Abstract
Purpose
Understanding how resources are used provides guidance to disseminating effective interventions. Here, we report data on implementation resources needed for the Rural Breast Cancer Survivors (RBCS) study that tested a telephone-delivered psychoeducational education and support intervention to survivors in rural Florida. Intervention resources included interventionists’ time on one intake assessment (IA) call, 3 education calls (ED), one follow-up education call (FUE), 6 support (SUP) calls, and documentation time per survivor.
Methods
Interventionists logged start and end times of each type of call. Average interventionist time in minutes was calculated by call type. Associations between interventionists’ time and participants’ characteristics including age, race/ethnicity, time since treatment, cancer treatment, depressive symptoms, education, income, employment, and support, was assessed using linear mixed models with repeated measures.
Results
Among 328 survivors, IA calls lasted 66.9 minutes (SD 21.7); ED lasted 50.6 (SD 16.7), 48.1 (SD 15.9), and 39.6 (SD 14.8); FUE lasted 24.7 (SD 14.8); and SUP 42.8 (SD 29.6) minutes. Documentation time was 18.4 minutes for IA, 23-27 for ED, 12.3 for FUE, and 23.0 for SUP.
Conclusion
Interventionists spent significantly more time with participants with depressive symptoms, who already used other support, and who received SUP calls before the ED vs. after. There were no significant differences by time since or type of cancer treatment, or other personal characteristics.
Implications for Cancer Survivors
Resources vary by survivor characteristics. Careful consideration of mental health status or support available is warranted for planning implementation and dissemination of effective survivorship interventions on a broad scale.
Keywords: implementation costs, dissemination and implementation, cancer disparities, rural breast cancer survivors, survivorship
PURPOSE
Dissemination and implementation scientists promote the adaptation of experimentally-tested and effective interventions for use with a broader population [1]. While increasing numbers of effective interventions are available, there is a lack of studies evaluating reach, adoption and implementation in clinical settings. In particular, few investigators report the resources needed for implementing survivorship interventions and consequently, the implementation costs. This information is fundamental to disseminate effective interventions. Mandelblatt and colleagues were among the first investigators to document intervention costs, specifically costs involved in the Moving Beyond Cancer (MBC) study that was a psychosocial and behavioral intervention in cancer survivorship [2, 3]. The MBC intervention costs ranged from $11.3 per person for printed materials to $134 per person for cancer education counseling interventions [2]. This study is one of the few papers reporting implementation costs of psychosocial or behavioral interventions.
Additional attention to research that determines resources and costs associated with implementing effective interventions is urgently needed [4, 5]. In addition, for strategic planning, it is fundamental that the variation in costs relative to the specific needs of the targeted populations is also examined. For example, implementation costs of support interventions may be greater for survivors who are recently diagnosed compared to long-term survivors who may have overcome some early survivorship challenges. Similarly, survivors in need of mental health support may require more intervention resources compared to those who do not have this need. A clear understanding of variation is valuable for those entities planning implementation of survivorship interventions because implementation costs can be accurately estimated based on the characteristics of the populations served.
One survivorship intervention having potential for broad dissemination is the Breast Cancer Education Study (BCEi). This randomized trial showed the effectiveness of a psychoeducational intervention in improving quality of life outcomes among early stage breast cancer survivors [6]. The BCEi was based on a breast cancer survivorship care model emphasizing patient-centered care through education and support for self-management of treatment effects, psychosocial concerns, cancer surveillance, and family, work, and insurance challenges [6]. The program was cited in a 2012 Cochrane database review as the single behavioral intervention that combined education and support to improve patient-reported outcomes among breast cancer survivors [7]. The BCEi was later evaluated by an expert panel of the Research-Tested Intervention Programs at the National Cancer Institute. The RTIPs panel evaluated the BCEi using RE-AIM principles [8] and judged the program as an effective, evidence-based intervention with high dissemination capability. Building on this evidence, the authors sought to extend reach to a broad population of rural underserved breast cancer survivors [9]. They modified the BCEi intervention delivery using telephone instead of face to face contact. The telephone-based intervention was called the Rural Breast Cancer Survivors Intervention (RBCS).
To examine the RBCS implementation resource utilization and variation, we collected time data documenting the interventionists’ time in minutes spent in delivering the intervention to the survivors. The time included the intake assessment, education calls, follow-up education call, support calls, and the related intervention activities such contacting survivors and documenting the interventions. The time spent by interventionists was the primary intervention resource in the RBCS study and thus, it was the major cost associated with implementing the intervention. Furthermore, we hypothesized that the time spent by the interventionists with survivors would vary depending on several factors such as time since the end of primary treatment, type of treatment late effects, and the mental status of the survivors.
