Abstract
Common mental disorders are highly prevalent in emergency centre (EC) patients, yet few brief screening tools have been validated for low- and middle-income country (LMIC) ECs. This study explored the psychometric properties of the SRQ-20 screening tool in South African ECs using the Mini Neuropsychiatric Interview (MINI) as the gold standard comparison tool. Patients (n=200) from two ECs in Cape Town, South Africa were interviewed using the SRQ-20 and the MINI. Internal consistency, screening properties and factorial validity were examined. The SRQ-20 was effective in identifying participants with major depression, anxiety disorders or suicidality and displayed good internal consistency. The optimal cutoff scores were 4/5 and 6/7 for men and women respectively. The factor structure differed by gender. The SRQ-20 is a useful tool for EC settings in South Africa and holds promise for task-shifted approaches to decreasing the LMIC burden of mental disorders.
Keywords: Common mental disorder screening, Psychometric properties of the SRQ-20, Low- and middle-income country, Task-shifting, Emergency centre or department
Mental disorders are highly prevalent globally and make a considerable contribution to the burden of disease (World Health Organization 2008). Data from the World Mental Health Surveys reveal that between 12 and 47 % of a country’s population will suffer one or more mental disorders in their lifetime (Kessler et al. 2007), yet a substantial proportion of these people do not receive treatment (Kohn et al. 2004). This discrepancy is even larger in low- and middle-income countries (LMICs) where between 76 and 85 % of people with a serious mental disorder remain untreated, and often undiagnosed (Demyttenaere et al. 2004). It has been advocated that opportunistic screening for mental disorders is a necessary part in addressing the treatment gap (Bower et al. 2006; Patel et al. 2008). With the scarcity of mental health resources in these countries (Kakuma et al. 2011), there is a need for tools to aid general medical staff and lay health workers in detecting mental disorders.
One of the most challenging, time-limited primary care contexts is the emergency centre (EC) which may function as the access point to primary health care for many individuals (Becker et al. 2012; Dale et al. 1995; Hodkinson and Wallis 2009). Furthermore, the EC population is an at-risk group for mental disorders. Data from high-income countries (HICs) show that between 16 and 38 % of patients in ECs are either diagnosed with at least one mental disorder or report symptoms in keeping with poor mental health such as feeling down or concentration difficulties (Cunningham et al. 2009; Saliou et al. 2005; Richmond et al. 2007; Booth et al. 2011). LMIC emergency population data reveal high rates of problem alcohol and drug use (Plüddemann et al. 2004; Cherpitel 2007; Parry et al. 2005). Although data is scarce regarding the prevalence of other mental disorders in this group, a high prevalence rate is expected due to high levels of comorbid disorders commonly found in substance use disorder patients (Grant et al. 2004). Thus there is a need for mental disorder screening in EC settings.
A number of mental health screening tools have been developed for clinical and research use. Some tools, such as the Beck Depression Inventory – Short Form (BDI-SF) (Beck and Steer 1993) focus on specific disorders such as depression. Screening for general psychological distress is the focus of another category of screeners, such as the K10 scale (Kessler et al. 2002), and the 20-item Self Reporting Questionnaire (SRQ-20) (Harding et al. 1980). In certain instances, tools screening for nonspecific psychological distress are preferable to disorder-specific tools as the nonspecific tools will also provide an indicator of the severity of the distress regardless of the actual diagnosis (Kessler et al. 2002). This attribute is beneficial in the primary care and EC setting indicating the level of intervention required, and this is especially important in poorly resourced settings where it may be necessary to allocate the limited resources to the more severely distressed individuals (Patel et al. 2008).
Of the many screening tools available, the SRQ-20 is one of the few specifically designed for the LMIC primary care setting. The SRQ-20 is a 20-item screening tool which was developed by the World Health Organization and it has been widely used in LMICs. The short format and dichotomous (yes/no) answers employed in the SRQ-20 make it a promising tool for the busy primary care setting. A number of studies from the developing world have investigated the psychometric properties of the SRQ-20. For example, investigations in Brazil (Iacoponi and Jair de Jesus 1989), China (Chen et al. 2009), Vietnam (Giang et al. 2006) and India (Patel et al. 2008) show that this tool is suitable for use in LMIC contexts.
Validation data from these LMICs vary widely with regard to internal consistency and factor structure (Ventevogel et al. 2007; Patel et al. 2008; Chen et al. 2009; Scholte et al. 2011a). Moreover, ideal cut-off points for identifying cases of common mental disorder are dependent on the setting. For example, investigators have recommended a cutoff threshold of 7/8 (i.e. scores of 8 and above indicate clinically significant distress) in rural Vietnamese women (Tuan et al. 2004) and, in India, cut-off points between 11/12 or 12/13 in India (Patel et al. 2008). In South Africa, the SRQ-20 has been evaluated predominantly in community settings with one study being conducted in a primary care clinic (Thom et al. 1993; Rumble et al. 1996; Cherian et al. 1998), and in three of the studies a gold standard diagnostic interview was not utilised (Bhagwanjee et al. 1998; Harding et al. 1980; Rumble et al. 1996). The optimal cutoff points reported in these studies, which included male and female participants, were identified as 6/7 and 7/8 (Bhagwanjee et al. 1998; Thomet al. 1993; Rumble et al. 1996).
