Abstract
During the last two decades, the use of maternal health services has increased dramatically in Pakistan, with nearly 80% of Pakistani women making an antenatal care (ANC) visit during their pregnancy. Yet, this increase in use of modern health services has not translated into significant increases in the adoption of contraception. Even though Pakistan has had a national family planning programme and policies since the 1950s, contraceptive use has increased slowly to reach only 35% in 2012–13. No evidence is currently available to demonstrate whether the utilization of maternal health services is associated with contraceptive adoption in Pakistan. This study uses data from a large-scale survey conducted in Sindh province in 2013 to examine whether ANC utilization is a significant predictor of subsequent contraceptive use among women. In an analysis which controls for a range of variables known to be important for family planning adoption, the findings show that ANC is the strongest predictor of subsequent family planning use among women in Sindh. The antenatal visit represents an enormous opportunity to promote the adoption of family planning in Pakistan. The family planning programme should ensure that high-quality family planning counselling is provided to women during their ANC visits. This approach has the potential for contributing to substantial increases in contraceptive use in Pakistan.
Keywords: Antenatal care, contraceptive use, family planning, maternal health services, Pakistan
Key Messages
During the last two decades, there has been a tremendous increase in the utilization of maternal health services in Pakistan without any noteworthy increase in the use of contraception.
Although maternal health and family planning service provision are, in principle, integrated health providers do not offer family planning counselling or services during maternal health visits.
Antenatal care use is a powerful predictor of subsequent contraceptive use, indicating the increasing emphasis on family planning counselling during antenatal care has the potential to have a significant impact on the adoption of contraception.
Introduction
Pakistan has experienced high population growth since becoming an independent country in 1947. The population is estimated to have reached 188 million by 2015 (Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat 2012) and is increasing by 2.1% annually, leading to concerns about the detrimental impact of this growth on social and economic development (Royan and Sathar 2013). The national family planning programme has had limited success in the last two decades: starting from a low base of 12%, the annual increase in contraceptive use has averaged ∼1 percentage point per year between 1990–91 and 2012–13 to reach 35% (National Institute of Population Studies and ICF International 2013); traditional method use has been increasing at a faster rate than modern method use (Carton and Agha 2012) and reached 9.3% by 2012–13 (National Institute of Population Studies and ICF International 2013).
Many causes have contributed to the slow increase in contraceptive use; the most important barriers to the adoption of family planning are thought to be inadequate quality of service provision and poor follow-up of clients (Casterline et al. 2001; Fikree et al. 2005; Agha 2010). In spite of the slow increase in contraceptive use and the reliance on traditional methods such as withdrawal or short-term methods such as condoms, fertility declined in Pakistan, from 5.5 births per woman in 1990–91 to 3.8 births per woman in 2012–13 (National Institute of Population Studies and ICF International 2013). This decline is thought to have been driven by a rising age at marriage (Nasrullah et al. 2014) and high levels of abortion (Sathar et al. 2007). Although the uptake of contraceptive use by Pakistani women has been slow, the use of maternal health services has increased dramatically during the same period: between 1990–91 and 2012–13, antenatal care (ANC) use during pregnancy increased from 26 to 78%, and the institutional delivery rate increased from 12 to 52% (Agha 2013).
Studies in several countries suggest that the increased use of maternal and child health services has contributed to higher contraceptive use. Two previous studies used econometric techniques to examine the relationship between maternal health service utilization and family planning adoption in Morocco and Guatemala (Hotchkiss et al. 1999; Seiber et al. 2005). The authors measured the intensity of maternal child health (MCH) service use by developing an index for the use of ANC, delivery care, postnatal care and childhood immunization. These studies found that the intensity of MCH service use was a significant determinant of subsequent contraceptive use in both Morocco and Guatemala, even after controlling for a broad range of supply and demand side variables and after taking selection factors into account. The results of these studies suggest that counselling and promotional efforts by health facility staff may have been responsible for the positive effects of MCH service utilization on contraceptive adoption.
A study by Ahmed and Mosley (2002) used Demographic and Health Survey data from countries with extremely different cultural and service delivery contexts (including Zimbabwe, Thailand, Egypt, Tunisia, Guatemala and Colombia) to examine the relationship between MCH service utilization and contraceptive use. The study tested whether MCH service utilization independently influenced contraceptive adoption. In every country included in the study, maternal and child health service utilization was significantly associated with contraceptive use, independent of any common predictor variables. The authors concluded that, in a wide variety of contexts, women made simultaneous choices to improve both the survival of their children and their own health.