METHODS
This study was approved by the Institutional Review Boards of the University of Alabama at Birmingham and the Florida Department of Health. The present study consisted of data collected on the time spent by RBCS interventionists on intervention activities.
Participants
Eligibility criteria included women diagnosed with Stage 0-III breast cancer, living in rural Florida, within the first three years following completion of primary breast cancer treatment, at least 21 years of age, and with telephone or cellphone access. Rural eligibility was based on two criteria: residence in one of 33 Florida rural counties designated by Florida statute [10] or residence in a rural pocket of one of 34 Florida urban with an Index of Research Access (IRA) score equal to or greater than 4 [11]. The IRA score was used because it provided a granular determination of rurality that is not obtained by county residence alone [11].
Recruitment consisted of approved use of the State of Florida Cancer Registry Data combined with active recruitment strategies [12]. Breast cancer survivors (BCS) received no more than three contacts through two letters of invitation and telephone call. Survivors responded via mail or telephone call to our toll-free land line. Survivors who agreed to participate via telephone subsequently provided written informed consent. A research staff called survivors to schedule an intake within one week after receipt of informed consent. The recruitment goal for the primary RBCS study was 432 BCS. The present analysis included 328 participants for whom the main outcome (interventionists’ time) was collected.
RBCS Intervention
The RBCS was designed for twelve months of study participation with random assignment to either the Early Education and Support Intervention or the Delayed Education and Support Intervention group. The four components of the RBCS intervention included one intake assessment (IA); three education calls (ED); one follow-up education call (FUE); and six support calls (SUP). Supplemental written RBCS print materials consisting of a 140 page Education Manual and 38 Tip sheets enhanced teaching and learning activities. The two groups differed in the timing of the three ED with Early Education group receiving ED in Month 1, and the Delayed Education group receiving ED in Month 7.
The IA established telephone contact with participants to get to know them and allow for the collection of baseline data. The three education calls were framed within a quality of life model. In ED #1, the interventionists discussed physical effects of treatment including cancer-related fatigue, lymphedema, pain, and menopausal symptoms. In ED #2, the interventionists discussed ways to promote healthy lifestyle behaviors of physical activity and healthy nutrition; changes in family and social relationships; and work, financial, and/or insurance challenges. In ED #3, the interventionists explored psychological late effects including anxiety and depression, fear of recurrence, and spiritual changes. The FUE was designed to evaluate participants’ learning of survivorship instruction and reinforcement for follow through on cancer surveillance activities, health and wellness activities, and symptom management. The fourth component was support calls (SUP) that were scheduled between intervention and data collection calls to “check in” with participants in a more unstructured format.
The RBCS interventionists consisted of two full-time research nurses who were new to cancer care, and two part-time research nurses having a combined total of 50 years of cancer care experience. The educational level of the research nurses varied; two had master’s degrees, one had a baccalaureate degree, and one had a diploma in nursing. The interventionists received two days of training in cancer survivorship, rural and health disparities, telephone intervention delivery and intervention fidelity. Training methods included didactic instruction, role playing, and intensive review of the RBCS Policies & Procedures Training Manual. The interventionists participated in weekly RBCS meetings to discuss issues and/or challenges that arose during the interventions and to review weekly enrollment and retention data. Three research nurses remained in the RBCS study over the five year period; one research nurse participated for three and a half years of the study period.
Main Outcome
Interventionists’ time was defined as the number of minutes spent in the IA and ED participant calls and documentation of the interaction. The interventionists recorded the time spent with participants using digital technology that allowed determination of the precise number of minutes spent on telephone calls. Interventionist time was collected using the Cost of Intervention Survey-3, an instrument developed by the investigators specifically to log in the time spent on the various implementation activities. The interventionists used this survey to log start and end times of the intake assessment, education calls, follow up education, and time for documentation. To address reliability of the intervention, two research staff who independently listened to the digital tapes and used a checklist to document whether the ED calls covered the topics. We further examined areas of agreement between the research staff for both the presentation of the intervention and participants’ responses.
