Abstract
There is a known high disparity in access to perinatal care services between urban and rural areas in Tanzania. This study analysed repeated cross-sectional (RCS) data from Tanzania to explore the relationship between antenatal care (ANC) visits, facility-based delivery and the reasons for home births in women who had made ANC visits. We used data from RCS Demographic and Health Surveys spanning 20 years and a cluster sample of 30 830 women from ∼52 districts of Tanzania. The relationship between the number of ANC visits (up to four) and facility delivery in the latest pregnancy was explored. Regional changes in facility delivery and related variables over time in urban and rural areas were analysed using linear mixed models. To explore the disconnect between ANC visits and facility deliveries, reasons for home delivery were analysed. In the analytic model with other regional-level covariates, a higher proportion of ANC (>2–4 visits) and exposure to media related to an increased facility delivery rate in urban areas. For rural women, there was no significant relationship between the number of visits and facility delivery rate. According to the fifth wave result (2009–10), the most frequent reason for home delivery was ‘physical distance to facility’, and a significantly higher proportion of rural women reported that they were ‘not allowed to deliver in facility’. The disconnect between ANC visits and facility delivery in rural areas may be attributable to physical, cultural or familial barriers, and quality of care in health facilities. This suggests that improving access to ANC may not be enough to motivate facility-based delivery, especially in rural areas.
Keywords: Antenatal care, facility delivery, repeated cross-sectional study
Key Messages
A higher regional proportion of women who had antenatal care visits twice or more was associated with higher facility delivery rate in urban area. In rural areas, at least one to four antenatal visits was not related to facility delivery.
Antenatal care visits at least four times was not related to the facility-based delivery rate in urban and rural areas.
Introduction
Tanzania has experienced tremendous social changes and this has affected the health status of vulnerable populations over the last few years (Mujinja and Kida 2014). Rural women especially have been placed in a worse health-care position compared with urban women (Tanzania Gender Networking Program and Macro 2007). Since the 1990s, despite the fact that free medical services are provided to mothers and children, indicators such as nutritional status of mothers, ANC attendance and facility-based delivery have not correspondingly improved (National Bureau of Statistics Tanzania and ICF Macro 2000; Maletnlema 2002; Abubakar et al. 2012). The situation is worse in rural Tanzania because of poor sociocultural, physical and financial accessibility (Kruk et al. 2008; Gabrysch and Campbell 2009). Tanzania has a network of health facilities at national, regional, district, divisional, ward and village level enabling >90% of population to be within 10 km of a health facility (Mella 2003). Overall 60% of health services are provided by public sector and the government exempts the poor and vulnerable groups from user-fees in essential maternal and child health services (Ministry of Health 2003). In urban areas, health-care services is more easily accessible than in rural areas due to available and reliable transportation and higher coverage of health facilities (Pfeiffer and Mwaipopo 2013).
Maternal mortality is one of the key indicators of women’s health status. Despite the global efforts to improve maternal health, the mortality rate is still unacceptably high in Tanzania. According to a World Health Organization (2012) report, the maternal mortality ratio in 2010 was 460 per 100 000 live births and annually, around 8500 women die from pregnancy-related causes. Because most of the maternal deaths occur during and immediately after childbirth (AbouZahr 1998), delivery in a health facility has been suggested as the key component for prevention of pregnancy-related death.
There are four groups of determinants of delivery service use: (1) sociocultural, (2) perceived need, (3) economic accessibility and (4) physical accessibility (Gabrysch and Campbell 2009). These factors are found to influence use of delivery care at community and individual level (Gage and Guirlène Calixte 2006; Asp et al. 2014). Among individual factors, attending ANC visits at least two or three times is known to be a strong predictor of facility delivery along with the mother’s age, parity, her education and that of her partner and frequent media exposure (Amooti-Kaguna and Nuwaha 2000; Simkhada et al. 2008; Gabrysch and Campbell 2009; Anyait et al. 2012; Pervin et al. 2012; Kitui et al. 2013; Worku et al. 2013; Asp et al. 2014; Feyissa and Genemo 2014). According to previous reports, more than three ANC visits is related to an higher probability of subsequent facility delivery compared with only two ANC visits and this relationship is affected by various factors across the different geographical regions (Pervin et al. 2012; Trujillo et al. 2013). Since a large proportion of the variation in facility delivery rate is explained by factors at the area level (Gage 2007), this persistently steady change in the facility-based delivery could be explained better with regional or systemic factors such as a regional-ANC rate.