In Pakistan, MCH and family planning service delivery have historically been implemented as vertical programmes. After the devolution of authority to provincial governments under the 18th constitutional amendment, these two programmatic areas were to be integrated at the provincial level. However, integration of the devolved public health programmes did not follow as anticipated (Nishtar et al. 2013). An external evaluation of the Pakistan National Maternal and Child Health Program in 2012 found evidence of failure in the achievement of a key objective—provision of comprehensive family planning services—because functional integration between the Provincial Health Departments and the Provincial Population was not followed (Technical Resource Facility 2012). The continued separation of health and population areas in these two departments, each with its distinct leadership at the provincial level, continues to complicate integration. Not surprisingly, empirical evidence is not available to demonstrate whether integration of service delivery in Pakistan has led to increased use of contraception. Nor is it known whether the integration of these two programmatic areas has led to provider behaviour change. For example, at the health facility level, it is not known whether providers counsel mothers about birth spacing during an ANC visit. The limited available information suggests that family planning counselling is usually not conducted during ANC visits in Pakistan: the 2012–13 Demographic and Health Survey shows that while more than 80% of women are in contact with health services, only 6% of women receive counselling on family planning (National Institute of Population Studies and ICF International 2013).
Several studies in India have shown that providers have a preference for promoting ANC and institutional delivery but are less likely to provide advice on contraception. A recent study in Uttar Pradesh shows that when family planning advice is provided during an ANC visit, it leads to an increase in current use of contraception (Yadav and Dhillon 2015). Another study examined the effect of ANC use on adoption of post-partum contraception in Kenya and Zambia. The study found that in both countries the intensity of ANC use was significantly associated with the adoption of post-partum contraception (Do and Hotchkiss 2013).
This study uses data from Sindh, Pakistan’s second largest province, with a population of ∼45 million, to examine whether ANC use is associated with higher contraceptive use during the 2 years following a live birth. Empirical evidence of a link between the ANC visit and subsequent contraceptive adoption would highlight the importance of the ANC visit for family planning adoption. At present, the ANC visit is primarily seen as a vehicle for reducing poor maternal health outcomes.
Methods
Sample
Detailed information about the survey methodology is available online (Agha and Williams 2013). Briefly, data were collected to serve as the baseline for a large-scale maternal and child health programme funded by the US Agency for International Development. A multi-stage, stratified sampling design was used to select women who had a live birth during the past 2 years. Data collected from face-to-face interviews with female respondents included self-reported information on age, parity, educational status, health care utilization and current contraceptive use. All districts of Sindh were included in the survey, and data were collected from 4000 women who were 15–49 years old and had a live birth during the 2 years before the survey. The survey oversampled rural districts of Sindh. Weights were attached to the data to take the oversampling into account and provide a representative picture of Sindh. The sample was designed to provide reliable estimates for key indicators for Sindh province.
Instrument
The survey instrument used for this study was adapted from the instrument used for the Demographic Health Survey of Pakistan and the Knowledge, Practice and Coverage Survey instrument developed by the Johns Hopkins University/Child Survival Support Program 1990 and revised more recently by the US Agency for International Development-funded Maternal Child Health Integrated Project. Data were collected during interviews at women’s households, by female data collectors who were trained in survey methodology and employed by a local research firm with >10 years of experience conducting survey research Pakistan. All participants provided informed consent, and the study was approved by institutional review boards from the Johns Hopkins Bloomberg School of Public Health and the National Bioethics Committee of Pakistan.
Outcome variable
Current contraceptive use is included in the analysis as a binary variable. Current users of contraception include users of condoms (34.2%), injectables (20.9%), pills (12%), sterilization (10.8%), IUD (7.2%), implants (1.5%) and traditional methods (13.4%). The proportion of reversible modern method users in our Sindh survey is higher than in the 2012–13 Pakistan Demographic and Health Survey Sindh sample. In the Demographic and Health Survey Sindh sample, condom users comprise 27% of current users of contraception and injectable users comprise 11% of current users. The higher rate of reversible method use in our Sindh survey is because the sample comprises of currently married women 15–49 who have delivered in the last 2 years, whereas the Demographic and Health Survey sample comprises of all currently married women 15–49 years, including women who may not have had a birth in the last 5 or 10 years due to natural causes or due to the deliberate use of female sterilization after completion of their desired family size.