Participant Data
Data from participants were collected at baseline and at 3-month intervals for a total of five data collection time points over the 12 month study participation. Data used in this study were from the baseline assessment and included:
Survivor characteristics and cancer treatment variables collected using the Sociodemographic and Treatment tool that has been used in prior work by the investigators [9];
Depressive symptoms collected using the Center for Epidemiologic Studies of Depression (CES-D) [13], a widely used short self-report scale that was designed to measure depressive symptoms in the general population. Total score ranges from 0 to 60, where higher scores indicate higher depressive symptomatology. Scores ≥ 16 suggest clinically significant levels of psychological distress. In the present study, the CES-D had Cronbach alpha reliability of .91.
Income, employment and health insurance collected using the Work Finances Inventory (WFI), a descriptive 46-item survey used in prior work by the investigators [14, 15] that was adapted and modified from Given et al [16].
Social support data were collected using the Medical Outcomes Study - Social Support Survey, a 19-item survey used to assess dimensions of social support [17]. The MOS-SSS contains four functional support subscales (i.e., emotional/informational, tangible, affectionate, and positive social interaction) and an overall functional social support index. The MOS-SSS scores range from 0 to 100, where higher scores indicate higher levels of perceived social support. In the present study at baseline, the MOS-SSS overall functional social support index had alpha reliability of .96.
ANALYSIS
Average Interventionist time in minutes was calculated by the type of call. Descriptive statistics for other survivor variables were also computed at baseline. We determined the association between interventionist time and participant characteristics including age, race/ethnicity, marital status, time since diagnosis, cancer treatment, depressive symptoms (CES-D score ≥ 16), education, income, employment, and support using linear mixed models with repeated measures.
The mixed model approach allows incorporation of a covariance structure to account for dependence among repeated measures on the same individuals. In the presence of missing data (29% attrition at 12 months), mixed models provide unbiased estimates of parameter estimates, provided that the missing data are missing at random.
An initial full model with all participant baseline characteristics of interest was fitted and in an effort to identify the covariates most strongly associated to the outcome, a reduced model was obtained using likelihood ratio tests sequentially to trim the initial full model to include only the characteristics associated with the interventionist time at the 0.01 significance level. Furthermore, due to an association of the risk of drop-out with baseline levels of self-reported mental health [18] the impact of the missing data was further mitigated by including baseline CES-D scores (as a proxy of mental health) as a covariate in the models. From the reduced model, we then obtained the least square means of interventionists’ time for each type of call and by relevant predictors. We examined more closely the effect of social support on the reduced model using an overall index of social support obtained from the Medical Outcomes Study Social Support Survey (MOS-SSS) [19], a 20-item instrument designed to measure aspects of social support in chronically ill patients also applicable to other populations. The overall index can range from 0 to 100, with higher scores indicating more perceived social support. We included the baseline MOS-SSS in the reduced model as an additional predictor and examined its relevance as well as whether it caused changes in the other model parameters. The analyses were conducted using SAS [20].
RESULTS
Table 1 shows the socio-demographic characteristics and cancer treatment variables of the 328 RBCS participants included in this analysis. There were no significant differences between the two study groups with respect to age, marital status, education, employment or family income. About 48.8% were at 65 years or older, 72.9% were married or partnered, 5% with high school or less education, 46% retired, 16% had income ≤$20,000, and about 25% had depressive symptoms (CES-D ≥ 16). Furthermore, there were no significant differences between the groups with respect to type of surgery, chemotherapy, radiation therapy, or hormonal therapy. In general, the participants received standard breast cancer treatment with the majority receiving lumpectomy and radiation therapy for control of local disease, and chemotherapy for control of regional systemic disease. About 58% received chemotherapy, 70.7% received radiation, and 66% received hormone blocking agents.
Table 1. Sociodemographic & Treatment Characteristics.
