Abstract
Coronary artery disease is common in patients with chronic obstructive pulmonary disease (COPD). Previous studies have shown that patients with COPD have a higher risk of mortality than those without COPD after coronary artery bypass grafting (CABG). However, most of the previous studies were small, single-center studies with limited case numbers (or their only focus was mortality). The aim of our study was to focus on readmission, acute myocardial infarction (AMI), acute respiratory failure (ARF), cerebrovascular accident, and venous thromboembolism rates after CABG in an Asian COPD population.
We conducted a nationwide case–control study in Taiwan using the claims database of hospitalization between January 1, 2009 and December 31, 2013. Patients with COPD before CABG were defined as the case groups. Each case was propensity score-matched by age, sex, hypertension, diabetes, dyslipidemia, cardiovascular disease, cerebrovascular disease, and chronic kidney disease, with 2 controls selected from CABG patients without COPD. The outcomes of interest were mortality, wound infection, and the readmission rate over 30 days for the following diseases: AMI, pneumonia, ARF, cerebrovascular accident, and venous thromboembolism.
There were 14,858 patients without COPD and 758 patients with COPD who underwent CABG. After propensity score matching, the 30-day mortality and 30-day readmission rates and AMI were higher in the non-COPD group. The incidences of pneumonia and ARF after CABG were higher in the COPD group.
Chronic obstructive pulmonary disease does not necessarily lead to mortality, readmission, or AMI after CABG, and the major respiratory complications associated with CABG in patients with COPD were pneumonia and ARF.
INTRODUCTION
Coronary artery disease is common in patients with chronic obstructive pulmonary disease (COPD) because these 2 conditions share smoking as a common risk factor. Previous studies have shown that patients with COPD who underwent coronary artery bypass grafting (CABG) had high morbidity and mortality rates.1–6 A prospective study enrolled patients with coronary artery disease who underwent CABG between 1992 and 2001,7 and found that patients with only COPD had a higher mortality rate than those with no comorbidities, and COPD patients with more than 1 comorbidity had the worst prognosis. Another study documented a high mortality rate in patients with COPD who underwent CABG, especially those older than 75 years with severe COPD and receiving steroids.8 However, these studies had some limitations, including focusing on the prognosis of mortality without investigating the postoperative complications, studies performed at a single center with limited case numbers without an Asian population, and the fact that many studies were published more than 20 years ago. The advancements in surgery and anesthesia over the past decade have had a significant impact on the outcome; however, the postoperative complication rate associated with CABG in Asian patients with COPD remains unknown. To resolve this important issue, we conducted a nationwide study on the mortality rates in various time periods and for postoperative complications in these patients.
METHODS
Data Source
The Taiwan National Health Insurance Research Database (NHIRD) was used in this study. The NHIRD is a claim database based on Taiwan's National Health Insurance program, which covers 99% of the population. The NHIRD contains all registered inpatient and outpatient medical records based on the medical expenditure applications and the clinical modification of the International Classifications of Disease-9 (ICD-9-CM). To avoid the possibility of ethical violations, personal identifications were encrypted to secure the confidentiality of the individuals. The study was approved by an institutional review board of Chi Mei Medical Center (10412-E01).
Study Subjects
The study included patients older than 40 years who underwent CABG (ICD-9-CM code of surgical procedures: 36.1 and 36.2) between January 1, 2009 and December 31, 2013. Those with a discharge diagnosis of COPD (ICD-9-CM: 490–492, 496) within 1 year before CABG were defined as the case groups. Those with a history of cancer (ICD-9-CM: 140–208) with a catastrophic illness card before CABG were excluded. Each case was propensity score-matched by age, sex, hypertension, diabetes, dyslipidemia, cardiovascular disease (CVD), cerebrovascular accident (CVA), and chronic kidney disease (CKD). Two controls were selected from CABG patients without COPD. Comorbidities, such as hypertension, diabetes, dyslipidemia, CVD (extracardiac vascular disease included carotid artery disease and peripheral vascular disease and excluded heart valve disease), CVA (cerebrovascular disease included subarachnoid hemorrhage, intracerebral hemorrhage, unspecified intracranial hemorrhage, stenosis of the precerebral arteries, occlusion of the cerebral arteries, transient cerebral ischemia, late effects of cerebrovascular disease, and conditions caused by problems that affect the circulation of blood to the brain), and CKD were evaluated within 1 year before the day of surgery. The outcomes of interest in this study were mortality, infection (wound infection included deep and superficial sternal wound infection and saphenous vein harvest wounds), and readmission within 30 days postoperatively for the following diseases: acute myocardial infarction (AMI; ICD-9-CM: 410), pneumonia (ICD-9-CM: 480–488), acute respiratory failure (ARF; ICD-9-CM: 518.5, 518.81, 518.82, and 518.84), and CVA. Patients with deep vein thrombosis (ICD-9-CM: 453.4 and 451.8) and pulmonary embolism (ICD-9-CM: 415.1) were also considered. All of the study subjects were followed up until the occurrence of the aforementioned outcomes or until the end of the study (December 31, 2013).
