Background:
Currently, there is no validated quality-of-life instrument that evaluates both functional and aesthetic outcomes after rhinoplasty. The goal of this study was to develop and validate a comprehensive quality-of-life instrument to assess patient satisfaction with both functional and aesthetic outcomes after rhinoplasty.
Methods:
The study was designed as a prospective instrument validation study at a university-affiliated academic medical center. Inclusion criteria included patients with nasal obstructive symptoms, nasal aesthetic deformity, or both, who underwent functional and/or aesthetic rhinoplasty by a single surgeon between December 2014 and June 2015. A novel 10-item instrument (the Rhinoplasty Health Inventory and Nasal Outcomes [RHINO] scale) was developed to assess physical, mental, and social well-being after functional and/or aesthetic rhinoplasty. Instrument validation was performed by assessment of test–retest reliability, internal consistency reliability, construct validity, and concurrent validity.
Results:
Twenty-two patients (10 males and 12 females) were enrolled. Mean age was 34.9 years (range: 18–67 years). All patients were followed for a minimum of 12 weeks (range: 12–23 weeks; mean: 16.5 weeks). Mean RHINO score was 51.4 ± 13.8 on the first preoperative evaluation and 51.7 ± 12.5 when repeated preoperatively on the day of surgery (r = 0.94; P < 0.001). Internal consistency demonstrated Cronbach’s α value of 0.74. Mean postoperative RHINO score was 84.7 ± 14.1 (mean difference from preoperative RHINO = 33.2 ± 18.9; P < 0.001).
Conclusions:
The RHINO instrument demonstrates robust reliability and validity in assessing patient-reported satisfaction with rhinoplasty outcomes.
Assessment of treatment efficacy and outcomes in rhinoplasty can be implemented using a variety of objective or subjective measures. A well-recognized criticism of objective outcome measures in rhinoplasty is the frequent and often significant divergence between objectively quantifiable measurements and subjective patient-reported outcomes.1 As a result, subjective quality-of-life (QOL) instruments have assumed an increasingly prevalent role in the assessment of outcomes after nasal surgery. This is intuitive to cosmetic nasal surgery as patient satisfaction is the most critical indicator of a successful outcome but is also equally as applicable to functional rhinoplasty.
To this end, various QOL instruments have been developed to assess patient-reported outcomes after nasal surgery. Two of the most widely applied instruments include the Nasal Obstructive Symptom Evaluation (NOSE) scale and the Rhinoplasty Outcomes Evaluation (ROE) scale.2,3 The former has been used to study outcomes of functional rhinoplasty procedures and to create a severity scale for nasal obstruction.4–6 Studies using the latter scale, namely measuring aesthetic outcomes, have been much less common. It is interesting to note that both these validated instruments have segregated the assessment of aesthetic and functional outcomes after nasal surgery. In many ways, this is an artificial distinction as it is well accepted that nasal function and aesthetics are closely related.
It is evident that to achieve successful results after rhinoplasty, patients must report satisfaction with both functional and aesthetic outcomes. The goal of this study was to develop and validate a comprehensive QOL instrument to assess patient satisfaction with functional and aesthetic outcomes after rhinoplasty.
METHODS
Patients
This prospective instrument validation study was performed at Stanford University, after approval by the Stanford Institutional Review Board. All patients were consented for the study using an informed consent document reviewed and approved by the Stanford Institutional Review Board. Data were obtained prospectively by consecutive enrollment of patients evaluated and treated by the single surgeon (S.P.M.). The study period extended from December 2014 to June 2015, during which time surgeries were performed by the senior author, and patients were followed for a minimum of 3 months postoperatively. Inclusion criteria included (1) patient aged 18 years or older; (2) patient presenting complaint of nasal obstruction, nasal aesthetic deformity, or both; and (3) patients who are appropriate candidates for functional or aesthetic rhinoplasty. Exclusion criteria included (1) patient aged younger than 18 years and (2) patients who were planned for functional or aesthetic rhinoplasty in combination with concurrent sinus surgery or sleep apnea surgery.
Instrument Development and Validation
The World Health Organization has defined health as a state of physical, mental, and social well-being.7 Accordingly, measurements of these 3 domains have been targeted by health-related QOL instruments. The Rhinoplasty Health Inventory and Nasal Outcomes (RHINO) scale was correspondingly developed as a 10-item questionnaire to evaluate outcomes in these 3 health domains. In addition, the RHINO scale assesses each of these 3 domains as it specifically pertains to either nasal function or aesthetics, with equal halves (5 items each) divided between the 2. Each item in the survey is scored on a Likert scale from 1 to 5, with high numbers indicating greater satisfaction. The 10-item scores are then summated and multiplied by 2, to create a final score on a 100-point scale. The RHINO instrument is demonstrated in Figure 1.