Generally, at least four ANC visits are recommended for safe motherhood (World Health Organization, Department of Making Pregnancy Safer 2006). Most of the policies to promote the mother’s health have focused on improving economic and physical accessibility to increase the number of ANC visits at least four times (Olsen et al. 2005; Finlayson and Downe 2013). In 2002, Tanzania’s Ministry of Health and Social Welfare implemented focused antenatal care (FANC) model from World Health Organization. The principle of this model was to integrate ANC through health promotion, disease prevention, detection and treatment of diseases and birth preparedness (von Both et al. 2006). The FANC had been expected to serve as a mechanism for increasing facility-based deliveries (Kearns et al. 2014). During the past two decades, however, the percentage of women who had four or more ANC visits has declined, regardless of whether they are from urban or rural areas despite all the efforts made to encourage them (National Bureau of Statistics Tanzania and ICF Macro 2011). Nevertheless, the prevalence of facility delivery has remained around 40–50% with little change (Tanzania Gender Networking Program and Macro 2007). These findings suggest four times of ANC visits would not always associate with higher probability of facility-based delivery. Considering the variations in reasons women give for delivering at home depending on the different settings (Kitui et al. 2013), the relationship between the number of ANC visits and facility-based delivery needs to be explored (Exavery et al. 2014).
The wide urban–rural differentials have been concealed by aggregate figures. According to the Tanzania Demographic and Health Survey (TDHS) 2004–05, <25% of deliveries occurred in health facilities in Zanzibar North, whereas around 90% of deliveries in Dar es Salaam were facility-based (National Bureau of Statistics Tanzania and ICF Macro 2005). Furthermore, the gap between urban and rural areas regarding facility delivery rates has remained unchanged up to now (Ndao-Brumblay et al. 2013). This disparity may reflect social or systemic determinants of place of delivery that operate differently in urban and rural settings.
To explain this discrepancy between minimum of four ANC visits and facility-based delivery in urban and rural areas, we hypothesized that countries with a considerable urban–rural gap, such as Tanzania, could show different patterns in the association between ANC visits and facility-based delivery. Previous studies regarding the contribution of ANC visiting and facility-based delivery used cross-sectional studies because of a lack of proper longitudinal data (Moyer and Mustafa 2013). This study explores how the frequency of ANC visits mediates longitudinal trends of facility delivery at the regional level using repeated survey data from Tanzania over 20 years.
Methods
Data
This study used the DHS data for Tanzania from the United States Agency for International Development from five time points. TDHS is a nationally representative survey of over 10 000 households selected from sample points. All reproductive-aged women in these households are individually interviewed. National, urban or rural estimates of major indicators are produced from the survey. The sampling design and survey method of this national representative survey are described elsewhere (Canavan et al. 2014). Individual women’s self-reported data were also included to calculate the regional data of each time dimension. To obtain the most recent information, only the women who delivered their babies within 5 years of the survey were included for the analysis. Of those who had more than one delivery in the last 5 years, only information on the latest delivery was adopted for analysis. Therefore, the values of several indicators in this study could be different from those of official DHS reports, which include all reported pregnancy cases.
To explore the association between regional factors and longitudinal changes in facility delivery rate, the regional mean level of indicators was used as panel data. Because the set of observations is not from identical individuals across all waves, this kind of data aggregation over a time period has been referred to as repeated cross-sectional (RCS) or ‘pseudo-panel’ data (Lebo and Weber 2014). This RCS design was also used in a recent study on the relationship between sugar and occurrence of population-level diabetes (Basu et al. 2013). In our study, there are five time points according to the year of survey: Time point 1 covers DHS data from 1991 to 1992; 1996 is Time point 2; 1999 is Time point 3; Time point 4 is 2004–05 and Time point 5 is 2009–10 according to the survey year. The survey is conducted every 5 years taking 3–5 months at each time period (National Bureau of Statistics Tanzania and ICF Macro 2000, 2005, 2011).
Key variables were included in reference to the results of previous studies and availability of the data. The mean age of the women, mean number of total live births, percentage of women and partners who had completed secondary education, proportion of number of ANC visits made, proportion of women who were exposed to mass media and the percentage of nulliparous women were calculated by region. Those women who read newspapers or listened to radio or watched television at least once a week were assumed to be exposed to mass media. Because the variables for level of household wealth and type (public/private and health centre/dispensary) of ANC providers were only available in Time points 4 and 5, these factors could not be considered in the analyses. Finally, responses to the question ‘Why didn’t you deliver in a health facility?’, which was only included in TDHS 2009–10, were analysed to explore the reasons why some women who had visited for ANC at least once gave birth to their babies at home. Because the study utilizes only publicly available, anonymous data, the institutional review was not required in our institution.
Statistical analysis
The calculation and comparison of each variable between urban and rural areas was done using weighted values. Because the regional rate of facility delivery is not normally distributed and the mean value is relatively large, the log-transformed value was used in the analysis. Regional factors related with facility-based delivery rate were analysed in urban and rural areas separately. Linear mixed model was used in exploring the association between proportion of ANC visits (1–4 times) and regional facility-based delivery rates to consider the correlation structure within and between the repeated regional data of facility delivery in different time points. Model 1 indicates the random coefficient model without exploring the error; Model 2 explores the correlation structures within the regional facility delivery rate and Model 3 contains the covariance between and within the regional facility delivery rate. Regional-level covariates were applied in the multivariable models to identify the adjusted effect of proportions of ANC ≥ 2. The Akaike information criteria (AIC) of each linear mixed model were calculated by the method recommended by Diggle and Wolfinger using the restricted maximum likelihood for variance–covariance structure selection (Wolfinger 1996). The analyses were done using SAS software, version 9.3 (SAS Institute Inc., Cary, NC).
