Abstract
Anterior cervical osteophytes are found in 20-30% of elderly patients. Rarely, severe osteophytes can cause dysphagia, dysphonia, and dyspnea. Here, we illustrate a case of severe dysphagia caused by a large post-traumatic osteophyte with oropharyngeal swallow study showing a significant mass effect on the pharynx and resolution following osteophytectomy. We also review the literature regarding the etiology, diagnosis, and treatment of symptomatic anterior cervical osteophytes.
Keywords: cervical osteophyte, osteophytectomy
Introduction
Greater than 75% of people aged 65 and older have varying degrees of cervical spine degenerative changes, including hypertrophic anterior cervical osteophytes [1-3]. Specifically, anterior cervical osteophytes have a prevalence of 20-30% in the elderly population [4]. Causes of cervical osteophytes include diffuse idiopathic skeletal hyperostosis, ankylosing spondylitis, degenerative changes, and prior trauma, including surgery [5]. Anterior cervical osteophytes are generally asymptomatic; however, in rare cases, they can lead to dysphagia, dysphonia, and dyspnea [6-7]. Such symptoms are generally correlated with the size of the hypertrophic spurs [8]. Here, we present a case of a 63-year-old man presenting with a large anterior osteophyte causing severe dysphagia, whose symptoms resolved following cervical osteophytectomy.
Case presentation
A 63-year-old man with a history of neck trauma resulting in vocal cord injury ten years prior presented with two years of progressive dysphagia. He was unable to swallow solid foods, and could tolerate only a puree and liquid diet. He had no dysphonia or dyspnea but did have some odynophagia on swallowing. He was otherwise healthy with no other medical history. Informed patient consent was obtained for treatment.
Computed tomography (CT) of the cervical spine showed a large anterior osteophyte spanning from C3 to C6 and measuring 19 mm at its greatest anteroposterior extent (Figure 1A, arrow). An oropharyngeal swallow study showed a significant mass effect on the pharynx and splitting of the contrast into two tracts (arrowheads) around the osteophyte (asterisk) during active swallow on the anteroposterior view (Figure 1B). In addition, cricopharyngeus (CP) hypertrophy with mild narrowing of the upper esophageal sphincter was observed (thin arrow). Aspiration of liquids and, to a lesser extent, pureed foods, was noted on swallow studies.
Figure 1. Anterior cervical osteophyte before and after osteophytectomy.
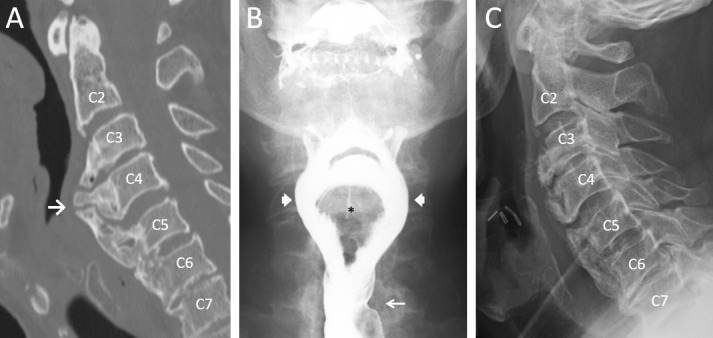
The patient underwent an anterior cervical osteophytectomy with concomitant CP myotomy. Bone wax was used intra-operatively to prevent bone regrowth [9]. A postoperative lateral plain film showed the removal of the anterior osteophyte (Figure 1C). The patient reported significant improvement of dysphagia immediately postoperatively and complete resolution of symptoms at his one-month follow-up. At his one-year follow-up, the patient continued to report resolution of his symptoms with normal swallow function. Of note, NSAIDs were administered postoperatively to prevent osteophyte regrowth [10].
Discussion
Osteophytes can form at any cervical level but are most common at C5-6 and C6-7, likely due to greater load-bearing and mobility [11]. Dysphagia in patients with anterior osteophytes may be explained by the fact that the esophagus rests on the anterior border of the cervical vertebrae from C4-7. Etiologies of dysphagia include a large osteophyte causing significant mechanical compression, a smaller osteophyte causing obstruction at the level of the cricoid cartilage, and inflammation secondary to local mass effect [12-15].