Fig. 1.
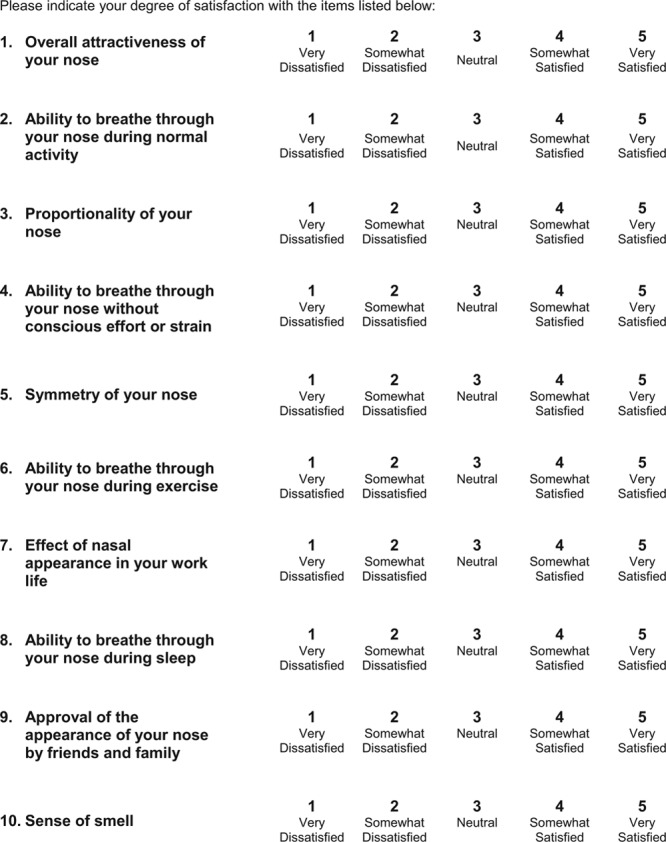
The RHINO scale.
Patients enrolled in the study were asked to complete the RHINO instrument on 3 separate occasions: (1) preoperatively at the consultation visit, (2) preoperatively on the day of surgery, and (3) postoperatively approximately 3 months after surgery. Statistical analysis was completed using SPSS version 22.0 (IBM Corp., Armonk, N.Y.). Test–retest reliability was assessed via Pearson’s correlation coefficient. Internal consistency reliability was assessed via Cronbach’s α, a statistical tool that determines the correlation of items in a survey instrument and is commonly used to estimate the reliability of psychometric tests. Construct validity was confirmed by analyzing responsiveness to change by comparison of preoperative and postoperative RHINO scores via paired samples t-test. Concurrent validity was assessed by cross-referencing patient RHINO scores for functional items with NOSE scores obtained at the same visit, using Pearson’s correlation coefficient.
RESULTS
Patients
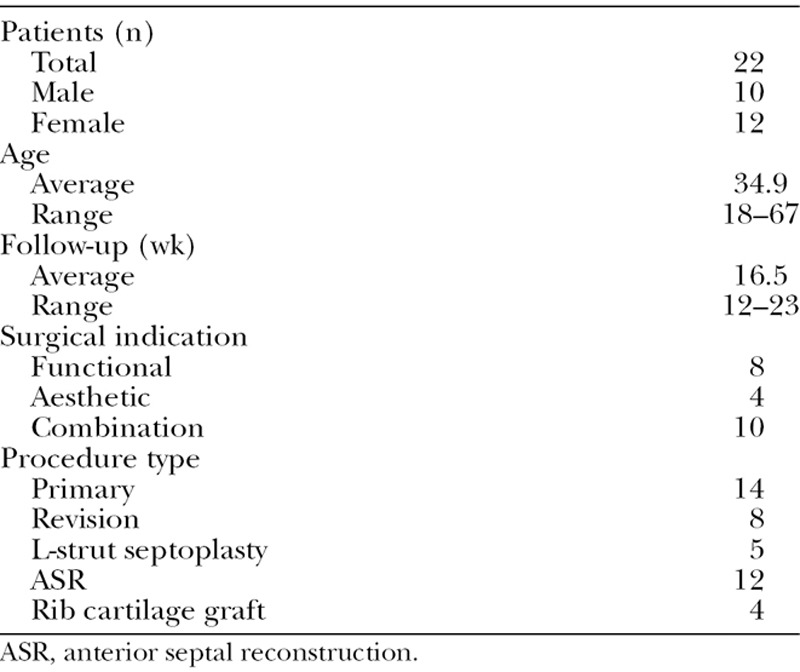
A total of 22 patients (10 males and 12 females) who met all inclusion criteria were enrolled in the study. Patient age ranged from 18 to 67 years, with an average age of 34.9 years. All patients were followed for a minimum of 3 months postoperatively. Follow-up time ranged from 12 to 23 weeks, with an average of 16.5 weeks. Of the 22 nasal surgeries, 8 (36.4%) were performed for functional indications, 4 (18.2%) for aesthetic indications, and 10 (45.5%) for a combination of functional and aesthetic indications. Seven patients (31.8%) had a documented history of prior nasal fracture/trauma. Septoplasty surgery was performed in 17 (77.3%) cases. Five (22.7%) were performed using L-strut septoplasty technique, and 12 (54.5%) were performed using a modified extracorporeal septoplasty technique (anterior septal reconstruction) as previously described by the senior author.8 Eight of the 22 surgeries (36.4%) were revision cases, that is, secondary septorhinoplasty patients who had initial nasal surgery performed elsewhere. Four patients (18.2%) underwent harvest of autologous rib cartilage for grafting purposes. There were no surgical complications identified in the study period. Patient data are summarized in Table 1.