Thus, at the present time, despite being utilised in primary healthcare settings in South Africa, the psychometric properties of the SRQ-20 have not been fully investigated in the primary healthcare setting, and not at all in South African emergency settings. Therefore this study attempts to address this by exploring the psychometric properties of the SRQ-20 using the Mini Neuropsychiatric Interview version 6.0 (MINI) as the gold standard.
Methods
Study Design
This cross-sectional study was approved by the Human Research Ethics Committee of the University of Cape Town and the Institutional Review Board (IRB) of the University of California Los Angeles.
Study Setting and Population
This study was undertaken in two 24-hour emergency centres (ECs) in two urban, low socioeconomic areas in Cape Town, namely Elsies River and Khayelitsha. Both of these facilities provide services for walk-in patients and refer to a tertiary hospital for specialised services.
A convenience sample of 200 individuals was recruited. Eligible participants included those who were 18 years or older and presented to the EC for treatment of an assault-related injury or injury due to unintentional causes such as falls, burns etc. Individuals were excluded if they had self-inflicted injuries, were medically unstable, if they required referral to a higher level of care, or were unable to provide informed consent (due to being intoxicated, receiving pain medication, etc.).
Study Procedure
During day, night and weekend shifts at the EC from December 2012 to March 2013, patients were approached by field workers after they had been triaged and found to be medically stable. The triage process is a scoring system which enables medical staff to prioritise patients according to the severity of their injury or medical condition. The study staff did not have access to the EC patient log, but approached patients in the waiting areas. If they were amenable to being interviewed, the study was fully described in a private room or treatment area. If the patient agreed to participate, informed consent was taken. Prior to the interview, each participant was informed about the confidentiality of the process. They were assured that participation was voluntary, and that they could withdraw from the study at any time. If the participant was required by the medical personnel, the field workers would temporarily suspend the interview and continue after the medical care had been completed. Participants requiring referral for mental health or social services were provided with referrals. Participants requiring urgent attention were referred directly to the EC medical staff. On completion of the interview, participants were given a R40 (£2.50) supermarket voucher to compensate them for their time.
Measures
In addition to basic demographic information such as age, gender, race, marital status, education and employment, the following measures were included:
Mental Health Screening
The SRQ-20 is a 20-item self-report screening tool developed by the World Health Organization specifically for the LMIC primary healthcare setting. It employs a yes/no answer format and is designed to detect non-specific psychological distress, including suicidality (Beusenberg and Orley 1994). The original format of the tool was utilised.
Mental Disorder Diagnosis
The Mini Neuropsychiatric Interview version 6.0 (MINI) is a validated, structured diagnostic interview which is compatible with the International Classification of Diseases (ICD-10) and the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (Sheehan et al. 1998). The MINI is widely used in clinical and research settings. This measure provided a psychiatric diagnosis for 12 month and lifetime prevalence of a mental disorder. The MINI consists of the following modules: major depressive disorder (current, past and recurrent), suicidality, manic episode (current and past), hypomanic episode (current and past), bipolar I and II disorders (current and past), bipolar disorder not otherwise specified (current and past), panic disorder (current and lifetime), agoraphobia (current), social phobia (current), obsessive-compulsive disorder (current), post-traumatic disorder (current), alcohol abuse and dependence (past 12 months), substance abuse and dependence (past 12 months), psychotic disorders (current and lifetime), mood disorders with psychotic features (current and lifetime), anorexia nervosa (current), bulimia nervosa (current), generalised anxiety disorder (current) and antisocial personality disorder (lifetime).
Sample Size Determination
The sample size determination was conducted on the basis of an estimated mental disorder prevalence of 20 %. The calculations utilised 2-sided tests at alpha=0.05 and beta=0.1 i.e. 90 % power. A sample of 186 produces a two-sided 95 % confidence interval with a width equal to 0.12 when the sample proportion is 0.200. To account for attrition we increased the sample size to 200.