Results
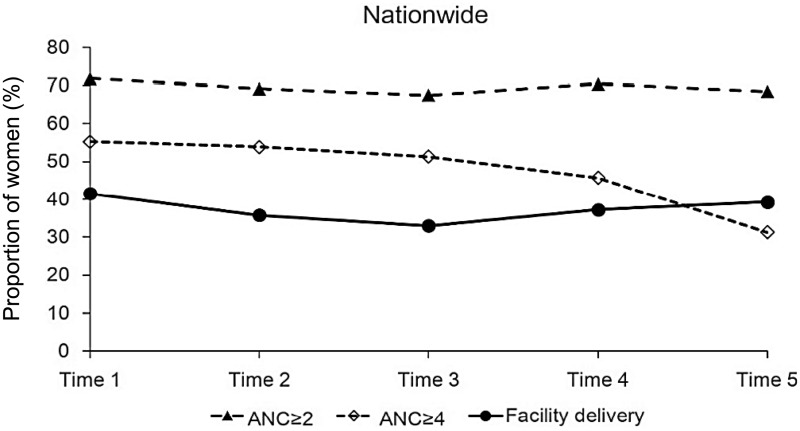
The TDHS data were available from 1991 to 2010. A total of 30 830 women who delivered their babies within 5 years at the time of survey in up to 52 districts were included for the analysis. Between 1991 and 2010, the national proportion of women who had more than four ANC visits during their last pregnancy had decreased from 56.1% to 33.3% as shown in Figure 1. In the same period, there was a decreasing trend in facility delivery followed by a relatively modest increase in the latter timeframe (50.3% in 1991–92, 38.4% in 1999 and 45.1% in 2009–10).
Figure 1.
Proportion of women with ANC visits > 2 or 4 and those delivered in health facility, nationwide (TDHS 1991–2010).
Table 1 summarizes key indicators according to different periods of the survey in urban and rural areas. The mean age, number of live births were higher in rural than urban area in all timeframes. On the other hand, percentage of media exposure, secondary education and facility delivery of women who gave birth within 5 years of the survey, as well as the proportion of nulliparous women, were consistently higher in urban than in rural areas throughout the study period. When the percentages of specific numbers of ANC visits were compared, the proportion of women who had two, three or more ANC visits has been higher in rural than in urban areas since 1996. For the percentage of ANC ≥ 4, there were no significant differences between urban and rural areas for Time points 1–4. Since 2004, some rural areas showed a higher proportion of women who had at least four ANC visits than in urban districts; this was the case in Dar es Salaam (63.8 in rural vs 55.5% in urban), Dodoma (56.3 in rural vs 47.4% in urban) and Town West (55.7 in rural vs 64.1% in urban; data of each district is not shown).
Table 1.
Comparison of maternal age, number of children, percentage of ANC, media exposure, education, nulliparity and facility delivery, urban and rural area
| Period regional indicators | Time 1 (1991–92) |
P | Time 2 (1996) |
P | Time 3 (1999) |
P | Time 4 (2004–05) |
P | Time 5 (2009–10) |
P | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | ||||||
| Maternal age (years) | 26.5 ± 0.3 | 27.8 ± 0.1 | < 0.01 | 26.2 ± 0.2 | 28.1 ± 0.1 | <0.01 | 25.7 ± 0.3 | 27.9 ± 0.2 | <0.01 | 26.2 ± 0.2 | 27.9 ± 0.1 | <0.01 | 26.7 ± 0.2 | 28.4 ± 0.1 | <0.01 |
| Number of live birth | 3.1 ± 0.1 | 3.6 ± 0.0 | <0.01 | 2.9 ± 0.1 | 3.6 ± 0.0 | <0.01 | 2.5 ± 0.1 | 3.5 ± 0.1 | <0.01 | 2.7 ± 0.1 | 3.5 ± 0.0 | <0.01 | 2.6 ± 0.1 | 3.6 ± 0.0 | <0.01 |
| % of ANC ≥ 1 | 99.1 | 95.7 | <0.01 | 99.7 | 97.2 | <0.01 | 99.5 | 96.9 | 0.01 | 97.3 | 96.9 | 0.57 | 99.0 | 97.9 | 0.07 |
| % of ANC ≥ 2 | 71.3 | 71.9 | 0.77 | 64.1 | 70.5 | <0.01 | 59.6 | 70.4 | <0.01 | 62.3 | 73.2 | <0.01 | 62.3 | 70.5 | <0.01 |
| % of ANC ≥ 3 | 69.3 | 67.1 | 0.25 | 61.8 | 66.7 | <0.01 | 57.1 | 64.3 | 0.01 | 58.1 | 65.7 | <0.01 | 55.5 | 58.6 | 0.06 |
| % of ANC ≥ 4 | 58.0 | 54.4 | 0.10 | 54.8 | 53.6 | 0.49 | 52.4 | 50.9 | 0.62 | 46.1 | 45.6 | 0.75 | 35.9 | 29.6 | <0.01 |
| Media exposure rate (%) | 77.5 | 38.4 | <0.01 | 74.4 | 34.6 | <0.01 | 50.7 | 20.5 | <0.01 | 86.2 | 57.5 | <0.01 | 82.6 | 53.3 | <0.01 |
| Secondary education rate (women) (%) | 8.1 | 1.2 | <0.01 | 11.5 | 1.6 | <0.01 | 13.3 | 2.3 | <0.01 | 15.4 | 2.1 | <0.01 | 20.3 | 3.8 | <0.01 |
| Secondary education rate (partner) (%) | 14.7 | 4.7 | <0.01 | 20.5 | 5.3 | <0.01 | 17.0 | 3.7 | <0.01 | 21.6 | 5.0 | <0.01 | 27.1 | 5.1 | <0.01 |