Table 1.
Patient Data
Instrument Reliability and Validity Assessment
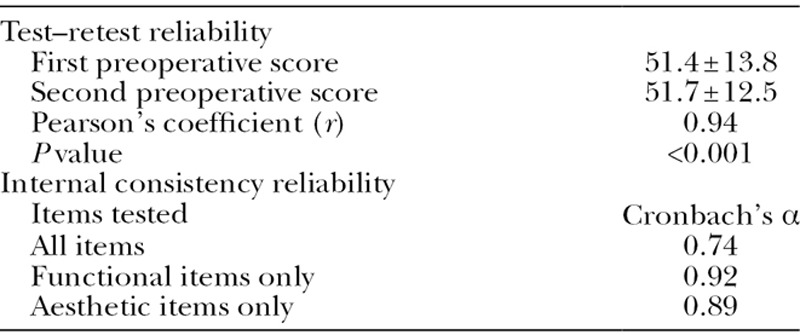
All 22 patients completed the test–retest reliability portion of the validation process. The average RHINO score was 51.4 ± 13.8 on the first preoperative evaluation and 51.7 ± 12.5 when repeated preoperatively on the day of surgery. Test–retest reliability was evaluated via Pearson’s correlation coefficient (r = 0.94; P < 0.001), with results indicating statistically significant reliability and reproducibility. Internal consistency reliability was assessed by calculating Cronbach’s α coefficient, with an α > 0.70 generally considered acceptable for instrument reliability.9 Analysis of internal consistency for the entire 10-item inventory demonstrated adequate internal consistency, with α = 0.74. When the functional and aesthetic items were assessed separately, α = 0.92 for the 5 functional items and α = 0.89 for the 5 aesthetic items. Reliability assessment results are summarized in Table 2.
Table 2.
Reliability Assessment
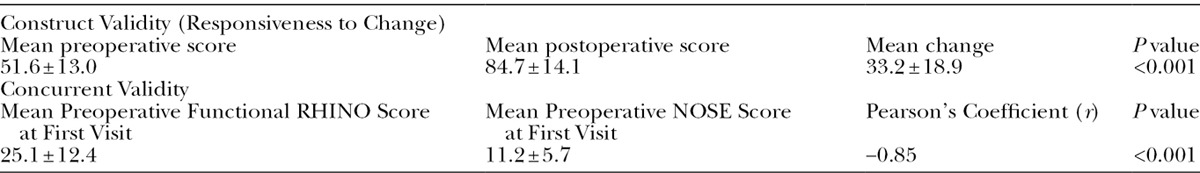
Construct validity was evaluated by calculating the responsiveness to change after nasal surgery. The mean preoperative averaged RHINO score was 51.6 ± 13.0 when compared with a mean postoperative RHINO score of 84.7 ± 14.1. The difference between preoperative and postoperative scores ranged from −1 to 61, with a mean difference of 33.2 ± 18.9. A paired samples t-test was performed comparing the averaged preoperative RHINO scores with the postoperative RHINO score, demonstrating a statistically significant increase in scores postoperatively (P < 0.001). To determine concurrent validity of the RHINO scale with the current gold standard NOSE scale, RHINO scores for the 5 functional items obtained at the first preoperative visit were cross-referenced with NOSE scores obtained at the same visit. Of the total 22 patients, 21 had preoperative NOSE and RHINO data available for data analysis. The mean preoperative functional RHINO score for the 21 patients was 25.1 ± 12.4, and the mean NOSE score was 11.2 ± 5.7. Pearson’s correlation coefficient demonstrated a statistically negative correlation (r = −0.85; P < 0.001) between RHINO and NOSE scores, indicating significant concurrent validity. As a point of additional clarification, the correlation coefficient was negative due to the fact that the RHINO and NOSE instruments were designed on inversely related scales, that is, high NOSE scores that indicate a high degree of nasal obstruction will correspond to low RHINO scores that indicate poor nasal function. Results are summarized in Table 3.