| Characteristic | Delayed Education (n=166) n (%) |
Early Education (n=162) n (%) |
P |
|---|---|---|---|
| Age groups | 0.676 | ||
| 35-45 | 6 (3.6) | 5 (3.1) | |
| 46-64 | 83 (50) | 74 (45.7) | |
| 65-90 | 77 (46.4) | 83 (51.2) | |
|
| |||
| Marital status | 0.535 | ||
| Never married | 5 ( 3) | 2 (1.2) | |
| Married or living w/ partner | 118 (71.1) | 121 (74.7) | |
| Separated / divorced/ widowed | 43 (25.9) | 39 (24.1) | |
|
| |||
| Minority | 6 (3.6) | 11 (6.8) | 0.195 |
|
| |||
| Education | 0.739 | ||
| < High school | 9 (5.4) | 7 (4.3) | |
| High school grad. | 32 (19.3) | 41 (25.3) | |
| Technical school /some college | 55 (33.1) | 52 (32.1) | |
| Completed college | 47 (28.3) | 40 (24.7) | |
| Postgraduate | 23 (13.9) | 22 (13.6) | |
|
| |||
| Employment status | 0.406 | ||
| Full-time | 47 (28.3) | 36 (22.2) | |
| Part-time | 19 (11.4) | 27 (16.7) | |
| Retired | 76 (45.8) | 76 (46.9) | |
| Homemaker | 11 (6.6) | 7 (4.3) | |
| Other | 13 (7.8) | 16 (9.9) | |
|
| |||
| Family income | 0.821 | ||
| $20,000 or less | 27 (16.3) | 28 (17.3) | |
| $20,001 to $30,000 | 23 (13.9) | 22 (13.6) | |
| $30,001 to $40,000 | 13 (7.8) | 10 (6.2) | |
| $40,001 to $50,000 | 18 (10.8) | 19 (11.7) | |
| Greater than $50,000 | 67 (40.4) | 58 (35.8) | |
| Declined to answer | 18 (10.8) | 25 (15.4) | |
|
| |||
| Health insurance | 157 (94.6) | 155 (95.7) | 0.644 |
|
| |||
| Months since end of treatment a | 0.260 | ||
| <=12 | 44 (27.2) | 35 (22.2) | |
| 13-24 | 89 (54.9) | 101 (63.9) | |
| 25+ | 29 (17.9) | 22 (13.9) | |
|
| |||
| Hormonal therapy b | 110 (66.3) | 109 (67.3) | 0.845 |
|
| |||
| Treatment mix | 0.930 | ||
| Surgery only | 20 ( 12) | 22 (13.6) | |
| Surgery, chemotherapy | 26 (15.7) | 28 (17.3) | |
| Surgery, radiation | 50 (30.1) | 45 (27.8) | |
| Surgery, chemo, radiation | 70 (42.2) | 67 (41.4) | |
|
| |||
| Depressive symptoms c | 45 (27.1) | 35 (21.6) | 0.245 |
|
| |||
| Support servicesd | 30 (18.1) | 35 (21.6) | 0.422 |
n=8 women did not provide end of treatment date;
On hormonal treatment at the time the data were collected;
CES-D scores ≥ 16;
Cancer support groups, counseling, support websites
Table 2 displays the time in minutes spent on intervention activities. On average, the intake assessment calls lasted 66.9 minutes (SD=21.7); the three education calls required 50.6 minutes (SD=16.7), 48.1 minutes (SD =5.9), and 39.6 (SD=14.8) minutes respectively; the follow-up education calls lasted 24.7 minutes (SD=14.8); and the support calls lasted 42.8 (SD=29.6) minutes. Time taken to document the interaction with participants is also listed in Table 2. On average, it took 18.4 minutes to document time for intake assessment, 23-27 minutes for education calls, 12.3 minutes for follow-up calls, and 23.0 minutes for support calls. The calls for data collection (data not shown) lasted an average of approximately 51 minutes, with documentation time of 11.5 minutes.
Table 2. Interventionist Time Recorded in the RBCS Study (N=328).