| Proportion of nulliparous women (%)(%) | 26.0 | 18.0 | <0.01 | 27.4 | 18.8 | <0.01 | 31.7 | 17.7 | <0.01 | 27.3 | 16.9 | <0.01 | 26.5 | 15.7 | <0.01 |
| Proportion of facility delivery (%) | 64.4 | 34.9 | <0.01 | 55.6 | 30.2 | <0.01 | 50.8 | 26.2 | <0.01 | 53.4 | 31.8 | <0.01 | 55.4 | 33.7 | <0.01 |
| Number of included regions | 12 | 42 | 43 | 52 | 50 | ||||||||||
ANC, antenatal care.
All the calculations were done with weighted value. All continuous variables are presented as mean ± standard error.
Table 2 summarizes the results of multivariable analysis including the proportion of women having ANC ≥ 4 in the districts. For both urban and rural data, Model 2, which assumes that the effect of different times is the same in all districts and that there is an autocorrelation structure within districts, showed the best fit for the data. In urban area, the percentage of mothers with ANC ≥ 4 and media exposure showed a positive association with the facility delivery rate. Model 2 indicates that if the percentage of women with ANC ≥ 4 increased by 10% then the facility delivery rate in the region would increase by 5%. However, in rural regions, the relationship between ANC ≥ 4 and facility delivery rate was not significant in all three models. According to models 2 in rural data, increase in mean number of live births by one in the region would reduce regional-facility delivery rate by 26%. On the other hand, the increased proportion of nulliparous women in the district by 10% would raise the facility delivery rate by 26%. Most of the relationships between key determinants including ANC visits and facility delivery were not changed with or without considering the autocorrelation structure for the within-districts variation in facility delivery rates. In all models, fixed effect of time points was not significant.
Table 2.
Result of with three mixed regression models for facility delivery rate in the district, urban and rural area (TDHS, 1991–2010)
| Covariates | Urban |
Rural |
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Time pointa | 1.01 | 1.01 | 1.02 | 0.96 | 0.96 | 0.96 |
| Mean maternal age | 0.99 | 0.99 | 0.99 | 1.10* | 1.10* | 1.11* |
| Mean number of total live birth | 1.08 | 1.08 | 1.07 | 0.74* | 0.74* | 0.73* |
| Secondary education rate (women)b | 0.99 | 1.02 | 1.02 | 0.93 | 0.90 | 0.88 |
| Secondary education rate (partner) | 0.98 | 0.94 | 0.94 | 1.10 | 1.13 | 1.15 |
| Media exposure rate | 1.03 | 1.05* | 1.04* | 1.03 | 1.03 | 1.03 |
| Proportion of nulliparous women | 1.07 | 1.06 | 1.05 | 1.26* | 1.26* | 1.27* |
| ANC ≥ 4 visits | 1.05 | 1.05* | 1.05* | 0.93 | 0.94 | 0.94 |
| AR(1) | P = 0.006 | P < 0.001 | P < .001 | P = 0.029 | ||
| AIC | 23.2 | 17 | 17.9 | 67.1 | 60.9 | 64.6 |
*P < 0.05, **P < 0.01, ***P < 0.001. All values are rounded down to second decimals.
ANC, antenatal care.
Model 1 indicates the random coefficient model without exploring the error (random coefficient model); Model 2 explores the correlation structures within the district and Model 3 contains the covariance between and within the district.
aRisk ratio in timeframe, mean maternal age and mean number of total live birth means that increment of facility delivery rate with increment of the numbers by one.
bRisk ratio in secondary education rate, ANC visits, media exposure and nulliparous women mean that increment of facility delivery rate with increment of the proportion by 10%.