Statistical Analysis
Pearson chi-square test or Fisher exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables were used to compare the differences between the CABG patients with/without COPD. The conditional logistic regression model was applied to estimate the odds ratio of death adjusted for potential risk factors. A P value <0.05 was set as statistically significant. All of the analyses were performed using Statistical Analysis System statistical software (version 9.4; SAS Institute, Inc., Cary, NC).
RESULTS
There were 14,858 patients without COPD (males 76%) and 706 with COPD (males 87%) who underwent CABG. The age distribution differed between these 2 groups. Approximately one-third of the patients without COPD were 60–69 years old, and one-third were older than 70 years, compared with 24% (60-69 years) and 65% (70 years) of the patients with COPD (Table 1).
TABLE 1.
Demographic Analysis of COPD and Non-COPD Patients With CABG Between 2009 and 2013
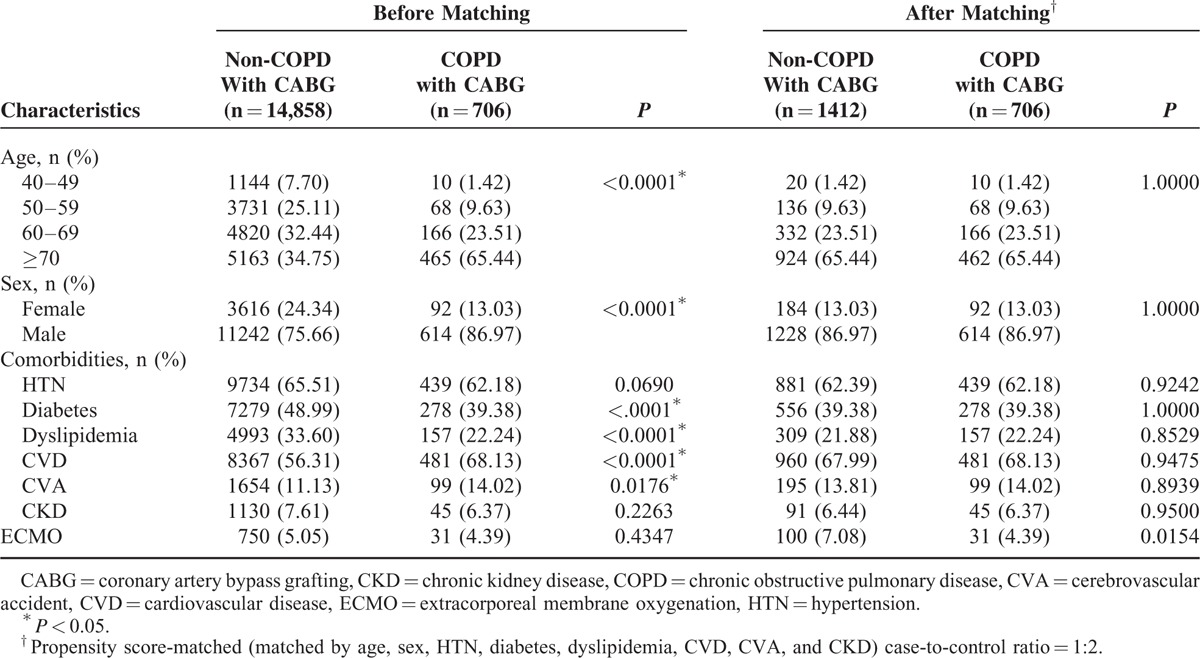
In the non-COPD group, hypertension was the most prevalent comorbidity (66%), followed by CVD, diabetes, dyslipidemia, and CVA. In the COPD group, CVD was the most prevalent comorbidity (68%), followed by hypertension, diabetes, dyslipidemia, and CVA.
