Abstract
Traditional medicine is commonly assumed to be a crucial health care option for poor households in developing countries. However, little research has been done in Asia to quantify the reliance on traditional medicine and its determinants. This research contributes to filling in this knowledge gap using household survey data collected from 571 households in three rural and peri-urban sites in Nepal in 2012. Questions encompassed household socioeconomic characteristics, illness characteristics, and treatment-seeking behaviour. Treatment choice was investigated through bivariate analyses. Results show that traditional medicine, and especially self-treatment with medicinal plants, prevail as treatment options in both rural and peri-urban populations. Contrarily to what is commonly assumed, high income is an important determinant of use of traditional medicine. Likewise, knowledge of medicinal plants, age, education, gender and illness chronicity were also significant determinants. The importance of self-treatment with medicinal plants should inform the development of health policy tailored to people’s treatment-seeking behaviour.
Keywords: Determinants, health care, medicinal plants, Nepal, self-treatment, South Asia, traditional medicine
Key Messages
Traditional medicine, and especially self-treatment with medicinal plants, prevail as treatment options for rural as well as peri-urban populations.
High income and knowledge of medicinal plants are important determinants of use of traditional medicine. This challenges the common assumption that poor and marginalized people are most reliant on traditional medicine due to its availability.
Future health policies shall consider the high reliance on self-treatment and the importance of knowledge held within the household in relation to this.
Introduction
Traditional medicine continues to play an important role in improving and maintaining health in developing countries (Cunningham et al. 2008). WHO defines traditional medicine as ‘diverse health practices, approaches, knowledge and beliefs incorporating plant, animal, and/or mineral based medicine, spiritual therapies, manual techniques and exercises applied singularly or in combination to maintain well-being, as well as to treat, diagnose or prevent illness’ (WHO 2002, p.7). Policies for the integration of traditional medicine into public health care systems have to varying extents been formulated in some countries (WHO 2001) and the share of the population using traditional medicine are reported to be as high as 40% in China and 80% in Africa (WHO 2002). As a consequence of the pluralistic nature of health care systems, people’s treatment-seeking behaviour is characterized by the use of multiple treatment types sequentially or simultaneously (Weller et al., 1997; Ryan 1998). Many studies on treatment-seeking behaviour in developing countries include only people’s first treatment choice (Ahmed et al. 2000a; Pillai et al. 2003; Pokhrel and Sauerborn 2004). To fully understand the importance of traditional medicine it is, however, necessary not to confine analyses solely to first recourse treatments, as the real patterns of traditional medicine utilization might only be revealed when including multiple recourses (Sato 2012a).
The geographical coverage of studies quantifying the use of traditional medicine and its socioeconomic determinants is uneven across developing countries, and focus is generally on Africa (Pouliot 2011; Sato 2012b; Chenge et al. 2014). Despite the diversity of medical traditions prevailing in Asia, few studies quantify the reliance on traditional medicine, except a few illness-specific studies (Chaturvedi et al. 2009) and studies on whether households have ever used traditional medicine (Sydara et al. 2005). Furthermore, traditional medicine is not a homogenous entity (Frank and Stollberg 2002) and many studies fail to capture the full range of traditional treatments which may be available to people, leading to underreport of actual utilization. Practices of self-treatment with or without the use of traditional medicines are sometimes completely excluded from studies (Pillai et al. 2003; Mayxay et al. 2013) despite the continued evidence that such practices prevail (Cocks and Dold 2000; Mathez-Stiefel et al. 2012). Many studies quantifying the use of ‘informal’ treatment practices do not pay specific attention to traditional types of medicine and instead group all treatment types other than visits to allopathic treatment facilities into the same treatment category [e.g. traditional healer treatments are grouped together with pharmacy visits, e.g. Sreeramareddy et al. (2006), Chenge et al. (2014)].
Traditional medicine is generally considered highly available and accessible to people in developing countries (e.g. Anyinam 1987). Consequently, poor and marginalized people are commonly assumed to be most reliant on traditional medicine for their healthcare (Cunningham et al. 2008). Differences in reliance have also been observed between rural and urban areas (Chaturvedi et al. 2009). However, those patterns have rarely been studied in Asia, and little is known on the determinants of traditional medicine use. How many people are reliant on traditional medicine and what factors determine this reliance? For example, while traditional knowledge of medicinal plants has been studied in ethnobotanic and ethnoecological research (Bhattarai et al. 2010), the link between traditional knowledge and use of traditional medicine in general and medicinal plants in particular has rarely been documented. This study uses data on treatment-seeking behaviour to quantify the reliance on traditional medicine as well as its household-level determinants in Nepal.
In Nepal, several medical systems are utilized by the population, but not all of these are recognized by the government. Allopathic medicine has been prioritized by the government since its inclusion into Nepalese health care policy in the 1950s (Cameron 2008). Ayurveda was formally recognized and a policy of Ayurveda formulated in 1996. This policy encompassed establishment and further development of ayurvedic health care facilities, education and human resource development, research as well as the manufacturing of medicines from local medicinal plants (Department of Ayurveda 1996). More specific activities for the development of Ayurveda were outlined in the second Nepal Health Sector Programme, e.g. promoting the collection of locally available herbs and introducing Local Ayurveda Kits for Health programme (Ministry of Health and Population 2010). Other types of traditional treatments utilized by the population include self-treatment with medicinal plants, spiritual healing by Dhami-Jhankris, a healing tradition using chanting, possession states and animal sacrifices (Biswas et al. 2000), as well as traditional Tibetan doctors (Amchis) and traditional healers using locally available medicinal plants (Koirala 2007). Nepal has a doctor to patient ratio of around 1:5000 (UNDP 2013), but this figure varies greatly between urban and rural areas. In contrast, a study from 1996 carried out in 6 Village Development Committees identified 408 traditional healers using locally available medicinal plants to treat illnesses, corresponding to an average healer to patient ratio of 1:39 (Himalayan Ayurveda Research Institute 1996). Though very limited in geographical scope, this study provides the best indicator of the availability of healers in rural Nepal. The continued importance and utilization of medicinal plants for health care are frequently reported in studies listing known medicinal plants in different locations in Nepal (Bhattarai et al. 2010; Uprety et al. 2010). None of these studies, however, quantify actual use. The objective of this article is hence to quantify the use of traditional medicine and the use of medicinal plants for self-treatment as well as their determinants. By studying not only the types of medicine included in current government policy in Nepal, but rather the variety of treatments practiced by the population, this research aims to improve our understanding of treatment-seeking behaviour which may inform the development of better targeted health interventions and policies.