Key explanatory variable
Women were asked how many times they had received ANC during their last pregnancy. The variable was recoded as a categorical variable with three categories: 0, 1–3 visits, 4 or more visits.
Other explanatory variables (residential and sociodemographic characteristics)
Current residence in urban or rural areas, age of last child (1–6 months, 7–12 months, 13–18 months, 19–24 months), number of children (1, 2, 3 or more), whether an additional child is wanted or not, the highest level of school attended (no formal education, primary or middle school, secondary or higher education). A variable measuring household wealth was created using principal component analysis and used data collected in the survey on the following assets and amenities: ownership of mobile phone, motorcycle, television, refrigerator, cupboard/cabinet, washing machine, bed, clock, sofa, sewing machine, livestock, construction material use for the floor, construction material used for the roof, construction material used for the wall, primary fuel used by the household, whether the household had a water pump and whether the household had a toilet. This approach is similar to what is used widely by the Demographic Health Surveys (Filmer and Pritchett 2001; Rutstein and Johnson 2004).
Statistical analysis
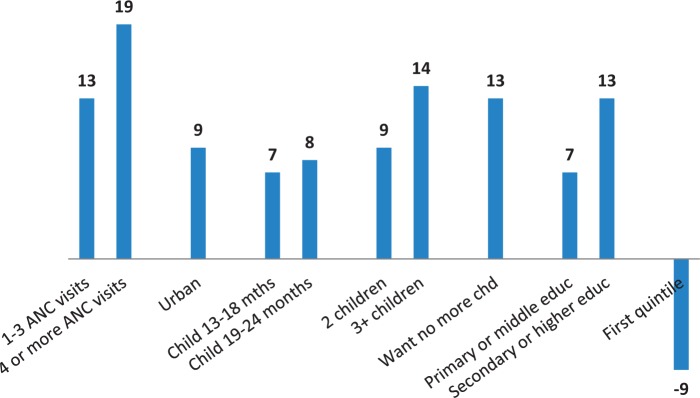
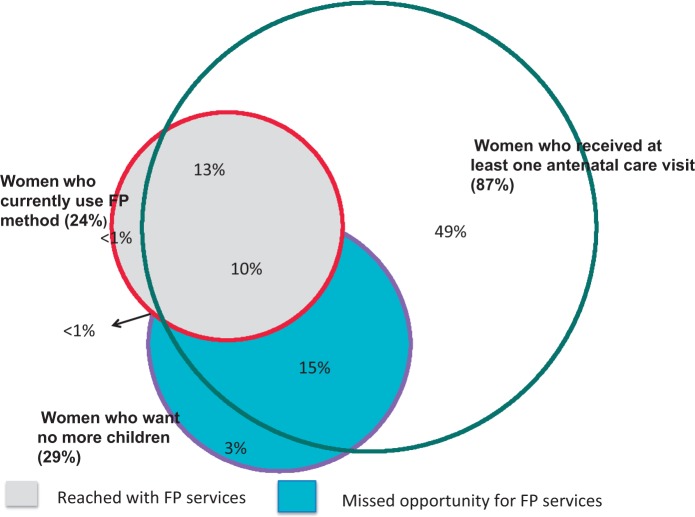
Data analysis was conducted using Stata 12.1 (StataCorp 2011). Bivariate analysis was conducted to show the relationship between the number of ANC visits and contraceptive use as well as relationships between sociodemographic variables and contraceptive use. The unadjusted odds of contraceptive use demonstrate the significance of relationships between variables at the bivariate level. Logistic regression was used to determine the adjusted odds of contraceptive use. The SVY suite of commands in STATA was used to conduct weighted analysis and control for clustering at the level of the primary sampling unit. Variables were selected for the multivariate model based on a review of the literature. Marginal effects were calculated for the adjusted logistic regression model (Bartus 2005) (Figure 1). Proportional Venn diagrams were constructed to illustrate the overlapping associations between ANC visits, contraceptive use and future intentions regarding child-bearing (Figure 2).
Figure 1.
Marginal effects of number of ANC visits and sociodemographic factors on current contraceptive use in Sindh province.
Figure 2.
Venn diagram: overlap between women who received at least one antenatal case visit, women who currently use family planning and women who want no more children.