The main complications in COPD and non-COPD patients after CABG before and after propensity score matching are shown in Table 2. Before matching, the length of stay was longer in patients with COPD than in those without COPD (patients with COPD had a median of 20 days). Compared with patients without COPD, those with COPD had a higher mortality rate at 365 days; however, there was no difference at 30 or 90 days. The wound infection rates were also similar between these 2 groups. The 30-day readmission rate before matching and reasons for readmission, including AMI, pneumonia, ARF, and CVA, were higher in the COPD group than in the non-COPD group.
TABLE 2.
Main Complications of COPD and Non-COPD Patients Undergoing CABG, Before and After Propensity Score Matching
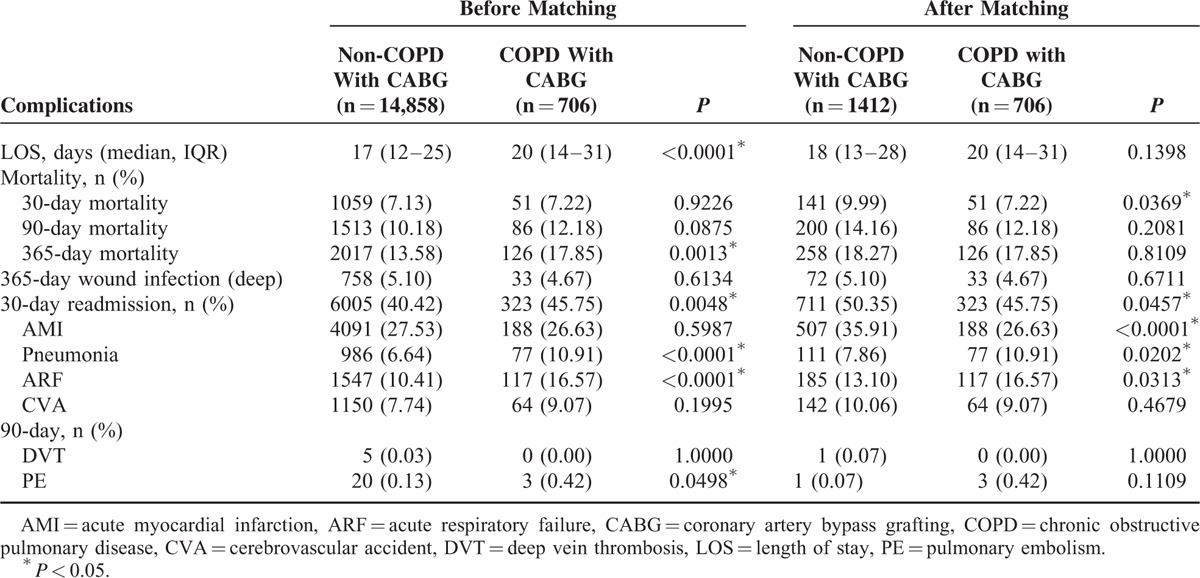
After propensity score matching by age, sex, hypertension, diabetes, dyslipidemia, CVD, CVA, and CKD, the 30-day mortality and 30-day hospital readmission rates were higher in the non-COPD group than in the COPD group. AMI was the most common reason for 30-day readmission after CABG (35.91%). There were a few cases of pulmonary embolism in these 2 groups.
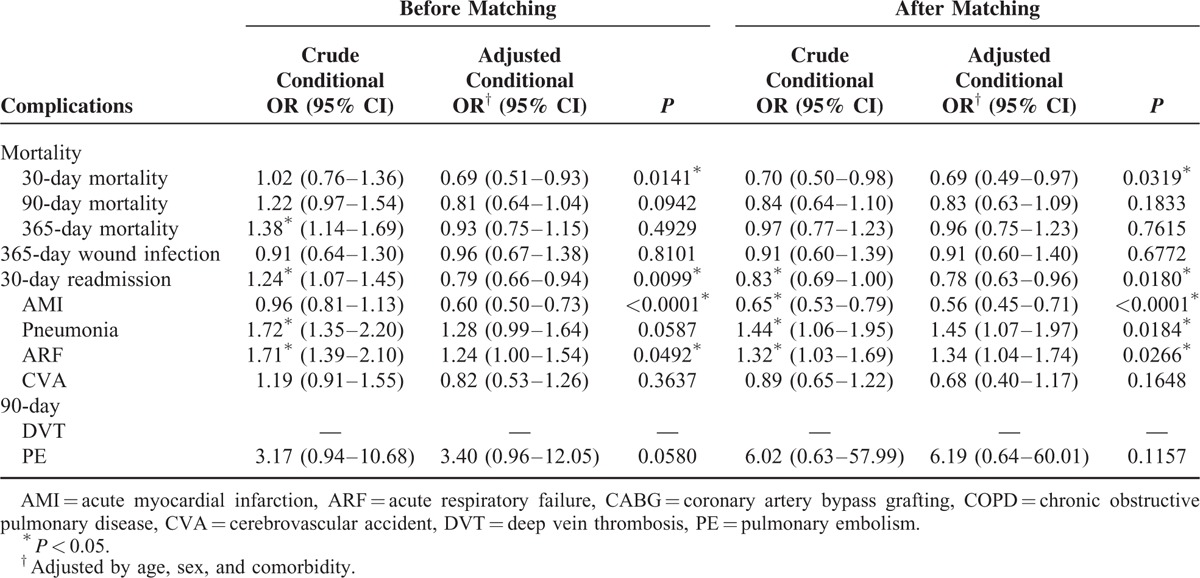
Table 3 shows the conditional odds ratios for the majority of the complications within each group. After matching, the patients with COPD had 45% and 34% increased risks for pneumonia and ARF, respectively, after CABG, compared with patients without COPD.