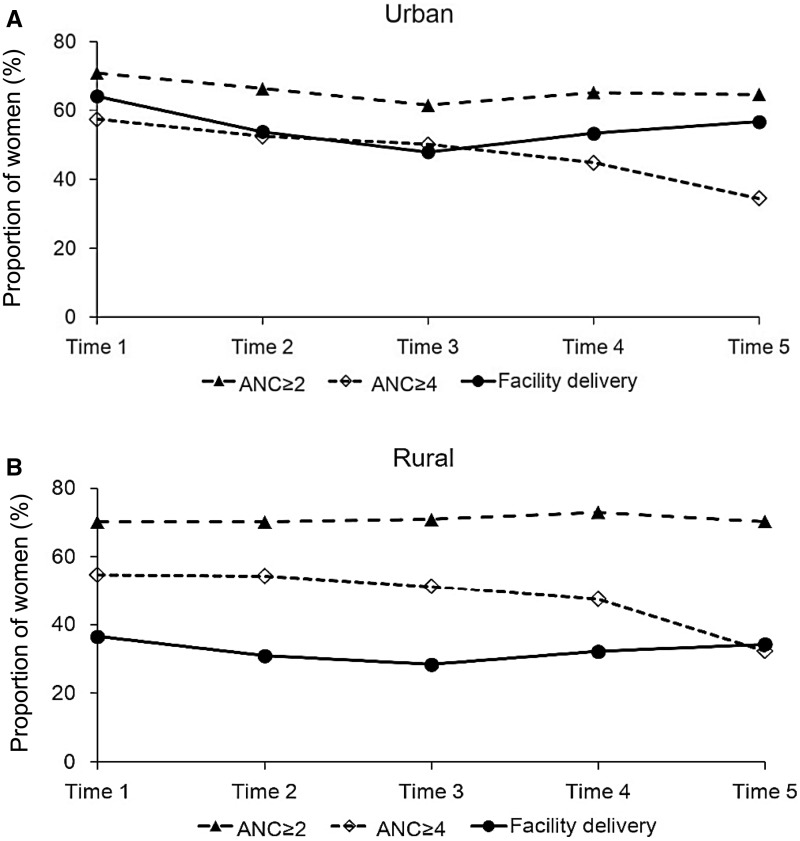
Longitudinal analyses of the proportion of women who had 1–4 ANC visits in urban and rural areas revealed that the association is different between the two areas (Table 3). An increase by 10% of the district percentage of women who had two or three ANC visits was related to 12–22% higher facility-based delivery rate in urban areas. For rural areas, there was no significant relationship between specific numbers of ANC visits and the facility-based delivery rate in all three models. As shown in Figure 2A and B, the change of facility delivery rate followed a similar trend of women having at least two ANC visits nationwide, in both urban and rural areas. The gap between ANC ≥ 2 and facility-based delivery rate was larger in rural areas than in urban areas.
Table 3.
Adjusted risk ratio of facility-based delivery according to percentage of women who had >1–4 ANC visits in three models, urban and rural area (TDHS, 1991–2010)
| Percentage of women in the area | Urban |
Rural |
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| ANC ≥ 1 | 1.12 | 1.10 | 1.12 | 0.93 | 0.93 | 0.93 |
| ANC ≥ 2 | 1.14*** | 1.13*** | 1.14*** | 0.92 | 0.92 | 0.92 |
| ANC ≥ 3 | 1.22*** | 1.11*** | 1.11*** | 0.94 | 0.92 | 0.92 |
| ANC ≥ 4 | 1.05 | 1.05* | 1.05* | 0.93 | 0.94 | 0.94 |
* P < 0.05, **P < 0.01, ***P < 0.001.
ANC, antenatal care.
Model 1 indicates the random coefficient model without exploring the error (random coefficient model); Model 2 explores the correlation structures within the district and Model 3 contains the covariance between and within the district. Risk ratio means that increment of facility delivery rate with increment of percentage of >1–4 ANC by 10%. All risk ratios were adjusted for covariates (time points, mean maternal age, mean number of total live birth, secondary education of women and partner, proportion of media exposure and nulliparous women).
Figure 2.
Proportion of women with ANC visits > 2 or 4 and those delivered in health facility, urban and rural area (TDHS 1991–2010).
For the exploration of the reasons for this gap between ANC and facility delivery, the responses to the question ‘Why didn’t you deliver in a health facility?’ in TDHS 2009–10 were analysed (Table 4). Among the 5244 women who had ANC visits at least once during their latest pregnancy in 2009–10, 2388 (45.5 %) reported that they did not deliver the baby in a health facility. In both urban and rural areas, ‘Too far/no transportation’ was the most frequent reason. And ‘not necessary’, ‘not customary’ and ‘cost’ were the other major inhibitory factors. When the proportions were compared, rural women reported more partner and familial factors than urban women (P = 0.04).
Table 4.