Results
Column 1 of Table 1 shows characteristics of the sample. Consistent with the rapid increase of ANC use in Pakistan, approximately one-half of study participants made four or more antenatal visits during their last pregnancy (51%). Nearly one-half of respondents lived in urban areas (49%). Approximately 55% of respondents had a child <1 year of age. Approximately 52% of respondents had three or more children. Approximately 30% of women did not want another child. The majority of women in the sample had no formal education (57%).
Table 1.
Sample distribution, percentage using contraception and odds ratios of contraceptive use
| Column 1 | Column 2 | Column 3 | ||
|---|---|---|---|---|
| Sample distribution (n = 4000) (%) | Percentage of women using a contraceptive method (%) | Unadjusted odds of contraceptive use | Number of cases | |
| Number of ANC visits | ||||
| 0 | 13.3 | 7.5 | 1.00 | 534 |
| 1–3 | 35.3 | 17.9 | 2.67*** | 1411 |
| 4 or more | 51.4 | 32.2 | 5.79*** | 2055 |
| Residence | ||||
| Urban | 48.8 | 34.4 | 3.28*** | 1951 |
| Rural | 51.2 | 13.8 | 1.00 | 2049 |
| Age of last child | ||||
| 1–6 months | 18.8 | 20.6 | 1.00 | 751 |
| 7–12 months | 36.2 | 21.9 | 1.07 | 1446 |
| 13–18 months | 24.2 | 26.5 | 1.38* | 969 |
| 19–24 | 20.8 | 27.2 | 1.44* | 834 |
| Number of living children | ||||
| 1 | 24.5 | 14.8 | 1.00 | 981 |
| 2 | 23.9 | 24.7 | 1.89*** | 956 |
| 3 or more | 51.6 | 27.8 | 2.22*** | 2063 |
| Desire for more children | ||||
| Want more, undecided | 70.5 | 18.8 | 1.00 | 2822 |
| Want no more | 29.5 | 36.0 | 2.43*** | 1178 |
| Participant’s education level | ||||
| No education | 56.6 | 15.3 | 1.00 | 2265 |
| Primary or middle | 19.5 | 29.7 | 2.33*** | 779 |
| Secondary or higher | 23.9 | 39.4 | 3.60*** | 956 |
| Wealth quintiles | ||||
| First/poorest | 20.0 | 8.1 | 1.00 | 802 |
| Second | 20.0 | 14.9 | 1.99** | 800 |
| Middle | 20.0 | 26.7 | 4.15*** | 800 |
| Fourth | 19.9 | 32.0 | 5.34*** | 798 |
| Fifth/richest | 20.0 | 37.6 | 6.85*** | 800 |
| Total | 100.0 | 23.9 | 4000 | |
* P < 0.01, ** P < 0.05, *** P < 0.01
Column 2 of Table 1 shows the percentage of women who were using a contraceptive method at the time of the survey, by independent variables. Overall, 24% of women who had a live birth in the 2 years before the survey were using a contraceptive method at the time of the survey. Use of contraception increased with the number of ANC visits: 32% of women with four or more ANC visits were using contraception, compared with 18% of women who made between 1 and 3 antenatal visits and 8% of women who did not make an antenatal visit.
Urban residence was associated with higher use of contraception: 34% of urban women and 14% of rural women were current users of contraception. Contraceptive use appears to increase with the age of the youngest child: 27% of women with children older than 1 year used contraception compared with 22% of women with children below 1 year of age. Contraceptive use increased with the number of living children: 28% of women with three or more children used a contraceptive method, compared with 15% of women with only one child. Compared with women who wanted an additional child or were undecided, contraceptive use was nearly twice as high among women who did not want an additional child: 36% of women who did not want another child used a contraceptive method, compared with 19% of other women.
Education and wealth were associated with higher contraceptive use. Women with secondary or higher education use contraception at a rate nearly three times higher than that of women with no education: 39% of women with secondary education use a contraceptive method, compared with 15% of women with no education. Women in the fifth/richest quintile used contraception at nearly five times the rate of women in the first/poorest quintile: 38% of women in the fifth/richest quintile use a contraceptive method, compared with 8% of women in the first/poorest quintile.
Column 3 shows the unadjusted odds of contraceptive use. At the bivariate level, the associations between all independent variables and contraceptive use were statistically significant.