Conceptual framework
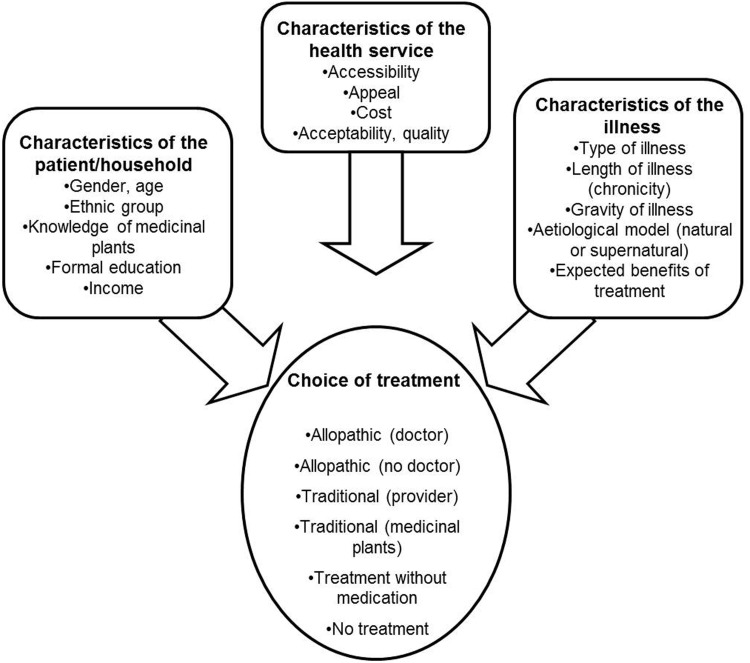
The conceptual framework used in this study is based on Kroeger’s determinant model (Kroeger 1983) and was adapted to the local situation. As medicinal plant consumption has widely been studied by looking at people’s medicinal plant knowledge (Giovannini et al. 2011; Bignante and Tecco 2013), we include the explanatory variable ‘knowledge of medicinal plants’ in the framework (Figure 1). The model suggests that patient choice of treatment is a function of three groups of factors: characteristics of (i) the patient/household; (ii) the health service; and (iii) the illness. Treatments and providers are grouped into five treatment types, making up the dependent variables. ‘Allopathic (doctor)’ includes treatments from public and private health care facilities such as hospitals and clinics where educated doctors are available. ‘Allopathic (no doctor)’ includes treatments from health posts and dispensaries where no doctors are available. ‘Traditional (provider)’ consists of treatments from Ayurvedic health care facilities, Ayurvedic dispensaries, traditional healers, Tibetan Amchis or spiritual healers whereas ‘traditional (self-treatment)’ includes self-treatment with medicinal plants. Finally ‘treatment without medication’ consists of any action taken as a response to an illness, such as drinking hot water, putting on warm clothes, resting or sleeping, excluding any intakes of medicines and medicinal plants.
Figure 1.
Determinants influencing choice of treatment. Conceptual framework adapted from Kroeger’s model (Kroeger, 1983).
Methods
Study area
Nepal is one of the poorest countries in the world with 57.3% of the population living on less than 2 USD a day (World Bank 2014). The country is ranked 145th out of 187 countries on the Human Development Index and had in 2012 a total population of 31 million of which 17.3% lived in urban areas (UNDP 2013). Life expectancy is 68.8 years (UNDP 2014). Public health services are provided through a system of 3129 sub-health posts, 676 health posts, 209 primary health care centers and 65 district hospitals. Additionally, there are zonal/regional/central level hospitals providing specialized care. Public Ayurvedic health services are also provided through 214 Ayurveda dispensaries, 61 district Ayurveda health centers, and a total of 16 zonal/central level Ayurveda hospitals (Department of Health Services 2012). Nepal also has a large private health sector, receiving about half of all outpatient visits for acute illnesses (WHO 2007). Health care delivery is a challenge in the hilly and mountainous parts of the country due to the lack of infrastructure (Bentley 1995).
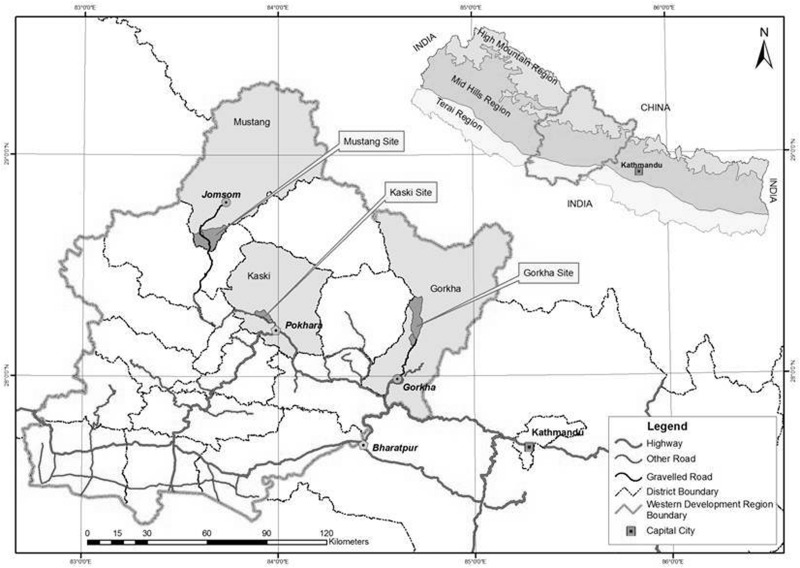
Data were collected in three sites located in the Mid-Hills and High Mountain regions and representing differences in availability of health care facilities, livelihoods and accessibility to roads and towns. All sites are located in the Western Development Region: (i) Mustang District in the high mountains, hereafter referred to as the rural mountain site; (ii) mid-hills in Kaski District, peri-urban site; (iii) Gorkha District, rural hills site (Figure 2). Summary characteristics of the sites are shown in Table 1. Public primary health care facilities are available in all sites as are Dhami-Jhankris. All sites also have dispensaries where the owner provides check-ups and minor health advice in addition to selling allopathic and sometimes Ayurvedic medicines. Private allopathic and Ayurvedic facilities are accessible within 1 hour’s travel in the peri-urban site and more than half a day in the rural sites. Two traditional healers providing treatments for fractures only are available in the rural mountain site whereas four traditional healers are available in the rural hills site. Traditional healers are not present in the peri-urban site. Medicinal plants are available from gardens, fields or forests in all sites and sellers of Ayurvedic medicine or medicinal plants come to all sites on an irregular basis.
Figure 2.
Study sites. The Mustang site is also referred to as the rural mountain site, Kaski site as the peri-urban site and Gorkha site as the rural hills site.
Table 1.
Site characteristics
| Kaski district—peri-urban site | Gorkha district—rural hills site | Mustang district—rural mountain site | |
|---|---|---|---|
| District Human Development Index valuesa | 0.576 | 0.481 | 0.508 |
| Major caste/ethnic groupsb | Chhetri and Brahmin | Gurung | Thakali and Dalit |
| Nearest hospital | 15 km (1/2 h private car or motorbike/1 h bus) | Min. 45 km (min. 1 h walk + 5 h bus) | Min. 28 km (min. 3 h bus) |
| Nearest road | 0 min to paved road | Min. 1 h walk to dry weather road | 0–2 h walk to dry weather road |
| Populationc | 12 262 | 5712 | 1550 |
| Householdsc | 3019 | 1257 | 396 |
| Sampled households | 116 | 275 | 180 |
Data collection
An initial questionnaire focusing on household demographics, income and assets was administered in 2012 on a quarterly basis to 571 randomly selected households as part of the ComForM project (for details see Larsen et al. 2014). Households were selected by random sampling in a first survey round conducted in 2006 based on either census lists or (in Kaski) lists of members of forest user groups. Some households left the survey due to for example migration between 2006 and 2012. The main respondent was the household head, though other household members occasionally joined the interview. Local enumerators with at least 8 years of schooling administered the questionnaire. A questionnaire on health-seeking behaviour was administered in September and October 2012 in the same households (following testing outside the frame in July 2012), focusing on (1) illness episodes faced by household members including symptoms, length of illness, and whether the patient stayed in bed or not; (2) treatments carried out during each illness episode and characteristics of these; e.g. type of treatment, sequence of treatment, costs and previous experience with treatment; (3) patient characteristics such as age, gender and education; (4) information about the use of medicinal plants. Verbal informed consent was obtained for this particular part of the questionnaire.
