Abstract
Empathy deficits represent an important social impairment in autism spectrum disorders (ASD), but little is known about the early development of empathy prior to diagnosis. This study examined empathic responding to parental distress in toddlers at risk for an ASD. Children later diagnosed with an ASD engaged in less empathic responding at 24 and 30 months than children with no later diagnosis. Lower empathic responding was associated with higher autism symptomatology at 30 months. This is the first study to examine empathy deficits in response to parental distress in toddlers prior to ASD diagnosis. Early empathic responding may represent a unique developing social skill that indexes the overall severity of later ASD symptomatology in at-risk children.
Keywords: Empathy, Response to distress, At-risk siblings, Autism spectrum disorders
Introduction
Empathy is the ability to feel or imagine another’s emotional experience. The experience of empathy is thought to promote socially competent behaviors, such as prosociality (Eisenberg and Fabes 1998). Social interaction impairments, including difficulties with social and emotional reciprocity, are central deficits in autism spectrum disorders (ASD; APA 2000). These social difficulties may be related to a deficit in empathy. Although several studies have shown clear deficits in empathic responding and emotion recognition abilities in children and adults with an ASD (e.g., Yirmiya et al. 1992; Dyck et al. 2001), less is known about the early development of empathy in this population. The current study addressed this gap in the literature by examining early empathic responding to parental distress in toddlers at heightened risk for an ASD, due to having an older sibling with an ASD diagnosis.
Early Empathy Development in Typically Developing Children
The emergence of empathy has been well documented among typically developing children. In the first days of life, infants demonstrate pre-cursors to empathic feelings, through the experience of reflexive crying in response to other infants’ cries (Martin and Clark 1982; Sagi and Hoffman 1976). This experience of personal distress in response to others’ negative emotions is characteristic of pre-empathic behavior in the first year of life. During the second year of life, children commonly transition from personal distress in response to another’s distress to demonstrating concern for others (Zahn-Waxler et al. 1992). By approximately 18 months of age, a majority of typically developing toddlers display concern about others’ distress (e.g., sad look, “I’m sorry”), and are capable of a wide variety of helping behaviors (e.g., verbal or physical comfort, sharing, and distracting the person in distress; Knafo et al. 2008; Zahn-Waxler et al. 1992). Children tend to engage in more empathy-related behaviors, particularly prosocial behaviors, in response to the simulated distress of their mother rather than an examiner’s during the second and third years of life (Zahn-Waxler et al. 1992). The current study utilized a simulated distress paradigm to measure early empathic responding to parental distress during the third year of life.
Empathy Deficits in Autism Spectrums Disorders
Although the early development of empathy in typically developing children is well established, less is known about the development of empathy in the context of risk for ASD. Multiple theories of autism, including the extreme male brain theory (Baron-Cohen 2002), the mirror neuron hypothesis (e.g., Oberman and Ramachandran 2007), and the ‘theory of mind’ theory (e.g., Baron-Cohen et al. 1985) posit a central role of empathy deficits in the disorder. The latter theory of autism proposes a prominent role of deficits in the ability to understand the perspectives of others, or cognitive empathy, in contributing to the pervasive social and communication deficits present in individuals with ASDs (Baron-Cohen et al. 1985; White et al. 2009).
A small number of cross-sectional investigations have examined the empathic abilities of young children with an ASD diagnosis. In a seminal study, Sigman et al. (1992) examined children’s responses to the distress of an examiner and their parent, in a sample of preschool-aged children with autism and intellectual disabilities, and mental age-matched typically developing controls. Utilizing continuous measures of several empathy-related behaviors, they found that children with autism attended more to the toys and less to both distressed adults than typically developing children and children with intellectual disabilities. Children with autism were also rated as less concerned than controls during the emotional displays of the adults, although displays of negative affect and comforting behaviors were rare across groups. In Bacon et al. (1998) examination of preschool-aged children’s responses to an examiner’s simulated distress, a low-functioning autism group (Nonverbal IQ < 80) exhibited less response to distress than other groups (i.e., children with high-functioning autism, mental retardation, language deficits, and typically developing children), with nearly half of the children with low-functioning autism showing no response to the examiner. Finally, Charman et al. (1997) examined the empathic responding of very young children diagnosed with autism (20 months). All of the children in the comparison groups (including typically developing children and children with developmental delays) paid attention to the person in distress; however, less than half of the autism group looked to the distressed adult. Strikingly, none of the children in the autism group showed signs of facial concern (e.g., brow furrowing), in comparison to approximately half of the children in the other groups.
