Abstract
Introduction:
Male infertility factor is defined if the total number of motile spermatozoa (TMSC) < 20 × 106/ejaculated, and unexplained infertility if spermiogram is normal with normal female factor.
The aim:
of this study was to determine the predictive value of TMSC for spontaneous pregnancy (ST) and pregnancy after treatment with intrauterine insemination (IUI) in couples with male factor and unexplained infertility.
What is known already:
According to the WHO qualification system abnormal spermiogram can be diagnosed as oligozoospermia (O), asthenozoospermia (A), teratozoospermia (T) or combination (O+A+T) and azoospermia (A). Although this classification indicates the accuracy of findings its relevance for prognosis in infertile couple and the choice of treatment is questionable.
Materials and Methods:
The study included 98 couples with male infertility factor (bad spermiogram) and couples with normospermia and normal female factor (unexplained infertility). Testing group is randomized at: group (A) with TMSC> 3,106 / ejaculate and a spontaneous pregnancy, group (B) with TMSCl <3 x 106 / ejaculate and pregnancy after IUI, plus couples who have not achieved SP with TMSC> 3 x 106 / ejaculate and couples who have not achieved pregnancy.
Main results:
From a total of 98 pairs of men’s and unexplained infertility, 42 of them (42.8%) achieved spontaneous pregnancy, while 56 (57.2%) pairs did not achieve spontaneous pregnancy. TMSC was significantly higher (42.4 ± 28.4 vs. 26.2 ± 24, p <0.05) in the group A compared to group B. Couples with TMSC 1-5 × 106 ejaculate had significantly lower (9.8% vs. 22.2%, p <0.0001) rate of spontaneous pregnancy in comparison to couples after IUI treatment. Couples with unexplained infertility had significantly higher (56.8% vs. 29.9%, p <0.01) spontaneous pregnancy rate compared to couples after IUI treatment. Infertile couples had significant pregnancy rate with TMSC 5-10 x 106 / ejaculate (OR = 1.45, 95% CI:1.26-1.78, <0.01); with TMSC 10-20 x 106 / ejaculate (OR = 1.36, 95% CI: 1:12 to 1:46, <0.0001) with TMSC> 20 x 106 / ejaculate (RR = 1.7, 95% CI: 1.56-1.82, <0.001) after treatment with IUI compared to spontaneous pregnancy.
Conclusion / interpretation:
Based on these results we can conclude that couples with the TMSC> 5 x 106 / ejaculate are indicated for treatment with IUI. TMSC can be used as the method of choice for diagnosis and treatment of male infertility.
Keywords: Total motile sperm count, Male infertility, Unexplained infertility, Intrauterine insemination, Spontaneous ongoing pregnancy rate
1. INTRODUCTION
The World Health Organization (WHO) designated the infertility as a disease, and its treatment as one of the fundamental human rights. Infertility is defined as the inability to conceive after 1 year of unprotected relations of couples in the reproductive age (1). Male infertility factor is the most common cause of not having children (2, 3). The diagnosis is based on the results of the analysis of semen. The WHO revised and defined cut-off value for differentiating normal and abnormal semen (4). Van der Steeg and his associates in 2011, tried to check the WHO criteria parameter analysis of seed in 1999 (5) for a spontaneous pregnancy, and it was concluded that the predictive value of the WHO classifications seed analysis was deficient. In other words, although the WHO proposed classification accuracy of seed analysis, relevance for prognosis and treatment choices are bad (6). The parameter for assessing the quality of sperm is the total motile sperm count (TMSC). The total number of mobile sperm has a better predictive value for spontaneous pregnancy (ST) then of the WHO classification system. Sperm morphology parameter is not used in this calculation (7). Van der Weert et al. (2004) showed in a meta-analysis of 16 studies that post wash TMSC between 0.8 × 106 and 5 × 106 has a prognostic value in couples who underwent IUI (8). Badawy et al. (2009) showed that the IUI is less successful when TMSC post wash is low with poor morphology (9). So, there is a need for new parameter values in seed analysis for clinical use in sorting out male infertility factors and selecting the treatment. The majority of the published studies show that IUI is more effective than planned sexual intercourse regardless of whether they are couples with unexplained infertility or male infertility. Intrauterine insemination shows a significant increase in pregnancy rates compared to the planned time sexual intercourse in natural cycles, regardless of the type of infertility (OR = 2.43) (10). The aim of this study was to determine the predictive value TMSC for spontaneous pregnancy (ST) and pregnancy after treatment with IUI in couples with male factor and unexplained infertility.