Table 2 shows the adjusted odds of contraceptive use by independent variables. After adjusting for other variables, contraceptive use increased with the number of ANC visits: women who made between 1 and 3 antenatal visits had 2.31 times higher odds of contraceptive use compared with women who did not make an antenatal visit: women who made four or more antenatal visits had 3.37 times higher odds of contraceptive use compared with women who did not make an antenatal visit.
Table 2.
Adjusted odds of contraceptive use, by use of ANC and sociodemographic factors
| Adjusted odds ratios | 95% confidence intervals | |
|---|---|---|
| Number of ANC visits | ||
| 0 | 1.00 | |
| 1–3 | 2.31*** | 1.63–3.28 |
| 4 or more | 3.37*** | 2.35–4.85 |
| Residence | ||
| Urban | 1.83*** | 1.41–2.38 |
| Rural | 1.00 | |
| Age of last child | ||
| 1–6 months | 1.00 | |
| 7–12 months | 1.11 | 0.86–1.43 |
| 13–18 months | 1.55** | 1.17–2.04 |
| 19–24 | 1.60** | 1.20–2.14 |
| Number of living children | ||
| 1 | 1.00 | |
| 2 | 1.79*** | 1.36–2.35 |
| 3 or more | 2.43*** | 1.85–3.20 |
| Desire for more children | ||
| Want more, undecided | 1.00 | |
| Want no more | 2.16*** | 1.73–2.70 |
| Education | ||
| No education | 1.00 | |
| Primary or middle | 1.58*** | 1.21–2.01 |
| Secondary or higher | 2.20*** | 1.68–2.88 |
| Wealth quintiles | ||
| First/poorest | 0.55** | 0.37–0.81 |
| Second-fifth/richest | 1.0 | |
| Pseudo R2 | 14.08% | |
* P < 0.01, ** P < 0.05, *** P < 0.01
Relative to living in a rural area, urban residence was associated with a 1.83 times higher odds of contraceptive use. Compared with having a child below 6 months of age, having a child older than 1 year was associated with a 1.60 times higher odds of contraceptive use. Relative to women with one child, women with two living children had a 1.79 times higher odds of contraceptive use, while women with three or more children had a 2.43 times higher odds of contraceptive use. Women who wanted no more children had approximately twice the odds of contraceptive use relative to women who wanted an additional child or were unsure about their future fertility desires. Primary- or middle-level education (odds ratio = 1.58) and secondary or higher education (odds ratio = 2.20) were strongly associated with a higher odds of contraceptive use. Women in the poorest quintile had a lower odds of contraceptive use compared with women in the other four quintiles (odds ratio = 0.55). After adjusting for other factors, there were no other differences in contraceptive use by wealth quintiles. Overall, the model explained ∼14% of the variance in the outcome.
Figure 1 compares the influence of independent variables on contraceptive use in Sindh. Marginal effects are presented. Of all variables in the model, ANC has the strongest effect on contraceptive use: women who make an antenatal visit have a 13% percentage point higher chance of contraceptive use within 2 years of delivery; women who make four or more ANC visits have a 19 percentage point higher change of contraceptive use within 2 years of delivery.
Urban residence is associated with a 9 percentage point higher chance of contraceptive use than rural residence. Having a child older than 1 year is associated with a 7 or 8 percentage point higher chance of contraceptive use. Women with two children have a 9 percentage point higher chance of contraceptive use, while women with three or more children have a 14 percentage point higher chance of contraceptive use. Women who want no more children have a 13 percentage point higher chance of contraceptive use. Primary education increases the chance of contraceptive use by 7 percentage points, while secondary education increases the chance of contraceptive use by 13 percentage points. Women in the poorest quintile have a 9 percentage point lower chance of contraceptive use.
ANC: an opportunity for reaching women
Figure 2 shows a Venn diagram that shows overlaps between use of ANC during the last pregnancy, the desire to not have an additional child and the use of family planning at the time of the survey.
Of the 24% of women in Sindh who were current contraceptive users, 96% made an ANC visit during their last pregnancy. Although the ANC visit was nearly universal among contraceptive users, the majority of women who made an ANC visit and did not want another child were not using contraception: 60% of women who used ANC during their last pregnancy and did not want another child were not using contraception at the time of the survey.