Although these studies provide evidence of empathy impairments in children with autism from a relatively early age, it is not clear whether these impairments preceded diagnosis. Moreover, the cross-sectional nature of these studies precluded an evaluation of the development of empathy-related behaviors over time. In contrast, Dissanayake et al. (1996) conducted a longitudinal investigation of the stability of children with autism’s responses to an examiner’s distress between preschool age and a follow-up time point 5 years later. Children’s empathy ratings from preschool age predicted their later empathic responding to similar emotional displays 5 years later, suggesting long-term stability of the measure and construct. The present study examined empathic responding at two time points that occurred early in development and prior to an ASD diagnosis.
More recently, Hutman et al. (2010) conducted a longitudinal study examining response to distress in toddlers at risk for an ASD. Children were considered high-risk if they had an older sibling with an ASD. Distress response was measured at 12, 18, 24, and 36 months of age by examining children’s reactions to an examiner pretending to hurt herself during play. Children who were later diagnosed with an ASD paid less attention to and showed less affective response to the examiner’s distress than comparison children (high- and low-risk children with no later diagnosis) across all time points, even after controlling for verbal abilities.
The Current Study
The current study investigated the presence of empathy deficits prior to an ASD diagnosis, as measured by children’s responses to their parent’s distress. Studies of typically developing children have suggested that young children may be more likely to empathize with a parent than with an examiner (Zahn-Waxler et al. 1992). However, response to parental distress is less well-studied in the ASD population, and, to the authors’ knowledge, has not been studied in children at risk for an ASD. We asked whether empathy deficits observed in toddlers at risk for an ASD are apparent during interactions with a familiar social partner. To best capture the variability in children’s empathy-related behaviors and autism symptomatology, we utilized continuous measures of these behaviors. Autism symptomatology was measured at 30 months of age with the Autism diagnostic observation schedule (ADOS; Lord et al. 2000), a commonly used structured observational measure (e.g., Hutman et al. 2010; Yoder et al. 2009). The calibrated ADOS severity score, proposed and validated by Gotham et al. (2009), served as a continuous measure of ASD symptomatology. This study examined the empathic responding of toddlers who received an ASD diagnosis at 3 years of age and those who did not receive a diagnosis. Empathy-related behaviors were measured at 24 and 30 months of age, ages at which typically developing children are expected to have begun responding empathically to others in distress. We looked prospectively at young children with an increased risk for an ASD (i.e., had an older sibling with an ASD diagnosis) to examine early manifestations of empathy prior to diagnosis.
The current study tested the following hypotheses:
Empathy-related behaviors will increase from 24 to 30 months of age.
Children later diagnosed with an ASD will show less empathic responding than children who do not receive an ASD diagnosis.
There will be an interaction between age and diagnosis, with the empathic responding of children who were later diagnosed with an ASD increasing less over time than children who did not receive a diagnosis.
Level of empathic responding at 24 and at 30 months of age will be associated with the level of autism symptomatology at 30 months of age, with more empathic responding corresponding to lower symptomatology.
