condition” follow-up item met the duration-of-condition criterion (90.4% to 97.3% across the 5 items).
US prevalence estimates for CSHCN using the CS range from 12.8% in the 2001 NS-CSHCN to 19.8% in the 2011–2012 NSCH. The upward trend in CSHCN prevalence since the first NS-CSHCN was conducted in 2001 is consistent with other national survey data showing rising prevalence of childhood chronic conditions and limitation of activity due to chronic conditions.21 Prevalence estimates of CSHCN using the CS in population-based surveys in other countries are similar.22,23
However, CSHCN prevalence estimates may differ between surveys depending on how the CS is administered to parents with more than 1 child.10 Similar to findings for questions that identify persons with disabilities or health problems,24 CSHCN prevalence is generally lower when surveys use a family-level CS (“Do any of your children need or use . ?” and if yes, “Who?”) rather than a sequential person-level CS (“Does Amy need or use . ?” followed by “Does Bob need or use. ?”).10 Despite these variations, once identified using the CS, demographic and health-related characteristics of CSHCN and distributions identified across qualifying criteria are consistent.10
Common Questions Related To the CS
Common questions regarding the CS were identified through an assessment of published studies using the CS and through logs kept by CAHMI, which provided technical assistance to CS users since 2000. In addition, common questions asked of statistical experts at the National Center for Health Statistics were identified. Exhibit B lists 12 common questions addressed in this review. Brief answers to each are provided here for each question and largely draw on findings from previously published studies and official in-depth government-sponsored reports used in the evaluation of the CS for use in the CAHPS and national surveys. This includes findings from the non-publicly released 2005–2006 NS-CSHCN referent sample of children without SHCN. These data permitted a robust assessment of the potential under- or over-identification of CSHCN using the CS. Using more recent data from the 2009–2010 NS-CSHCN, we updated results of previously published analyses specifying algorithms to identify subgroups of CSHCN according to the complexity of their health and health service needs.
In addition, we report on findings from data collected during the initial (1998–2000) field testing of the CS. These findings were widely reviewed and included in official documentation provided by the CAHMI to the Agency for Healthcare Research Quality and the National Committee for Quality Assurance in 1999, when the latter endorsed the use of the CS as part of a 2-stage, mixed-data method specified by the CAHMI to identify CSHCN in the CAHPS-CCC.11,25–27
Finally, we report results from analyses conducted to inform identification of CSHCN in pediatric practices and hospital settings. Specifically, we compare health care utilization and expenditures for CSHCN identified by the CS to those identified using a diagnostic code list set forth for use by providers participating in the Affordable Care Act’s Patient Centered Primary Care Home Program (Section 2703).9 The 2008 MEPS Full Year Consolidated Data File was used for these analyses, and a standard 2-part model28 was used to accommodate the skewed distribution of health care expenditures, adjusting for age, sex, race/ethnicity, and household income. Although youth and adult self-reported versions of the screener have been developed and used in national samples, here we only report findings from the parent-reported version of the CS.29,30
Questions regarding the conceptual logic of the CS
What is the rationale for using a non-condition-specific identification method anchored to health-related consequences?
Identification of children on the basis of the consequences they experience from a health problem was first promulgated by Pless and Pinkerton31 and rested on the observations that: 1) many service need and functional, psychological, and social consequences of childhood health problems are common across different diseases; 2) there is great variation in service needs and functioning (consequences) within diagnostic groups;16,32–34 and 3) eliciting valid information about the presence of specific chronic conditions by either parent report or medical records is impractical and highly prone to errors.11–13,35–37 Thus, use of a non-condition-specific method for the CS was selected in recognition of these factors and inherent limits of diagnostic-based methods, including limitations in the standardization, accessibility, and validity of clinical administrative data, especially where CSHCN rely on services from multiple systems whose data systems are not integrated. Additional rationales were the relatively low prevalence of many individual conditions and the need for a sufficiently robust CSHCN prevalence to support quality measurement with reliable denominators at the health plan or clinical level.16,38 Using the CS consequences-based approach, those identified are more homogenous in health care needs and health-related consequences14,33,39 and impacts than are children identified based on the condition check list alone.19,40,41
Why aren’t all children identified as CSHCN at one point in time identified as CSHCN at a second, later point in time?
Only 87.1% of children identified as CSHCN in the 2003–2004 MEPS were identified in the 2005–2006 MEPS.42 Other diagnostic and physical examination methods display similar test–retest reliability (or lack thereof) over time.21,43 Children move in and out of classification schemes as a result of changes in their diagnosis, treatment plan, symptoms, or development. A small amount of this movement may be the result of measurement error (including, for example, a change in which parent completed the screener). It is common for health status and utilization for a child with chronic health problems to vary over time.44
Why is there a separate item on treatment or counseling for an ongoing emotional, developmental, or behavioral condition?
The emotional, developmental, and behavioral (EDB) conditions and treatment criterion are included to optimize the possibility of capturing children with EDB conditions and who have needs for nonmedical, health-related services. Cognitive testing of candidate CS items revealed that some parents of children with EDB conditions did not consider them to be health conditions, and their children would be under-identified without a separate item.11,25–27 For example, on the basis of data from the 2009–2010 NS-CSHCN, children with 1 or more ongoing EDB condition that requires counseling or treatment represent 31.8% of the CSHCN population, with half qualifying only on this criterion. This criterion also enables stratification of CSHCN by EDB conditions. CSHCN with EDB conditions often experience greater unmet needs, child and family impacts, and deficits of quality of care than other CSHCN.21,45
Questions related to potential under- and over-identification
Why aren’t all children reported as having chronic conditions or functional difficulties counted as CSHCN?