TABLE 3.
The Conditional ODDS Ratio of Majority Complications Within COPD and Non-COPD Patients Undergoing CABG
DISCUSSION
This first-ever national survey of CABG showed that patients with COPD had lower 30-day readmission, mortality, and AMI rates compared with those without COPD. However, the rates for pneumonia and ARF after CABG were higher in the COPD groups.
Comorbidities in Patients Undergoing CABG
In our study, the most common comorbidity was hypertension in patients undergoing CABG, and no statistically significant differences were found between the COPD and non-COPD groups. Diabetes and dyslipidemia were higher in the non-COPD than the COPD group, whereas the cardiovascular and cerebrovascular disease rates were higher in the COPD group. A previous multicenter and regional database study7 showed that among CABG patients who had COPD and other comorbidities, vascular disease was the most prevalent comorbid condition (48.1%) followed by diabetes (47.2%). In our study, the COPD patients had a higher prevalence of CVD. COPD and CVD shared the risk factor of smoking, and COPD is a chronic systemic inflammatory disease that results in atherosclerosis. However, there was no clear definition of vascular disease in the previous study, and individually determining the prevalence of hypertension, CVD, and CVA was difficult.
Mortality in CABG Patients With COPD
In our study, CABG patients with COPD had lower 30-day mortality, readmission, and AMI rates; this was also observed in another study.9 Having COPD did not necessarily predict a poor outcome for patients undergoing CABG. Therefore, COPD should not preclude undergoing CABG surgery based on the current study. Intensive pulmonary rehabilitation after operation and effective drug therapy for COPD may improve outcome after CABG in patients with COPD.
In our study, the 30-day mortality rate in patients with COPD undergoing CABG was 7.23%. Bruce et al7 reported a 7.2% annual incidence of death. Medalio et al10 reported 37 patients with COPD and higher rates of readmission in the COPD group, with a 4% annual incidence of death after 8.6 years of follow-up. DeRose et al evaluated 544 patients with an ejection fraction of less than 25% who underwent CABG and 122 patients with COPD in a study group. The 30-day mortality rate in these patients with congestive heart failure was 5.5%. The study was performed at a single hospital from 1992 to 2002, and focused on long-term (5 and 10-year) survival rates.11 We enrolled 14,858 patients undergoing CABG and 706 patients with COPD, and documented a short survival and postoperative complications, including wound infection, readmission, AMI, pneumonia, ARF, CVA, deep vein thrombosis, and pulmonary embolism.
A previous study enrolled 832 patients who underwent CABG between 1995 and 1996. Risk factors for 5-year mortality were preoperative renal impairment, diabetes, congestive heart failure, COPD, and old age.12 Another single-center retrospective study of 221 patients with COPD who underwent CABG between 1998 and 2003 revealed that these patients had a slightly longer hospital stay than controls. Pulmonary infections were more frequent in patients with severe COPD compared with those with mild to moderate COPD, and none of the patients with COPD who underwent CABG died 30 days postoperatively.9
Whether the mortality is associated with CABG remains controversial. A Danish database study reported that the 30-day mortality rate after CABG surgery has greatly improved over the past decade; however, the 1-year mortality rate remained constant.13 In our study, the 30-day mortality rate was lower in patients with COPD after CABG than the control group. This protective effect may be due to surgery being performed after the stabilization of the patient's general conditions. Furthermore, a COPD diagnosis may have influenced the behavior of the surgeon to minimize complications or perform the surgery under favorable conditions. In our study, a preoperative diagnosis of COPD did not seem to place the patient at considerable risk during CABG.