Method
Participants
Participants were enrolled in a longitudinal study examining the early social and emotional development of infants at risk for developing an ASD. Several recruitment strategies were utilized, including: (1) obtaining referrals from a university-based autism service, (2) distributing a brochure at autism-related events and other functions to parents of infants, (3) mailing a brochure to parents of infants whose addresses and names were obtained from county birth records, (4) contacting child care programs, and (5) “word of mouth.” Of participants eligible for this study, 11 were lost due to attrition or missed appointments, and 4 due to technical difficulties with video recordings of the empathy task. The sample included in this report (N = 38) consisted of participants who completed the empathy task at both 24 and 30 months, and had diagnostic outcome data available at 30 and 36 months. Infants were considered to be high-risk if they had at least one older sibling with an ASD diagnosis. Older sibling diagnoses were confirmed by an experienced, licensed psychologist, based upon DSM-IV-TR diagnostic criteria and results from the ADOS (Lord et al. 2000). See Table 1 for participant information.
Table 1.
Participant information by diagnostic group
| ASD | No ASD | |
|---|---|---|
| N | 13 | 25 |
| Gender | ||
| Female | 3 | 6 |
| Male | 10 | 19 |
| Ethnicity | ||
| White/Caucasian | 5 | 8 |
| African–American | 0 | 1 |
| Hispanic/Latino | 4 | 11 |
| Asian/Pacific Islander | 1 | 0 |
| Mixed ethnicity/other | 3 | 5 |
| Mean (SD) level of maternal education (1 = less than high school; 6 = advanced/professional degree) | 4.77 (1.54) | 4.88 (1.36) |
| Mean (SD) 36-month developmental scores | ||
| Early learning composite (standard score) | 77.62 (16.13) | 95.32 (11.83) |
| Receptive language (T-score) | 35.23 (12.32) | 45.64 (8.62) |
| Expressive language (T-score) | 42.69 (13.18) | 49.24 (7.13) |
| Mean 30-month ADOS severity | 5.15 (2.15) | 2.16 (1.28) |
ASD autism spectrum disorder, ADOS autism diagnostic observation schedule. Developmental scores were obtained from the Mullen Scales of Early Learning (MSEL; Mullen 1995), which is a normed standardized developmental measure for children from birth to 68 months of age. Standardized scores from the 24-month MSEL were used for three participants in lieu of 36-month MSEL scores due to missing data. Diagnostic groups were significantly different on MSEL scores and ADOS severity
Assessment of ASD Diagnosis and Severity
Following the 36-month time point, younger siblings were diagnosed, yielding the following clinical outcomes: Autistic Disorder (autism), Pervasive Developmental Disorder—Not Otherwise Specified (PDD), or No ASD. Diagnoses were made by an experienced, independent licensed psychologist who was blind to sibling group status. Diagnostic decisions were made according to DSM-IV-TR criteria, informed by results from the Autism diagnostic inventory—revised (ADI-R; administered at 36 months; two children, who did not have a 36-month ADI-R, had an ADI-R administered between 4 and 5 years of age; Lord et al. 1994) and the ADOS (administered at 30 months). The ADI-R is a semi-structured parent interview that assesses specific symptoms of ASDs in the domains of social interaction, communication, restricted and repetitive behaviors and interests, and early development. The ADOS is a play-based structured observational measure designed to elicit behaviors that are relevant to an ASD diagnosis (Lord et al. 2000). Reliability of these diagnoses was assessed by a second expert licensed psychologist who reviewed the videotapes and records for a large subset (84%) of this sample. Good diagnostic reliability was established (Kappa = .94, 97% agreement). The autism and PDD diagnoses were combined to form one ASD group, yielding 13 children diagnosed with an ASD and 25 children with no ASD diagnosis.
To provide a continuous measure of ASD symptomatology, ADOS severity scores were calculated for each child (Gotham et al. 2009). In accordance with Gotham et al.’s (2009) criteria, severity scores were assigned based on the children’s ADOS algorithm score, age, and language level. Severity scores in this study ranged from 1 to 10. All ADOS protocols were scored by experienced clinicians who had attained research reliability with a designated ADOS trainer.
Assessment of Empathic Responding
Procedure
At the 24- and 30-month time points, families visited the university laboratory. Prior to the session, a trained examiner gave the parent the following instructions for the empathy task: “After you and [child’s name] play for a while, I will step into the room to alert you to begin pretending that you have something in your eye. Act like it really bothers you by saying ‘Oh, I have something in my eye.’ Carry on like this for a while but don’t say your child’s name or suggest your child do anything to help you feel better.” If the parent did not begin the empathy task at the first prompt, the examiner prompted the parent unobtrusively up to two times. The task lasted approximately 1 min. It was terminated when the examiner re-entered the room and instructed the parent to tell the child that his or her eye felt better.