By design, not all children whose parents separately report presence of a chronic condition or functional difficulties are identified as CSHCN using the CS. This is due to the wide range of needs and complexity within diagnostic groups16,32–34 as well as inherent errors in diagnosis and reporting, whether by parents or clinicians.11–13,35–37 Analysis of the 2005–2006 NS-CSHCN referent sample shows that if all children whose parents reported that they had been diagnosed with 1 or more of 20 listed chronic conditions and/or experience 1 or more of 14 listed functional difficulties were counted as CSHCN, the prevalence would have been 34.4% compared to 13.9% using the CS. Similarly, in the 2011–2012 NSCH, 23.6% of all US children had parents who reported 1 or more of 18 listed chronic conditions, yet only 65.8% qualified as CSHCN using the CS. Analysis of the 2011–2012 NSCH and NS-CSHCN 2005–2006 referent sample data sets document that children not meeting CS criteria but who have parents reporting the presence of chronic conditions also have significantly and substantially lower rates of 1) services use, 2) unmet need, 3) inadequate insurance, 4) developmental and behavioral concerns, 5) above-routine amount of missed school, and 6) poor school engagement. As expected, observed rates are higher than those of non-CSHCN whose parents do not report conditions, but they are nonetheless far lower than CSHCN, suggesting that this may be a group of children to classify as being at risk for CSHCN.46
Similar to reports of conditions, almost 1 (19.2%) in 5 children without SHCN had 1 or more of the 14 functional difficulties asked about in the 2005–2006 NS-CSHCN.34,46–48 However, for these children, their functional difficulties did not result in a commensurate report of service needs or use or ongoing limitations in day-to-day activities due to a health condition. This is not unexpected, as functional difficulties may also be minor or due to transient acute conditions or injuries common in childhood.46
Why is the prevalence of CSHCN lower for Hispanic children?
A frequent question about the CS is whether the lower prevalence estimates observed for Hispanic children are the result of differential access to care, differences in cultural understanding, or translational issues. National- and state-level CSHCN prevalence for Hispanic children from Spanish-language households has been consistently estimated to be less than half that of Hispanic children from English-language households.10,49,50 The interview language remains a strong predictor of lower prevalence estimates, even when statistically controlling for group differences in age, sex, race/ethnicity, and household poverty level.10 The Spanish-language translation of the CS has undergone multiple rounds of cognitive testing, confirming that parents correctly understood CS concepts and answered translated questions appropriately, and translations did not require revisions.51 To date, studies have not demonstrated that access to care or parental knowledge of their child’s health influences identification of CSHCN overall. Lower prevalence for Hispanic children living in Spanish-speaking homes is consistent with other studies on the health of Hispanic children51–53 and it is therefore presumed to not be due to unique characteristics of the CS per se. Rather, it appears that lower rates for children living in Spanish-speaking homes reflects other issues related to cultural views on health and cultural norms related to health-seeking behavior or reporting health problems and concerns.
Do problems with health care access lead to under-identification of CSHCN?
Ensuring the CS does not select among CSHCN with better access to care was a central goal in its development and testing. When access to care is limited, a child may not be identified as having a health condition and/or may not receive needed services. To attenuate the risk of not identifying a child as CSHCN due to access barriers, the CS was designed to identify children with chronic conditions with an elevated need for or use of services. Nonetheless, some CSHCN may go undetected because their parents do not perceive a need or health condition that may in fact exist and consequently do not access the health care system.
Analyses consistently show that children living in poverty are more likely than other children to be identified as CSHCN (adjusted odds ratio ≈1.4–1.5).10 Because lower household income is generally associated with problems accessing health care regardless of level of need, we believe that health care access is not likely to have a strong influence on the identification of CSHCN. Similarly, children experiencing delayed or foregone health care are also more likely to be identified as CSHCN (adjusted odds ratio = 2.86). We recommend additional evaluations to ensure that the CS optimizes the identification of children meeting criteria as CSHCN. Of course, in the absence of a gold standard set of criteria, such evaluations must be done against a clear definition of CSHCN and set of qualifying criteria.
Allergies and asthma are the most common conditions reported among CSHCN. Are children with only these conditions really CSHCN?
On the basis of national data, more than half of CSHCN have parent-reported environmental or food allergies, and about one third have asthma.49,54,55 Some data users question whether these children should be considered CSHCN, presumably due to assumptions that they have inherently lower health and health service need and impacts than children with other types of chronic conditions. Because it is the most commonly named condition, some even erroneously conclude that most CSHCN are children with allergies and fail to account for the fact that nearly 90% of these children have co-occurring conditions with related health needs and impacts.47
It is true that children who qualified on the CS and had only asthma (7% of CSHCN) or only allergies (11% of CSHCN) or both asthma and allergies (16% of CSHCN) were less likely than other CSHCN to experience health-related consequences, such as functional difficulties and impacts on the family. However, they were significantly more likely to experience these consequences when compared to non-CSHCN (Table 1). It is also important to note that some children in this “asthma and/or allergies only” group experience much higher levels of need and impact on daily functioning than children with conditions commonly considered more serious, such as cerebral palsy, cystic fibrosis, and epilepsy. For instance, 54.2% of CSHCN with allergies experience difficulties with 1 or more daily activities compared to 47.6% of CSHCN with cystic fibrosis. Similarly, 93.8% of CSHCN with asthma experience difficulties with 1 or more bodily functions compared to 83.2% of CSHCN with cerebral palsy.34
Table 1.