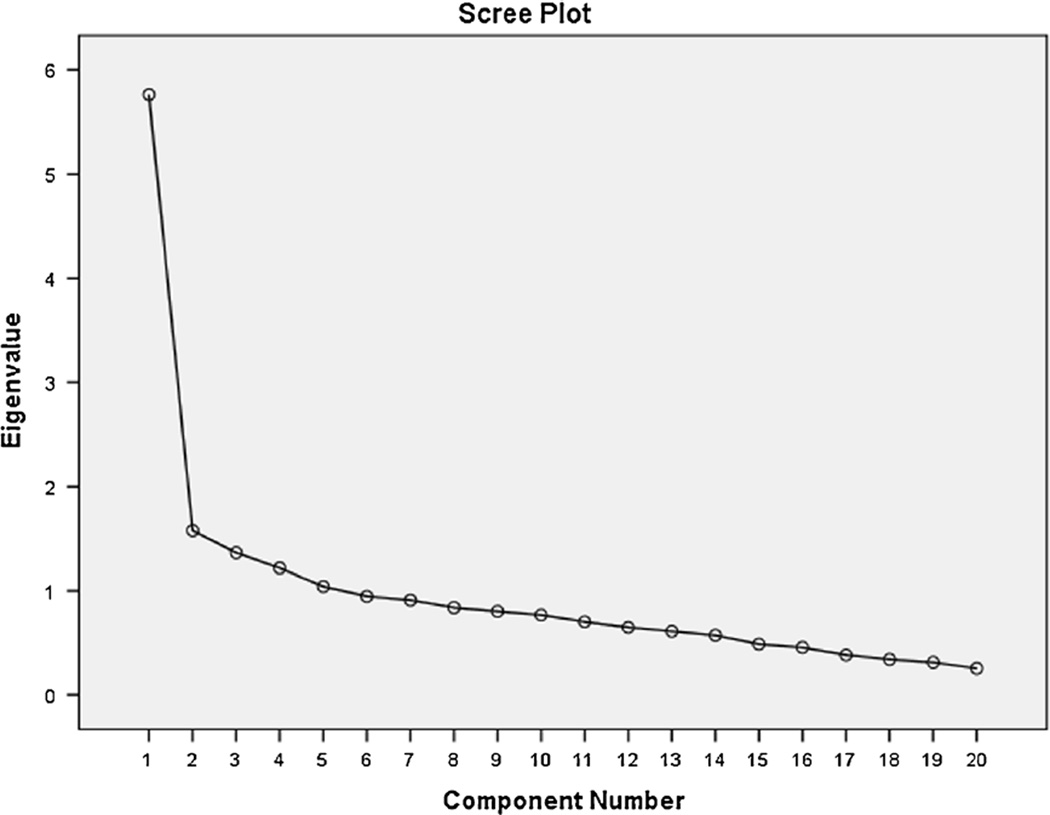
Data Analysis
Data were analysed using IBM SPSS Statistics version 20. Receiver operating characteristic (ROC) analysis was performed to evaluate the screening properties of SRQ-20, using the MINI as the gold standard. The coordinates of this curve were tabulated in SPSS, indicating the sensitivities and specificities at various cutpoints. The area under the curve (AUC) statistic was calculated as a measure of the accuracy of the SRQ-20. (Positive cases on the MINI were those participants with a diagnosis of either current major depression, any current anxiety disorder or current suicidality as measured by the MINI suicidality module or any combination of the three.) Factorial validity was measured by performing a principal component analysis (PCA) with varimax rotation. The Kaiser-Guttman criterion (Guttman 1954; Kaiser 1960) was employed to extract factors with eigenvalues above one. As this approach is known to overestimate the number of factors extracted (Zwick and Velicer 1986), the scree plots were examined to identify the optimal number of factors for extraction (Cattell 1966). Only items with factor loadings above 0.4 were considered for the composition of the factors, in accordance with guidelines based on sample size (Stevens 2002). Cronbach’s alpha coefficient was examined to assess the internal consistency.
Results
Within the sample, the majority of the respondents were men (67 %, n=134), younger than 40 years old (73 %, n=146), and had not completed high school (67 %, n=135). (See Table 1.) Just over half of the sample were single and employed. There were no statistically significant differences between the groups, except in the high school education variable. Significantly more female participants had completed high school (42 % vs 28 %, p=0.04). Of the 200 participants, current depressive, anxiety disorders or suicidality were diagnosed in 54 individuals (27 %) A diagnosis of current major depression was present in 28 individuals (14 %) and current suicidality was diagnosed in 35 participants (18 %). The current anxiety disorders diagnosed in this sample were: panic disorder (n=4, 2 %), limited panic symptoms not meeting criteria for panic disorder (n=4, 2 %), agoraphobia (n=10, 5 %), social phobia (n=2, 1 %) and post-traumatic stress disorder (n=13, 7 %).
Table 1.
Sociodemographic characteristics of the study participants by gender
| Variables | Total sample n=200 (%) | Male n=134 (%) | Female n=66 (%) |
|---|---|---|---|
| Age | |||
| 18–25 | 60 (30 %) | 42 (31 %) | 18 (27 %) |
| 25–40 | 86 (43 %) | 55 (41 %) | 31 (47 %) |
| >40 | 54 (27 %) | 37 (28 %) | 17 (26 %) |
| Relationship status | |||
| Partner | 93 (47 %) | 61 (46 %) | 32 (48 %) |
| Single | 105 (53 %) | 71 (54 %) | 34 (52 %) |
| Completed high school education | |||
| Yes | 65 (33 %) | 37 (28 %) | 28 (42 %) |
| No | 135 (67 %) | 97 (72 %) | 38 (58 %) |
| Employment status | |||
| Employed | 104 (52 %) | 69 (52 %) | 35 (53 %) |
| Unemployed | 96 (48 %) | 65 (48 %) | 31 (47 %) |
General Reliability and Validity of the SRQ-20
Cronbach’s alpha of 0.84 indicated good internal consistency. A balance between sensitivity and specificity was achieved at 4/5 in the male group, 6/7 in the female group and 5/6 for the overall sample. (See Table 2.) Some investigators have recommended a cutoff score of 7/8 (Harpham et al. 2003) which provided a sensitivity of 63 % and a specificity of 88 %.