Following other treatment-seeking studies (e.g. Sepehri et al. 2008; Pouliot 2011; Seeberg et al. 2014), illness episodes recorded were based on self-reporting of illnesses experienced within a 1-month recall period, as well as chronic illnesses currently experienced by household members. When asked about treatments, respondents were specifically asked to include all actions taken—and not only visits to providers outside the household—in order to capture practices of self-treatment. As respondents are likely to better remember treatments associated with high out-of-pocket expenditures or severe illnesses (Das et al. 2012), we specifically prompted about treatments used within the household, e.g. treatments without medication. All types of treatments, from drinking hot water to visiting hospitals, were hence recorded. Prior ethical approval for the study was received from Nepal Health Research Council and all participants gave their informed consent.
Model and analysis
In line with previous studies of determinants of the use of allopathic (Develay et al. 1996; Weller et al. 1997) and traditional medicine (Pouliot 2011; Sato 2012b), we use probit models to capture the influence of patient, household and illness characteristics on: (1) overall traditional medicine use (encompassing both self-treatment and treatment from providers), and (2) self-treatment with medicinal plants (a subcomponent of traditional medicine use). Based on previous studies (Pouliot 2011), determinants of the use of medicinal plants for self-treatment are expected to be different from the determinants of traditional medicine use; hence, the need for running two separate models.
The probit model is a binary response model in which the response variable can take only the values 0 and 1. The predicted values of a probit model are thus interpreted as a probability, specifically, the probability that an ill person will use traditional medicine or medicinal plants. The covariates explain the response variable through a function G of patient/household, health service and illness specific attributes ‘x’ and assumes that e is normally distributed such that
| (1) |
Where y = 1[y* > 0] and y* = βx + e.
Variables hypothesized to be significant determinants of traditional medicine/medicinal plant consumption were initially included in the models. These encompass patient/household characteristics (age, gender, education, income, ethnic group, knowledge of medicinal plants), health service characteristics (accessibility to medical facilities) and illness characteristics (chronicity and severity). Insignificant variables were sequentially removed until all remaining variables met the criteria for inclusion (P < 0.1 for at least one of the models). The descriptive statistics of the variables included in the empirical model and their expected effect on the use of traditional medicine/medicinal plants are presented in Table 2.
Table 2.
Expected signs and description of the independent variables used in the analyses
| Variables | Expected sign | References |
|---|---|---|
| Child (10 and below) | − | Traditional medicine is used less when seeking treatment for ill children than for other age groups (Kleinman 1980; Sato 2012b). This is the case both when seeking traditional providers (Pouliot 2011) and using traditional types of self-treatment (Gedif and Hahn 2003; Pouliot 2011) |
| Elder (60 and above) | + | Elders are more often using traditional medicine (Kleinman 1980; Gedif and Hahn 2003) |
| Household headed by a female | +/− | Use of allopathic maternal health services are reported to be highly influenced by the position of women within the household (Furuta and Salway 2006). Thorsen (2015) reports that households headed by females have limited access to medicinal plants when those are collected far from the house |
| Education of household head (years) | − | Patients from households with educated heads of households were less likely to use traditional medicine for treating febrile illness in north-east India (Chaturvedi et al. 2009) and sought care from individuals with allopathic professional medical training more often in Bangladesh (Ahmed et al. 2000a). Pouliot (2011) also reported that households with lower education levels used traditional self-treatment at a higher frequency |
| Chronic | + | The longer an illness episode, the more likely that patients recourse to traditional medicine (Kroeger 1983;; Develay 1996; Pouliot 2011; Sato 2012a). Sepheri et al. (2008) reported that the longer the illness lasts, the more likely that people seek care instead of using self-treatment or no treatment |
| Rich (4th or 5th inc quintile) | +/− | Although lower economic status increases child health care seeking from traditional providers (Pillai et al. 2003) and increasing income leads to a decrease in traditional medicine use (Sato 2012b), Pouliot (2011) finds that higher income leads to increased use of traditional medicine providers. For self-treatment with traditional medicine, higher income, however, decreases consumption (Pouliot 2011). Higher income reduces the likelihood of households using any type of self-treatment (Sepehri et al. 2008) |
| Knowledge of medicinal plants (in household) | + | People stated knowledge of required ingredients as an important factor when deciding to use traditional medicines for self-treatment (Edgeworth and Collins 2006). Budhathoki and BC (2008) reported decreasing medicinal plant use when resettling due to lack of knowledge of medicinal plants in the new location |
| Location (rural) | + | Traditional medicine use is more prevalent in rural than in town areas (Pillai et al. 2003; Chaturvedi et al. 2009) and access to allopathic medicine facilities increases the use of this type of medicine (Sato 2012b) |
Due to the fact that the selected study sites are very different in terms of socioeconomic characteristics and infrastructure, we ran the probit models for each site separately to study if the same variables determined traditional medicine/medicinal plant consumption in the three sites. Income quintiles were generated by dividing the sample in five equal groups based on reported total net annual household income. Again, because sites differ tremendously, computation of income quintile groups was done separately for each site. The regression results differed between the sites and are presented separately.
Through the StataIC/12 programme, we used the probit command with a Huber/Whites sandwich standard error estimator ((vce(robust)). Tests of normality and homoscedasticity of residuals were also conducted.
Results
Among the 571 sampled households (with a total of 3095 household members), 535 reported at least one illness episode during the past four weeks. The total number of illness episodes reported was 1129, meaning that the average morbidity rate was 36.4% (34.1% in the rural mountain site, 42.4% in the peri-urban site, and 35.6% in the rural hills site). Overall, 16% of the reported illness episodes were chronic illnesses (Table 3). The average number of treatments per illness episode was 2.1, and this value did not show significant variation between sites. For 25 illnesses (10 in the rural mountain site and 15 in the rural hills site), no treatment was sought. Almost one-third (31%) of the reported illness episodes were treated using traditional medicine at some point during the treatment-seeking strategy (Table 3). Many types of traditional treatments were used by ill people in the sample (Table 4), the most common of them being self-treatment with medicinal plants (66.8% of the traditional medicine used was in the form of medicinal plants). In fact, 22% of the ill people used medicinal plants at some point during their treatment-seeking strategy (Table 3). The high frequency of usage of this specific type of traditional treatment warrants focusing parts of the analysis on the determinants of its consumption, and this will be done in the following section.
Table 3.