2. MATERIALS AND METHODS
Study design
Prospective study included examination of 223 infertile couples for marriage infertility with duration longer than 1 year. The study was conducted from January 2013 throughout December 2015 in the Department of Human Reproduction “Dr Hajder” Tuzla. Treatment of infertility was conducted in accordance with the guidelines for infertility (NICE) and consists of the examinations of both partners. All married couples underwent the following examinations: spermiogram, analysis of sex hormones in the early follicular phase of the cycle, ultrasonic cycle monitoring (folliculometry), mid-luteinizing progesterone measuring, microbiological and immunological treatment of the infection, hystero sonosalpingographia, diagnostic laparoscopy in indicated cases.
Study population
Total cohort consisted of 223 infertile couples. Of these, 115 pairs were excluded from the study due to female factor infertility, such as disorders of ovulation, tubal disease, endometriosis, cervical factor or sexual dysfunction. The study also excluded couples with a combination of female and male factors, couples in which the male partner had azoospermia and couples with TMSC <1 x 106 / ejaculate. The study included 98 couples with male infertility factor (bad spermiogram) and couples with normospermia and normal female factor (unexplained infertility). The study group was randomized to: group (A) with TMSC> 3x106 / ejaculate and a spontaneous conception; group (B) with TMSC <3 x 106 / ejaculate and conception after IUI, plus couples who did not achieve SP with TMSC> 3 x 106 / ejaculate and couples who did not achieve pregnancy. Both groups were classified in five subgroups based on TMSC subgroup (1) with TMSC 1-5 × 106 / ejaculate; subgroup (2) with TMSCl 5-10 × 106 / ejaculate; subgroup (3) with TMSCl 10-20 × 106 / ejaculate; subgroup(4) with TMSCl> 20 × 106 / ejaculate and subgroup (5) with unexplained infertility
Definition. Infertility is defined as the failure of conception, despite 12 months of unprotected intercourse (Ciglar). Normozoospermia is defined according to the WHO criteria, 2010. TMSC is calculated by multiplying the concentration of sperm / milliliter (SC) x volume (ml) x motility (A + B) divided by 100%. Sperm is normal if TMSC> 20 × 106 / ejaculate, lower values are considered abnormal spermiogram and define male infertility factor. Infertile couples with normozoospermia and normal female factor were considered unexplained infertility. The normal menstrual cycle is between 25 and 35 days, the level of progesterone in the medium luteal phase is> 27 mmol / l, the duration of the luteal phase > 11 days.
Treatments
Couples with TMSC> 3x106 / ejaculate, with the chance of conceiving> 30% (mild cases)were given an advice on planned sexual relations with ultrasound monitoring of follicular growth. Six IUI cycles were offered to couples with TMSC from 1 to 3 x 106 / ejaculate with a forecast of conception <30% (moderate male infertility), and couples with TMSC> 3 x 106 / ejaculate with a conception prognosis> 30%, that did not achieve SPafter 6 months of planned sexual intercourse. After six unsuccessful IUI cycles couples were offered in vitro fertilization (IVF) and were excluded from the study. Couples with TMSC <1 × 106 / ejaculate were immediately offered in vitro fertilization by intracytoplasmic sperm injection (ICSI) and were excluded from the study.