| Intervention Components |
Minutes spent | |||||
|---|---|---|---|---|---|---|
| N | Min. | Mean | Median | Max. | SD | |
| Intake Assessment | ||||||
| Calls | 323 | 30 | 66.95 | 61 | 180 | 21.71 |
| Documentation | 315 | 5 | 18.43 | 20 | 40 | 6.6 |
| Total | 325 | 15 | 84.40 | 80 | 205 | 24.95 |
| Education Call 1 | ||||||
| Calls | 286 | 13 | 50.65 | 50 | 120 | 16.67 |
| Documentation | 281 | 10 | 27.51 | 30 | 60 | 8.96 |
| Total | 286 | 25 | 77.68 | 75 | 147 | 21.18 |
| Education Call 2 | ||||||
| Calls | 275 | 15 | 48.08 | 45 | 120 | 15.91 |
| Documentation | 270 | 10 | 26.53 | 30 | 60 | 8.5 |
| Total | 275 | 37 | 74.12 | 75 | 180 | 20.16 |
| Education Call 3 | ||||||
| Calls | 277 | 15 | 39.56 | 40 | 90 | 14.84 |
| Documentation | 274 | 10 | 22.98 | 25 | 60 | 7.7 |
| Total | 277 | 25 | 62.29 | 61 | 141 | 19.71 |
| Follow-up Education | ||||||
| Calls | 276 | 5 | 24.71 | 20 | 105 | 14.78 |
| Documentation | 270 | 2 | 12.28 | 10 | 50 | 8.43 |
| Total | 276 | 6 | 36.72 | 31.5 | 143 | 19.91 |
| Support (6 calls total) | ||||||
| Calls | 309 | 5 | 42.83 | 35 | 165 | 29.65 |
| Documentation | 309 | 2 | 23.01 | 21 | 60 | 11.96 |
| Total | 310 | 7 | 65.63 | 58.5 | 195 | 37.79 |
Table 3 shows the results from the repeated measures models for interventionists’ time. In both full and reduced models, apart from the type of contact, longer interventionists’ time was significantly associated with participants’ higher depression symptom levels (p =0.0001), and concurrent or prior use of support services such as support groups or counseling (p=0.0048).Shorter interventionists’ time use was associated with assignment to the Delayed Education group (p = 0.0077). Time since end of treatment and treatment type and mix were not significantly associated with interventionists’ time.
Table 3. Repeated Measures Models for Interventionist Time.
| Covariate / Characteristic | Full model | Reduced model | |||
|---|---|---|---|---|---|
| Estimate (SE) |
P | Estimate (SE) | P | ||
| Intercept | 71.87 (7.39) | <.0001 | 71.87 (2.69) | <.0001 | |
|
| |||||
| Delayed Education group | −6.29 (2.06) | 0.0024 | −5.28 (1.97) | 0.0077 | |
|
| |||||
| Contact | Intake Assessment | 18.24 (1.55) | <.0001 | 18.71 (1.53) | <.0001 |
| ED 1 | 9.74 (1.61) | <.0001 | 10.41 (1.59) | <.0001 | |
| ED 2 | 6.27 (1.63) | 0.0001 | 6.79 (1.61) | <.0001 | |
| ED 3 | −5.54 (1.63) | 0.0007 | −4.86 (1.6) | 0.0025 | |
| FUE | −31.32 (1.63) | <.0001 | −30.42 (1.61) | <.0001 | |
| SUP | Ref. | . | Ref | . | |
|
| |||||
| Age ≥ 65 | 1.42 (2.95) | 0.6309 | - | - | |
| Minority | −3.04 (4.71) | 0.5196 | - | - | |
|
| |||||
| Married or partnered | −2.28 (2.73) | 0.4056 | - | - | |
| Depressive symptoms a | 9.04 (2.58) | 0.0005 | 9.1 (2.36) | 0.0001 | |
| Using support services b | 6.9 (2.63) | 0.0092 | 7.03 (2.47) | 0.0048 | |
|
| |||||
| Education | < High school | 0.38 (5.56) | 0.9462 | - | - |
| High school graduate | −2.58 (3.77) | 0.4947 | - | - | |
| Technical /some college | −0.21 (3.48) | 0.9525 | - | - | |
| Completed college | −0.46 (3.42) | 0.8921 | - | - | |
| Postgraduate | Ref. | . | - | - | |
| Employment | Full-time | Ref. | . | - | - |
| Part-time | 1.46 (3.63) | 0.6883 | - | - | |
| Retired | −1.91 (3.42) | 0.577 | - | - | |
| Homemaker | 9.82 (4.79) | 0.0412 | - | - | |
| Other | 5.27 (4.39) | 0.2305 | - | - | |
| Income | $20,000 or less | −4.36 (3.73) | 0.2427 | - | - |
| $20,001 to $30,000 | −1.65 (3.72) | 0.6568 | - | - | |
| $30,001 to $40,000 | −2.77 (4.3) | 0.5208 | - | - | |
| $40,001 to $50,000 | 1.9 (3.62) | 0.6003 | - | - | |
| Greater than $50,000 | Ref. | . | - | - | |
| Declined to answer | −4.34 (3.39) | 0.2016 | - | - | |
| With health insurance | 1.54 (5.3) | 0.7713 | - | - | |
