Abstract
Introduction:
Dynamic Hip Screw fixation is currently considered as a standard treatment for pre-trochanteric fractures; however, due to the long-term hospitalization and some other complications, some researchers have proposed intramedullary nailing as the alternative surgical treatment. The aim of this study was to compare and examine the consequences of the using intramedullary nailing method versus Dynamic Hip Screw.
Methods:
In this study 114 patients with unstable Intertrochanteric fracture refer to Rasoul Akram hospital during 2011 to 2013 has been selected. After reduction, fixation surgery with PFN nail (60 patients) and Dynamic Hip Screw (54 patients) has been performed. All patients were screen during surgery and six months after surgery and some parameters like, bleeding, union, as well as complications such as collapse, varus and medialization of the distal fragment were record and patients.
Results:
About some parameters like cutting length, surgery duration, bleeding there were significant differences between two groups. In six months follow up period 2 patinas from nail and 8 patients from DHS group had non-union. Also from the point of radiologic and clinical parameters, like anterior thigh pain, cut out, medialization of the distal fragment, collapse of the neck, walking recovery and daily activities were significant between two groups.
Conclusion:
Due to the reduced hospital stay in intramedullary nailing method and the necessity of doing repeated surgery and applying intramedullary nailing when the patients are not treated with external fixation, the researchers recommend intramedullary nailing as the first option in treating such patients.
Keywords: Fracture Fixation, Intramedullary, Bone Plates, Hip Fractures, Fractures, Bone
1. INTRODUCTION
Pertrochanteric fracture is one of the most common cases that orthopedic surgeons interfere during medical treatment. Due to the substantial increase in average age of the population, exposure to these kind of fracture are increasing. Mortality and morbidity of the fracture is high because of underlying factors and despite advances in methods and orthopedic equipment, quality and results of the fixation of the fracture has been not satisfactory progressed (1, 2).
1.1. Mechanism of Injury and the Early Reviews
This damage usually happened due to falling when walking in women over fifty years although sometimes it happens in young people with severe trauma and other fractions (1). In most cases the affected limb shortens and externally rotates.
1.2. Types of Treatment
Today non-surgical treatment are less recommended and limited to patients who are high-risk for surgery. In general, a variety of surgical options can be listed as following items.
-
*
Plate structures with Bolt / Nail for head fixation;
-
*
Nail structures with Bolt / Nail for head fixation;
-
*
External Fixation;
-
*
Arthroplasty.
Fixation structures with plate divide into Impaction Class, Dynamic Compression, plates with Rotary Stability or Linear Compression and Hybrid Locking plates.
Cephalomedullary devices which is designed based on use of internal canal for fixation of long bones concept also divide into four groups: Impaction Class, Dynamic Compression, Reconstruction Nails Class and InterTAN Class.
1.3. Choosing Best Method for Internal Fixation
A review of new sources such as published articles and comments in orthopedic community reveals that among treatment options for intertrochanteric and pertrochanteric fractures, plates (CHSs) and nails (Gama and Reconstruction) are more acceptable (3-7). Although in some cases depending on the type of fracture choosing the best fixation option is quiet obvious but it seems that skill and knowledge level of surgeons with mentioned technique could affect the choice. The aim of this study is examining investment for nailing the patients and compare it with patients with treated Dynamic Hip Screw (5, 8, 9). This study, has been performed with a view to improving the technical level of orthopedic procedures and more benefit to patients.
2. MATERIALS AND METHODS
This analytical cohort has been performed during 2011 to 2013 and participants were selected from patients with intertrochanteric fracture referred to Rasol Akram Hospital in Tehran, Iran. Then patients divided to two Nail and DHS surgery groups.
2.1. Inclusion and Exclusion Criteria
Subjects with unstable intertrochanteric fractures include below items which consider as `inclusion criteria.
Posteromedial large fragment fracture;
Reverse oblique fractures;
Displaced greater trochanter fracture (Fractures of the lateral wall);
Basocervical pattern;
Failure to reduce the fracture fracture before internal fixation.
Patients older than 80 and younger than 30 years old, multiple trauma patients, have a history of hip fracture or surgery on the same side and patients without the ability to walk before the fracture has been excluded from study.