Table 2.
Sensitivity and specificity of the SRQ-20 at various cut-off scores for detecting common mental disorders diagnosed using the MINI
| Cut-off scores |
Total sample | Male | Female | |||
|---|---|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |
| 1/2 | 96.5 | 44.5 | 96.3 | 45.8 | 96.3 | 41.0 |
| 2/3 | 94.4 | 55.5 | 92.6 | 58.9 | 96.3 | 46.2 |
| 3/4 | 87.0 | 63.0 | 77.8 | 68.2 | 96.3 | 48.7 |
| 4/5 | 85.2 | 69.2 | 74.1 | 74.8 | 96.3 | 53.8 |
| 5/6 | 83.3 | 76.0 | 70.4 | 79.4 | 96.3 | 66.7 |
| 6/7 | 68.5 | 82.9 | 63.0 | 85.0 | 74.1 | 76.9 |
| 7/8 | 63.0 | 88.4 | 59.3 | 89.7 | 66.7 | 84.6 |
| 8/9 | 55.6 | 93.8 | 48.1 | 95.3 | 63.0 | 89.7 |
| 9/10 | 50.0 | 95.2 | 40.7 | 97.2 | 59.3 | 89.7 |
| 10/11 | 46.3 | 95.9 | 37.0 | 98.1 | 55.6 | 89.7 |
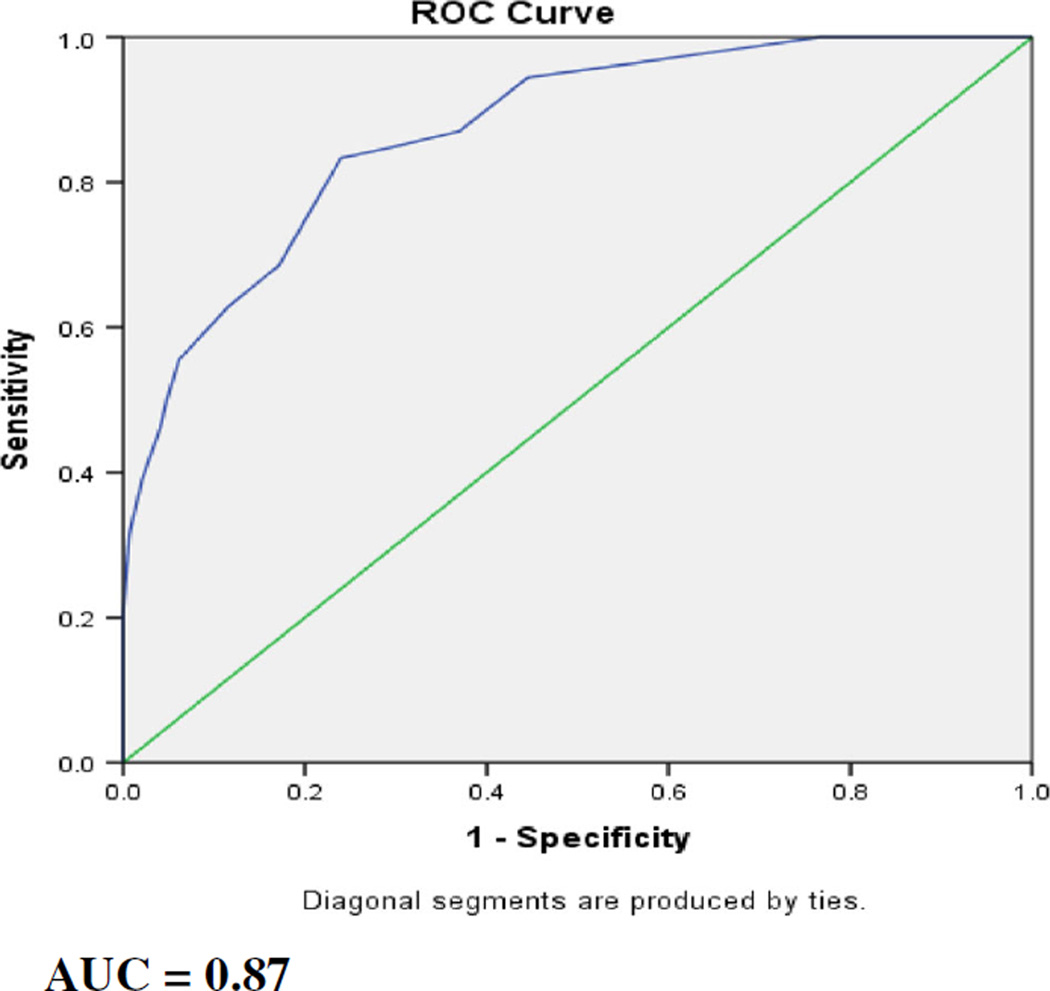
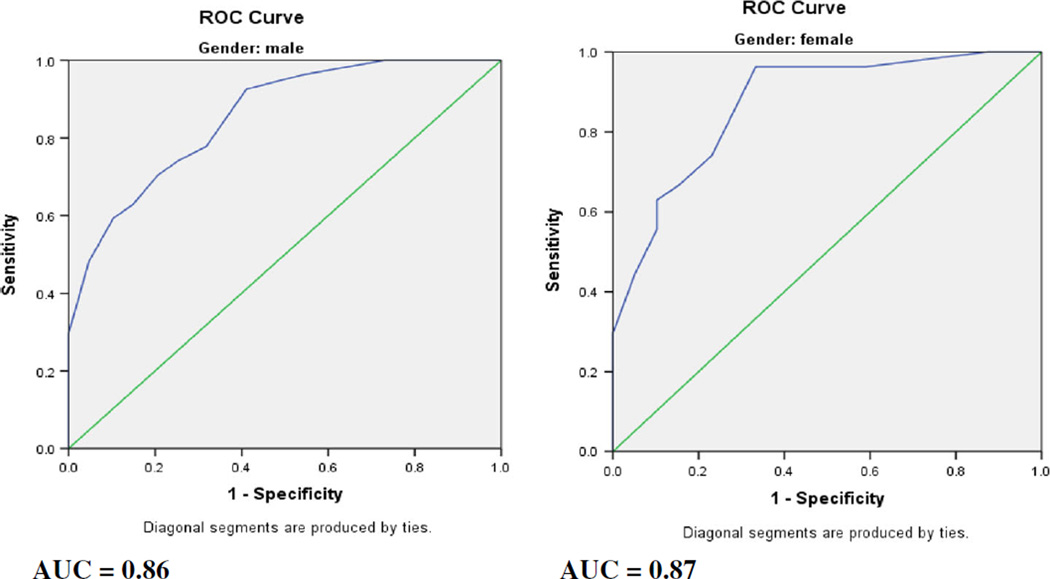
The receiver operator characteristic (ROC) curve analysis for the total sample (see Fig. 1) revealed an area under the curve (AUC) statistic of 0.87 (SE=0.03, 95 % CI 0.82–0.92). For male participants (see Fig. 2), the AUC statistic was 0.86 (SE=0.04, 95 % CI 0.78–0.93) and the AUC statistic for the female participants (see Fig. 2) was 0.87 (SE=0.04, 95 % CI 0.79–0.96).
Fig. 1.
Receiver operating curve for the total sample
Fig. 2.
Receiver operating curves for the male and female participants
Factorial Validity
A principal components analysis (PCA) was conducted on the SRQ-20 data with orthogonal rotation (varimax). The tests of suitability for PCA indicated that this analysis was appropriate. The Kaiser-Meyers-Olkin (KMO) test result of 0.828 confirmed the sampling adequacy for the procedure. Bartlett’s test of sphericity was significant indicating that it was appropriate to perform a PCA.