Outcome measures
The primary objective was to determine the rate of spontaneous pregnancies without treatment and pregnancy rates after IUI treatment. Pregnancy is defined by ultrasound measurement of the fetal heart beat after the 12th week of pregnancy, and increased b-hCG after 1-2 days of the period, the values of which should be doubled when re-measurement after 48-72 hours.
Semen analysis
The men had their spermiogram made on arrival at the Institute. In the case of abnormal spermiogram, a second sample was analyzed 10 weeks later. Male partners gave a semen sample after 2-3 days of sexual abstinence. The seeds were stored in the Institute in sterile plastic container, or at home and delivered to the laboratory of the Institute within 1 hour. During the analysis volume was measured by a numbered syringes. The sperm was read in Megler chamber, with an increase of 200 times MAKLER COUNTING CHAMBER for rapid sperm analysis (11). Mobility was expressed as a percentage of: (A) fast forward progressive sperm, (B) slowly forward progressive, (C) non-progressive (D) immovable sperm within the total number of 200 sperm in at least five fields, according to WHO guidelines (WHO, 2010) . Sperm morphology was scored according to the criteria of Tygerberg (12), 200 spermatozoas were analyzed. This study used a floating techniques of seed processing that is simple and inexpensive. Treated seed is then inseminated with soft catheter (MedGyn intrauterine insemination catheter, MedGyn Products, Inc., USA).
Statistics
The data were entered into a database. Statistical analysis was performed by application software called SPSS for Windows version 16.0 (Statistical Package for Social Sciences, SPSS, Chicago, IL, USA) that was used for this analysis.
Numerical data were presented as mean + -SD, the absolute number is expressed in%, 95% confidence interval (CI). To test the hypothesis between the groups independent students t–test and Fisher exact test (univariate analysis) were used, with the level of significance of p <0.05. A binary logistic regression was performed for the dependent variable (such as pregnancy), which has two endpoints, i.e. spontaneous pregnancy and pregnancy after treatment IUI. Relative risk ratio (RR) and their 95% confidence interval (CI) was calculated for each subgroup TMSC.
3. RESULTS
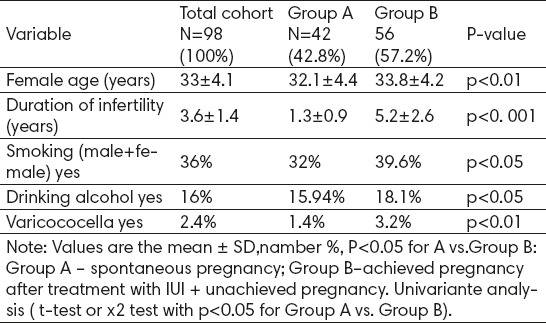
The study included a total of 223 couples with marital infertility. After examination of patients, 115 of them (55%) had a female infertility factor, and were excluded from the study. According to the WHO criteria, after seed analysis, 108 pairs (45%) had male infertility factor, of which 10 (11%) had azoospermia and were excluded from the study. The study included 98 (89%) of couples with male and unexplained infertility. After analyzing semen according to the WHO criteria 76 couples (77.5%) had male infertility and unexplained infertility 22 (22.5%) pairs. According to TMSC range, male infertility, i.e.. Abnormal semen was found in 56 (57.1%) pairs, and unexplained infertility and unexplained infertility with normozoospermia 42 (42.9%) pairs. Results of clinical parameters in pairs with male factor and unexplained infertility who achieved the spontaneous pregnancy, pregnancy after treatment with IUI plus pairs which did not achieve any pregnancy are presented in Table 1. Of the total of 98 pairs, 42 (42.8%) achieved spontaneous pregnancy, while 56 (57.2%) pairs did not achieved spontaneous pregnancy. Results of univariate analysis showed significantly lower values of age (p <0.01), duration of infertility (p <0.001), less cigarette smokers (p <0.05), less surgical treated varicocele (p <0.01) in the group A, compared to the group B.
Table 1.