Comparison of Selected Measures of Health Care Use, and Health and Family Impact for Children With and Without Special Health Care Needs
| Characteristic | Non- CSHCN |
CSHCN* | CSHCN with Only Asthma and/or Allergies† |
CSHCN with Conditions Other than Allergies and/or Asthma† |
CSHCN with None of the 16 Conditions Included in Survey |
|---|---|---|---|---|---|
| Percentage of all CSHCN | NA | 100% | 34.7% | 56.3% | 8.9% |
|
| |||||
| Average # of doctor visits | 2.3 | 5.1 | 4.5 | 5.7 | 4.5 |
|
| |||||
| Percent with 9+ visits | 3.1% | 21.6% | 14.3% | 26.9% | 17.0% |
|
| |||||
| Percent with 2+ emergency room visits |
4.8% | 19.3% | 16.2% | 22.2% | 13.3% |
|
| |||||
| Average # of specialist/special services needed (of 10 included in survey‡) |
0.3 | 1.5 | 1.0 | 1.8 | 1.3 |
|
| |||||
| Average # of functional difficulties reported (of 14 included in survey§) |
0.3 | 2.5 | 1.2 | 3.6 | 1.2 |
|
| |||||
| Percent with 2+ functional difficulties (of 14 included in survey) |
6.7% | 54.2% | 22.2% | 77.9% | 29.4% |
|
| |||||
| Average # of current conditions reported (of 16 included in survey) |
0.3 | 1.9 | 1.5 | 2.5 | NA |
|
| |||||
| Percent with 2+ current conditions reported (among 16 included in the survey) |
4.3% | 57.2% | NA | 73.7% | NA |
|
| |||||
| Percent whose parents cut back or stopped working due to child’s health needs |
3.9% | 23.8% | 12.7% | 31.9% | 15.8% |
CSHCN indicates children with special health care needs.
Data source: National Survey of Children with Special Health Care Needs, 2005–2006, including both the public use interview file and referent data file. All health care visit and need measures were assessed for the past 12 months.
CSHCN comprised 14.8% all children aged 0 to 17 years.
Among the 16 conditions asked about,7%had asthma only; 11% allergies only; 16% both; 75.8% of these children qualified on prescription medication CSHCN Screener criterion only; 15% qualified on the activity limitations criterion.
Including specialist care; mental health care; occupational therapy, physical therapy, or speech therapy; substance abuse treatment; home health care; hearing aids/hearing care; mobility aids; communication aids; medical supplies; durable medical equipment.
Functional difficulties included: learning, understanding or paying attention; breathing or other respiratory problems, feeling anxious or depressed, behavior problems, speaking, communicating, or being understood, making and keeping friends, repeated or chronic physical pain, including headaches, taking care of self, such as eating, dressing, bathing, coordination or moving around, swallowing, digesting food, or metabolism, using his/her hands, seeing even when wearing glasses or contact lenses, hearing even when using a hearing aid/other device, blood circulation.
Many CSHCN qualify only on the prescription medications need or use criterion. Are these really CSHCN?
Nearly 40% of CSHCN qualify only on the prescription medication need or use CS criterion. A frequent question is whether CSHCN meeting only the prescription medication criterion should be categorized as CSHCN. As shown in Table 2, using data from the 2009–2010 NS-CSHCN, those who qualify only on the prescription medication need or use criterion do appear to have less complex needs compared to other CSHCN. However, this is not uniformly the case. More importantly, these children have much higher rates of health services utilization and greater numbers of health conditions and functional difficulties compared to non-CSHCN. The MEPS data show that CSHCN qualifying only on the prescription medication need or use criterion had medical care expenditures that were 3 times higher than for non-CSHCN ($2,705 vs $856) (Table 2).4 Prior studies based on a comparable item included in the QuICCC demonstrate evidence that many children who receive medication on a prolonged basis for a chronic condition would in fact have consequences in terms of their daily lives if they failed to take these medications.14
Table 2.
Stratification Options Using the CSHCN Screener: Variation in Total Medical Expenditures and Examples of Potential Relevance of Stratification Categories
| CSHCN Subgroup | CSHCN Screener Scoring Criteria |
Adjusted Average Medical Expenditure |
Potential Relevance of Each Subgroup |
|---|---|---|---|
| CSHCN with less complex needs |
Meets only criterion 1 on need or use of medication |
$2,705 | In primary care settings |
|
| |||
| CSHCN with more complex needs |
Meets 2 or more of any criteria, indicating multiple types of needs |
$4,003 | For efforts seeking to coordinate or integrate services between primary care and specialist care |
|
| |||
| CSHCN with limitation in daily activities due to ongoing health conditions |
Meets activity limitations criterion in addition to any other criterion (virtually all meet other criteria) |
$4,866 | For efforts related to transition to adulthood or improving coordination of care with non-medical, health-related community- based services |
|
| |||
| CSHCN who met 3 or more criteria |
CSHCN who meet 3 or more criteria |
$6,755 | For efforts focused on reducing medical expenditures and overall system integration efforts, including initiatives to reduce hospitalization |
|
| |||
| CSHCN with more complex EDB |
CSHCN meeting EDB criterion (question 5) and at least 1 other criterion |
$5,813 | For efforts to reduce medical expenditures and integrating primary care and behavioral/mental health care services |
CSHCN indicates children with special health care needs; EDB, emotional, developmental, and behavioral conditions.
Data source: 2008 Medical Expenditure Panel Survey (average expenditures adjusted using 2-part model to account for outliers).
Why does the CS include an item on activity limitations when such limitations are not specifically mentioned in the MCHB definition?
The CS activity limitation criterion was included in order to improve the probability of identifying CSHCN whose conditions have a large impact on their daily functioning but whose need for health services may be more intermittent or unpredictable.56 Although over 92% of children qualifying on this criterion qualify on other CS criteria as well, those who qualify on this criterion alone (1.9% of identified CSHCN, or approximately 273,000 children, based on 2011–2012 NSCH data) disproportionately include children with vision problems (eg, blindness), intellectual disabilities, cerebral palsy, spina bifida, or some combination of these. It is important to identify these children as CSHCN when using the CS to support systems of care for CSHCN.
Dropping the activity limitations CS criterion would only reduce the national prevalence of CSHCN by 0.4 percentage points (from 19.8% to 19.4% using the 2011–2012 NSCH). Despite this, its inclusion is maintained because of the unique children identified by this criterion alone as well as because of the power of this single item to provide a useful stratifying variable for CSHCN. Repeated testing documents that although nearly all CSHCN experience 1 or more of the 14 functional difficulties on the NS-CSHCN, reports of having a limitation in day-to-day activities due to a chronic condition are much rarer and differentiate CSHCN with greater needs and impacts due to their condition (Table 3).12,13
Table 3.