Descriptive statistics for variables used in the models
| Variables | Rural mountain (n = 310) |
Peri-urban (n = 252) |
Rural hills (n = 567) |
Total (n = 1129) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std. Dev. | Min | Max | Mean | Std. Dev. | Min | Max | Mean | Std. Dev. | Min | Max | Mean | Std. Dev. | Min | Max | |
| Use of traditional medicine (0/1) | 0.46 | 0.50 | 0 | 1 | 0.15 | 0.36 | 0 | 1 | 0.30 | 0.46 | 0 | 1 | 0.31 | 0.46 | 0 | 1 |
| Use of medicinal plants (0/1) | 0.33 | 0.47 | 0 | 1 | 0.12 | 0.32 | 0 | 1 | 0.21 | 0.41 | 0 | 1 | 0.22 | 0.42 | 0 | 1 |
| Child (10 and below) (0/1) | 0.18 | 0.39 | 0 | 1 | 0.18 | 0.38 | 0 | 1 | 0.20 | 0.40 | 0 | 1 | 0.19 | 0.39 | 0 | 1 |
| Elder (60 and above) (0/1) | 0.22 | 0.41 | 0 | 1 | 0.27 | 0.44 | 0 | 1 | 0.16 | 0.37 | 0 | 1 | 0.20 | 0.40 | 0 | 1 |
| Household headed by a female (0/1) | 0.26 | 0.44 | 0 | 1 | 0.21 | 0.41 | 0 | 1 | 0.18 | 0.38 | 0 | 1 | 0.21 | 0.41 | 0 | 1 |
| Education of household head (years) | 2.69 | 3.97 | 0 | 13 | 6.96 | 5.21 | 0 | 18 | 1.35 | 2.88 | 0 | 16 | 2.97 | 4.41 | 0 | 18 |
| Chronic (0/1) | 0.15 | 0.36 | 0 | 1 | 0.30 | 0.46 | 0 | 1 | 0.11 | 0.31 | 0 | 1 | 0.16 | 0.37 | 0 | 1 |
| Rich (4th or 5th income quintile) (0/1) | 0.39 | 0.49 | 0 | 1 | 0.39 | 0.49 | 0 | 1 | 0.40 | 0.49 | 0 | 1 | 0.39 | 0.49 | 0 | 1 |
| Knowledge of medicinal plants (in household) (0/1) | 0.93 | 0.26 | 0 | 1 | 0.78 | 0.42 | 0 | 1 | 0.49 | 0.50 | 0 | 1 | 0.67 | 0.47 | 0 | 1 |
Table 4.
Frequency of use of different traditional treatment types
| Traditional treatment | Frequency (n) | Share (%) | |
|---|---|---|---|
| Self-treatment with medicinal plants | 288 | 66.8 | |
| Private ayurvedic doctor | 2 | 0.5 | |
| Tibetan/Amchi doctor | 2 | 0.5 | |
| Traditional healer | 18 | 4.2 | |
| Spiritual healers (Dhami-Jhankri) | 93 | 21.6 | |
| Ayurvedic medical shop | 28 | 6.4 | |
| Total | 431 | 100 |
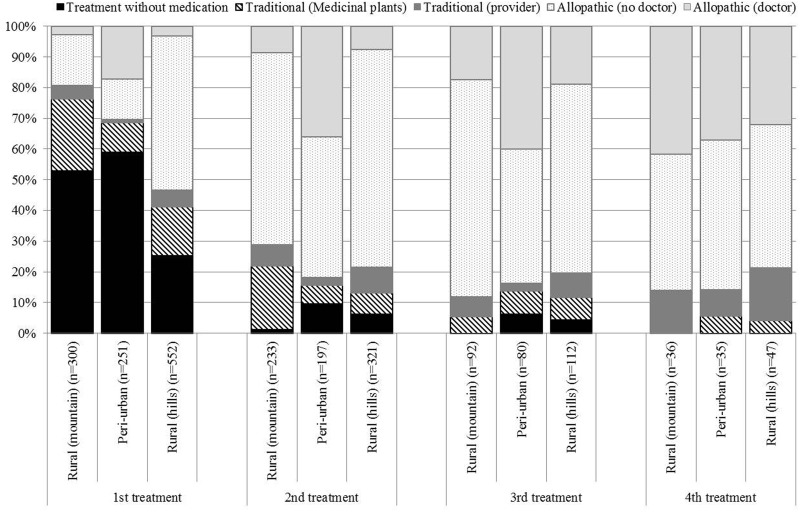
Figure 3 presents a site-level overview of treatment types and their sequence. For example, respondents used treatment without medication in close to 60% of cases as a first treatment in the peri-urban site. This figure is lower in the rural sites and especially in the rural hills site where it was only 25%. Traditional medicine was used by a considerable number of ill people. In total, it was used by 21% of respondents as the first treatment, by 17% as the second treatment, 13% as the third treatment and 17% as the fourth treatment. Note that not all ill people had recourse to more than one treatment (see sample sizes for different treatment sequences in Figure 3). The type of traditional medicine used changed during the treatment-seeking strategy. A higher share of ill people had recourse to traditional medicine providers at later stages of their treatment-seeking strategy in all three sites; only 3% of respondents used traditional medicine providers as a first treatment, while close to 13% of the respondents having recourse to a fourth treatment used traditional medicine providers. Self-treatment with medicinal plants was the most often used type of traditional medicine in all sites as both a first and second recourse treatment. The rural mountain site is the site where self-treatment with medicinal plants was the most important (in shares), followed by the rural hills site. In the peri-urban site, only around 10% of ill people reported using medicinal plants for self-treatment as a first recourse treatment.
Figure 3.
Share of respondents reporting different treatment types, by treatment sequence and site.
Several determinants of traditional medicine use were found (Table 5). First, in the rural mountain site, children were less likely to be treated with traditional medicine than other household members. Oppositely, being an elder increased the likelihood of traditional medicine use in both rural sites. Moreover, in the rural hills site, households headed by a more educated person were less likely to consume traditional medicine. In the same site, having a chronic illness increased the probability of having recourse to traditional medicine. Belonging to the most wealthy income quintile groups was a significant positive determinant of traditional medicine use in the rural mountain and peri-urban sites. In all sites, households who reported to hold knowledge of medicinal plants were more likely to use traditional medicine.
Table 5.
Determinants of traditional medicine and medicinal plant use
| Variables | Coefficients for determinants of use of traditional medicinea |
Coefficients for determinants of use of medicinal plants |
||||
|---|---|---|---|---|---|---|
| Rural mountain (n = 310) | Peri-urban (n = 252) | Rural hills (n = 567) | Rural mountain (n = 310) | Peri-urban (n = 252) | Rural hills (n = 567) | |
| Child | −0.47 (0.20)** | −0.01 (0.29) | −0.22 (0.16) | −0.41 (0.21)* | −0.64 (0.33)* | −0.44 (0.19)** |
| Elder | 0.32 (0.18)* | −0.38 (0.25) | 0.45 (0.15)** | 0.15 (0.19) | −0.42 (0.25)* | 0.44 (0.16)** |
| Household headed by a female | −0.16 (0.18) | 0.11 (0.28) | −0.20 (0.16) | −0.32 (0.18)* | 0.07 (0.28) | −0.19 (0.17) |
| Education of household head | 0.006 (0.02) | −0.01 (0.02) | -0.05 (0.02)** | −0.01 (0.02) | −0.04 (0.02)* | -0.06 (0.02)** |
| Chronic | −0.10 (0.22) | 0.20 (0.23) | 1.04 (0.18)*** | −1.06 (0.27)*** | 0.30 (0.25) | 0.37 (0.18)** |
| Rich | 0.28 (0.16)* | 0.50 (0.21)** | −0.11 (0.12) | 0.11 (0.16) | 0.44 (0.22)** | −0.28 (0.13)** |
| Knowledge of medicinal plants | 1.40 (0.40)*** | 1.26 (0.40)** | 0.51 (0.12)*** | 1.03 (0.39)** | 0.52 (0.13)*** | |
| Constant | −1.47 (0.43)*** | −2.29 (0.43)*** | −0.81 (0.11)*** | −1.19 (0.42)** | −1.09 (0.27)*** | −0.95 (0.12)*** |
aValues in bracket are standard errors.