Baseline clinical characteristics of couples with male infertility and unexplained
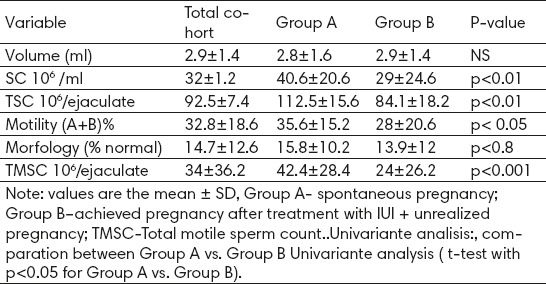
Results of univariate analysis of medium parameter TMSC were significantly higher in the group (A) compared to the group B. In the subgroup A statistically significant higher values of the concentration of seeds were identified(SC) (p <0.01), the concentration of the total number of seeds (TSC) (p <0.01), semen motility (A + B)% (p <0.01) and total motile sperm count (TMSC) (p <0.001) in comparison to the group B, while there were no significant differences in the parameters of the volume of the seeds between the groups (Table 2).
Table 2.
The basal characteristics of the parameters of semen analysis in couples with male factor and unexplained infertility
After sorting the pairs by categories of the quality of the seeds, the results of univariate analysis showed that couples with TMSC with <5 × 106 / ejaculate had a significantly lower chance of spontaneous pregnancy than couples with TMSC with> 5 × 106 / ejaculate. Couples with TMSCl 1-5 × 106 /ejaculate showed significantly lower (p <0.01) chances of the spontaneous pregnancy compared to the pairs after IUI treatment. Couples with unexplained infertility had significantly higher rate of spontaneous pregnancy (p <0.01) compared to pairs after treatment. The difference was not significant (NS) in the categories of TMSC with TMSC 5-10; 10-20:> 20 x 106/ejaculate in a group A compared to the group B (Table 3).
Table 3.
TMSC groups sorted by the quality seeds categories of couples with male factor and unexplained infertility
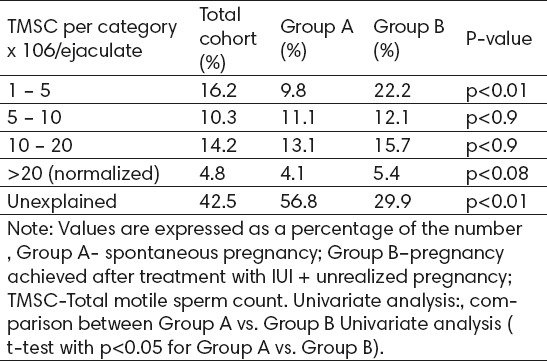
Table 4 shows a comparison between RR spontaneous pregnancies and pregnancies after IUI treatment according to TMSC categories. Infertile couples that are sorted by categories with TMSC 5-10; 10-20; > 20 x 106 / ejaculate had a significantly higher pregnancy rates after IUI treatment. Subgroup with TMSC 5-10 x 106 / ejaculate had significantly higher (RR = 1.45, 95% CI: 1.26-1.78, <0.01) pregnancy rate in group II than in the group I.
Table 4.
Rate comparisons of spontaneous pregnancies (group I) and total pregnancies (I + II) after treatment sorted by TMSC categories in couples with male factor and unexplained infertility.
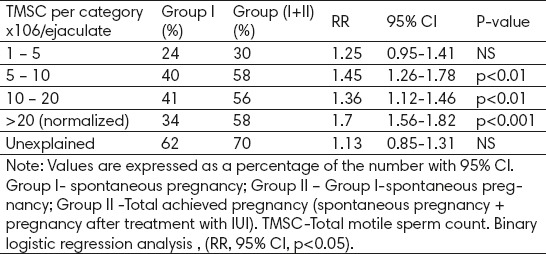
Subgroup with TMSCl 10-20 x 106 / ejaculate showed higher (RR = 1.36, 95% CI: 1:12 to 1:46, <0.01) pregnancy rate in group (I + II) in comparison with group I. Subgroup with TMSC > 20 x 106 / ejaculate showed higher (RR = 1.7, 95% CI: 1.56-1.82, <0.001) pregnancy rate in group (I + II) in comparison to group I. While there were no significant difference t (NS) in TMSC subgroup with 1-5 x 106 / ejaculate and subgroup with unexplained infertility after IUI treatment in comparison to the rate of spontaneous pregnancy.