Variations in Health Service Needs, Expenditures, and Functioning Across CSHCN Screener Subgroups
| All CSHCN in US |
CSHCN with Less Complex Needs |
CSHCN with More Complex Needs |
CSHCN With Limitation in Daily Activities Due to Ongoing Health Conditions |
CSHCN who Met 3 or More Criteria |
CSHCN with More Complex EDB |
|
|---|---|---|---|---|---|---|
| Proportion of CSHCN in each subgroup | 100.0% | 39.3% | 60.7% | 23.5% | 27.9% | 26.8% |
|
| ||||||
| Estimated number of children (in thousands) | 11,102 | 4,358 | 6,743 | 2,607 | 3,093 | 2,973 |
|
| ||||||
| Child utilizes multiple health care services | 75.6% | 56.0% | 88.4% | 91.5% | 95.7% | 94.0% |
|
| ||||||
| Need and/or use of specialist care | 47.5% | 36.4% | 54.6% | 63.3% | 63.0% | 55.2% |
|
| ||||||
| Four or more functional difficulties noted | 45.6% | 17.7% | 63.6% | 78.5% | 82.2% | 81.9% |
|
| ||||||
| Daily activities consistently affected often or a great deal |
27.1% | 5.8% | 40.9% | 69.1% | 60.3% | 53.0% |
|
| ||||||
| Missed 11+ school days in past year | 15.5% | 8.4% | 20.1% | 27.0% | 25.7% | 21.1% |
|
| ||||||
| 2 or more ED visits in past year | 21.6% | 16.2% | 25.1% | 31.0% | 28.5% | 24.5% |
|
| ||||||
| Average adjusted total health care expenditures per child |
$3,392 | $2,705 | $4,003 | $4,866 | $6,755 | $5,813 |
|
| ||||||
| 10 or more office-based visits in past year | 17.1% | 8.6% | 23.2% | 23.6% | 34.9% | 32.4% |
|
| ||||||
| Families paid more than $1,000 in out-of-pocket medical expenses |
22.1% | 17.1% | 25.4% | 28.3% | 30.5% | 28.2% |
|
| ||||||
| CSHCN whose conditions cause financial problems for the family |
21.6% | 9.7% | 29.2% | 40.0% | 39.8% | 35.7% |
|
| ||||||
| Families who spend 11+ hours providing/coordinating child's health care |
13.1% | 5.5% | 18.1% | 29.5% | 26.7% | 21.7% |
|
| ||||||
| CSHCN whose conditions cause family members to cut back/stop working |
25.0% | 9.4% | 35.1% | 49.8% | 48.3% | 42.3% |
|
| ||||||
| Family member(s) avoided changing jobs in order to maintain health insurance for child |
17.7% | 11.3% | 21.8% | 28.0% | 26.7% | 24.2% |
CSHCN indicates children with special health care needs; EDB, emotional, developmental, and behavioral conditions; and ED, emergency department.
Data source: National Survey of Children with Special Health Care Needs, 2009–2010; 2008 Medical Expenditure Panel Survey.
It should be noted that the activity limitations CS qualifying criterion is not intended to serve as a disability screener or as a substitute for a more complete assessment of functional difficulties CSHCN experience. The question itself is cognitively complex, asking parents to consider not only their own children’s capabilities but also those of other children of the same age. Questions about specific functional domains are more specific and easier to answer, but the desired brevity of the CS precluded the addition of such questions. Nevertheless, validity analyses continue to demonstrate that this item performs as intended for purposes of identifying CSHCN.
Question about stratification
Can data for children identified by the CS be further stratified to provide information about complexity according to the type, severity, impact of health conditions, or type or intensity of health care needs?
Children identified using the CS vary in the complexity of their SHCN. Since first used in the CAHPS-CCC and the 2001 NS-CSHCN, scoring algorithms based on the number and type of CS criteria have been used to differentiate subgroups of CSHCN according to impact on the family, medical expenditures, and complexity of child’s condition.57 Although options for identifying more or less complex CSHCN using the CS vary according to the user’s purpose, the methodologies listed in Table 2 have been shown to discriminate subgroups according to costs of care. These groups also discriminate among CSHCN according to complexity of service needs, functional impact of conditions, and costs of care. Table 3 illustrates these and additional differences across these complexity subgroups.
Questions of application across settings and in comparison with other methods
Can the CS be used to identify children for clinical purposes? If so, can a health care professional complete the CS for patients?
The CS was initially designed to identify, characterize, and monitor the health and health care quality for populations of children in health plans and national and state geographic contexts. It has since been used in pediatric practices and hospitals to identify populations of patients for a variety of purposes.56,58–66 Because many providers may not be aware of all services a child receives outside of their clinic or of the child’s day-to-day functioning, the CS may be valuable in identifying populations of CSHCN within a practice’s panel of patients, some of whom the practice would not otherwise consider to be CSHCN. Conversely, because the CS selects a subset of children with conditions who experience service use and other consequences, we also expect some children clinicians consider to be CSHCN on the basis of diagnosis alone would not be identified. We do not believe there is sufficient evidence to recommend that providers/clinical staff complete the CS on behalf of parents because they may not be aware of all the services a child receives or how their conditions impact their daily life.17 More research is required to determine the value and methods for using the CS in clinical settings for purposes other than identifying populations of CSHCN for quality measurement or improvement or to refer to children programs specific to CSHCN.
How does use of the CS compare to administrative methods for identifying CSHCN?
Field test findings conducted during CS development included comparison of classifications by the CS with classifications using a diagnostic list set forth by the then active Research Consortium on Children with Chronic Conditions (RCCCC)67 as well as the more complex Clinical Risk Groups (CRG) methodology, which is based on administrative records.68 Half of children (52%) identified on the RCCCC-derived diagnostic algorithm met CS criteria. Similar results have been reported comparing the CS to algorithms that are based on data about conditions and service use from the National Health Interview Survey.69 Comparisons consistently show that children identified by the CS have greater utilization of health services compared to children identified by these other methods alone.