2.2. Ethical Considerations
Primary reduction has been performed on all patients then according to correct techniques listed in references fixation surgery with intramedullary nailing and PFN or DHS has been performed on all patients. Both mentioned procedures are listed as accepted and standard treatment methods for patients with intertrochanteric fraction and there is no problem in the point of moral and ethical view. Also all the radiography actions were followed the standard methods. Finally all the data and properties of the patients has been recorded and will keep secretly.
2.3. Materials
In this study Proximal Femoral Nails (PFN) has been used which made by ChM company located in Poland. These intramedullary nails distributed as CHARFIX Femoral Nail brand name.
2.4. Statistical Analysis
After gathering the data, statistical analysis has been performed with SPSS 16 (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.). To compare the data between two nail and DHS groups for quantitative data t-test and for qualitative data chi-square test has been used.
3. RESULTS
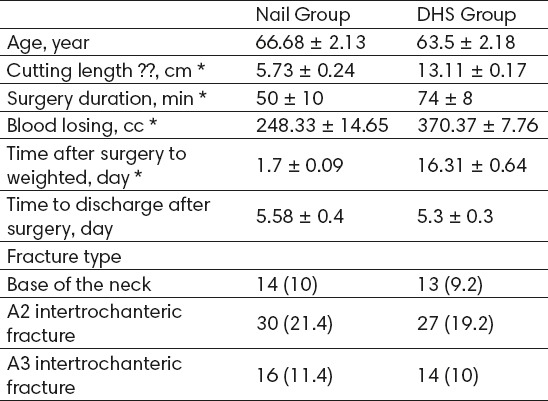
During this study fixation surgery has been performed on 75 patients with intramedullary nailing with PFN and 65 patients with DHS. Finally 60 patients with nail and 54 patients with DHS interred into 6 months follow up period. The rest were exclude from the study due to death or not coming back for further follow up. Demographic characteristics of patients are shown in Table 1.
Table 1.
Demographic Characteristics of the Patients During Surgery. Data in table are presented as Mean ± SD or No. (%). Items marked by * showed significant differences between two groups.
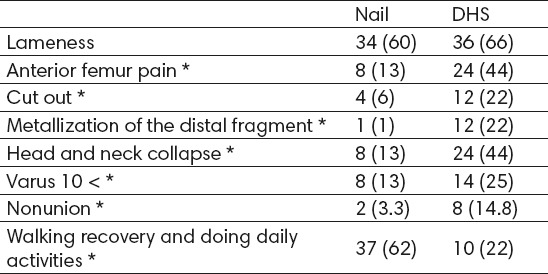
Clinical and radiologic results were recorded in third month after surgery and results are shown in Table 2. As you can see in Table 2 all the results expect lameness group showed a significant differences between two groups.
Table 2.
Clinical and Radiologic Results Three Months after Surgery. Data are presented as No. (%). Items marked by * showed significant differences between two groups.
Finally after radiographic follow up in sixth month two patients has no results of union yet. One patient had relative union and showed more recover during next months. Three patients were experienced treatment failure. One patient had femoral fractures from distal nail and one patient showed neck collapse and screw cut out. Some union cases with nailing method are shown in Figure 1.
Figure 1.

Union Cases with Nailing Method A) Base of the Neck Fracture; B) A2 Fracture; C) A3 Fracture
4. DISCUSSION
As we expect these fracture are attributed to old age caused by factors such as osteoporosis and underlying disease. Since the patients in this study were in the seventh and eighth decades of life. There are also several consideration.
In a study performed by Huat Chua et al. in 2013 in Singapore, short-term outcomes doing PFNA vs. DHS compared in patients with intertrochanteric fractures. For mentioned study 63 patients with A2 and A3 fractures were selected with mean age of 60 years old. Choosing the instrument for patient performed based on surgeon experience and type of fracture. Based on results patients with PFNA treatment after 6 and 12 months follow up had more independence movement and more score than PMS. Huat Chua et al. concluded that using PFNA in intertrochanteric fractures can be regarded as an appropriate treatment option (4).