Coding
An empathy coding system, originally established for use with typically developing toddlers by Zahn-Waxler et al. (1992) and adapted by Young et al. (1999) was utilized for this study. Since our sample was at risk for language deficits, minor adaptations were made to this coding system to remove any bias toward higher scores for verbal rather than non-verbal responses. Two undergraduate research assistants who were blind to sibling group status and eventual diagnosis were trained to reliability on this coding system. Each episode was given ratings on four empathy-related dimensions: Empathic Concern (1–4), Prosocial Behavior (1–4), Arousal Level (1–5), and Global Empathy (1–7). See Table 2 for more specific information on these dimensions. To ensure the quality of the parent performances, an independent undergraduate research assistant rated them for Credibility (1—not believable, 2—passable, 3—particularly authentic) and Affective Intensity (1—little or no affect, 2—moderate level of affect, 3—high affect and pain expressed; Young et al. 1999).
Table 2.
Description and ratings of empathy-related dimensions
| Dimension | Description | Ratings | |
|---|---|---|---|
| Empathic concern | Facial, gestural, and vocal signs of distress and sympathy | 1 = none | |
| 2 = sobering of attention, slight concern | |||
| 3 = moderate concern, including brow furrowing | |||
| 4 = strong facial concern, brow furrowing, reflecting sadness; sympathetic expression | |||
| Prosocial behavior | Children’s attempts to comfort or relieve parent’s distress | 1 = none | |
| 2 = briefly assisting | |||
| 3 = moderate assistance | |||
| 4 = repeated or prolonged assistance | |||
| Arousal level | Body tension (e.g., stiff posture, discontinuing play, attention to parent) | 1 = child ignores parent | |
| 2 = child attends to victim with little body tension, play is uninterrupted | |||
| 3 = moderate arousal, play is disrupted | |||
| 4 = moderately high arousal, body tension, postural freezing | |||
| 5 = high arousal, prolonged body tension, postural freezing | |||
| Global empathy | Overall quality of the children’s empathic responding | 1 = none | |
| 3 = mild concern, no prosocial action | |||
| 5 = moderate concern, some prosocial behavior | |||
| 7 = strong expressions of concern and caring behavior | |||
Coding system adapted from Young et al. (1999)
Reliability
Thirty percent of the total 24- and 30-month videotapes in the sample were double-coded to assess reliability. Intra-class correlations, using mean absolute-agreement on the four empathy-related dimensions, indicated good reliability: Empathic Concern (.80), Prosocial Behavior (1.00), Arousal Level (.93), and Global Empathy (.85). With respect to parent performance, there was high agreement on Credibility (96%) and Affective Intensity (100%) scores. All parents in the sample were rated as having at least a passable performance, and most parents expressed a moderate level of affect. These ratings are consistent with those reported by Young et al. (1999). Parent performance scores were not associated with corresponding 24- or 30-month Global Empathy ratings (24-month, Credibility, r(37) = −.07, ns; 24-month, Intensity, r(37) = .12, ns; 30-month, Credibility, r(37) = .14, ns; 30-month, Intensity, r(37) = .25, ns) or ADOS severity scores (Mean Credibility, r(37) = −.02, ns; Mean Intensity, r(37) = .09, ns); accordingly, they were not included in subsequent analyses.
Results
Preliminary Analyses
Pearson’s correlations were computed for empathy-related dimensions within and between each time point (see Table 3). At each time point, most of the empathy-related dimensions were significantly correlated with one another. In addition, the empathy-related dimensions of Empathic Concern, Arousal Level, and Global Empathy were stable between 24 and 30 months.
Table 3.