A 90% agreement at the child level (identified or not identified) was observed between the CS classifications and the CRG algorithm. Despite this agreement, the CS identified 5% to 10% more children as CSHCN across the health plans evaluated in the study than the CRG method did,70 indicating that nearly all identified by the CRG method are identified by the CS, but the reverse is not true. Rather, only 72.7% of children who met the CS were classified as CSHCN using the CRG administrative data–based methodology.12,70 As mentioned earlier, lack of a diagnosis in administrative records for children identified as CSHCN by the CS could be due to a child receiving diagnoses or services in settings other than those in the database, errors in coding, or inaccurate or missed diagnoses. Children can also have SHCN due to elevated service needs for an ongoing condition that is either complex or not yet diagnosed. The latter occurs when diagnostic criteria are less certain or valid, which is one reason for the disproportionate representation of younger children among those identified by the CS who do not have a medical records-based diagnosis.
Comparison of the CS and CRG showed that if the CRG methodology is used alone, at a population level, children with chronic conditions and above-routine needs would not be identified.12,70 To illustrate, children identified by the CS but not the CRG were substantially more likely to have parents who reported a need for coordination of care with school or day care than those identified by the CRG algorithm only. These CS-only children were also more likely to need care from multiple types of providers as well as specialized services (eg, medical equipment, special therapy, mental health services); 41.2% needed specialized services (based on parent report) compared to 11.3% of those identified by the CRG method alone.70
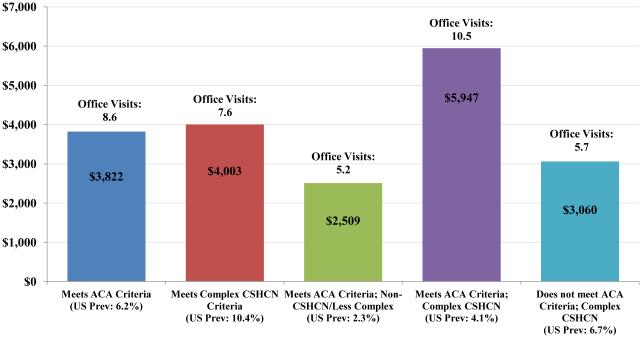
Similar to the CRG method, an 84% agreement in classifying individual children was found between the CS and classifications based on the CMS/ACA code list released in 2012 for use by Primary Care Medical Home demonstration efforts.4,9 Also similarly, the CS identified substantially more children (17.8% identified by the CS vs 6.2% identified using the short CMS/ACA code list). The lower prevalence rate from the CMS/ACA list is likely to yield samples of children in individual primary care practices that may be too small to allow quality-of-care measures to be compared across practices. Further, the additional children identified using the more broad-based CS have health services use and health impact profiles indicative of the presence of SHCN (Fig. 2).
Figure 2.
Prevalence of children qualifying on CS and/or ACA medical home section 2703 condition list and their average adjusted total medical expenditures and average annualized number of office visits. Data source: 2008 MEPS Full Year Consolidated Data File. A standard 2-part model was used to accommodate the skewed distribution of health care expenditures, adjusting for age, sex, race/ethnicity, and household income.
Concluding Comments
To effectively inform and guide health care services, policies and programs, methods of identifying CSHCN must be 1) practical and sustainable for the settings in which they will be used, 2) standardized across children and environments, and 3) result in identifying children whose characteristics are understood and sufficiently homogenous to guide decision making. Specifying an identification method requires addressing a wide range of conceptual and methodological issues. Many of these stem from the inherent lack of a gold standard for defining CSHCN, and the highly context-dependent nature of defining and identifying CSHCN in a way that addresses the various purposes for which identification is required (eg, quality measurement, program planning, quality improvement, program enrollment).
Although designed and tested before the year 2000, the purposes and key issues considered in the design of the CS remain relevant to today’s priorities for identifying CSHCN at the population, health system, practice, and individual levels. In addition to its relevance to quality measurement reporting requirements set forth through CHIPRA and the ACA,71 the CS also has relevance to the Meaningful Use standards for electronic health records advanced through the Health Information Technology for Economic and Clinical Health Act enacted as part of the American Recovery and Reinvestment Act.72,73 Inclusion of data from the parent-reported CS into the medical health record would enable the stratification of Meaningful Use quality indicators by CSHCN status.
The CS may also have relevance for emerging accountable or coordinated care organizations. These systems can utilize the CS to identify robust subgroups that are more homogenous in complexity and costs of care for purposes of triaging children for alternative payment, care coordination, and cross-cutting, non-diagnostic specific health and quality measurement and improvement strategies. When used at a population level, children meeting CS criteria and not administrative code–based algorithms might be ideal groups for prevention efforts, as CSHCN with current unmet needs may be included. These may be children whose health issues may escalate into costly future utilization of services.44
Here we address only a subset of common questions, design features, and findings from the use of the CS that have emerged since 2000. The highlighted issues are intended to inform consideration of the use of the CS in the new contexts for which it may now be even more relevant, as well as to advance its valid use in research, practice, and policy contexts. Although there is no gold standard in identifying CSHCN and numerous methods are appropriate depending on the purpose for identification, the CS continues to provide an efficient, well-tested, flexible, discriminating, and patient-centered method for identifying CSHCN in populations of children, and it provides numerous options for scoring and identifying relevant subgroups of CSHCN. Further research is especially required to better understand ongoing issues of identification for non-English-speaking populations and for clinical application purposes.
What’s new.
In response to renewed national focus on children with special health care needs (CSHCN), we recap the development, design features, and findings on the use of the CSHCN Screener since 2000. Current perspectives on common questions about is validity and use in research, policy, and practice are addressed.
Acknowledgments
This paper was supported through The Child and Adolescent Health Measurement Initiative and the National Data Resource Center for Child and Adolescent Health (DRC), funded by the federal Maternal and Child Health Bureau through Cooperative Agreement # 1-U59-MC06980-01. The views expressed in this report are those of the authors and do not necessarily represent those of HRSA or CDC/NCHS. The authors thank Narangerel Gombojav, PhD for her periodic data analysis assistance during the preparation of this manuscript.