In another study by Shen et al. in 2012 that has been designed to compare the performance and safety of PFNA vs. DHS, some factors like surgery duration, bleeding and complications of surgery has been evaluated. In this study five subjects in nailing group had lower bleeding and complications of surgery in compare with PFNA group. Also death rate showed no significant differences in both groups. Shen et al. believed that the differences between two groups are because of different level of experience in surgeons (5).
Dousa et al. in 2006 performed a study and 41 patients with A2 and A3 fractures fixed with PFN. After six months follow up 95% of patients completely recovered with maintaining the anatomical status (10). Also in a study by Windolf et al. in 2005, 121 cases of patients with nailing fixation has been followed up and resulted 7 cases with local complication after surgery and 21 cases with ease of insertion during surgery and important factor in nailing failure is incomplete reduction and using improper screw (11). Ming Hui et al. in 2014 studied 163 patients with A2 fractures that treated with nailing method, after 15 months follow up Hip scoring showed 25% excellent and 56% good results (12).
Small incision and lower bleeding is one of the advantage of nail method. However, to achieve reduction, in some patients a longer incision are needed but the mean length of incision are 6 cm and mean reported bleeding is under 100 cc (12-16). 10 present of patients had clinical symptoms like pain in internal or external side of the femur after surgery that were responsive to different doses of NSAID drugs (13, 15, 17).
Some researches reported that collapse and shortening in first year are lower in nail group in compare with DHS group, but cut out rate was same in both group. On the other hand a lot of meta-analysis reported that during long period some factors like improper placement of the head screw, fracture the end of the nail and need to several next surgeries are the weak points of nail method (18-22).
5. CONCLUSION
This study as well as others tried to compare a new treatment method in compare with an ordinary method. Recorded information of this study during surgery and after follow up period showed a comparative advantage of intramedullary nailing method vs. DHS but despite some advantages like small incision and less bleeding, some components especially during long term are the case of challenge between surgeons. Like all the other studies it should be noted that although the principles of nailing are note more complicated than other methods but in order to more control and improve results there is need for continuous training.
Footnotes
• Author’s contribution: All authors contributed in all phases of preparing this article. Final proof reading was made by first author.
• Conflict of interest: none declared.
REFERENCES
- 1.Bucholz RW. Rockwood and Green's Fractures in Adults: Two Volumes Plus Integrated Content Website. Rockwood, Green, and Wilkins' Fractures): Wolters Kluwer Health; 2012. [Google Scholar]
- 2.Krischak G, Durselen L, Roderer G. [Treatment of peritrochanteric fractures: biomechanical considerations] Unfallchirurg. 2011;114(6):485–90. doi: 10.1007/s00113-011-1976-z. [DOI] [PubMed] [Google Scholar]
- 3.Aktselis I, Kokoroghiannis C, Fragkomichalos E, Koundis G, Deligeorgis A, Daskalakis E, et al. Prospective randomised controlled trial of an intramedullary nail versus a sliding hip screw for intertrochanteric fractures of the femur. Int Orthop. 2014;38(1):155–61. doi: 10.1007/s00264-013-2196-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chua IT, Rajamoney GN, Kwek EB. Cephalomedullary nail versus sliding hip screw for unstable intertrochanteric fractures in elderly patients. J Orthop Surg (Hong Kong) 2013;21(3):308–12. doi: 10.1177/230949901302100309. [DOI] [PubMed] [Google Scholar]
- 5.Shen L, Zhang Y, Shen Y, Cui Z. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res. 2013;99(4):377–83. doi: 10.1016/j.otsr.2012.12.019. [DOI] [PubMed] [Google Scholar]