*Significant at 10% level, ** Significant at 5% level, *** Significant at 1% level.
Determinants of self-treatment with medicinal plants differed from those of traditional medicine to some extent (Table 5). Differences worth mentioning are: (1) being an elder was shown to affect medicinal plant consumption negatively in the peri-urban site; (2) individuals from households headed by a woman were less likely to consume medicinal plants in the rural mountain site; (3) having a chronic illness decreased the incidence of medicinal plant consumption in the rural mountain site, while it increased it in the rural hills site; (4) being from a household belonging to the fourth or fifth income quintile increased the chances of consuming medicinal plants in the peri-urban site, while it decreased them in the rural hills site. Knowledge of medicinal plants was still a very important determinant of medicinal plant consumption in all sites. For the peri-urban site, this variable had to be excluded from the model to avoid perfect prediction, as all the respondents who had recourse to medicinal plants reported having knowledge of medicinal plants.
Discussion
Morbidity
Slightly above one-third (36.4%) of the people in the sample reported having suffered an illness during the 4 weeks preceding the interview. This is comparable with the illness incidents reported in the latest Living Standard Survey in Nepal (20% acute illness and 12% chronic illness) (Central Bureau of Statistics 2011) and elsewhere, with reported prevalence of illness of 15–40% of sampled populations (Kroeger et al. 1988; Develay et al. 1996; Hotchkiss et al. 1998; Pouliot 2011). Prevalence of illness differed between the sites and peaked in the peri-urban site at 42.4%. The site difference may be due to variation in illness perception with more prevalent underreporting among poorer households for which illnesses are seen as a part of daily lives (Das et al. 2012; Seeberg et al. 2014). Overall, 16% of the reported illness episodes were chronic illnesses, again with variability between sites and a maximum of 30% in the peri-urban site. In Nepal, the report of chronic illnesses have risen from 6.5% in 1995/96 to 11.7% in 2010–11 with reported incidents differing from 7.9% in the poorest income quintile group to 15.3% in the richest income group (Central Bureau of Statistics 2011). This could be due to the increase in lifestyle diseases with increasing income in South Asia (Yusuf et al. 2001). Income levels are higher in urban areas in Nepal, with mean incomes of rupees 318 167 per capita in urban areas and rupees 171 950 per capita in rural areas (Central Bureau of Statistics 2011). This could explain the higher incidence of reported chronic illnesses in the peri-urban site.
Traditional medicine use and treatment-seeking strategies
In this study, around one-third (31%) of the illness episodes were treated using traditional medicine at some point during the treatment-seeking strategy. This is one of the first such estimates in Nepal and South Asia and suggests that traditional medicine is important in maintaining and improving health care in the study area. Most studies quantifying the reliance on traditional medicine are from Africa, and report rates of reliance ranging from 5.6% (Chenge et al. 2014) to 51.5% (Pouliot 2011) of sampled populations. Average rates of reliance on traditional medicine showed high variation between sites: only 15% of illness episodes in the peri-urban site were treated using traditional medicine, but this figure increased in the sites with more difficult access to public hospitals (31 and 46% for the rural hills and rural mountain sites, respectively). The increase in use of allopathic medicine (or decrease in use of traditional medicine) with increasing access to allopathic health facilities has been documented in many other studies (e.g. Srivastava and Bhandari 1974; Weller et al. 1997; Pouliot 2011). The fact that we included a peri-urban site in our sample hence has a great effect on overall traditional medicine consumption rates. Reliance rates could, however, also be affected by access to traditional medicine providers. Contrary to what is often suggested in the literature in Nepal and elsewhere (WHO 2002; Bhattarai et al. 2010), availability of traditional healers was low and Ayurvedic health facilities were non-existing within sites. A study from Sri Lanka also found that lack of Ayurvedic providers at village level affected utilization levels of traditional medicine (Weerasinghe and Fernando 2010). Most traditional medicine providers in all sites were Dhami-Jhankris. Being providers of spiritual treatments, Dhami–Jhankris are considered very different from other traditional medicine providers who offer treatments based on medicinal plants (Thorsen 2015). The lack of traditional medicine providers also explains why the majority of traditional medicine treatments (66.8%) were self-treatment with medicinal plants. Traditional medicine providers were, on the other hand, relied upon later during people’s treatment-seeking strategies. This could be due to the relatively higher time cost of visiting those providers due to their low availability.
Medicinal plants were available for collection in all sites, and this study found that 22% of the ill people used medicinal plants for self-treatment at some point during their treatment-seeking strategy. Generally, few studies report on frequencies of medicinal plant use, though medicinal plants for self-treatment were reported to be consumed by 12.5% in a study population in Ethiopia (Gedif and Hahn 2003), 20.7% in Sudan (Awad et al. 2006), and the use of herbal medicines for HIV treatment in a study population in South Africa were reported to be 29.6% (Peltzer et al. 2008). Importantly, this study found that 41% of the reported treatments including medicinal plants were conceptualized as common sense and hence recorded as a treatment without medication by the respondents rather than as a treatment per se. This means that other studies risk underreporting the use of medicinal plants if not accounting for these treatments without medication.
The reliance on traditional medicine and medicinal plants changed during people’s treatment-seeking strategy. Multiple treatments were common but respondents had recourse to the different treatments in a rather specific sequence. For example, treatments without medication were mainly used as first recourse treatments, whereas the share of ill people visiting treatment providers (allopathic or traditional) increased in later recourses. The share of ill people using medicinal plants was highest for the first recourse and decreased through subsequent recourses. These results suggest that home care (treatment without medication or traditional) is very common in early stages of treatment-seeking strategies. Similar findings have been reported for treatment seeking in relation to malaria in Kenya (Nyamongo 2002), whereas Ryan (1998) found that while the rate of home treatments use remained almost constant throughout the treatment sequence, pharmacy visits decreased while treatment provider visits increased. These findings have important policy implications, as current policy is focused on expanding provision of public Ayurvedic facilities and promoting manufacturing of Ayurvedic medicines (Department of Ayurveda 1996). Several programmes have also focused on training of traditional healers in aspects of allopathic medicine (Jimba et al. 2005). Expanding provision is necessary from an accessibility point of view, as few traditional medicine providers are currently available in the study sites. Policy, however, also needs to consider current practices and the importance of self-treatment and treatments without medication as first recourses, also where providers of allopathic medicine are present. Ahmed et al. (2000b) speculated that health education programmes increases people’s recognition, diagnosis and self-treatment of illnesses. This indicates the importance of promoting self-care practices and patient empowerment through knowledge and means to recognize and treat illnesses without resorting to external providers (Edgeworth and Collins 2006). However, as noted by Edgeworth and Collins (2006), household and patient empowerment is only a positive health behaviour provided that households have an adequate level of human and social capital, enabling them to take the right treatment decisions.