Footnotes
Conflicts of Interest/Corporate Sponsors: None.
References
- 1.McPherson M, Arango P, Fox H, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137–140. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 2.Sebelius K. Report to Congress: HHS Secretary’s Efforts to Improve Children’s Health Care Quality in Medicaid and CHIP. Department of Health and Human Services; Washington, DC: 2010. Available at: https://www.medicaid.gov/medicaid-chip-program-information/by-topics/quality-of-care/downloads/RTC_childhealthimprovement.pdf; [Google Scholar]
- 3.Department of Health and Human Services. Centers for Medicare and Medicaid Services State health official letter on the children’s health care quality measures. SHO 11–001. Available at: https://downloads.cms.gov/cmsgov/archived-downloads/SMDL/downloads/SHO11001.pdf.
- 4.Public Law 111-148, Section 2703. March 23, 2010. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/pdf/PLAW-111publ148.pdf.
- 5.Agency for Healthcare Research and Quality Pediatric Quality Measures Program (PQMP) Centers of Excellence grant awards. Available at: http://www.ahrq.gov/policymakers/chipra/pubs/pqmpfact.html.
- 6.Centers for Medicare and Medicaid Services Children’s Health Insurance Program Reauthorization Act (CHIPRA) of 2009. Public Law 111–113. Available at: http://www.gpo.gov/fdsys/pkg/PLAW-111publ3/html/PLAW-111publ3.htm. Accessed January 1, 2010.
- 7.Sebelius K. Report to Congress: Approaches for Identifying, Collecting, and Evaluating Data on Health Care Disparities in Medicaid and CHIP. Department of Health and Human Services; Washington, DC: 2011. Available at: http://www.healthcare.gov/news/reports/disparities09292011a.pdf; Accessed September 2011. [Google Scholar]
- 8.Fairbrother G, Simpson L. Measuring and reporting quality of health care for children: CHIPRA and beyond. Acad Pediatr. 2011;11:S77–S84. doi: 10.1016/j.acap.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Oregon Health Authority Diagnosis codes for ACA-qualified conditions from patient-centered primary care home program. Updated March 7, 2012. [Google Scholar]
- 10.Bethell C, Read D, Blumberg S, Newacheck P. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern Child Health J. 2008;12:1–14. doi: 10.1007/s10995-007-0220-5. [DOI] [PubMed] [Google Scholar]
- 11.Child and Adolescent Health Measurement Initiative. FACCT—The Foundation for Accountability The children with special health care needs consumer quality measurement module CAHPS/AHRQ submitter’s kit. May 2001. Available at: http://childhealthdata.org/identifying-cshcn.
- 12.Bethell C, Read D, Neff J, et al. Comparison of the children with special health care needs screener to the questionnaire for identifying children with chronic conditions—revised. Ambul Pediatr. 2002;2:49–57. doi: 10.1367/1539-4409(2002)002<0049:cotcws>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 13.Bethell C, Read D, Stein R, et al. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2:38–48. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 14.Stein R, Westbrook L, Bauman L. The Questionnaire for Identifying Children with Chronic Conditions: a measure based on a noncategorical approach. Pediatrics. 1997;99:513–521. doi: 10.1542/peds.99.4.513. [DOI] [PubMed] [Google Scholar]
- 15.Stein R, Silver E, Bauman L. Shortening the Questionnaire for Identifying Children with Chronic Conditions (QuICCC): what is the consequence? Pediatrics. 2001;107:pe61. doi: 10.1542/peds.107.4.e61. [DOI] [PubMed] [Google Scholar]
- 16.Stein RE, Bauman LJ, Westbrook LE, et al. Framework for identifying children who have chronic conditions: the case for a new definition. J Pediatr. 1993;122:342–347. doi: 10.1016/s0022-3476(05)83414-6. [DOI] [PubMed] [Google Scholar]
- 17.Stein R, Bauman L, Epstein S, et al. How well does the QuICCC identify individual children who have chronic conditions? Arch Pediatr Adolesc Med. 2000;154:447–452. doi: 10.1001/archpedi.154.5.447. [DOI] [PubMed] [Google Scholar]
- 18.Stein R. To be or not to be… non-categorical. J Dev Behav Pediatr. 1996;17:36–37. doi: 10.1097/00004703-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 19.FACCT—The Foundation for Accountability Comparison of case finding questions by conceptual domain. 2000 Available at: http://childhealthdata.org/identifying-cshcn.
- 20.NCQA Technical Advisory Group Pediatric Living With Illness Screener and Supplemental Survey Module (LWIM) Prepared October 1999, Revised May 2000. Available at: http://childhealthdata.org/identifying-cshcn.
- 21.Halfon N, Houtrow A, Larson K, Newacheck PW. The changing landscape of disability in childhood. Future Child. 2012;22:13–42. doi: 10.1353/foc.2012.0004. [DOI] [PubMed] [Google Scholar]
- 22.Scheidt-Nave C, Ellert U, Thyen U, Schlaud M. [Prevalence and characteristics of children and youth with special health care needs (CSHCN) in the German Health Interview and Examination Survey for Children and Adolescents (KiGGS)] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:750–756. doi: 10.1007/s00103-007-0237-3. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt S, Thyen U, Petersen C, Bullinger M. The performance of the screener to identify children with special health needs in an European sample of children with chronic conditions. Eur J Pediatr. 2004;163:517–523. doi: 10.1007/s00431-004-1458-1. [DOI] [PubMed] [Google Scholar]
- 24.Hess JM, Pascale J, Rothgeb J, et al. The effects on person-level versus household-level questionnaire design on survey estimates and data quality. Public Opin Q. 2001;65:574–584. [Google Scholar]
- 25.Child and Adolescent Health Measurement Initiative Advisory Committee; CAHMI Living With Illness Task Force 2.5H Child Survey: a method for modifying the CAHPS 2.0H Child Survey to measure experience of care for children with ongoing health conditions. Measure work-up. Available at: http://childhealthdata.org/identifying-cshcn.