Using a combination of the Kaiser-Guttman criterion and the scree plot method (see Fig. 3), we decided to extract two factors for the entire sample which explained 37 % of the variance in the sample. We labelled factor 1 ‘depression and anxiety’ and this factor included the following items: unhappiness, lack of enjoyment, nervousness, difficulty thinking, tiredness, easily frightened, poor sleep, difficulty making decisions and crying. The second factor was labelled ‘somatic symptoms’ and included the following items: uncomfortable feelings in the stomach, unable to be useful, poor digestion, work suffering, shaking hands and poor appetite. Three items were excluded (being tired easily, thoughts of ending your life and loss of interest) as they had low factor loadings on both factors. See Table 3 for the factor loadings.
Fig. 3.
Scree plot of components
Table 3.
Factor loadings of the principal component analysis in the total sample
| Items | Factor 1 | Factor 2 |
|---|---|---|
| Headaches | 0.336 | 0.354 |
| Poor appetite | 0.241 | 0.445 |
| Poor sleep | 0.542 | −0.004 |
| Easily frightened | 0.565 | −0.153 |
| Hands shaking | 0.025 | 0.498 |
| Nervousness | 0.589 | 0.024 |
| Poor digestion | −0.023 | 0.579 |
| Difficulty thinking | 0.582 | 0.249 |
| Unhappiness | 0.648 | 0.170 |
| Crying | 0.487 | 0.334 |
| Lack of enjoyment | 0.626 | 0.260 |
| Difficulty making decisions | 0.522 | 0.345 |
| Work suffering | 0.283 | 0.575 |
| Unable to be useful | 0.020 | 0.658 |
| Loss of interest | 0.410 | 0.450 |
| Worthlessness | 0.538 | 0.338 |
| Suicidal thoughts | 0.444 | 0.425 |
| Tiredness | 0.578 | 0.155 |
| Uncomfortable feelings in the stomach | 0.168 | 0.664 |
| Being tired easily | 0.491 | 0.407 |
(Factor loadings >0.4 are in bold text.)
Using the methods explained above, three factors were extracted from the female sample and two factors from the male group, explaining 46 and 40% of the variance, respectively. The KMO test result of 0.812 indicated that the male sample was adequately sized for PCA to be performed, while the KMO result of the female sample was 0.626 indicating that the sample size was less suited to performing a PCA. In both cases the Bartlett’s test of sphericity was significant.