|
| |||||
| Months since tx | ≤ 12 | −3.08 (3.45) | 0.3725 | - | - |
| 12.1 – 24 | −4.56 (2.95) | 0.1235 | - | - | |
| > 24 | Ref. | . | - | - | |
| Treatment mix | Surgery only | −3.34 (3.51) | 0.3423 | - | - |
| Surgery, chemotherapy | −1.13 (3.06) | 0.713 | - | - | |
| Surgery, radiation | −0.49 (2.69) | 0.8545 | - | - | |
| Surgery, chemo, | |||||
| radiation | Ref. | . | - | - | |
CES-D scores ≥ 16;
Cancer support groups, counseling, support websites
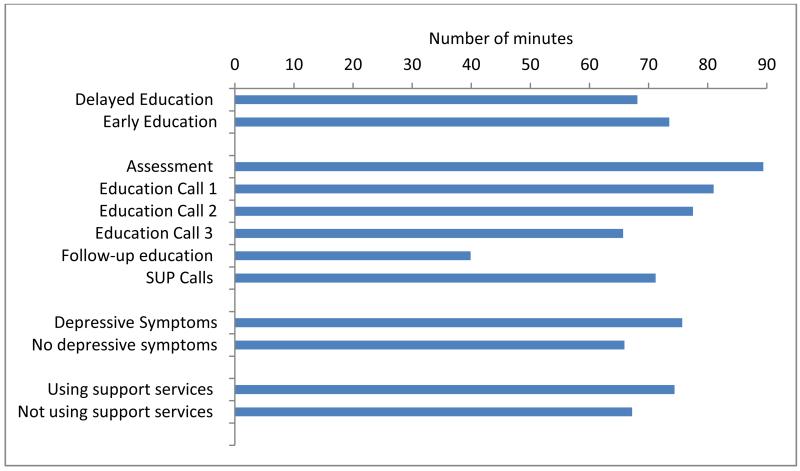
Figure 1 presents the least square mean of interventionists’ time by type of call and other predictors. Thus, for an average representative participant, the interventionists’ time ranged from 86.5 minutes for the intake assessment to 37.4 for the follow-up education call. Moreover, interventionists spent an average of 75.7 minutes with survivors with depressive symptoms, compared to 65.9 minutes with survivors who did not have such distress, as well as an average of 71.4 minutes with survivors who had previously used support services such as support groups or counseling, compared to 64.4 minutes spent on average with survivors who had not used this type of services.
Figure 1. Least Square Means of Total Interventionists’ Time by Type of Call and Significant Predictors.
The observed range for the baseline MOS-SSS overall social support index among the 328 study participants was 17 to 100, with mean=78.8 and SD=21.6. After fitting the overall social support index as an additional predictor in the reduced model we found that, on average, a standard deviation increase in the social support index was associated to a decrease in interventionist time per call of about 2.65 minutes (SE=1.079, p=0.0192). Inclusion of social support did not affect the model parameters and significance tests for contact occasion, study group, and use of support services, but it decreased the effect of CESD≥16 (B=7.01, SE=2.65, p=0.0079).
DISCUSSION
Education and support interventions are known to improve the quality of life of breast cancer survivors. The primary resource used to implement these interventions is the time spent by interventionists with participants and on related activities, such as documentation of the interactions. For the intervention implemented in the RBCS study, one hour of time with a participant was accompanied by another 30 minutes of time devoted to documentation. Using this and appropriate salary information, the cost of implementing this intervention can be calculated in various settings and for each intervention component. Importantly, we determined that the use of resources varied by the characteristics and needs of participants. Thus, the intervention implementation cost will differ depending on the characteristics of the population served by the intervention. In particular, how long interventionists spent with each survivor in this rural population did not depend on cancer-related factors, but on factors related to the survivors’ mental health and possibly social support needs. These considerations are important to adequately plan for these interventions.
To evaluate the personnel required to implement a telephone-based intervention such as the RBCS presented here, it is important to understand the intervention activities and what additional time costs may be needed. Since the RBCS intervention was delivered to underserved rural breast cancer survivors by telephone, the intake assessment naturally took more time to get to know, engage, and assess each survivor, and was the most resource-intense call. Each subsequent education session took accordingly less time, likely due to the rapport established and the information gathered during the intake assessment call.