Pneumonia and ARF in CABG Patients With COPD
Similar to the previous study,9 our study showed that patients with COPD had a higher incidence of pneumonia than CABG complications. Although no statistically significant differences were found for the length of hospital stay between the 2 groups, patients with COPD tended to have a longer hospital stay. Additionally, COPD had a significant effect on ARF after CABG surgery. Compared with patients without COPD, those with COPD had a 34% increased incidence of ARF. The immune system may be weakened in patients with COPD due to airway inflammation, obstruction, the destruction of epithelium, and the loss of defensive abilities. The respiratory complications of pneumonia and ARF were higher after CABG in the COPD group compared with the non-COPD group in our study.
Thromboembolism in CABG Patients With COPD
The risk of thromboembolism increases after surgery, especially orthopedic surgery, and the prognosis is poor if thromboembolism occurs after surgery.14 Previous studies reported a high prevalence of venous thromboembolism in patients with COPD, including an acute exacerbation.15 Deep vein thrombosis and pulmonary embolism were less common in Asian patients with COPD or patients who underwent orthopedic surgery.16,17 Patients with COPD have a higher incidence of deep vein thrombosis and pulmonary embolism17; however, these incidences were very low in patients with COPD undergoing CABG in our study, and there was no significant difference in the rate of thromboembolism after CABG between the COPD and non-COPD groups. The unfractionated heparin and low-molecular-weight heparin were discontinued before operation. In our study, patients with deep vein thrombosis or pulmonary embolism did not receive extracorporeal circulation. In this study, we demonstrated a low incidence of deep vein thrombosis and pulmonary embolism in Asian COPD patients after CABG, and the bleeding tendency in the Asian population indicates that the surgeon should more strongly consider anticoagulant or antiplatelet treatments before surgery.
Savas Oz et al18 showed that moderate-risk patients with COPD who received inhaled bronchodilator and steroid treatment for 10 days before CABG had improved outcomes and reduced adverse events and complications. Therefore, in patients with COPD receiving CABG, they recommend the use of preoperation treatment. This treatment would decrease the lengths of intensive care unit stay, hospital stay, and inotropic support. In our study population, patients with COPD maintain their regular medical treatment (including bronchodilator inhalation). This may lead to better outcomes in COPD patients. In accordance with Bilgehan et al, we thought that a multidimensional approach including preoperative medical treatment and pulmonary rehabilitation after surgery should improve postoperative outcomes.
Limitations
The results of the current study highlight the research gap in assessing complications after CABG in Asian patients with COPD. This study has some limitations. First, pulmonary function tests and laboratory data were not available in the database. Therefore, the accuracy of the diagnosis and classification of COPD may be criticized. The ICD-9-CM codes for COPD diagnosis have been widely used in other studies and demonstrate the coding validity.19–21 Second, there is no ejection fraction assessment (heart function), and the severity of coronary artery disease also cannot be evaluated. The association between disease severity and complications is also lacking. We only show a relationship between CABG and COPD in a nationwide database. Third, we do not have information on medication adherence; this key factor may associate with postoperative complications. We believe that the large number of patients with CABG drawn from the NHIRD and the complete patient enrollment provide representative results.
CONCLUSIONS
The mortality, readmission, and AMI rates were not higher in patients with COPD after CABG than those without COPD. The risk of deep vein thrombosis and pulmonary embolism was also very low in the Asian CABG patients with COPD, and this risk was not significantly different from those without COPD. Respiratory complications associated with CABG may lead to deleterious consequences. To improve the outcome after CABG in patients with COPD, we must understand the underlying cause of the respiratory disease and devise early prevention strategies.
Footnotes
Abbreviations: AMI = acute myocardial infarction, ARF = acute respiratory failure, CABG = coronary artery bypass grafting, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVA = cerebrovascular accident, CVD = cardiovascular disease, HR = hazard ratio, ICD-9-CM = International Classifications of Disease, Ninth Revision, Clinical Modification, NHI = National Health Insurance, NHIRD = National Health Insurance Research Database.
Conflicts of interest: There are no conflicts interest.