Factor 1 of the male sample was labelled ‘depression and somatic symptoms’ and included: work suffering, uncomfortable feelings in the stomach, difficulty making decisions, unable to be useful, thoughts of ending your life, crying, loss of interest, worthlessness, poor digestion and poor appetite. Factor 2, labelled ‘anxiety and depression’ consisted of headaches, tiredness, easily frightened, lack of enjoyment, unhappiness, being tired easily, nervousness and difficulty thinking.
In the female sample, the three factors extracted were labelled ‘depression and anxiety’, ‘somatic symptoms’ and ‘lethargy’. Factor 1 (‘depression and anxiety’) consisted of worthlessness, difficulty making decisions, unhappiness, difficulty thinking, crying, nervousness, poor sleep and easily frightened. Factor 2 (‘somatic symptoms’) comprised uncomfortable feelings in the stomach, headaches, shaking hands, unable to be useful, poor appetite and poor digestion. Factor 3 (‘lethargy’) included the following items: loss of interest, being tired easily, tiredness, lack of enjoyment and work suffering.
Discussion
This study resulted in a number of important findings. First, the SRQ-20 was shown to be a useful tool for the screening of psychological distress in an LMIC primary healthcare EC setting. Second, the ideal cut-off scores for the SRQ-20 differed by gender. Third, the factor structure of the SRQ-20 reported by males and females differed, with the items relating to somatic and depressive symptoms grouping together in the male sample and separately in the female group.
In keeping with other international studies, our data indicates that the SRQ-20 is a useful tool in the South African primary healthcare EC setting. In the present study, the area under the ROC curve statistic was 0.87. This is consistent with findings from other LMIC primary care settings where the area under the ROC curve ranged from 0.83 in China (Chen et al. 2009) to 0.88 in India (Patel et al. 2008). As found in other studies internationally, the AUC for men and women in our sample were similar, being 0.86 and 0.87 respectively indicating that the SRQ-20 was just as effective in distinguishing between cases and non-cases in both groups (Giang et al. 2006; Ventevogel et al. 2007). The SRQ-20 has not been validated in ECs previously, yet since the results are consistent with findings in primary healthcare settings, the SRQ-20 appears to be suited to the busy EC environment.
In the present study, a balance between sensitivity and specificity was achieved at the higher cutoff score of 6/7 for female participants, as compared to the 4/5 cutoff score in the male group. Studies conducted in Rwanda and Brazil have also reported gender differences in SRQ scores, with higher cutoff scores performing better for female participants than for their male counterparts (Scholte et al. 2011a; Mari and Williams 1986; Gonçalves et al. 2008). However, a few studies have found no difference in optimal cutoff scores in males and females (Giang et al. 2006; Chipimo and Fylkesnes 2010). It has been recommended that optimal cutoff scores be explored in different settings before the screening tools are used in research or clinical practice (Scholte et al. 2011b; Harpham et al. 2003). It has also been suggested that the resource level of the setting be taken into account when deciding on cutoff scores for identifying patients with probable mental disorder, with scores favouring specificity be employed in lower resourced settings (Patel et al. 2008). These findings have implications for research, clinical practice and identification of mental disorders using screening tools.
The investigation of the factor structure of the SRQ-20 has resulted in mixed findings, with little data available exploring gender differences. In our sample, the factor structure of the SRQ-20 differed for males and females. Male participants’ data revealed a grouping of depressive and somatic symptoms in the one factor and anxiety/depression symptoms in the second factor. By contrast, in female participants, depressive and anxiety symptoms were mixed in the first factor, with somatic symptoms in another factor and the last factor comprising symptoms indicative of lethargy. At the present time, no studies have examined the factor structure of the SRQ-20 for males and females separately. Stratton et al. (2013) commented that the factor structure for their male and female participants did indicate that there were differences in participants’ endorsement of various items, but the factors were not further explored (Stratton et al. 2013). Studies conducted in India (Sen 1987) and South Africa (Cherian et al. 1998), with a high proportion of female respondents (76 and 59 % respectively) found a factor with mixed anxiety and depressive symptoms, and another factor containing somatic symptoms. In contrast, a study in a Chinese community (Chen et al. 2009) with 58 % female participation, found three factors corresponding to depressive symptoms, anxiety symptoms and somatic complaints. The wide variety of results emanating from studies exploring the factor structure of the SRQ-20 has led researchers to recommend that the factors found in the SRQ-20 not be used as separate domains or subscales (Scholte et al. 2011a). The investigation of the factor structure of the SRQ-20 may be more useful in exploring cultural differences amongst populations than classifying patients into a disorder-specific category and this could be the focus of future studies.
There are a few limitations of this study. As the sample was relatively small, comprised injured patients only and took place in two ECs in Cape Town, the results may not be generalisable to other EC or healthcare settings. Furthermore, the relatively small number of female participants also limits the generalisablity of the gender differences explored in this study.