The recorded interventionists’ time with survivors ranged between 30-60 minutes with 45 minutes on average across the different types of calls. This time was within the range of minutes allotted for the intake assessment and subsequent education calls. However, a considerable amount of time, 22% to 37% of the total time related to an intervention call, was spent by interventionists documenting each phone call. The interventionists took notes and typed a narrative of each participant encounter. This time also varied by type of call as well as the additional survivorship questions, concerns, and needs identified by the participants. The interventionists also spent time scheduling the next follow-up call, which was relatively brief, and rescheduling missed appointments. In particular, more time was needed if the participant was unavailable at a scheduled time and/or more time was needed for repeated attempts to contact. Moreover, over the course of the year, after development of a trusting relationship with the interventionists, some participants would ask to continue talking “off the record.” In these cases the interventionists turned off the recording device. Participants often wanted to discuss aspects of their lives that they felt were personal or unrelated to their survivorship. For example, a participant who was dealing with infertility and pursuing adoption wanted to discuss adoption with her interventionist. Time spent on these calls was not included in our analyses: however, given that the rapport established with the interventionist was particularly meaningful for these rural survivors “off the record” conversation should be considered when implementing support interventions in this population.
Our findings also reinforce those by Stagl et al [21] who reported that breast cancer survivors at risk for depressive symptoms after treatment benefit from early cognitive-behavioral intervention to reduce the incidence of depression. Moreover, others have shown that survivors with depression require more resources: the time spent by a nurse care manager in a telecare management intervention for pain and depression for cancer survivors was higher among survivors with depression than for the overall group of participants [22]. Breast cancer survivors who already sought or engaged in support services also required more interventionist time, independent of their depressive symptoms. Likely, they are survivors having high need for support and actively seeking counseling and other forms of communication.
There was no difference in time spent by the interventionists with survivors who recently completed treatment and those who experienced common late effects of chemotherapy or radiation therapy. We infer from these results that support interventions in a rural population of breast cancer survivors are as valuable for long-term survivors as for early term survivors, regardless of the survivor treatment history. Moreover, treatment late effects may become less relevant compared to other quality of life concerns, for example those related to mental health. It may also be that the intervention adequately planned to address issues related to treatment during the education calls, but underestimated the time needed to address additional depression and support issues. These considerations are important for future implementation of this intervention.
Our findings lead us to several considerations about implementing our intervention in the future. We tested a comprehensive and extensive survivorship intervention package in our RBCS study. However, it might be opportune to consider a basic survivorship care plan with additional resources in terms of interventionists’ time for survivors with depression or with lack of support. However, further research is needed to determine the optimal level of support for those with depression, and for those who do not have these characteristics. Overall, for planners who consider implementing survivorship interventions, assessing the mental health and psychosocial distress of the target population can help better plan for adequate level of personnel needed. Moreover, while our intervention was delivered by nurses, depending on the needs of the population, a combination of professional and non-professional interventionists may lead to a less costly but equally effective intervention. However, further research is needed to assess the effectiveness of such a combination of personnel on survivors’ outcomes.
Finally, the calls in the Delayed Education and Support intervention were on average about five minutes shorter than in the Early Education and Support Intervention after controlling for survivors’ characteristics and type of call. This finding leads to considerations about the delivery of telephone-based interventions. In the Delayed Education Group, support calls were provided during the first 6 months, and the education calls in the latter six months. Thus, the establishment of rapport through the support calls in an intervention in which there was no face-to-face contact may ultimately lead to lower use of resources and, thus, lower intervention costs. It may also be that the needs of survivors related to depressive symptoms and high need of support are addressed up front in the delayed intervention, and thus less time was needed later for the education/support calls.
Several study limitations are noted. First, we did not include here all intervention activities such as research staff meetings. Thus, the interventionists’ time may not reflect the overall time spent on the intervention. There may also be other intervention activities whose time varies by the characteristic of the participant. For example, it is conceivable that survivors with depressive symptoms or high need of support were discussed more at length in team meetings or informally among interventionists. Second, the population-based sample of rural breast cancer survivors in the RBCS, while representative of Florida, may not be representative of the larger rural breast cancer survivor population in the United States. While few minorities participated in the study, this characteristic reflects the population of Florida where minority populations live in urban areas. Third, the trial was not initially developed to assess costs of interventions and collection of data on interventionists time started after the first 150 participants had already enrolled. However, despite the smaller sample size for which interventionists’ time was collected, our data were collected after an initial learning phase for interventionists, and, thus, reflect true implementation costs.
Implications for Survivors
To inform the broad scale implementation of effective survivorship interventions, a better understanding of how implementation resources are ultimately allocated based on survivors’ needs is vital. Overall, our study suggests that a careful consideration of the mental health status and the need of support is needed when planning the implementation of effective survivorship interventions on a broad scale.