Correlations between empathy-related dimensions within and between time points (N = 38)
| Dimension | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 24 months | ||||||||
| 1. Empathic concern | – | .38* | .73** | .72** | .45** | .15 | 31 | .42** |
| 2. Prosocial behavior | – | .26 | .72** | .49** | .11 | .28 | .28 | |
| 3. Arousal level | – | .77** | .39* | .20 | .44** | .43** | ||
| 4. Global empathy | – | .57** | .24 | .44** | .49** | |||
| 30 months | ||||||||
| 5. Empathic concern | – | .43** | .72** | .75** | ||||
| 6. Prosocial behavior | – | .49** | .86** | |||||
| 7. Arousal level | – | .75** | ||||||
| 8. Global empathy | – |
Significant at .05 level
Significant at .01 level
Four 2 (Age) × 2 (Gender) Mixed Design ANOVAs were conducted to assess for gender differences in Empathic Concern, Prosocial Behavior, Arousal Level, or Global Empathy. No gender differences were found on any of these dimensions; thus, gender was not included in further analyses.
Empathic Responding and ASD Diagnosis
Descriptive statistics for ratings of empathy-related dimensions by diagnostic group are presented in Table 4. Global Empathy ratings were approximately normally distributed. A 2 (Age) × 2 (Diagnosis) Mixed Design ANOVA was conducted, with the Global Empathy rating used as the dependent variable. First, we hypothesized that children would respond more empathically at 30 months than at 24 months. Support was found for this hypothesis, F(1,36) = 8.71, p < .01, partial η2 = .20. Next, we hypothesized that children later diagnosed with an ASD would show lower global empathic responding than children with no later diagnosis. Support was found for this hypothesis, F(1,36) = 6.33, p < .05, partial η2 = .15. Finally, we hypothesized that children later diagnosed with an ASD would show smaller increases in empathy with age than children with no later diagnosis. No support was found for this hypothesis, F(1,36) = .04, ns.
Table 4.
Means (and SDs) for empathy-related dimensions by age and diagnosis
| Diagnosis group | Empathic concern (1–4) | Prosocial behavior (1–4) | Arousal level (1–5) | Global empathy (1–7) |
|---|---|---|---|---|
| 24 months | ||||
| ASD | 1.31 (.48) | 1.08 (.28) | 2.00 (1.16) | 1.77 (1.01) |
| No ASD | 1.84 (.75) | 1.60 (.87) | 2.88 (1.33) | 2.96 (1.40) |
| 30 months | ||||
| ASD | 1.54 (.66) | 1.85 (1.28) | 2.38 (1.71) | 2.69 (1.75) |
| No ASD | 2.04 (.94) | 2.20 (1.23) | 2.96 (1.14) | 3.76 (1.83) |
ASD autism spectrum disorder. ASD n = 13, No ASD n = 25
Age and Diagnosis group differences in Empathic Concern, Prosocial Behavior, and Arousal Level were explored. Although a MANOVA would have controlled for correlations between these variables, the increased parametric assumptions of a MANOVA and sample size considerations led us to conduct separate ANOVAs. Three 2 (Age) × 2 (Diagnosis) Mixed Design ANOVA tests were conducted. The 24-month Empathic Concern and Prosocial Behavior variables were not normally distributed (24-mo Empathic Concern: Skewness = 1.09, Kurtosis = 1.80; 24-month Prosocial Behavior Skewness = 1.85, Kurtosis = 2.95), so nonparametric analyses were also conducted for these variables. As these nonparametric analyses revealed parallel results, only the results of the ANOVAs are reported. For Empathic Concern, a main effect of Diagnosis was found, F(1,36) = 5.64, p < .05, partial η2 = .14; children who were later diagnosed with an ASD showed lower levels of facial, vocal, and gestural concern than those with no later diagnosis. No other significant effects were found for Empathic Concern. For Prosocial Behavior, a main effect of Age was found, F(1,36) = 8.21, p < .01, partial η2 = .19, with younger children showing lower levels of help attempts. There were no other significant effects for Prosocial Behavior, indicating a lack of difference in helping behavior between diagnostic groups. In addition, a marginally significant effect of Arousal Level was found, F(1,36) = 3.75, p < .07, partial η2 = .09; children who were later diagnosed with an ASD tended to exhibit less bodily arousal in response to parental distress than children with no later diagnosis. No other effects were found for Arousal Level.