4. DISCUSSION
According to the new WHO classification system normozoospermia is based on the cut-off values obtained on a sample of 1,953 couples with proven fertility. Although this classification indicates the accuracy, relevance for prognosis in infertile couple and the choice of treatment is questionable. Abnormal spermiogram can be diagnosed as oligozoospermia (O), astenozoospermia (A), teratozoospermia (T) or a combination of these, and azoospermia (image x) .. TMSC is obtained by multiplying the volume of semen x concentration x the percentage of concentration of A and B sperm divided by 100. TMSC shows a better correlation with spontaneous pregnancy rate (SOPR) than the WHO classification system from 2010. For everyday practice, there are three prognostic groups: couples with TMSCl <5 × 106, couples with TMSC 5- 20 x 106 and couples with TMSCl greater than 20 × 106 ejaculate normozoospermia (7). It is significant to point out that there is no difference in SOPR if TMSC was <1 × 106, 106 × 1-3 or 3-5 × 106. Spontaneous pregnancy are possible in the presence of extremely poor quality of sperm, although most doctors recommend ICSI. However it was noted that a quarter of couples conceived spontaneously. There is still evidence that the semen analysis is weak predictor of pregnancy in the low range (13) 345 consecutive couples presenting for subfertility. It is also illogical that 20% of couples with unexplained infertility and normospermia did not conceive (7). The National Institute for Health and Care (NICE) guidelines in fertility recommended repeated spermiogram in the event that the first was abnormal (7).
Results of this study showed that spontaneous pregnancy are present in all subgroups of TMSC. After treatment with IUI there was a statistically significant increase in pregnancy rates in the subgroup of TMSC> 5 x 106 ejaculate, while in sub-groups with TMSC <5 x 106/ejaculate and unexplained infertility after IUI pregnancies were reported, but without statistically significant differences. IUI is less expensive and less invasive than other ART methods, and this therapeutic treatment should be offered to couples with male factor and unexplained infertility as the first choice of treatment (14). Intrauterine insemination shows a significant increase in pregnancy rates compared to the planned time sexual intercourse in natural cycles, regardless of the type of infertility (OR = 2.43). In the analysis of 3,662 cycles showed that intrauterine insemination shows a significant increase in pregnancy rates compared to the planned time sexual intercourse in natural cycles, regardless of the type of infertility (OR = 2.43). It is also proven that the cycles of intrauterine insemination with controlled ovarian hyperstimulation (COH) show higher pregnancy rates (OR = 2.2) compared to the time planned intercourse in a natural cycle (10). Ayala et al. (1996) showed that in the group of 1,055 infertile couples TOPR was significantly higher if the TMSC was greater than 25 × 106 ejaculate compared to TMSC under 25 × 106/ejaculate [RR = 6.1. 95% CI: 7.4.-9.7] (15) 055 infertile couples seen at the Texas Institute for Reproductive Medicine and Endocrinology for a total of 9,409 follow-up months. The medians of sperm concentrations (SC. Van der Weert et al. (2004) showed in a meta-analysis of 16 studies that post wash TMSC between 0.8 × 106 and 5 × 106 ejaculate had prognostic value in couples undergoing IUI (8). Badawy et al. (2009) showed that the IUI was less successful when the total number of motile spermatozoa was low and post wash morphology was bad (9). Hamliton et al. (2015) in their study indicated that TMSC is better diagnostic and prognostic method for male infertility factor (7). Pregnancy after IUI were present in all subgroups TMSC, even in subgroups with TMSC <1 x 106 ejaculate.
5. CONCLUSION
TMSC is a better method for the classification of male infertility factor than the WHO classification system. IUI should be used as first-line therapy method of ART for male infertility factor with TMSC> 5 x 106 ejaculate and unexplained infertility.