Traditional medicine use and its determinants
In addition to access to traditional and allopathic medicine, this study has identified a number of determinants associated with the use of traditional medicine. Determinants differed across sites, but the determinant significant in all sites, and for both traditional medicine and medicinal plants for self-treatment, was whether someone in the household held knowledge of medicinal plants. This connection between knowledge and use of medicinal plants has been observed elsewhere (e.g. Budhathoki and BC 2008; Kassam et al. 2010), but the value of holding knowledge about medicinal plants is paramount particularly due to the central role of self-treatment. Whereas several studies have investigated community-level knowledge of medicinal plants by focusing mainly on traditional healers and other key informants with extensive knowledge (Bhattarai et al. 2010; Uprety et al. 2010), the pattern of treatment seeking found in this study points to its importance at household level.
Another important finding of the present study is that, oppositely to what is commonly assumed, richer households were more likely to use traditional medicine and medicinal plants in the peri-urban site and traditional medicine in the rural mountain site. Studies in developed countries have reported increased use of alternative medicine with rising incomes (Robinson et al. 2009). For the rural hills site, this study, however, found a decreased likelihood of medicinal plant use for rich households, supporting the common assumption that traditional medicine is mostly relied on by the poor and disadvantaged (Kroeger 1983; Shrestha and Dhillion 2003; WHO 2012). This difference among sites indicates the possibility of a u-shape relationship between income and reliance on traditional medicine (i.e. high reliance for the poorest and richest households), which could lead to increased traditional medicine consumption in Nepal in the future as general economic and social developments unfolds (Smith-Hall et al. 2012). This further points to the need for policy to address traditional medicine from other perspectives than formal education of providers and accessibility, as local and individual knowledge of medicinal plants play an important role in sustaining practices of traditional medicine use and practices of self-treatment, and as traditional medicine has potential to remain important as populations get richer.
The use of traditional medicine significantly decreased with education of household head in the rural hills site as did use of medicinal plants in the rural hills site and the peri-urban site. In this dataset, no significant correlation was found between education of household head and household income. Kroeger (1983) argued that formal education in developing countries is the strongest form of exposure to Western paradigms, and that educated people therefore tend to opt for allopathic medicine. Many other studies have documented this same trend (e.g. Ahmed et al. 2000b; Pouliot 2011; Sato 2012b). The insignificant effect of education on the use of traditional medicine in the rural mountain site could be explained by the relatively strong cultural ties to traditional medicine (Bhattarai et al. 2010).
Age influenced traditional medicine use. When illness was faced by a child, people were less likely to use medicinal plants for treatment. This finding was significant in all sites. In the rural mountain site, children were also less likely to consume traditional medicine when facing illness. These findings are in line with a string of studies showing that illnesses in children are most often treated exclusively with allopathic medicine (Kleinman 1980; Pouliot 2011). Being an elder was found to increase the likelihood of consuming traditional medicine (in both rural sites) and increase the likelihood of consuming medicinal plants in the rural hills site. However, being an elder decreased the likelihood of using medicinal plants in the peri-urban site. In South Asia, the incidence of non-communicable diseases such as coronary heart disease is increasing in parallel with the increase in life expectancy and household income (Yusuf et al. 2001). It can be hypothesized that household knowledge transmitted from older generations may not involve treatments for such ‘new’ types of illnesses, which are most likely to be found in urban and peri-urban areas, wherefore people are compelled to seek treatment from providers. In the rural hills site, chronicity of the encountered illness increased the likelihood of consuming traditional medicine and medicinal plants. This finding coincides with one of Kroeger’s (1983) postulates, which says that the more chronic the condition, the more time the ill person has to recourse to different therapies, and thus the higher the probability of recourse to traditional medicine. This result has also been verified empirically by Develay et al. (1996), Pouliot (2011) and Sato (2012a). However, in the rural mountain site, the likelihood of using medicinal plants decreased when having a chronic illness rather than an acute. Some studies have shown that patients with a chronic illness are more likely to seek care from a provider than patients with acute diseases (Sepheri et al. 2008; Chenge et al. 2014), hence self-medication generally may not be preferred. Looking at the overall treatment-seeking strategies in the rural mountain site (Figure 3), medicinal plants are very important first and second recourses. A speculation could be that, due to the time elapsed since the initiation of the first treatments taken during chronic illness episodes, self-treatments tend to be forgotten.
In the rural mountain site, households headed by a female were less likely to use medicinal plants for self-treatment. The role of gender in treatment seeking has mainly been discussed in relation to gender of the patient (Develay et al. 1996). Gender of the patient was not identified as a significant determining factor in this study. The role of the care takers has been studied in relation to medicinal plant use, and self-treatment with medicinal plants is found to be the domain of women (Singhal 2005). The reason why female-headed households in the rural mountain site use less medicinal plants could hence be associated with the social division of labor related to medicinal plant collection, as the medicinal plants in the rural mountain site to a larger extent are collected in the high mountains at a greater distance from the villages than in the other sites. Collection here is mainly carried out by men as it requires travelling longer distances (Thorsen 2015). Households without a male head may hence not have this opportunity. Similar findings have been observed in Tanzania (Kitula 2007).
Conclusion
A lack of quantitative data on the use of traditional medicine in developing countries has led researchers and policy makers to rely on outdated and/or uncertain estimates. This article contributes to filling in the knowledge gap surrounding the use of traditional medicine in Asia by showing that traditional medicine, and especially self-treatment with medicinal plants, prevail as treatment options for rural as well as peri-urban populations. We use data from three different sites to show both the similarity and variation of determinants between sites as well as the variation in the prominence of traditional medicine during people’s treatment-seeking strategies. These differences complicate the implementation of broad health care policies.
The common assumption among researchers and policy makers regarding the use of traditional medicine is that poor and marginalized people are most reliant on traditional medicine due to its availability. This article challenges those assumptions by showing that high income and knowledge of medicinal plants are important determinants of use of traditional medicine. Age, education, gender and illness chronicity are also shown to be significant determinants.
These findings support the current traditional medicine policy’s focus on expanding the coverage of traditional medicine facilities in Nepal. However, the importance of self-treatment with medicinal plants, despite the availability of allopathic medicine in all sites, gives evidence of people’s preference for home-based traditional treatments as first recourses. Given the importance of knowledge in using medicinal plants for self-treatment and the current lack of accessibility of traditional providers in our study sites, policy makers should also consider the need for building human capital in order to ensure that self-treatment with medicinal plants will remain an option in the future.
This article points to the fact that traditional medicine has different functions for people at different times during their treatment-seeking strategy. Development of a typology that recognizes the diverse relationships of people to traditional medicine and medicinal plants is important to support the needs of local people and to enable institutions to adapt to changing treatment-seeking patterns. Specifically, further studies on determinants of traditional medicine use in developing countries should investigate relationships between household income and traditional medicine use. For example, it is crucial to understand if rising income in developing countries will lead to an increase in traditional medicine use as has been observed in developed countries.
Acknowledgements
Helle Overgaard Larsen and Carsten Smith-Hall provided useful comments on earlier versions of this manuscript. Special thanks go to respondents in all three sites as well as to field assistants. The role of the Community-based Natural Forest and Tree Management in the Himalaya (ComForM) project in site selection and providing household background and income data is acknowledged.
Funding
This work was supported by the University of Copenhagen.
Conflict of interest statement. None declared.