- 26.Bethell C, Newacheck P. Memo to NCQA Technical Advisory Group: Recommended measure for children with chronic conditions. October 19, 1999. Available at: http://childhealthdata.org/identifying-cshcn. [Google Scholar]
- 27.National Committee for Quality Assurance NCQA Endorsement of Children with Ongoing Health Needs (CSHCN) module: HMOS Focus on Quality of Children’s Health Care Quality. October 2000. Available at: http://childhealthdata.org/identifying-cshcn.
- 28.Afifi A, Kotlerman J, Ettner S, Cowan M. Methods for improving regression analysis for skewed continuous or counted responses. Annu Rev Public Health. 2007;28:95–111. doi: 10.1146/annurev.publhealth.28.082206.094100. [DOI] [PubMed] [Google Scholar]
- 29.Child and Adolescent Health Measurement Initiative . Approaches to Identifying Children and Adults with Special Health Care Needs: A Resource Manual for State Medicaid Agencies and Managed Care Organizations. Centers for Medicare and Medicaid Services; Washington, DC: 2002. Available at: http://www.cahmi.org/wp-content/uploads/2014/06/CSHCNS-CMS-manual.pdf. [Google Scholar]
- 30.FACCT, Robert Wood Johnson Foundation . A Portrait of Adolescents in America, 2001. FACCT—The Foundation for Accountability; Portland, Ore: 2001. Available at: http://www.ohsuhealth.com/_resources/uploads/uploads/pdfs/port-adolescents.pdf. [Google Scholar]
- 31.Pless IB, Pinkerton P. Chronic Childhood Disorder: Promoting Patterns of Adjustment. Year Book Medical Publishers; Chicago, Ill: 1975. [Google Scholar]
- 32.Perrin E, Newacheck P, Pless I, et al. Issues involved in the definition and classification of chronic health conditions. Pediatrics. 1993;91:787–793. [PubMed] [Google Scholar]
- 33.Stein R, Jessop D. What diagnosis does not tell: the case for a noncategorical approach to chronic illness in childhood. Soc Sci Med. 1989;29:769–778. doi: 10.1016/0277-9536(89)90157-3. [DOI] [PubMed] [Google Scholar]
- 34.Child and Adolescent Health Measurement Initiative 2009/10 NS-CSHCN: Prevalence of specific difficulties among CSHCN with each condition. Data Resource Center, 2012. Available at: http://childhealthdata.org/docs/cshcn/functional-difficulties-by-condition_ 2009-10.pdf.
- 35.Carle A, Blumberg S, Poblenz C. Internal psychometric properties of the Children With Special Health Care Needs Screener. Acad Pediatr. 2011;11:128–135. doi: 10.1016/j.acap.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 36.Evaluation of National Health Interview Survey diagnostic reporting. Vital Health Stat 2. 1994;120:1–116. [PubMed] [Google Scholar]
- 37.Cox B, Cohen S. A comparison of household and medical provider reports of medical conditions. In: Cox B, Cohen S, editors. Methodological Issues for Health Care Surveys. Marcel Dekker Inc; New York, NY: 1985. pp. 150–189. [Google Scholar]
- 38.Bethell C, Read D, Brockwood K. Using existing population-based data sets to measure the AAP definition of Medical Home for all children and children with special health care needs. Pediatrics. 2004;113:1529–1537. [PubMed] [Google Scholar]
- 39.Kohen D, Brehaut J, Garner R, et al. Conceptualizing childhood health problems using survey data: a comparison of key indicators. BMC Pediatr. 2007;5:7–40. doi: 10.1186/1471-2431-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Child and Adolescent Health Measurement Initiative, Data Resource Center for Child and Adolescent Health Nationwide disparities snapshot: children with special health care needs. National Survey of Children’s Health. 2007 Available at: http://www.childhealthdata.org/browse/snapshots/nsch-profiles/performance?geo¼1. Accessed April 9, 2012.
- 41.Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau . Children With Special Health Care Needs in Context: A Portrait of States and the Nation. The National Survey of Children’s Health, 2007. Dept of Health and Human Services; Rockville, Md: 2011. [Google Scholar]
- 42.Bethell C, Read D. Taking stock of the CSHCN Screener: MEPS longitudinal comparison of CSHCN status and disability over time. Child and Adolescent Health Measurement Initiative. 2006 Available at: http://childhealthdata.org/identifying-cshcn. [Google Scholar]
- 43.Jessop D, Stein R. Consistent but not the same: effects of method on chronic conditions rates. Arch Pediatr Adolesc Med. 2010;149:1105–1110. doi: 10.1001/archpedi.1995.02170230059008. [DOI] [PubMed] [Google Scholar]
- 44.Ireys H, Anderson G, Shaffer T, Neff J. Expenditures for care of children with chronic illnesses enrolled in the Washington State Medicaid program, fiscal year 1993. Pediatrics. 1997;100:197–204. doi: 10.1542/peds.100.2.197. [DOI] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention (CDC) Mental health in the United States: health care and well being of children with chronic emotional, behavioral, or developmental problems—United States, 2001. MMWR Morb Mortal Wkly Rep. 2005;54:985–989. [PubMed] [Google Scholar]
- 46.Wilhelm C, Bethell C, Newacheck PN, Strickland BS. Advancing methods to measure and promote health and quality of care for children at risk for special health care needs. Child and Adolescent Health Measurement Initiative White Paper. 2014 Apr; [Google Scholar]
- 47.Child and Adolescent Health Measurement Initiative 2009/10 NS-CSHCN: Comorbidity of conditions and difficulties among CSHCN. Data Resource Center. 2012 Available at: http://childhealthdata.org/docs/cshcn/conditions-difficulties-09cshcn_feb-2-2012.pdf.
- 48.National Survey of Children With Special Health Care Needs Data query from the Child and Adolescent Health Measurement Initiative, Data Resource Center for Child and Adolescent Health. NS-CSHCN 2009/10. Available at: www.childhealthdata.org. Accessed February 25, 2013.