Empathic Responding and ASD Severity
The relation between Global Empathy and ADOS severity was also analyzed. Since ADOS severity evidenced considerable positive skew, Spearman’s and Pearson’s correlations are reported. We hypothesized that children who responded more empathically at 24 and 30 months would exhibit less autism symptomatology at 30 months. Support was found for this hypothesis at both 24 months, r(37) = −.45, p < .01 (see Fig. 1), rs(37) = −.46, p < .01, and 30 months, r(37) = −.43, p < .01, rs(37) = −.42, p < .01. At both ages, there was an inverse association between level of empathy and autism symptomatology.
Fig. 1.
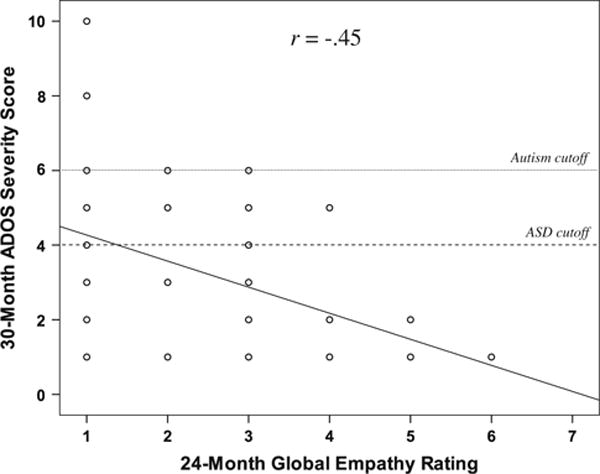
The prediction of 30-month ADOS severity score from 24-month global empathy. ASD autism spectrum disorder, ADOS autism diagnostic observation schedule. Significant at .01 level (N = 38)
Discussion
In this study, children who were later diagnosed with an ASD showed less global empathic responding to their parent’s distress than children with no later diagnosis. Specifically, children who were later diagnosed with an ASD showed less expressed concern, and tended to show less bodily arousal, in response to their distressed parent than children who did not receive a diagnosis. Importantly, children with lower levels of global empathic responding at 24 and 30 months of age exhibited higher levels of autism symptomatology at 30 months of age. This is one of the first studies to investigate empathic responding in high-risk toddlers prior to diagnosis with an ASD, the first to examine empathy in response to parental distress in a sample at risk for an ASD, and the first to find that pre-diagnosis levels of empathic responding predict later ASD severity.
The current results are consonant with findings of empathy deficits in young children with an ASD (Bacon et al. 1998; Charman et al. 1997; Sigman et al. 1992). In addition, the present results are consistent with those of Hutman et al. (2010), which showed deficits in high-risk children’s responses to an experimenter’s distress prior to ASD diagnosis, and extend those findings. The current results indicate that early empathy deficits can also be detected in the young child’s response to the distress of a primary caregiver from quite early in development, and prior to ASD diagnosis. This is also consistent with Sigman et al. (1992), who studied empathic responding to experimenter and parental distress in preschool-aged children after ASD diagnosis. As toddlers are more likely to respond empathically to a parent rather than a stranger in distress (Zahn-Waxler et al. 1992), these findings support the idea that empathy deficits in young children with an ASD occur across a range of situations and social partners, even when measured prior to an ASD diagnosis. Additionally, the robust findings for the analyses with ADOS severity, suggest that continuous measures of ASD symptomatology may be particularly sensitive to social-emotional differences in at-risk siblings.