Discussion
Our study found that ANC visits are a significant predictor of contraceptive adoption in Sindh province, even after adjusting for urban residence, education, household wealth, number of living children and fertility desires—factors that are known to influence contraceptive adoption. There was a dose–response relationship between ANC use and contraceptive adoption: compared with women who did not make an ANC visit, women with between 1 and 3 ANC visits had twice the odds of contraceptive use, and women with at least four ANC visits thrice the odds of contraceptive use. These findings are consistent with findings from multi-country studies that have used more sophisticated econometric techniques to show that an index of MCH service utilization independently predicts contraceptive use in a wide range of service delivery contexts. Our study contributes to the literature by specifically focusing on the ANC visit, which is one component of maternal and child health services. Earlier studies have not looked at the relationship between ANC use per se and contraceptive adoption.
The ANC visit offers a unique touch point with a large cross section of Pakistani women, including women from the poorest and most isolated communities, who may not have the level of family support needed to adopt contraception. In Sindh, 60% of women in the lowest wealth quintile made at least one ANC visit and 18% made at least four ANC visits (Agha and Williams 2013). A focus on the ANC visit lends itself to the development of tangible strategies to reach a broad spectrum of women with family planning counselling and services. ANC is not stigmatized in Pakistan and families from varied socioeconomic backgrounds support mothers-to-be in getting a health-related checkup during their pregnancy. The ANC visit has the potential to serve as a catalyst for changing Pakistani women’s willingness and opportunity to adopt family planning. These findings are important because of limited available evidence of best strategies to integrate maternal health care with family planning in a manner that will improve health outcomes (Dudley and Garner 2011; Ahmed et al. 2013).
This study does not tell us what it is about an ANC visit that might encourage Pakistani women to use contraception. One possibility is that repeated ANC visits help build a relationship of trust between the provider and the client, which helps a provider overcome her own barriers towards the provision of advice on family planning and simultaneously reduces a client’s fears of using family planning. Trust in providers is one of the major barriers to contraceptive adoption in Pakistan (Agha 2010). Until recently, the focus of the national family planning programme in Pakistan was on the reduction of population growth by limiting childbearing through the promotion of female sterilization. Longer term methods such as the IUD or hormonal methods such as the oral contraceptive and the injectable have not been accepted by Pakistani women because of fears that these methods will harm their reproductive abilities (Carton and Agha 2012). Husbands are also concerned about the negative health effects of contraception (Agha 2010). The lack of follow-up mechanisms available for clients who have experienced side effects has contributed to apprehensions about contraceptive use and has strengthened women’s perception of poor health associated with the use of contraception (Khan et al. 2013). These fears are thought to be a major reason for the much higher rates of adoption of less effective methods such as condoms and withdrawal compared with clinical or hormonal methods (Carton and Agha 2012).
Providers in Pakistan are often reluctant to initiate a discussion about the adoption of family planning with female clients because of the fear of backlash from clients’ families (Sarfaraz et al. 2010). Moreover, providers are often not trained sufficiently well to provide family planning counselling and services (Fikree et al. 2005). Counselling of clients who receive family planning services is very poor: one study found that only 33% of Pakistani women who received a contraceptive method were counselled on side effects at the time of method adoption (National Institute of Population Studies and ICF International 2013). Often, providers lack self-confidence in the provision of family planning. Many providers have concerns about the medical safety of clinical methods, which serve as a barrier to their provision of advice about contraceptive adoption (Agha et al. 2011).
The strengths of this study are its reliance on a large, representative sample from Sindh and with standard questions adopted from the 2012to 2013 Demographic and Health Survey of Pakistan. Data with this level of detail for a single province are rarely available in Pakistan. The focus of the survey on the 2-year period following a live birth is useful, as this is a particularly important time for improving health outcomes through birth spacing. A limitation of this study is that it is based on cross-sectional data and cannot demonstrate that the use of ANC led to the adoption of family planning. Another limitation is the reliance on reported information from mothers about their pregnancy and childbirth experience.
Whether health providers in Pakistan counsel women on contraceptive use during an ANC visit is not known. Indirect evidence from the 2012 to 2013 Pakistan Demographic and Health Survey which shows that 6% of women who visited a health facility in the last 12 months discussed family planning (National Institute of Population Studies and ICF International 2013) as well as informal reports from technical, service delivery related, personnel suggest that such counselling is not being provided. Nor is there is any programmatic emphasis on the provision of family planning counselling during an antenatal visit, reflected by the lack of monitoring of this behaviour. Data is urgently needed to determine the extent to which family planning counselling takes place during an ANC visit. In addition, operations research is needed to determine how best to increase the frequency and quality of family planning counselling during an ANC visit. A strategy that increases providers’ capacity and willingness to provide birth spacing counselling to pregnant women has the potential to substantially increase contraceptive use and reduce unmet need among women in Pakistan.