- 49.Drew JA. Does the FACCT Special Health Care Needs Screener produce biased estimates of children with chronic conditions?; Poster Presentation at: Population Association of America; Los Angeles, CA. Mar-Apr. 2006. [Google Scholar]
- 50.Blumberg SJ, Read D, Avila RM, Bethell CD. Hispanic children with special health care needs from Spanish-language households. Pediatrics. 2010;126(suppl 3):S120–S128. doi: 10.1542/peds.2010-1466E. [DOI] [PubMed] [Google Scholar]
- 51.Read D, Bethell C, Blumberg SJ, et al. An evaluation of the linguistic and cultural validity of the Spanish language version of the Children With Special Health Care Needs Screener. Matern Child Health J. 2007;11:568–585. doi: 10.1007/s10995-007-0207-2. [DOI] [PubMed] [Google Scholar]
- 52.Richardson LA. Seeking and obtaining mental health services: what do parents expect? Arch Psychiatr Nurs. 2001;15:223–231. doi: 10.1053/apnu.2001.27019. [DOI] [PubMed] [Google Scholar]
- 53.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11:496–518. [PubMed] [Google Scholar]
- 54.Child and Adolescent Health Measurement Initiative Who are children with special health care needs? Data Resource Center. 2012 Available at: http://childhealthdata.org/docs/nsch-docs/whoarecshcn_revised_ 07b-pdf.pdf. [Google Scholar]
- 55.National Survey of Children’s Health. NSCH 2007 Data query from the Child and Adolescent Health Measurement Initiative, Data Resource Center for Child and Adolescent Health. Available at: http://www.childhealthdata.org. Accessed October 22, 2012.
- 56.Farmer JE, Marien WE, Frasier L. Quality improvements in primary care for children with special health care needs: use of a brief screening measure. Child Health Care. 2003;32:273–285. [Google Scholar]
- 57.Bramlett MD, Read D, Bethell C, Blumberg SJ. Differentiating subgroups of children with special health care needs by health status and complexity of health care needs. Matern Child Health J. 2009;13:151–163. doi: 10.1007/s10995-008-0339-z. [DOI] [PubMed] [Google Scholar]
- 58.Leslie LK, Sarah R, Palfrey JS. Child health care in changing times. Pediatrics. 1998;101(4):746–752. pt 2. [PubMed] [Google Scholar]
- 59.Davidson EJ, Silva TJ, Sofis LA, et al. The doctor’s dilemma: challenges for the primary care physician caring for the child with special health care needs. Ambul Pediatr. 2002;2:218–223. doi: 10.1367/1539-4409(2002)002<0218:tdsdcf>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 60.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126:647–655. doi: 10.1542/peds.2009-3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burns KH, Casey PH, Lyle RE, et al. Increasing prevalence of medically complex children in US hospitals. Pediatrics. 2010;126:638–646. doi: 10.1542/peds.2009-1658. [DOI] [PubMed] [Google Scholar]
- 62.Cohen E, Jovcevska V, Kuo DZ, Mahant S. Hospital-based comprehensive care programs for children with special health care needs: a systematic review. Arch Pediatr Adolesc Med. 2011;165:554–561. doi: 10.1001/archpediatrics.2011.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burke RT, Alverson B. Impact of children with medically complex conditions. Pediatrics. 2010;126:789–790. doi: 10.1542/peds.2010-1885. [DOI] [PubMed] [Google Scholar]
- 64.Child Development and Rehabilitation Center (CDRC) Establishing an integrated and collaborative program to improve health outcomes for children with complex special health care needs (C-CSHCN) through coordinated pediatric tertiary care and community-based services. Proposal to state Medicaid program. Final, January 2012. [Google Scholar]
- 65.Naar-King S, Ellis DA, Frey MA. Assessing Children’s Well-Being: A Handbook of Measures. Lawrence Erlbaum Associates; Mahwah, NJ: 2004. [Google Scholar]
- 66.Agency for Healthcare Research and Quality . CAHPS 2.0 Surveys. Agency for Healthcare Research and Quality; Rockville, Md: 1998. [Google Scholar]
- 67.Pless IB, Stein RE, Walker DK. Research Consortium on Children with Chronic Conditions (RCCCC): a vehicle for interdisciplinary collaborative research. Matern Child Health J. 2010;14:9–19. doi: 10.1007/s10995-009-0484-z. [DOI] [PubMed] [Google Scholar]
- 68.Neff JM, FACCT—The Foundation for Accountability Living with illness field trial: National Association of Children’s Hospitals and Related Institutions (NACHRI) condition list and Living With Illness Screener status results. FACCT LWIM Field Trial Final Report, 1999. Available at: http://childhealthdata.org/identifying-cshcn. [Google Scholar]
- 69.Neff JM, Sharp VL, Muldoon J, et al. Identifying and classifying children with chronic conditions using administrative data with the clinical risk group classification system. Ambul Pediatr. 2002;2:71–79. doi: 10.1367/1539-4409(2002)002<0071:iaccwc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 70.Bethell C, Gombojav N, Stumbo S, et al. Using the National Health Interview Survey and Medical Expenditures Panel Survey to Assess the Use and Impact of Complementary and Alternative Medicine for Children in the US: A Meta-Data Methods Summary Report. Child and Adolescent Health Measurement Initiative; Baltimore, Md: 2012. [Google Scholar]
- 71.Bethell CD, Kogan MD, Strickland BB, et al. A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations. Acad Pediatr. 2011;11(3 suppl):S22–S33. doi: 10.1016/j.acap.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 72.American Recovery and Reinvestment Act (ARRA) Title XIII: Health Information Technology for Economic and Clinical Health Act (HITECH) Available at: http://www.hitechanswers.net/about/about-arra/. Accessed November 25, 2014.
- 73.Department of Health and Human Services. Centers for Medicare and Medicaid Services Medicare and Medicaid programs—electronic health record incentive program, stage 2. 2012 Available at: http://www.himss.org/files/HIMSSorg/content/files/2012-21050_PI.pdf. [PubMed]