Examination of specific dimensions of empathic responding, including empathic concern, prosocial behavior, and arousal level, revealed varying results. Consistent with findings from previous studies showing deficits in facial concern (Charman et al. 1997) and more general concern (Sigman et al. 1992) among children with an ASD, children who were later diagnosed with an ASD displayed less empathic concern than children with no diagnosis. Additionally, there was a marginal difference between groups on arousal level, suggesting that children later diagnosed with an ASD tended to exhibit lower levels of attention and bodily arousal to their distressed parents than the children with no diagnosis. This is consistent with previous literature indicating less attention to distressed adults in children with an ASD (e.g., Charman et al. 1997). Contrary to expectations, however, there was no difference between children with and without a later ASD diagnosis in prosocial behavior. The prosocial behavior of children with or at risk for an ASD is less well-studied than the previous empathy-related dimensions. This lack of difference may be partially attributed to the relatively low levels of pro-social behavior across groups, similar to findings in Sigman et al. (1992), but may also indicate that differences in helping behaviors in children with an ASD are not apparent at this young age.
We also investigated the possibility of an interaction effect between diagnosis and age on empathic behaviors. Contrary to our hypothesis, the present study did not find evidence of an interaction effect between ASD diagnosis and age on any of the empathy-related dimensions. This suggests that there were no differences between children with and without a later ASD diagnosis in age-related changes in empathic behaviors.
Although the current study did not distinguish among theories of autism, it provides general support for theories positing a central role of empathy impairments in the social and communication deficits present in autism (e.g., Baron-Cohen et al. 1985; Oberman and Ramachandran 2007). Overall, an emerging literature provides evidence for the significance of empathy difficulties in emerging ASD.
Limitations and Future Directions
Although this study makes important contributions to the literature, the current findings should be interpreted in light of study limitations. Sample size was small, although power was sufficient to indicate differences between groups and a significant association between empathic responding and ASD severity. Lack of power may have limited our ability to find significant differences in the empathy-related dimensions of arousal level and prosocial behavior. Additional longitudinal assessments of empathy, potentially in a range of situations and with a range of social partners, would strengthen the emerging literature on empathy deficits in children developing an ASD. In addition, it will be important to investigate possible contributors to individual differences in empathic ability, such as characteristics of early parent–child interactions, potential genetic contributors (e.g., oxytocin), and possible neural differences (e.g., mirror neuron system functioning). Finally, future studies should investigate possible implications of empathy deficits for children on the autism spectrum over time, including social competence and prosocial behavior.
Clinical Implications
In addition to suggesting avenues for future research, findings from this study have important clinical implications. As differences in empathy were apparent prior to diagnosis, observed or reported empathy deficits may be an important early marker for ASD risk, and, when used in conjunction with other measures, may constitute a useful tool for early assessment of ASD. Further, results from this study indicated more variability in ADOS severity at the lower end of the empathy spectrum than at the higher end. Children with higher empathy scores almost uniformly displayed low levels of later autism symptoms, yet children with lower empathy scores showed both high and low levels of later ASD symptoms. This suggests that empathy abilities, at least as assessed in this context, may be better thought of as a protective factor in emerging ASD. This may be especially true in high-risk siblings, with empathic abilities potentially buffering against other risk factors. A prospective focus of additional research in this area is the development of interventions to increase empathic responding and improve outcomes for infants and toddlers at risk for an ASD.
Acknowledgments
This study was supported by grants from the National Institutes of Health: R01 HD047417 and R01 HD057284, Autism Speaks, and the Marino Autism Research Institute. The authors would like to thank the children and families who participated in this longitudinal study. In addition, the authors are grateful for the behavioral coding contributions of Haley Gordon and Gizelle Robinson, as well as the valuable feedback provided by Naomi Ekas, Heather Henderson, Alexandra Quittner, and Kristin Lindahl. This study was originally prepared as the first author’s master’s thesis.