- 6.Yuan X, Yao Q, Ni J, Peng L, Yu D. [Proximal femoral nail antirotation versus dynamic hip screw for intertrochanteric fracture in elders: a meta-analysis] Zhonghua Yi Xue Za Zhi. 2014;94(11):836–9. [PubMed] [Google Scholar]
- 7.Ma KL, Wang X, Luan FJ, Xu HT, Fang Y, Min J, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: A meta-analysis. Orthop Traumatol Surg Res. 2014;100(8):859–66. doi: 10.1016/j.otsr.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 8.Upadhyay S, Raza HK. Letter to the editor: Proximal femoral locking plate versus dynamic hip screw for unstable intertrochanteric femoral fractures. J Orthop Surg (Hong Kong) 2014;22(1):130–1. doi: 10.1177/230949901402200132. [DOI] [PubMed] [Google Scholar]
- 9.Han FS, Guo FX, Zeng XT, Zhang B, Ping J. Comments on “Anti-rotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies” of L. Shen, Y. Zhang, Y. Shen, Z. Cui published in Orthop. Traumatol Surg Res. 2013;99:377–83. doi: 10.1016/j.otsr.2012.12.019. Orthop Traumatol Surg Res. 2014; 100 (2): 259-60. [DOI] [PubMed] [Google Scholar]
- 10.Dousa P, Bartonicek J, Jehlicka D, Skala-Rosenbaum J. [Osteosynthesis of trochanteric fractures using proximal femoral nails] Acta Chir Orthop Traumatol Cech. 2002;69(1):22–30. [PubMed] [Google Scholar]
- 11.Windolf J, Hollander DA, Hakimi M, Linhart W. Pitfalls and complications in the use of the proximal femoral nail. Langenbecks Arch Surg. 2005;390(1):59–65. doi: 10.1007/s00423-004-0466-y. [DOI] [PubMed] [Google Scholar]
- 12.Li M, Wu L, Liu Y, Wang C. Clinical evaluation of the Asian proximal femur intramedullary nail antirotation system (PFNA-II) for treatment of intertrochanteric fractures. J Orthop Surg Res. 2014;9:112. doi: 10.1186/s13018-014-0112-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Domingo LJ, Cecilia D, Herrera A, Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25(5):298–301. doi: 10.1007/s002640100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gadegone WM, Salphale YS. Proximal femoral nail - an analysis of 100 cases of proximal femoral fractures with an average follow up of 1 year. Int Orthop. 2007;31(3):403–8. doi: 10.1007/s00264-006-0170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Penzkofer J, Mendel T, Bauer C, Brehme K. [Treatment results of pertrochanteric and subtrochanteric femoral fractures: a retrospective comparison of PFN and PFNA] Unfallchirurg. 2009;112(8):699–705. doi: 10.1007/s00113-009-1642-x. [DOI] [PubMed] [Google Scholar]
- 16.Pu JS, Liu L, Wang GL, Fang Y, Yang TF. Results of the proximal femoral nail anti-rotation (PFNA) in elderly Chinese patients. Int Orthop. 2009;33(5):1441–4. doi: 10.1007/s00264-009-0776-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hohendorff B, Meyer P, Menezes D, Meier L, Elke R. [Treatment results and complications after PFN osteosynthesis] Unfallchirurg. 2005;108(11):938. doi: 10.1007/s00113-005-0962-8. 40, 41-6 passim. [DOI] [PubMed] [Google Scholar]
- 18.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010;9:CD000093. doi: 10.1002/14651858.CD000093.pub3. [DOI] [PubMed] [Google Scholar]
- 19.Labronici PJ, da Silva RF, Viana AM, Blunck SS, Franco JS, Neto SR, et al. Is there a difference in the positioning of sliding screws between stable and unstable extracapsular fractures? Rev Bras Ortop. 2015;50(1):30–7. doi: 10.1016/j.rboe.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhong B, Zhang Y, Zhang C, Luo CF. A comparison of proximal femoral locking compression plates with dynamic hip screws in extracapsular femoral fractures. Orthop Traumatol Surg Res. 2014;100(6):663–8. doi: 10.1016/j.otsr.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Evaniew N, Bhandari M. Cochrane in CORR (R): Intramedullary nails for extracapsular hip fractures in adults (review) Clin Orthop Relat Res. 2015;473(3):767–74. doi: 10.1007/s11999-014-4123-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar N, Kataria H, Yadav C, Gadagoli BS, Raj R. Evaluation of proximal femoral locking plate in unstable extracapsular proximal femoral fractures: Surgical technique & mid term follow up results. J Clin Orthop Trauma. 2014;5(3):137–45. doi: 10.1016/j.jcot.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