Reasons of home delivery in women with ANC visit more than once (N = 2388), urban and rural area (TDHS, 2009–10)
| Q: Why didn’t you deliver in a health facility? (Multiple responses) | % urban women (weighted n = 189) | % rural women (weighted n = 2356) | P value |
|---|---|---|---|
| Husband/family did not allow | 0.45 | 2.69 | 0.04 |
| Facility not open | 2.75 | 1.89 | 0.54 |
| Cost too much | 7.90 | 7.84 | 0.98 |
| Too far/no transportation | 33.17 | 42.93 | 0.09 |
| No female provider at the facilitya | 0.00 | 1.41 | 0.28 |
| Not necessary | 15.89 | 19.36 | 0.36 |
| Don’t trust facility/poor quality service | 1.83 | 1.57 | 0.83 |
| Not customary | 5.96 | 9.47 | 0.26 |
aPearson’s Chi-squared test with Yates’ continuity correction. All the calculations were done with weighted value.
Discussion
The findings in this study support the hypothesis that four or more ANC visits are not always associated with higher probability of facility-based delivery. Increase of ANC visits > 2–4 times was associated with higher facility delivery rate only in urban area. The proportion of at least four ANC visits was not related to facility delivery rates at the district level in rural Tanzania. This difference in the association between ANC visits and facility-based delivery rate could be one of the systemic factors causing persistent urban–rural disparity in facility-based delivery rate.
Contrary to the studies that have reported the positive relationship between ANC visits and facility delivery, Rockers et al. (2009) showed that a considerable proportion of women who had ANC did not go to a health facility for delivery in rural Tanzania. In addition, the declining trend in the rate of adequate ANC visits was not accompanied by a corresponding change in facility delivery incidence. Especially in rural areas, the percentages of women who had 1–4 ANC visits in the region were found to have no significant contribution to facility-based delivery rates. The gap between those who had ANC visits at least once and those who underwent facility-based delivery has been unexpectedly large nationally. More than 90% of women reported that they had visited a health facility (private or public) for ANC at least once, irrespective of urban or rural residence (National Bureau of Statistics Tanzania and ICF Macro 2011). The reason why some women who received ANC from a skilled provider, but did not deliver their babies in a health facility, is not yet clear. Limited evidence from TDHS 2009–10 shows several factors such as distance, cost and sociofamilial cultures as the leading cause of this gap. The findings of this study suggest that pregnant women in rural areas, who are found to have no abnormal findings during ANC visits, might not be motivated enough to visit a health facility given the expense and trouble. According to a recent quantitative study conducted in rural northeastern Tanzania, between 19 and 28% of women who had delivered in health facilities experienced disrespectful and/or abusive treatment from health providers during childbirth (Kruk et al. 2014). Generally positive attitude about ANC in this country despite its poor quality might have affected on the high prevalence of ANC visits <4 times (Mwifadhi et al. 2009; Nyamtema et al. 2012). This quality of care issue could have been one of the major inhibitory factors to facility-based delivery in rural settings. Because more than one-third (35.0%) of responses reported ‘other’ reasons for home delivery than these, further study using qualitative methods would explain the differences between urban and rural areas.
The origins of urban–rural differentials in facility-based delivery could be beyond the problem of accessibility. In Rahman’s (2008) research, the partner’s secondary education was a significant determinant in urban areas, while women’s secondary education and whether they read newspapers were found to be significant factors in rural Bangladesh. In a survey of rural Uganda, mass media exposure has no significant association with birth preparedness and showed a similar result as our study (Asp et al. 2014). Ndao-Brumblay et al. (2013) reported that nulliparous women are more likely to deliver their babies in health facilities than multiparous women in rural Tanzania. The proportion of nulliparous women was also found to be related with variation in regional-facility delivery rates over time in our rural data.
This study suggests policies focusing on improving accessibility to ANC to increase the number of ANC visits could be insufficient to promote facility delivery in rural setting. In urban area, expanding the coverage of ANC visits ≥ 2 times could be effective in increasing facility delivery rate. The barriers in the way from ANC to facility delivery and different determinants between urban and rural area should be investigated and considered when the policies are decided and implemented.
As a longitudinal study of data for the past two decades, this study has several limitations. The effects of education and media exposure could be associated with the level of household wealth which could not be included in the analyses. Studies have reported inconsistent result on the effect of poverty. Recent study in the three districts (urban and rural) of Tanzania indicated women in wealthiest quintile were three times more likely to have had delivered at health facilities (Exavery et al. 2014). On the other hand, survey research in rural area revealed that parity determines the odds of institutionalized delivery more than household poverty or education (Ndao-Brumblay et al. 2013). In the study on factors related with health facility childbirth, the association between socioeconomic position and facility childbirth was not significant in a rural district of Kenya (Ng’anjo Phiri et al. 2014). Household wealth data of further time points would enable us to measure the effect of longitudinal change of regional level of wealth.