Acknowledgments
The authors thank the breast cancer survivor participants who gave generously of their time.
Funding source: This study was supported by the National Institute of Nursing Research (R01NR-01185-03) and the National Cancer Institute (RO1CA-120638-07).
Acknowledgment and Disclosure: The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System under contract with the Department of Health (DOH). The views expressed herein are solely those of the authors and do not necessarily reflect those of the contractor or DOH.
Footnotes
Conflict of Interest: The authors declare no other conflict of interest
REFERENCES
- 1.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. Am J Public Health. 2012;102(7):1274–81. doi: 10.2105/AJPH.2012.300755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mandelblatt JS, Cullen J, Lawrence WF, et al. Economic evaluation alongside a clinical trial of psycho-educational interventions to improve adjustment to survivorship among patients with breast cancer. J Clin Oncol. 2008;26(10):1684–90. doi: 10.1200/JCO.2007.14.0822. [DOI] [PubMed] [Google Scholar]
- 3.Stanton AL, Ganz PA, Kwan L, et al. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23(25):6009–18. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- 4.Neta G, Glasgow RE, Carpenter CR, et al. A framework for enhancing the value of research for dissemination and implementation. Am J Public Health. 2015;105(1):49–57. doi: 10.2105/AJPH.2014.302206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribisl KM, Leeman J, Glasser AM. Pricing health behavior interventions to promote adoption: lessons from the marketing and business literature. Am J Prev Med. 2014;46(6):653–9. doi: 10.1016/j.amepre.2014.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meneses K, McNees P, Loerzel VW, Su X, Zhang Y, Hassey LA. Transition from treatment to survivorship: effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncol Nurs Forum. 2007;34(5):1007–16. doi: 10.1188/07.ONF.1007-1016. [DOI] [PubMed] [Google Scholar]
- 7.Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. The Cochrane Database of Systematic Reviews. 2012;11:CD007064. doi: 10.1002/14651858.CD007064.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meneses K, McNees P, Azuero A, Loerzel VW, Su X, Hassey LA. Preliminary evaluation of psychoeducational support interventions on quality of life in rural breast cancer survivors after primary treatment. Cancer Nurs. 2009;32(5):385–97. doi: 10.1097/NCC.0b013e3181a850e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Florida Department of Health . Rural population by census tract. Tallahassee, FL: [Google Scholar]
- 11.McNees P, Meneses K. Index of Research Access. Nurs Res Rev. 2012;3:5–7. [Google Scholar]
- 12.Meneses K, Benz R, Hassey L, Yang Z, McNees P. Strategies to retain rural breast cancer survivors in longitudinal research. Appl Nurs Res. 2013;26(40):257–62. doi: 10.1016/j.apnr.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Radloff L. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psych Meas. 1977;1(3):385–401. [Google Scholar]
- 14.Meneses K, Azuero A, Hassey L, McNees P, Pisu M. Does economic burden influence quality of life in breast cancer survivors? Gynecol Oncol. 2012;124(3):437–43. doi: 10.1016/j.ygyno.2011.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pisu M, Azuero A, Meneses K, Burkhardt J, McNees P. Out of pocket cost comparison between Caucasian and minority breast cancer survivors in the Breast Cancer Education Intervention (BCEI) Breast Cancer Res Tr. 2011;127(2):521–9. doi: 10.1007/s10549-010-1225-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Given BA, Given CW, Stommel M. Family and out-of-pocket costs for women with breast cancer. Cancer Pract. 1994;2(3):187–93. [PubMed] [Google Scholar]
- 17.Sherbourne C, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 18.Meneses K, Azuero A, Su X, Benz R, McNees P. Predictors of attrition among rural breast cancer survivors. Res Nurs Health. 2014;37(1):21–31. doi: 10.1002/nur.21576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherbourne C, Stewart AL. The MOS Social Support Survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 20.SAS. v9.4 Statistical Software. SAS Institute, Inc.; Cary, North Carolina: [Google Scholar]
- 21.Stagl JM, Antoni MH, Lechner SC, et al. Randomized controlled trial of cognitive behavioral stress management in breast cancer: A brief report of effects on 5-Year depressive symptoms. Health Psychol. 2014;34(2):176–80. doi: 10.1037/hea0000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Theobald W, Wu J, Norton K, Morrison G, Carpenter J, Tu W. Effect of telecare management on pain and depression in patients with cancer: A randomized trial. JAMA. 304(2):163–71. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]