Footnotes
• Author’s contribution: All authors contributed in all phases of preparing this article. Final proof reading was made by first author.
• Conflict of interest: none declared.
REFERENCES
- 1.Hajder M, Hajder E i suradnici. In: Neplodnost i reproduktivna endokrinologija. Tuzla: OFF SET, Tuzla; 2011. Indukcija ovulacije. [Google Scholar]
- 2.Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, et al. Population study of causes, treatment, and outcome of infertility. Br Med J (Clin Res Ed) 1985;291:1693–7. doi: 10.1136/bmj.291.6510.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brandes M, Hamilton CJCM, van der Steen JOM, de Bruin JP, Bots RSGM, Nelen WLDM, et al. Severity of oligo-asteno-teratozoospermia no longer determines overall success rate in male subfertility. Int J Androl. 2011;34(6 Pt 1):614–23. doi: 10.1111/j.1365-2605.2010.01128.x. [DOI] [PubMed] [Google Scholar]
- 4.Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HWG, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45. doi: 10.1093/humupd/dmp048. [DOI] [PubMed] [Google Scholar]
- 5.WHO. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. World Health Organization 1999. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- 6.Esteves SC, Zini A, Aziz N, Alvarez JG, Sabanegh ES, Agarwal A. Critical appraisal of world health organization's new reference values for human semen characteristics and effect on diagnosis and treatment of subfertile men. Urology. 2012;79(1):16–22. doi: 10.1016/j.urology.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton JM, Cissen M, Brandes M, Smeenk JMJ, de Bruin JP, Kremer JM, et al. Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Hum Reprod. 2015;30(5):1110–21. doi: 10.1093/humrep/dev058. [DOI] [PubMed] [Google Scholar]
- 8.van Weert JM, Repping S, Van Voorhis BJ, van der Veen F, Bossuyt PMM, Mol BWJ. Performance of the post wash total motile sperm count as a predictor of pregnancy at the time of intrauterine insemination: a meta-analysis. Fertil Steril. 2004;82(3):612–20. doi: 10.1016/j.fertnstert.2004.01.042. [DOI] [PubMed] [Google Scholar]
- 9.Badawy A, Elnashar A, Eltotongy M. Effect of sperm morphology and number on success of intrauterine insemination. Fertil Steril. 2009;91(3):777–81. doi: 10.1016/j.fertnstert.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Miskry T, Chapman M. The use of intrauterine insemination in Australia and New Zealand. Hum Reprod. 2002 Apr 1;17(4):56–9. doi: 10.1093/humrep/17.4.956. [DOI] [PubMed] [Google Scholar]
- 11.Makler A. Biotechnology of human reproduction 2003. In: Revelli A, Tur-Kaspa I, Holte JG, Massobrio M, editors. Biotechnology of Human Reproduction. New York: Parthenon Publishing Group; 2003. pp. 115–30. [Google Scholar]
- 12.Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S. Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril. 1988;9(1):12–7. doi: 10.1016/s0015-0282(16)59660-5. [DOI] [PubMed] [Google Scholar]
- 13.van der Steeg JW, Steures P, Eijkemans MJC, F Habbema JD, Hompes PG a, Kremer JM, et al. Role of semen analysis in subfertile couples. Fertil Steril. 2011;5(3):013–9. doi: 10.1016/j.fertnstert.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 14.van Rumste MME, Custers IM, van Wely M, Koks C a, van Weering HGI, Beckers NGM, et al. IVF with planned single-embryo transfer versus IUI with ovarian stimulation in couples with unexplained subfertility: an economic analysis. Reprod Biomed Online. 2014;28(3):336–42. doi: 10.1016/j.rbmo.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Ayala C, Steinberger E, Smith DP. The influence of semen analysis parameters on the fertility potential of infertile couples. J Androl. 1996;17(6):718–25. [PubMed] [Google Scholar]