A study using pseudo-panel data such as this one has its own limitations of unmeasured commonalities of units within the time points (Lebo and Weber 2014). This study used data collapsed into regional mean values at five time points to avoid debatable individual-level analyses. In addition, a relatively small number of cases in the first wave could be another limitation.
Despite these weaknesses, as the first longitudinal study on the relationships between the number of ANC visits and facility delivery using RCS data for two decades, the findings of this study may contribute to future investigation on the longstanding gap between ANC visits and facility delivery.
Conclusion
Undertaking more than one, two, three or even four ANC visits was not significantly associated with facility-based delivery in rural Tanzania. Different regional factors mediate the longitudinal changes in facility delivery rates between urban and rural areas. For more effective strategies to improve access to facility-based delivery and subsequent reduction of maternal mortality, these differences should be studied in greater depth.
Ethical approval
Only publicly available, anonymous data was used, the institutional review was not required.
Conflict of interest statement. None declared.
Acknowledgements
The authors are grateful for technical support from Jae Young Lee, Good Neighbors Korea and wish to acknowledge the DHS Program for granting access to the Tanzania Demographic and Health Survey data.
References
- AbouZahr CL. 1998. Lessons on safe motherhood. World Health Forum 19: 253–60. [PubMed] [Google Scholar]
- Abubakar A, Uriyo J, Msuya SE, Swai M, Stray-Pedersen B. 2012. Prevalence and risk factors for poor nutritional status among children in the Kilimanjaro region of Tanzania. International Journal of Environmental Research and Public Health 9: 3506–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amooti-Kaguna B, Nuwaha F. 2000. Factors influencing choice of delivery sites in Rakai district of Uganda. Social Science & Medicine 50: 203–13. [DOI] [PubMed] [Google Scholar]
- Anyait A, Mukanga D, Oundo GB, Nuwaha F. 2012. Predictors for health facility delivery in Busia district of Uganda: a cross sectional study. BMC Pregnancy and Childbirth 12: 132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asp G, Odberg Pettersson K, Sandberg J, Kabakyenga J, Agardh A. 2014. Associations between mass media exposure and birth preparedness among women in southwestern Uganda: a community-based survey. Global Health Action 7: 22904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S, Yoffe P, Hills N, Lustig RH. 2013. The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data. PLoS One 8: e57873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canavan ME, Sipsma HL, Kassie GM, Bradley EH. 2014. Correlates of complete childhood vaccination in East African countries. PLoS One 9: e95709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exavery A, Kanté AM, Njozi M, et al. 2014. Access to institutional delivery care and reasons for home delivery in three districts of Tanzania. International Journal for Equity in Health 13: 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feyissa TR, Genemo GA. 2014. Determinants of institutional delivery among childbearing age women in Western Ethiopia, 2013: unmatched case control study. PLoS One 9: e97194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finlayson K, Downe S. 2013. Why do women not use antenatal services in low- and middle-income countries? A meta-synthesis of qualitative studies. PLoS Medicine 10: e1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrysch S, Campbell OM. 2009. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth 9: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage AJ. 2007. Barriers to the utilization of maternal health care in rural Mali. Social Science & Medicine 65: 1666–82. [DOI] [PubMed] [Google Scholar]
- Gage AJ, Guirlène Calixte M. 2006. Effects of the physical accessibility of maternal health services on their use in rural Haiti. Population Studies 60: 271–88. [DOI] [PubMed] [Google Scholar]
- Kearns A, Hurst T, Caglia J, Langer A. 2014. Focused Antenatal Care in Tanzania. Women and Health Initiative & Maternal Health Task Force. http://www.mhtf.org/wp-content/uploads/sites/32/2014/09/HSPH-Tanzania5.pdf, accessed 4 March 2015. [Google Scholar]
- Kitui J, Lewis S, Davey G. 2013. Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy and Childbirth 13: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Kujawski S, Mbaruku G, et al. 2014. Disrespectful and abusive treatment during facility delivery in Tanzania: a facility and community survey. Health Policy and Planning : 1–8. [DOI] [PubMed] [Google Scholar]
- Kruk ME, Mbaruku G, Rockers PC, Galea S. 2008. User fee exemptions are not enough: out-of-pocket payments for ‘free’ delivery services in rural Tanzania. Tropical Medicine & International Health 13: 1442–51. [DOI] [PubMed] [Google Scholar]
- Lebo MJ, Weber C. 2014. An effective approach to the repeated cross-sectional design. American Journal of Political Science 59: 242–58. [Google Scholar]
- Maletnlema TN. 2002. A Tanzanian perspective on the nutrition transition and its implications for health. Public Health Nutrition 5: 163–8. [DOI] [PubMed] [Google Scholar]