Most anterior cervical osteophytes are asymptomatic; however, they are not an uncommon cause of dysphagia. Interestingly, one study in the veteran population showed anterior cervical bony protrusion in 10.6% of patients over 60 years of age undergoing dysphagia evaluation, suggesting that the incidence of cervical osteophytes causing dysphagia is higher than recognized in the medical community, and underscoring their place in the differential diagnosis of dysphagia [16].
The diagnosis of cervical osteophytes may be accomplished with a CT scan, which can clearly define the bony anatomy. A barium swallow is essential to confirm the presence of esophageal compression by the cervical osteophyte. Magnetic resonance imaging (MRI) may also be considered in patients with additional symptoms, such as dyspnea and dysphonia, to identify any soft tissue damage, perforations, or superinfection. MRI is also useful to evaluate any concomitant central or foraminal cervical stenosis that the surgeon may wish to address at the time of osteophytectomy.
The mainstay of treatment for cervical osteophytes is conservative, including anti-inflammatory medications and diet modification [17]. However, for patients in whom conservative management has failed, operative intervention may be considered. Some authors argue that cervical osteophytectomy should be considered in all patients with cervical osteophytes causing chronic dysphagia and dyspnea because of possible progression to acute respiratory distress. Maiuri, et al. reported a case of a patient with a two-year history of dysphagia who suffered sudden severe respiratory distress requiring emergency tracheotomy [18].
Surgery for cervical osteophytes has good long-term outcomes. Our patient continued to have symptomatic relief at his one-year follow-up. This is in keeping with a prior series published by Urrutia, et al. showing no recurrence of dysphagia and minimal radiographic regrowth at one to nine year (average 59.8 months) follow-up evaluations [19]. A second series published by Miyamoto, et al. reported immediate postoperative relief of dysphagia in all patients, but noted some radiographic recurrence at six‑ to 13-year follow-up evaluations (mean: nine years), with an average rate of regrowth of 1 mm/year [20]. Five out of seven of their patients remained asymptomatic, but two had moderate dysphagia 10 and 11 years after surgery, suggesting a low rate of late symptomatic recurrence [20].
Conclusions
Large anterior cervical osteophytes are a potential cause of dysphagia. The key imaging study is a barium swallow. Patients with significant symptoms who fail conservative management should be considered for osteophytectomy. Outcomes following osteophytectomy are very favorable.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Contribution of disc degeneration to osteophyte formation in the cervivcal spine: a biomechanical investigation. Kumaresan S, Yoganandan N, Pintar FA, Maiman DJ, Goel VK. J Orthop Res. 2001;19:977–984. doi: 10.1016/S0736-0266(01)00010-9. [DOI] [PubMed] [Google Scholar]
- 2.Degenerative disease of the vertebral column. Resnick D. http://dx.doi.org/10.1148/radiology.156.1.3923556. Radiology. 1985;156:3–14. doi: 10.1148/radiology.156.1.3923556. [DOI] [PubMed] [Google Scholar]
- 3.Dysphagia caused by ventral osteophytes of the cervical spine: clinical and radiographic findings. Seidler TO, Pèrez Alvarez JC, Wonneberger K, Hacki T. Eur Arch Otorhinolaryngol. 2009;266:285–291. doi: 10.1007/s00405-008-0735-4. [DOI] [PubMed] [Google Scholar]