This strategy should be developed jointly by the provincial Departments of Health and Population. Although functional integration of Departments of Health and Population has been slow, there are some positive signs: the Population Welfare Department has been providing contraceptives to the Department of Health, which was not happening until 2012 (Technical Resource Facility 2012). There may be an opportunity for the Population Welfare Department to contribute to strengthening the impact of the ANC visit on future contraceptive adoption.
Conclusion
ANC visits present an excellent opportunity to provide counselling on contraception. It is important for programmes to increase efforts to increase the frequency and quality of family planning counselling during an ANC visit. Since most women in Sindh now use ANC, an ANC visit may be the most cost-efficient way of reaching women with family planning messages via interpersonal communication. Discussion of birth spacing with a provider is strongly associated with contraceptive adoption in Pakistan (Fikree et al. 2001). Several studies have suggested that limits on women’s mobility may be a significant barrier to contraceptive adoption in Pakistan (Mumtaz and Salaway 2005). The ANC visit is an ideal opportunity to reach women who have already overcome many barriers to health service utilization and reached a health facility. By providing women who have reached a health facility with a better understanding of what family planning use entails, including an understanding of side effects that may occur, Pakistani women’s opportunity to make an informed decision about contraceptive adoption may be substantially increased.
Acknowledgements
This publication was made possible through support provided by the US Agency for International Development (USAID), under the terms of Associate Cooperative Agreement No. AID-391-LA-13-00001; Maternal, Newborn and Child Health Services Project. The opinions expressed herein are those of the author and do not necessarily reflect the views of USAID.
Conflict of interest statement. None declared.
Ethical approval
The study was approved by institutional review boards from the Johns Hopkins Bloomberg School of Public Health and the National Bioethics Committee of Pakistan.
References
- Agha S. 2010. Intentions to use contraceptives in Pakistan: implications for behavior change campaigns. BMC Public Health.www.biomedcentral.com/1471‐2458/10/450, accessed 26 January 2015.
- Agha S. 2013. Substantial Increases in Institutional Delivery in Sindh Province Along With Low Quality Service Provision.http://jhpiego.pk/site/wp-content/uploads/2015/01/IID_QoC_SA_16‐19Sept13.pdf, accessed 26 January 2015.
- Agha S, Fareed A, Keating J. 2011. Clinical training alone is not sufficient to reducing barriers to IUD provision among private providers in Pakistan. http://www.reproductive-health-journal.com/content/8/1/40, accessed 26 January 2015.
- Agha S, Williams E. 2013. Maternal and Child Health (MCH) Program Indicator Survey, Sindh Province. Karachi: USAID/Pakistan MCH Program. http://jhpiego.pk/site/annual-household-survey/mch13/, accessed 15 January 2015.
- Ahmed S, Mosley WH. 2002. Simultaneity in the use of maternal-child health care and contraceptives: evidence from developing countries. Demography 39: 75–93. [DOI] [PubMed] [Google Scholar]
- Ahmed S, Norton M, Williams E, Ahmed S, Shah R, Begum N. 2013. Operations research to add postpartum family planning to maternal and neonatal health to improve birth spacing in Sylhet District, Bangladesh. Global Health Science and Practice 12: 262–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartus T. 2005. Estimation of marginal effects using margeff. Stata Journal 5: 309–29. [Google Scholar]
- Carton TW, Agha S. 2012. Changes in contraceptive use and method mix in Pakistan: 1990–91 to 2006–07. Health Policy and Planning 27: 166–74. [DOI] [PubMed] [Google Scholar]
- Casterline JB, Sathar ZA, ul Haque M. 2001. Obstacles to contraceptive use in Pakistan: a study in Punjab. Studies in Family Planning 32: 95–110. [DOI] [PubMed] [Google Scholar]
- Do M, Hotchkiss D. 2013. Relationship between antenatal and postnatal care and post-partum modern contraceptive use: evidence from population surveys in Kenya and Zambia. BMC Health Services Research.www.biomedcentral.com/1472‐6963/13/6, accessed 24 May 2015.