References
- Ahmed SM, Adams AM, Chowdhury M, Bhuiya A. 2000a. Gender, socioeconomic development and health-seeking behaviour in Bangladesh. Social Science and Medicine 51: 361–71. [DOI] [PubMed] [Google Scholar]
- Ahmed SM, Adams AM, Chowdhury M, Bhuiya A. 2000b. Changing health-seeking behaviour in Matlab, Bangladesh: Do development interventions matter?. Health Policy and Planning 18: 306–15. [DOI] [PubMed] [Google Scholar]
- Anyinam C. 1987. Availability, accessibility, acceptability, and adaptability: four attributes of African ethno-medicine. Social Science & Medicine 25: 803–11. [DOI] [PubMed] [Google Scholar]
- Awad AI, Eltayeb IB, Capps PA. 2006. Self-medication practices in Khartoum State, Sudan. European Journal of Clinical Pharmacology 62: 317–24. [DOI] [PubMed] [Google Scholar]
- Bentley H. 1995. The organization of Health Care in Nepal. International Journal of Nursing Studies 32: 260–70. [DOI] [PubMed] [Google Scholar]
- Bhattarai S, Chaudhary RP, Quave CL, Taylor RSL. 2010. The use of medicinal plants in the trans-himalayan arid zone of Mustang district, Nepal. Journal of Ethnobiology and Ethnomedicine 6: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bignante E, Tecco N. 2013. Is indigenous health knowledge converging to herbalism? Healing practices among the Meru and the Maasai of the Ngarenyanyuki ward, Northern Tanzania. Geoforum 48: 177–86. [Google Scholar]
- Biswas A, See D, Kogon MM, Spiegel D. 2000. Hypnotizability and the use of traditional dhami-jhankri healing in Nepal. International Journal of Clinical and Experimental Hypnosis 48: 6–21. [DOI] [PubMed] [Google Scholar]
- Budhathoki CB, BC RK 2008. Perceptions of malaria and pattern of treatment seeking behaviour among Tharu and Pahari communities of Jhalari. Journal of Nepal Health Research Council 6: 84–92. [Google Scholar]
- Cameron M. 2008. Modern desires, knowledge control, and physician resistance: regulating Ayurvedic medicine in Nepal. Asian Medicine 4: 86–112. [Google Scholar]
- Central Bureau of Statistics. 2011. Nepal Living Standards Survey 2010/11: Statistical report, Volume one. Kathmandu: National Planning Commission Secretariat, Government of Nepal. [Google Scholar]
- Central Bureau of Statistics. 2012. National Population and Housing Census 2011 (Village Development Committee/Municipality). Kathmandu: National Planning Commission Secretariat, Government of Nepal. [Google Scholar]
- Chaturvedi HK, Mahanta J, Pandey A. 2009. Treatment-seeking for febrile illness in north-east India: and epidemiological study for the malaria endemic zone. Malaria Journal 8: 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chenge MF, Vennet JVD, Loboya NO, et al. 2014. Health-seeking behaviour in the city of Lubumbashi, Democratic Republic of the Congo: results from a cross-sectional household survey. BMC Health Services Research 14: 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cocks M, Dold A. 2000. The role of ‘African Chemists’ in the health care system of the Eastern Cape province of South Africa. Social Science and Medicine 51: 1505–15. [DOI] [PubMed] [Google Scholar]
- Cunningham AB, Shanley P, Laird S. 2008. Health, habitats and medicinal plant use. In: Colfer CJ. (ed). Human health and forests: A global overview of issues, practice and policy. People and Plants International Conservation Series. London: Earthscan, pp. 35–62. [Google Scholar]
- Das J, Hammer J, Sánchez-Paramo C. 2012. The impact of recall periods on reported morbidity and health seeking behavior. Journal of Development Economics 98: 76–88. [Google Scholar]
- Department of Ayurveda. 1996. The National Ayurveda Health Policy 2052 (1996). Kathmandu: Ministry of Health. [Google Scholar]
- Department of Health Services. 2012. Annual Report 2067/68 (2010/2011). Kathmandu: Ministry of Health and Population. [Google Scholar]
- Develay A, Sauerborn R, Diesfield HJ. 1996. Utilization of health care in an African urban area: results from a household survey in Ouagadougou, Burkina Faso. Social Science & Medicine 43: 1611–19. [DOI] [PubMed] [Google Scholar]
- Edgeworth R, Collins AE. 2006. Self-care as a response to diarrhea in rural Bangladesh: Empowered choice or enforced adoption? Social Science & Medicine 63: 2686–97. [DOI] [PubMed] [Google Scholar]
- Frank R, Stollberg G. 2002. Ayurvedic patients in Germany. Anthropology & Medicine 9: 223–44. [DOI] [PubMed] [Google Scholar]
- Furuta M, Salway S. 2006. Women’s position within the household as a determinant of maternal health care use in Nepal. International Family Planning Perspectives 32: 17–27. [DOI] [PubMed] [Google Scholar]
- Gedif T, Hahn HJ. 2003. The use of medicinal plants in self-care in rural central Ethiopia. Journal of Ethnopharmacology 87: 155–61. [DOI] [PubMed] [Google Scholar]
- Giovannini P, Reyes-García V, Waldstein A, Heinrich M. 2011. Do pharmaceuticals displace local knowledge and use of medicinal plants? Estimates from a cross-sectional study in a rural indigenous community, Mexico. Social Science & Medicine 72: 928–36. [DOI] [PubMed] [Google Scholar]
- Government of Nepal and UNDP. 2014. Nepal Human Development Report 2014 – Beyond Geography, Unlocking Human Potential. Kathmandu: Government of Nepal and UNDP. [Google Scholar]
- Himalayan Ayurveda Research Institute. 1996. Project report on medicinal plants and traditional medical practice in Gorkha District. Kathmandu: GTZ. [Google Scholar]
- Hotchkiss DR, Rous JJ, Karmacharya K, Sangraula P. 1998. Household health expenditure in Nepal: implications for health care financing reform. Health Policy and Planning 13: 371–83. [DOI] [PubMed] [Google Scholar]
- Jimba M, Aitken IW, Silwal RC, Poudyal AK, Wakai S. 2005. First aid kit: a challenging new tool for traditional healers in Nepal. Tropical Doctor 35: 113–14. [DOI] [PubMed] [Google Scholar]
- Kassam KA, Karamkhudoeva M, Ruelle M, Baumflek M. 2010. Medicinal plant use and health sovereignty: findings from the Tajik and Afghan Pamirs. Human Ecology 38: 817–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitula RA. 2007. Use of medicinal plants for human health in Udzungwa Mountains forests: a case study of New Dabaga Ulongambi Forest Reserve, Tanzania. Journal of Ethnobiology and Ethnomedicine 3: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A. 1980. Patients and healers in the context of culture. An exploration of the borderland between anthropology, medicine and psychiatry. Berkeley: University of California Press. [Google Scholar]
- Koirala RR. 2007. Country Monographs on Traditional System of Medicine.http://www.mohp.gov.np/english/files/news_events/5‐1-National-Policy-on-Traditional-Medicine.pdf,accessed 25 October 2013.