Despite these limitations, the results of the present study have implications for addressing the issue of screening for mental disorders in ECs. First, the SRQ-20 has been found to be useful in the busy emergency setting; yet further investigation is required in order to establish optimal cutoff scores for male and female EC patients, as these differed in this study. Second, the SRQ-20 provides easily acquired mental health symptom data which could be vital in advocating for increased mental health resources and common mental disorder screening in South Africa. Third, the SRQ-20 is easy to administer, using simple terminology and a yes/no structure. Given the scarce medical resources in LMICs, especially in the mental health sector, the SRQ-20 allows the vital screening aspect of mental health care to be task-shifted to lay health workers. In fact, healthcare staff in ECs have limited spare time and it may not be feasible to add the duties necessary for screening and brief interventions to the existing workload (Sorsdahl et al. 2013). Thus, the SRQ-20 is a useful tool for our LMIC busy emergency setting and can be used by lay health workers to identify patients in need of further mental health resources. In time-limited primary healthcare and EC settings, this could be a necessary and cost-effective approach when addressing the burden of common mental disorders such as substance use disorders and depression.
Acknowledgments
This study was funded by Phodiso Program, Fogarty International (grant number 1 D43 TW007278). The financial assistance of the National Research Foundation (NRF) towards this research is hereby acknowledged. Opinions expressed and conclusions arrived at, are those of the author and are not necessarily attributed to the NRF.
Footnotes
Informed consent All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Conflicts of interest The authors declare that they have no conflicts of interest.
References
- Beck AT, Steer RA. Beck depression inventory manual. San Antonio: Psychological Corporation; 1993. [Google Scholar]
- Becker J, Dell A, Jenkins L, et al. Reasons why patients with primary health care problems access a secondary hospital emergency centre. South African Medical Journal. 2012;102:800–801. doi: 10.7196/samj.6059. [DOI] [PubMed] [Google Scholar]
- Beusenberg M, Orley J. A user’s guide to the self reporting questionnaire. Geneva: Division of Mental Health, World Health Organization; 1994. [Google Scholar]
- Bhagwanjee A, Parekh A, Paruk Z, et al. Prevalence of minor psychiatric disorders in an adult African rural community in South Africa. Psychological Medicine. 1998;28:1137–1147. doi: 10.1017/s0033291798006965. [DOI] [PubMed] [Google Scholar]
- Booth B, Walton M, Barry K, et al. Substance use, depression, and mental health functioning in patients seeking acute medical care in an inner-city ED. Journal of Behavioral Health Services and Research. 2011;38:358–372. doi: 10.1007/s11414-010-9227-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower P, Gilbody S, Richards D, et al. Collaborative care for depression in primary care: making sense of a complex intervention: systematic review and meta-regression. The British Journal of Psychiatry. 2006;189:484–493. doi: 10.1192/bjp.bp.106.023655. [DOI] [PubMed] [Google Scholar]
- Cattell RB. The scree test for the number of factors. Multivariate Behavioral Research. 1966;1:245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- Chen S, Zhao G, Li L, et al. Psychometric properties of the Chinese version of the self-reporting questionnaire 20 (SRQ-20) in community settings. International Journal of Social Psychiatry. 2009;55:538–547. doi: 10.1177/0020764008095116. [DOI] [PubMed] [Google Scholar]
- Cherian V, Peltzer K, Cherian L. The factor structure of the self report questionnaire (SRQ20) in South Africa. East African Medical Journal. 1998;75:654–656. [PubMed] [Google Scholar]
- Cherpitel CJ. Alcohol and injuries: a review of international emergency room studies since 1995. Drug and Alcohol Review. 2007;26:201–214. doi: 10.1080/09595230601146686. [DOI] [PubMed] [Google Scholar]
- Chipimo PJ, Fylkesnes K. Comparative validity of screening instruments for mental distress in zambia. Clin Practice Epidemiology Mental Health. 2010;6:4–15. doi: 10.2174/1745017901006010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Murray R, Walton MA, et al. Prevalence of past year assault among inner-city emergency department patients. Annals of Emergency Medicine. 2009;53:814.e815–823.e815. doi: 10.1016/j.annemergmed.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale J, Green J, Reid F, et al. Primary care in the accident and emergency department: I. Prospective identification of patients. BMJ (Clin Res Ed) 1995;311:423–426. doi: 10.1136/bmj.311.7002.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Giang KB, Allebeck P, Kullgren G, et al. The Vietnamese version of the self reporting questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: a validation study. International Journal of Social Psychiatry. 2006;52:175–184. doi: 10.1177/0020764006061251. [DOI] [PubMed] [Google Scholar]
- Gonçalves DM, Stein AT, Kapczinski F. Avaliação de desempenho do self-reporting questionnaire Como instrumento de rastreamento psiquiátrico: um estudo comparativo com o structured clinical interview for DSM-IV-TR. Cadernos de Saúde Pública. 2008;24:380–390. doi: 10.1590/s0102-311x2008000200017. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Guttman L. Some necessary conditions for common factor analysis. Psychometrika. 1954;19:149–161. [Google Scholar]