- 4.The development of dysphagia and dysphonia due to anterior cervical osteophytes. Akbal A, Kurtaran A, Selcuk B, Gurcan A, Ersoz M, Akyuz M. Rheumatol Int. 2009;29:331–334. doi: 10.1007/s00296-008-0669-6. [DOI] [PubMed] [Google Scholar]
- 5.Diffuse idiopathic skeletal hyperostosis (DISH) [ankylosing hyperostosis of Forestier and Rotes-Querol] Resnick D, Shapiro RF, Wiesner KB, Niwayama G, Utsinger PD, Shaul SR. Semin Arthritis Rheum. 1978;7:153–187. doi: 10.1016/0049-0172(78)90036-7. [DOI] [PubMed] [Google Scholar]
- 6.Dysphagia and dysphonia secondary to anterior cervical osteophytes. Brandenberg G, Leibrock LG. Neurosurgery. 1986;18:90–93. doi: 10.1227/00006123-198601000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Retro-pharyngeal obstruction in association with osteophytes of the cervical spine. Fuerderer S, Eysel-Gosepath K, Schröder U, Delank KS, Eysel P. J Bone Joint Surg Br. 2004;86:837–840. doi: 10.1302/0301-620x.86b6.14933. [DOI] [PubMed] [Google Scholar]
- 8.Giant cervical hyperostosis of the prevertebral space: presentation of two cases and review of the literature (Article in Italian) Bruno E, Alessandrini M, De Angelis E. Acta Otorhinolaryngol Ital. 1996;16:532–536. [PubMed] [Google Scholar]
- 9.Bone healing after median sternotomy: a comparison of two hemostatic devices. Vestergaard RF, Jensen H, Vind-Kezunovic S, Jakobsen T, Søballe K, Hasenkam JM. J Cardiothorac Surg. 2010;5:117. doi: 10.1186/1749-8090-5-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Do nonsteroidal anti-inflammatory drugs affect bone healing? A critical analysis. Pountos I, Georgouli T, Calori GM, Giannoudis PV. ScientificWorldJournal. 2012;2012:606404. doi: 10.1100/2012/606404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cervical spondylosis. Schmidek HH. Am Fam Physician. 1986;33:89–99. [PubMed] [Google Scholar]
- 12.Vertebral spinal osteophytes. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Anat Sci Int. 2011;86:1–9. doi: 10.1007/s12565-010-0080-8. [DOI] [PubMed] [Google Scholar]
- 13.Cervical spine disease and dysphagia. Four new cases and a review of the literature. Lambert JR, Tepperman PS, Jimenez J, Newman A. Am J Gastroenterol. 1981;76:35–40. [PubMed] [Google Scholar]
- 14.Dysphagia due to cervical spondylosis. Crowther A, Ardran GM. J Laryngol Otol. 1985;99:1167–1169. doi: 10.1017/s0022215100098352. [DOI] [PubMed] [Google Scholar]
- 15.Cervical osteophytic dysphagia: single and combined mechanisms. Di Vito J. Dysphagia. 1998;13:58–61. doi: 10.1007/PL00009550. [DOI] [PubMed] [Google Scholar]
- 16.Anterior cervical osteophytes as a cause of pharyngeal stage dysphagia. Granville LJ, Musson N, Altman R, Silverman M. J Am Geriatr Soc. 1998;46:1003–1007. doi: 10.1111/j.1532-5415.1998.tb02757.x. [DOI] [PubMed] [Google Scholar]
- 17.Dysphagia due to cervical osteophytosis. Laus M, Malaguti MC, Alfonso C, Ferrari D, Zappoli FA, Giunti A. Chir Organi Mov. 1995;80:263–271. [PubMed] [Google Scholar]
- 18.Dysphagia and dyspnea due to an anterior cervical osteophyte. Maiuri F, Stella L, Sardo L, Buonamassa S. Arch Orthop Trauma Surg. 2002;122:245–247. doi: 10.1007/s00402-001-0369-0. [DOI] [PubMed] [Google Scholar]
- 19.Long-term results of surgical treatment of dysphagia secondary to cervical diffuse idiopathic skeletal hyperostosis. Urrutia J, Bono CM. Spine J. 2009;9:0–7. doi: 10.1016/j.spinee.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Postsurgical recurrence of osteophytes causing dysphagia in patients with diffuse idiopathic skeletal hyperostosis. Miyamoto K, Sugiyama S, Hosoe H, Iinuma N, Suzuki Y, Shimizu K. Eur Spine J. 2009;18:1652–1658. doi: 10.1007/s00586-009-1133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