- Dudley L, Garner P. 2011. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. Cochrane Database Systematic Reviews 7: CD003318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fikree FF, Khan A, Kadir MM, Sajan F, Rahbar MH. 2001. What influences contraceptive use among young women in urban squatter settlements of Karachi, Pakistan?. International Family Planning Perspectives 27: 130–6. [Google Scholar]
- Fikree FF, Saleem S, Sami N. 2005. A quality of care issue: appropriate use and efficacy knowledge of five contraceptive methods: views of men and women living in low socioeconomic settlements of Karachi, Pakistan. Journal of the Pakistan Medical Association 55: 363–8. [PubMed] [Google Scholar]
- Filmer D, Pritchett L. 2001. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 38: 115–32. [DOI] [PubMed] [Google Scholar]
- Hotchkiss DR, Magnani RJ, Rous JJ, Azelmat M, Mroz TA, Heikel J. 1999. The effects of maternal-child health service utilization on subsequent contraceptive use in Morocco. Journal of Biosocial Science 31: 145–65. [DOI] [PubMed] [Google Scholar]
- Khan AA, Khan A, Javed W, Hamza HB, Orakzai M, Ansari A. 2013. Family planning in Pakistan: applying what we have learned. Journal of the Pakistan Medical Association 63: S3–10. [PubMed] [Google Scholar]
- Mumtaz Z, Salway S. 2005. “I never go anywhere”: extricating the links between women’s mobility and uptake of reproductive health services in Pakistan. Social Science and Medicine 60: 1751–65. [DOI] [PubMed] [Google Scholar]
- Nasrullah M, Muazzam S, Bhutta ZA, Raj A. 2014. Girl child marriage and its effect on fertility in Pakistan: findings from Pakistan demographic and health survey, 2006–2007. Maternal Child Health Journal 18: 534–43. [DOI] [PubMed] [Google Scholar]
- National Institute of Population Studies and ICF International. 2013. Pakistan Demographic and Health Survey 2012–13. Islamabad, Pakistan, and Calverton, Maryland, USA: National Institute of Population Studies and ICF International. [Google Scholar]
- Nishtar S, Boerma T, Amjad S, Alam AY, Khalid F, ul Haq I. 2013. Pakistan’s health system: performance and prospects after the 18th Constitutional Amendment. Lancet 381: 2193–206. [DOI] [PubMed] [Google Scholar]
- Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. 2012. World Population Prospects: The 2012 Revision.http://esa.un.org/unpd/wpp/index.htm, accessed 27 January 2015. [PubMed]
- Royan R, Sathar Z. 2013. Population Trends in Pakistan. Population Council Book Series. www.onlinelibrary.wiley.com/doi/10.1002/j.2326‐4624.2013.tb00012.x/pdf, accessed 26 January 2015.
- Rutstein SO, Johnson K. 2004. The DHS Wealth Index. DHS Comparative Reports No. 6. Calverton, United States: ORC Macro. [Google Scholar]
- Sarfaraz A, Fashi S, Hussain SS. 2010. Care to Counsel. Social Marketing Campaign to Raise Awareness among Health Care Providers in Green Star’s Network. Karachi, Pakistan: Institute of Business Administration. [Google Scholar]
- Sathar ZA, Singh S, Fikree FF. 2007. Estimating the Incidence of Abortion in Pakistan. Studies in Family Planning 38: 11–22. [DOI] [PubMed] [Google Scholar]
- Seiber EE, Hotchkiss DR, Rous JJ, Berruti AA. 2005. Maternal and child health and family planning service utilization in Guatemala: implications for service integration. Social Science and Medicine 61: 279–91. [DOI] [PubMed] [Google Scholar]
- StataCorp. 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. [Google Scholar]
- Technical Resource Facility. 2012. Mid Term Evaluation of the National Maternal and Child Health Programme in Pakistan. Findings an Recommendations.http://www.trfpakistan.org/LinkClick.aspx?fileticket=0WOWUr-6vQI%3D&tabid=2618, accessed 1 May 2015.
- Yadav D, Dhillon P. 2015. Assessing the impact of family planning advice on unmet need and contraceptive use among currently married women in Uttar Pradesh, India. PLoS One http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0118584, accessed 24 May 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]