REFERENCES
- 1.Grover FL, Hammermeister KE, Burchfiel C. Initial report of the Veterans Administration Preoperative Risk Assessment Study for Cardiac Surgery. Ann Thorac Surg 1990; 50:12–26. [DOI] [PubMed] [Google Scholar]
- 2.Higgins TL, Estafanous FG, Loop FD, et al. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA 1992; 267:2344–2348. [PubMed] [Google Scholar]
- 3.Grover FL, Johnson RR, Marshall G, et al. Factors predictive of operative mortality among coronary artery bypass subsets. Ann Thorac Surg 1993; 56:1296–1306. [DOI] [PubMed] [Google Scholar]
- 4.Durand M, Combes P, Eisele JH, et al. Pulmonary function tests predict outcome after cardiac surgery. Acta Anaesthesiol Belg 1993; 44:17–23. [PubMed] [Google Scholar]
- 5.Kurki TS, Kataja M. Preoperative prediction of postoperative morbidity in coronary artery bypass grafting. Ann Thorac Surg 1996; 61:1740–1745. [DOI] [PubMed] [Google Scholar]
- 6.Samuels LE, Kaufman MS, Morris RJ, et al. Coronary artery bypass grafting in patients with COPD. Chest 1998; 113:878–882. [DOI] [PubMed] [Google Scholar]
- 7.Bruce JL, Cathy SR, Brian Spence, et al. Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation 2006; 114:I-430–I-434. [DOI] [PubMed] [Google Scholar]
- 8.Louis ES, Marla SK, Rohinton J. Morris, et al. Coronary artery bypass grafting in patients with COPD. Chest 1998; 113:878–882. [DOI] [PubMed] [Google Scholar]
- 9.Manganas H, Lacasse Y, Bourgeois S, et al. Postoperative outcome after coronary artery bypass grafting in chronic obstructive pulmonary disease. Can Respir J 2007; 14:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medalion B, Katz MG, Cohen AJ, et al. Long-term beneficial effect of coronary artery bypass grafting in patients with COPD. Chest 2004; 125:56–62. [DOI] [PubMed] [Google Scholar]
- 11.DeRose JJ, Jr, Toumpoulis IK, Balaram SK, et al. Preoperative prediction of long-term survival after coronary artery bypass grafting in patients with low left ventricular ejection fraction. J Thorac Cardiovasc Surg 2005; 129:314–321. [DOI] [PubMed] [Google Scholar]
- 12.van Domburg RT, Takkenberg JJ, van Herwerden LA, et al. Short-term and 5-year outcome after primary isolated coronary artery bypass graft surgery: results of risk stratification in a bilocation center. Eur J Cardiothorac Surg 2002; 21:733–740. [DOI] [PubMed] [Google Scholar]
- 13.Jan Jesper A, Laura Sommer H, Vibeke Elisabeth H, et al. 30-day mortality after coronary artery bypass grafting and valve surgery has greatly improved over the last decade, but the 1-year mortality remains constant. Ann Cardiac Anaesth 2015; 18:138–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clive K. Natural history of venous thromboembolism. Circulation 2003; 107:I-22–I-130. [DOI] [PubMed] [Google Scholar]
- 15.Gunen H, Gulbas G, In E, et al. Venous thromboemboli and exacerbations of COPD. Eur Respir J 2010; 35:1243–1248. [DOI] [PubMed] [Google Scholar]
- 16.Lee WS, Kim KI, Lee HJ, et al. The incidence of pulmonary embolism and deep vein thrombosis after knee arthroplasty in Asians remains low: a meta-analysis. Clin Orthop Relat Res 2013; 471:1523–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen CY, Liao KM. The Incidence of deep vein thrombosis in Asian patients with chronic obstructive pulmonary disease. Medicine (Baltimore) 2015; 94:e1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savas Oz B, Kaya E, Arslan G, et al. Pre-treatment before coronary artery bypass surgery improves post-operative outcomes in moderate chronic obstructive pulmonary disease patients. Cardiovasc J Afr 2013; 24:184–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liao KM, Lin WC, Lin TC, et al. Disease severity at the first hospitalization as a predictor for mechanical ventilation dependency in elderly patients with chronic obstructive pulmonary disease. Tohoku J Exp Med 2014; 234:263–269. [DOI] [PubMed] [Google Scholar]
- 20.Wang MT, Lo YW, Tsai CL, et al. Statin use and risk of COPD exacerbation requiring hospitalization. Am J Med 2012; 126:598–606. [DOI] [PubMed] [Google Scholar]
- 21.Wang MT, Tsai CL, Lo YW, et al. Risk of stroke associated with inhaled ipratropium bromide in chronic obstructive pulmonary disease: a population-based nested case-control study. Int J Cardiol 2012; 158:279–284. [DOI] [PubMed] [Google Scholar]