- Mella PP. 2003. Major factors that impact on women’s health in Tanzania: the way forward. Health Care for Women International 24: 712–22. [DOI] [PubMed] [Google Scholar]
- Ministry of Health. 2013. National Health Policy. United Republic of Tanzania. https://www.healthresearchweb.org/files/Tanzania%20National%20Health%20Policy%202003.pdf, accessed 2 March 2015. [Google Scholar]
- Moyer CA, Mustafa A. 2013. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reproductive Health 10: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mujinja PGM, Kida TM. 2014. Implications of health sector reforms in Tanzania: Policies, indicators and accessibility to health services. Tanzania Human Development Report 2014: Background Paper No 8. Economic and Social Research Foundation Discussion Paper 62. Dar es Salaam, Tanzania: The Economic and Social Research Foundation. [Google Scholar]
- Mwifadhi M, Brigit O, Joanna Schellenberg A, et al. 2009. The use of antenatal and postnatal care: perspectives and experiences of women and health care providers in rural southern Tanzania. BMC Pregnancy and Childbirth 9: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Bureau of Statistics Tanzania and ORC Macro. 2000. Reproductive and Child Health Survey 1999. Dar es Salaam, Tanzania: National Bureau of Statistics and ICF Macro. [Google Scholar]
- National Bureau of Statistics Tanzania and ORC Macro. 2005. Tanzania Demographic and Health Survey 2004–05. Dar es Salaam, Tanzania: National Bureau of Statistics and ORC Macro. [Google Scholar]
- National Bureau of Statistics Tanzania and ICF Macro. 2011. Tanzania Demographic and Health Survey 2010. Dar es Salaam, Tanzania: National Bureau of Statistics and ICF Macro. [Google Scholar]
- Ndao-Brumblay SK, Mbaruku G, Kruk ME. 2013. Parity and institutional delivery in rural Tanzania: a multilevel analysis and policy implications. Health Policy and Planning 28: 647–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng’anjo Phiri S, Kiserud T, Kvale G, et al. 2014. Factors associated with health facility childbirth in districts of Kenya, Tanzania and Zambia: a population based survey. BMC Pregnancy and Childbirth 14: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamtema A, Jong A, Urassa D, Hagen J, van Roosmalen J. 2012. The quality of antenatal care in rural Tanzania: what is behind the number of visits? BMC Pregnancy and Childbirth 12: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen OE, Ndeki S, Norheim OF. 2005. Availability, distribution and use of emergency obstetric care in northern Tanzania. Health Policy and Planning 20: 167–75. [DOI] [PubMed] [Google Scholar]
- Pervin J, Moran A, Rahman M, et al. 2012. Association of antenatal care with facility delivery and perinatal survival - a population-based study in Bangladesh. BMC Pregnancy and Childbirth 12: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer C, Mwaipopo R. 2013. Delivering at home or in a health facility? health-seeking behaviour of women and the role of traditional birth attendants in Tanzania. BMC Pregnancy and Childbirth 13: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman M. 2008. Factors associated with delivery assistance: does differentials exist between rural and urban areas in Bangladesh? The Internet Journal of Family Practice 7:2. [Google Scholar]
- Rockers PC, Wilson ML, Mbaruku G, Kruk ME. 2009. Source of antenatal care influences facility delivery in rural Tanzania: a population-based study. Maternal and Child Health Journal 13: 879–85. [DOI] [PubMed] [Google Scholar]
- Simkhada B, Teijlingen ER, Porter M, ` P. 2008. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. Journal of Advanced Nursing 61: 244–60. [DOI] [PubMed] [Google Scholar]
- Tanzania Gender Networking Program (TGNP) and Macro Internationa1 Inc., 2007 Women’s Health in Tanzania. Dar es Salaam Tanzania: TGNP and Macro International Inc. [Google Scholar]
- Trujillo JC, Carrillo B, Iglesias WJ. 2013. Relationship between professional antenatal care and facility delivery: an assessment of Colombia. Health Policy and Planning 29: 443–9. [DOI] [PubMed] [Google Scholar]
- von Both C, Flessa S, Makuwani A, Mpembeni R, Jahn A. 2006. How much time do health services spend on antenatal care? Implications for the introduction of the focused antenatal care model in Tanzania. BMC Pregnancy Childbirth 6: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfinger RD. 1996. Heterogeneous variance: covariance structures for repeated measures. Journal of Agricultural, Biological, and Environmental Statistics 1: 205–30. [Google Scholar]
- World Health Organization. 2012. Trends in Maternal Mortality: 1990 to 2010, WHO, UNICEF, UNFPA and the World Bank Estimates. Geneva: WHO. http://whqlibdoc.who.int/publications/2012/9789241503631_eng.pdf, accessed 4 November 2014. [Google Scholar]
- World Health Organization, Department of Making Pregnancy Safer. 2006. Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. Geneva: WHO. http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/effective_antenatal_care.pdf, accessed 4 November 2014. [Google Scholar]
- Worku AG, Yalew AW, Afework MF. 2013. Factors affecting utilization of skilled maternal care in Northwest Ethiopia: a multilevel analysis. BMC International Health and Human Rights 13: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]