References
- American Psychiatric Association. Diagnostic and statistical manual. 4th. 2000. Text Revision. [Google Scholar]
- Bacon AL, Fein D, Morris R, Waterhouse L, Allen D. The responses of autistic children to the distress of others. Journal of Autism and Developmental Disorders. 1998;28:129–142. doi: 10.1023/a:1026040615628. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S. The extreme male brain theory of autism. Trends in Cognitive Sciences. 2002;6:248–254. doi: 10.1016/s1364-6613(02)01904-6. [DOI] [PubMed] [Google Scholar]
- Baron-Cohen S, Alan AM, Frith U. Does the autistic child have a ‘theory of mind’? Cognition. 1985;21:37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- Charman T, Swettenham J, Baron-Cohen S, Cox A, Baird G, Drew A. Infants with autism: An investigation of empathy, pretend play, joint attention, and imitation. Developmental Psychology. 1997;33:781–789. doi: 10.1037//0012-1649.33.5.781. [DOI] [PubMed] [Google Scholar]
- Dissanayake C, Sigman M, Kasari C. Long-term stability of individual differences in the emotional responsiveness of children with autism. Journal of Child Psychology and Psychiatry. 1996;37:461–467. doi: 10.1111/j.1469-7610.1996.tb01427.x. [DOI] [PubMed] [Google Scholar]
- Dyck MJ, Ferguson K, Shochet IM. Do autism spectrum disorders differ from each other and from non-spectrum disorders on emotion recognition tests? European Child and Adolescent Psychiatry. 2001;10:105–116. doi: 10.1007/s007870170033. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Fabes R. Prosocial development. In: Eisenberg N, Damon (Series Ed) W, editors. Handbook of child psychology: Vol 3. Social, emotional, and personality development. 5th. New York: Wiley; 1998. pp. 701–778. [Google Scholar]
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39:693–705. doi: 10.1007/s10803-008-0674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutman T, Rozga A, DeLaurentis AD, Barnwell JM, Sugar CA, Sigman M. Response to distress in infants at risk for autism: A prospective longitudinal study. Journal of Child Psychology and Psychiatry. 2010;51:1010–1020. doi: 10.1111/j.1469-7610.2010.02270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knafo A, Zahn-Waxler C, Van Hulle C, Robinson JL, Rhee SH. The developmental origins of a disposition toward empathy: Genetic and environmental contributions. Emotion. 2008;8:737–752. doi: 10.1037/a0014179. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24:659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Martin GB, Clark RD. Distress crying in neonates: Species and peer specificity. Developmental Psychology. 1982;18:3–9. [Google Scholar]
- Mullen EM. Mullen scales of early learning. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- Oberman LM, Ramachandran VS. The simulating social mind: The role of the mirror neuron system and simulation in the social and communicative deficits of autism spectrum disorders. Psychological Bulletin. 2007;133:310–327. doi: 10.1037/0033-2909.133.2.310. [DOI] [PubMed] [Google Scholar]
- Sagi A, Hoffman ML. Empathic distress in the newborn. Developmental Psychology. 1976;12:175–176. [Google Scholar]
- Sigman MD, Kasari C, Kwon J, Yirmiya N. Responses to the negative emotions of others by autistic, mentally retarded, and normal children. Child Development. 1992;63:796–807. [PubMed] [Google Scholar]
- White S, Hill E, Happe F, Frith U. Revisiting the strange stories: Revealing mentalizing impairments in autism. Child Development. 2009;80:1097–1117. doi: 10.1111/j.1467-8624.2009.01319.x. [DOI] [PubMed] [Google Scholar]
- Yirmiya N, Sigman MD, Kasari C, Mundy P. Empathy and cognition in high-functioning children with autism. Child Development. 1992;63:150–160. [PubMed] [Google Scholar]
- Yoder P, Stone WL, Walden T, Malesa E. Predicting social impairment and ASD diagnosis in younger siblings of children with autism spectrum disorder. Journal of Autism Developmental Disorders. 2009;39:1381–1391. doi: 10.1007/s10803-009-0753-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SK, Fox NA, Zahn-Waxler C. The relations between temperament and empathy in 2-year-olds. Developmental Psychology. 1999;35:1189–1197. doi: 10.1037//0012-1649.35.5.1189. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Radke-Yarrow M, Wagner E, Chapman M. Development of concern for others. Developmental Psychology. 1992;28:126–136. [Google Scholar]