Table 3.
Validity Assessment
DISCUSSION
The aim of this study was to develop and validate a comprehensive QOL health instrument to assess patient satisfaction and outcomes after rhinoplasty. Currently, the gold standard QOL instrument for nasal surgery is the NOSE scale, as first described by Stewart et al.2 Notably, this instrument focuses on the assessment of nasal obstructive symptoms alone, and such its application is relatively limited with regard to surgery performed for primarily aesthetic or combined functional/aesthetic indications. The ROE scale is a complementary QOL instrument initially developed and validated by Alsarraf et al,3 with a focus on aesthetic outcomes after nasal surgery. In an analogous but reciprocal fashion to the NOSE scale, the ROE focuses solely on aesthetics to the exclusion of nasal functional evaluation. The NOSE scale has been much more widely adopted than the ROE instrument, though use of the ROE is increasingly as evidenced in several recent outcomes studies.10–12 As a consequence, we have much more data regarding outcomes with regard to function and little with regard to aesthetics. Likewise, we have even fewer examples of concurrent study of both. Our goal is to integrate nasal outcomes studies to include both domains, as both are acknowledged as of critical import in any type of rhinoplasty, functional or aesthetic.
The segregation of functional and aesthetic outcome assessment is a significant limitation to both the aforementioned QOL instruments. Decades of experience with rhinoplasty have demonstrated that the function and aesthetics of the nose are inseparably related.13 Aesthetic complaints, such as collapse or narrowing of the middle vault after a reductive rhinoplasty, will often present concurrently with functional nasal obstructive complaints. Similarly, functional correction of nasal valve compromise while simultaneously creating an aesthetically unacceptable appearance will almost universally result in poor patient satisfaction and by extension a poor outcome.
As such, a validated QOL instrument that comprehensively evaluates patient satisfaction with both nasal function and aesthetics is paramount to an adequate assessment of outcomes after rhinoplasty. As the limitations of objective measures of nasal function are well-documented, patient-reported outcome measures, that is, subjective QOL instruments, have become the current standard for outcome assessment in nasal surgery.1
Despite this, a recent review of the literature by Rhee et al14 demonstrated that only 14% of published functional rhinoplasty outcome studies involved the use of a validated patient-reported questionnaire. This inadequacy is equally manifest in the aesthetic rhinoplasty literature, as most outcome studies utilize qualitative assessments of either patient or physician satisfaction with surgical results.3 That there are so few outcomes studies that have utilized validated patient-reported outcome measures is interesting, in light of the fact that patient satisfaction is the primary goal in aesthetic surgery.3
In this study, we have developed and validated a unified scale assessing both functional and aesthetic patient-reported outcomes after rhinoplasty. This instrument demonstrated a high level of reliability and validity. Test–retest assessment showed significant reliability of scores when administered on separate days and in different settings, that is, in an outpatient clinic setting versus the preoperative holding area. The 10-item questionnaire was found to be internally consistent by Cronbach’s α, both when assessed as a whole and when assessed separately for the functional and aesthetic items. The RHINO scale was found to have appropriate construct and concurrent validity, as assessed by a statistically significant responsiveness to change and a high level of correlation between the functional item responses and the current gold standard, the NOSE scale.
The versatility of the RHINO scale becomes apparent when assessing patients in whom satisfaction with functional or aesthetic outcomes may be divergent from the overall satisfaction reported after surgery. In these patients, evaluating outcomes using a unidimensional functional or aesthetic QOL instrument may not correlate with the overall patient-reported outcome. As a case in point, this is exemplified in one patient in this study who expressed ambivalence regarding his surgical outcome (the sole patient in the study who reported a net negative change in his RHINO score after nasal surgery). His postoperative RHINO score was decreased by −1 compared with his preoperative average. Interestingly, when viewing the functional items in isolation, his score was slightly increased from a preoperative average of 26 to a postoperative score of 40. However, his aesthetic score decreased from a preoperative average of 27 to a postoperative score of 12. Overall, the patient related that his improvement in nasal obstruction was counterbalanced by his disappointment with his aesthetic appearance. Utilization of a unidimensional QOL instrument would not have revealed a comprehensive or accurate assessment regarding the patient’s overall self-reported outcome and satisfaction with surgery. This exemplifies why a unified functional and aesthetic scale is critical for the assessment of surgical outcomes after rhinoplasty.