- Harding TW, De Arango V, Baltazar J, et al. Mental disorders in primary health care: a study of their frequency and diagnosis in four developing countries. Psychological Medicine. 1980;10:231–241. doi: 10.1017/s0033291700043993. [DOI] [PubMed] [Google Scholar]
- Harpham T, Reichenheim M, Oser R, et al. Measuring mental health in a cost-effective manner. Health Policy and Planning. 2003;18:344–349. doi: 10.1093/heapol/czg041. [DOI] [PubMed] [Google Scholar]
- Hodkinson PW, Wallis LA. Cross-sectional survey of patients presenting to a South African urban emergency centre. Emergency Medicine Journal. 2009;26:635–640. doi: 10.1136/emj.2008.063362. [DOI] [PubMed] [Google Scholar]
- Iacoponi E, Jair de Jesus M. Reliability and factor structure of the Portuguese version of self-reporting questionnaire. International Journal of Social Psychiatry. 1989;35:213–222. doi: 10.1177/002076408903500301. [DOI] [PubMed] [Google Scholar]
- Kaiser HF. The application of electronic computers to factor analysis. Educational and Psychological Measurement. 1960;20:141–151. [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, et al. Human resources for mental health care: current situation and strategies for action. The Lancet. 2011;378:1654–1663. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- Kessler R, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:168–176. [PMC free article] [PubMed] [Google Scholar]
- Kohn R, Saxena S, Levav I, et al. The treatment gap in mental health care. Bulletin of the World Health Organization. 2004;82:858–866. [PMC free article] [PubMed] [Google Scholar]
- Mari JJ, Williams P. A validity study of a psychiatric screening questionnaire (SRQ-20) in primary care in the city of Sao Paulo. The British Journal of Psychiatry. 1986;148:23–26. doi: 10.1192/bjp.148.1.23. [DOI] [PubMed] [Google Scholar]
- Parry CDH, Pluddemann A, Donson H, et al. Cannabis and other drug use among trauma patients in three South African cities, 1999–2001: original article. 2005;95:429–432. [PubMed] [Google Scholar]
- Patel V, Araya R, Chowdhary N, et al. Detecting common mental disorders in primary care in India: a comparison of five screening questionnaires. Psychological Medicine. 2008;38:221–228. doi: 10.1017/S0033291707002334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plüddemann A, Parry C, Donson H, et al. Alcohol use and trauma in Cape Town, Durban and Port Elizabeth, South Africa: 1999–2001. Injury Control and Safety Promotion. 2004;11:265–267. doi: 10.1080/156609704/233/289599. [DOI] [PubMed] [Google Scholar]
- Richmond TS, Hollander JE, Ackerson TH, et al. Psychiatric disorders in patients presenting to the emergency department for minor injury. Nursing Research. 2007;56:275–282. doi: 10.1097/01.NNR.0000280616.13566.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumble S, Swartz L, Parry C, et al. Prevalence of psychiatric morbidity in the adult population of a rural South African village. Psychological Medicine. 1996;26:997–1007. doi: 10.1017/s0033291700035327. [DOI] [PubMed] [Google Scholar]
- Saliou V, Fichelle A, McLoughlin M, et al. Psychiatric disorders among patients admitted to a French medical emergency service. General Hospital Psychiatry. 2005;27:263–268. doi: 10.1016/j.genhosppsych.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Scholte W, Verduin F, van Lammeren A, et al. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Medical Research Methodology. 2011a;11:116. doi: 10.1186/1471-2288-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholte WF, Verduin F, van Lammeren A, et al. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Medical Research Methodology. 2011b;11:116. doi: 10.1186/1471-2288-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen B. An analysis of the nature of depressive phenomena in primary care using multivariate statistical techniques. Acta Psychiatrica Scandinavica. 1987;76:28–32. doi: 10.1111/j.1600-0447.1987.tb02858.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- Sorsdahl K, Myers B, Ward C, et al. Screening and brief interventions for substance use in emergency departments in the Western Cape province of South Africa: Views of health care professionals. International Journal of Injury Control and Safety Promotion. 2013 doi: 10.1080/17457300.2013.811267. [DOI] [PubMed] [Google Scholar]
- Stevens JP. Applied multivariate statistics for the social sciences. 4th ed. Hillsdale: Erlbaum; 2002. [Google Scholar]
- Stratton KJ, Aggen SH, Richardson LK, et al. Evaluation of the psychometric properties of the self-reporting questionnaire (SRQ-20) in a sample of Vietnamese adults. Comprehensive Psychiatry. 2013;54:398–405. doi: 10.1016/j.comppsych.2012.10.011. [DOI] [PubMed] [Google Scholar]
- Thom R, Zwi R, Reinach S. The prevalence of psychiatric disorders at a primary care clinic in Soweto, Johannesburg. South African Medical Journal. 1993;83:653–655. [PubMed] [Google Scholar]
- Tuan T, Harpham T, Huong NT. Validity and reliability of the self-reporting questionnaire 20 items in Vietnam. Hong Kong Journal of Psychiatry. 2004;14:15–18. [Google Scholar]
- Ventevogel P, De Vries G, Scholte WF, et al. Properties of the Hopkins symptom checklist-25 (HSCL-25) and the self-reporting questionnaire (SRQ-20) as screening instruments used in primary care in Afghanistan. Social Psychiatry and Psychiatric Epidemiology. 2007;42:328–335. doi: 10.1007/s00127-007-0161-8. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The global burden of disease: 2004 update. Geneva: World Health Organization; 2008. [Google Scholar]
- Zwick WR, Velicer WF. Comparion of five rules for determining the number of factors to retain. Psychological Bulletin. 1986;99:432–442. [Google Scholar]