- Kroeger A, Zurita A, Perez-Samaniego C, Berg H. 1988. Illness perception and use of health services in north-east Argentina. Health Policy and Planning 3: 141–51. [Google Scholar]
- Kroeger A. 1983. Anthropological and socio-medical health care research in developing countries. Social Science & Medicine 13B: 147–61. [DOI] [PubMed] [Google Scholar]
- Larsen HO, Rayamajhi S, Chhetri BBK, et al. 2014. The role of environmental incomes in rural Nepalese livelihoods 2005–2012: contextual information. Frederiksberg: Department of Food and Resource Economics, University of Copenhagen (IFRO Documentation; No. 2014/4). http://curis.ku.dk/ws/files/125231441/IFRO_Documentation_2014_4.pdf, accessed 21 November 2014.
- Mathez-Stiefel SL, Vandebroek I, Rist S. 2012. Can Andean medicine coexist with biomedical health care? A comparison of two rural communities in Peru and Bolivia. Journal of Ethnobiology and Ethnomedicine 8: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayxay M, Hansana V, Sengphilom B, et al. 2013. Respiratory illness healthcare-seeking behavior assessment in the Lao People’s Democratic Republic (Laos). BMC Public Health 13: 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Population. 2010. Nepal Health Sector Programme-2 – Implementation Plan (2010–2015). Kathmandu: Ministry of Health and Population. [Google Scholar]
- Nyamongo IK. 2002. Health care switching behaviour of malaria patients in a Kenyan rural community. Social Science & Medicine 54: 377–86. [DOI] [PubMed] [Google Scholar]
- Peltzer K, Preez NFD, Ramlagan S, Fomundam H. 2008. Use of traditional complementary and alternative medicine for HIV patients in KwaZulu-Natal, South Africa. BMC Public Health 8: 255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pillai RK, Williams SV, Glick HA, et al. 2003. Factors affecting decisions to seek treatment for sick children in Kerala, India. Social Science and Medicine 57: 783–90. [DOI] [PubMed] [Google Scholar]
- Pokhrel S, Sauerborn R. 2004. Household decision-making on child health care in developing countries: the case of Nepal. Health Policy and Planning 19: 218–33. [DOI] [PubMed] [Google Scholar]
- Pouliot M. 2011. Relying on nature’s pharmacy in rural Burkina Faso: Empirical evidence of the determinants of traditional medicine consumption. Social Science & Medicine 73: 1498–507. [DOI] [PubMed] [Google Scholar]
- Robinson N, Loranc A, Blair M. 2009. Developing a decision-making model on traditional and complementary medicine use for children. European Journal of Integrative Medicine 1: 43–50. [Google Scholar]
- Ryan GW. 1998. What do sequential behavioral patterns suggest about the medical decision-making process?: Modelling home case management of acute illnesses in a rural Cameroonian village. Social Science and Medicine 46: 209–25. [DOI] [PubMed] [Google Scholar]
- Sato A. 2012a. Revealing the popularity of traditional medicine in light of multiple recourses and outcome measurements from a user’s perspective in Ghana. Health Policy and Planning 27: 625–37. [DOI] [PubMed] [Google Scholar]
- Sato A. 2012b. Does socio-economic status explain use of modern and traditional health care services?. Social Science & Medicine 75: 1450–59. [DOI] [PubMed] [Google Scholar]
- Seeberg J, Pannarunothai S, Padmawati RS, et al. 2014. Treatment seeking and health financing in selected poor urban neighbourhoods in India, Indonesia and Thailand. Social Science and Medicine 102: 49–57. [DOI] [PubMed] [Google Scholar]
- Sepehri A, Moshiri S, Simpson W, Sarma S. 2008. Taking account of context: how important are household characteristics in explaining adult health-seeking behaviour? The case of Vietnam. Health Policy and Planning 23: 397–407. [DOI] [PubMed] [Google Scholar]
- Shrestha PM, Dhillion SS. 2003. Medicinal plant diversity and use in the highlands of Dolakha district, Nepal. Journal of Ethnopharmacology 86: 81–96. [DOI] [PubMed] [Google Scholar]
- Singhal R. 2005. Medicinal plants and primary health care: the role of gender. Journal of Health Management 7: 277–93. [Google Scholar]
- Smith-Hall C, Larsen HO, Pouliot M. 2012. People, plants and health: a conceptual framework for assessing changes in medicinal plant consumption. Journal of Ethnobiology and Ethnomedicine 8: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sreeramareddy CT, Shankar RP, Sreekumaran BV, et al. 2006. Care seeking behaviour for childhood illness – a questionnaire survey in Western Nepal. BMC International Health and Human Rights 6: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava AB, Bhandari SC. 1974. Utilisation and pattern of demand for the C.G.A.: S. Aryuveti dispensaries in Delhi. New Delhi: National Institute of Health and Family Welfare; Research Report no. 18. [Google Scholar]
- Sydara K, Gneunphonsavath S, Wahlström R, et al. 2005. Use of traditional medicine in Lao PDR. Complementary Therapies in Medicine 13: 199–205. [DOI] [PubMed] [Google Scholar]
- Thorsen R. 2015. Conceptualizations of pluralistic medical fields: exploring the therapeutic landscapes of Nepal. Health and Place 31: 83–9. [DOI] [PubMed] [Google Scholar]
- UNDP. 2013. Human Development Report 2013 – The rise of the South: Human progress in a diverse world. New York: United Nations Development Programme. [Google Scholar]
- UNDP. 2014. Nepal Human Development Report 2014 – Beyond geography, unlocking human potential. Kathmandu: Government of Nepal, National Planning Commission and United Nations Development Programme, Nepal. [Google Scholar]
- Uprety Y, Asselin H, Boon EK, Yadav S, Shrestha KK. 2010. Indigenous use and bio-efficacy of medicinal plants in the Rasuwa District, Central Nepal. Journal of Ethnobiology and Ethnomedicine 6: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weerasinghe MC, Fernando DN. 2010. Paradox in treatment seeking: an experience from rural Sri Lanka. Qualitative Health Research 21: 365–72. [DOI] [PubMed] [Google Scholar]
- Weller SC, Ruebush TR, Klein RE. 1997. Predicting treatment-seeking behavior in Guatemala: a comparison of the health services research and decision-theoretic approaches. Medical Anthropology Quarterly 11: 224–45. [DOI] [PubMed] [Google Scholar]
- WHO. 2001. Legal status of traditional medicine and complementary/alternative medicine: a worldwide review. Geneva: WHO. http://apps.who.int/medicinedocs/pdf/h2943e/h2943e.pdf, accessed 25 October 2014.
- WHO. 2002. WHO Traditional Medicine Strategy 2002–2005. Geneva: WHO. http://whqlibdoc.who.int/hq/2002/WHO_EDM_TRM_2002.1.pdf, accessed 25 October 2014.
- WHO. 2007. Health System in Nepal: Challenges and Strategic Options. Kathmandu: World Health Organization, Country office for Nepal. [Google Scholar]
- WHO. 2012. Traditional and Complementary Medicine Policy. Geneva: WHO. http://apps.who.int/medicinedocs/documents/s19582en/s19582en.pdf, accessed 21 November 2014.
- World Bank. 2014. World Development Indicators. World Bank Group. Data available from http://data.worldbank.org/country/nepal, accessed 1 November 2014.
- Yusuf S, Reddy S, Ounpuu S, Anand S. 2001. Global burden of cardiovascular diseases: Part II: Variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation 104: 2855–64. [DOI] [PubMed] [Google Scholar]