One relative limitation of this study is the small sample size of patients enrolled. Fortunately, this did not meaningfully affect our validation analysis, as the reliability and validity of the RHINO scale was found to be quite robust by all statistical measures performed. Additionally, the current study’s sample size of 22 patients compares favorably to the standards set by previously published validations studies, including an n = 21 in the NOSE validation study and an n = 26 for the ROE validation study.2,3
In summary, this study reports the development and validation of a novel disease-specific QOL instrument pertaining to functional and aesthetic rhinoplasty. Statistical analyses in a sample of 22 patients demonstrate the RHINO scale to be both statistically reliable and valid in assessing patient-reported satisfaction with rhinoplasty outcomes, as assessed by test–retest reliability, internal consistency reliability, construct validity, and concurrent validity. The use of this statistically validated instrument is recommended for future studies evaluating outcomes after rhinoplasty.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Lam DJ, James KT, Weaver EM. Comparison of anatomic, physiological, and subjective measures of the nasal airway. Am J Rhinol. 2006;20:463–470. doi: 10.2500/ajr.2006.20.2940. [DOI] [PubMed] [Google Scholar]
- 2.Stewart MG, Witsell DL, Smith TL, et al. Development and validation of the Nasal Obstruction Symptom Evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004;130:157–163. doi: 10.1016/j.otohns.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 3.Alsarraf R, Larrabee WF, Jr, Anderson S, et al. Measuring cosmetic facial plastic surgery outcomes: a pilot study. Arch Facial Plast Surg. 2001;3:198–201. doi: 10.1001/archfaci.3.3.198. [DOI] [PubMed] [Google Scholar]
- 4.Most SP. Analysis of outcomes after functional rhinoplasty using a disease-specific quality-of-life instrument. Arch Facial Plast Surg. 2006;8:306–309. doi: 10.1001/archfaci.8.5.306. [DOI] [PubMed] [Google Scholar]
- 5.Rhee JS, Poetker DM, Smith TL, et al. Nasal valve surgery improves disease-specific quality of life. Laryngoscope. 2005;115:437–440. doi: 10.1097/01.mlg.0000157831.46250.ad. [DOI] [PubMed] [Google Scholar]
- 6.Lipan MJ, Most SP. Development of a severity classification system for subjective nasal obstruction. JAMA Facial Plast Surg. 2013;15:358–361. doi: 10.1001/jamafacial.2013.344. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Geneva: WHO; 1948. Constitution of the World Health Organization. [Google Scholar]
- 8.Surowitz J, Lee MK, Most SP. Anterior septal reconstruction for treatment of severe caudal septal deviation: clinical severity and outcomes. Otolaryngol Head Neck Surg. 2015;153:27–33. doi: 10.1177/0194599815582176. [DOI] [PubMed] [Google Scholar]
- 9.Lance CE, Butts MM, Michels LC. The sources of four commonly reported cutoff criteria: what did they really say? Organ Res Methods. 2006;9:202–220. [Google Scholar]
- 10.Ilhan AE, Saribas B, Caypinar B. Aesthetic and functional results of lateral crural repositioning. JAMA Facial Plast Surg. 2015;17:286–292. doi: 10.1001/jamafacial.2015.0590. [DOI] [PubMed] [Google Scholar]
- 11.Biggs TC, Fraser LR, Ward MJ, et al. Patient reported outcome measures in septorhinoplasty surgery. Ann R Coll Surg Engl. 2015;97:63–65. doi: 10.1308/003588414X14055925059075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrne M, Chan JC, O’Broin E. Perceptions and satisfaction of aesthetic outcome following secondary cleft rhinoplasty: evaluation by patients versus health professionals. J Craniomaxillofac Surg. 2014;42:1062–1070. doi: 10.1016/j.jcms.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Hahn S, Becker DG. What are some tips and pearls for preserving and improving nasal function when performing a cosmetic rhinoplasty? Curr Opin Otolaryngol Head Neck Surg. 2014;22:58–62. doi: 10.1097/MOO.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 14.Rhee JS, Daramola OO. No need to fear evidence-based medicine. Arch Facial Plast Surg. 2012;14:89–92. doi: 10.1001/archfacial.2011.1182. [DOI] [PubMed] [Google Scholar]


