Abstract
Deep vein thrombosis (DVT) and pulmonary embolism (PTE) are known as venous thromboembolism (VTE). DVT occurs when a thrombus (a blood clot) forms in deep veins of the body, usually in the lower extremities. It can cause swelling or leg pain, but sometimes may occur with no symptoms. Awareness of DVT is the best way to prevent the VTE. Patients with trauma are at increased risk of DVT and subsequent PE because of coagulopathy in patients with multiple trauma, DVT prophylaxis is essential but the VTE prophylaxis strategy is controversial for the trauma patients. The risk factors for VTE includes pelvic and lower extremity fractures, and head injury.
Key Words: Management, Deep Vein Thrombosis, DVT, Prophylaxis, Trauma, Patients
Introduction
Trauma is one of the main causes of hospitalization, mortality and morbidity in Iran and the world [1,2]. Trauma patients are at high risk for deep vein thrombosis (DVT) and subsequent pulmonary embolism (PE) which are collectively referred to venous thromboembolism (VTE) [3-5]. VTE is associated with high mortality and morbidity and increased hospitalization duration and costs [6,7]. The incidence of DVT in patients with traumatic injuries is as high as 5-63% [8]. The prophylaxis of DVT is trauma practice in order to prevent the subsequent VTE [8,9]. Previous reports have shown that the incidence of VTE is up to 15% in trauma patients in prophylaxis [10]. Currently, the optimal VTE prophylaxis strategy for trauma patients is unknown. According to current lines of evidence it is believed that long bone fractures, pelvic fractures, traumatic brain injury and prolonged hospitalization are risk factors of VTE in patients with trauma. However the definition of high-risk group for VTE prophylaxis is yet to be defined. The prophylaxis options for VTE consist of mechanical prophylaxis, pharmacological anticoagulation and placing inferior vena cava (IVC).
Modalities available for trauma patient thromboprophylaxis are classified into pharmacologic anticoagulation, mechanical prophylaxis, and inferior vena cava (IVC) filters. Mechanical prophylaxis includes graduated compression stockings (GCSs), pneumatic compression devices (PCDs), and A-V foot pumps. Administration of prophylactic dosages of low-dose heparin (LDH), low molecular weight heparin (LMWH), and factor Xa inhibitors is considered the pharmacologic anticoagulation. Both the Eastern Association for the Surgery of Trauma (EAST) and American College of Clinical Pharmacy (ACCP) guidelines recommend primary use of LMWHs in trauma patients; however there are still controversies regarding the definitive VTE prophylaxis in trauma patients. Large randomized prospective clinical studies would be required to provide level I evidence to define the optimal VTE prophylaxis in trauma patients. An autopsy study found 20% death of PE [9,10] and 65% of fatally injured patients by DVT [7,8].The cost of economic burden of PE and DVT is high, due not only to the initial hospitalization [11]. Therefore, it will increase the likelihood of progression to death, which preventable and it shows the need for prophylaxis [12-14].
The conditions of traumatic injuries management are more different and harder than prescription of prophylaxis DVT and other medical groups. Because it will make the active and potential bleeding of these victims, such as intracranial hemorrhage, spinal fractures, pelvic fractures associated with hematoma, bleeding internal organs caused by trauma, and prescription of drugs that can aggravate bleeding.
Process Methods
This is a narrative review being performed by searching the main databases including PubMed (National Library of Medicine) and Scopus with keywords of DVT, PE, VTE prophylaxis and trauma from 1975 through 2015. Out of 1109 articles recognized, prospective studies were selected and reviewed. Data collected and a consensus was received for the opinion of recommendations.
Risk Factors and Pathophysiology
Many factors can increase the risk of developing DVT. Several studies showed the risk of DVT after trauma [9]. The risk factors for DVT includes age over 40 years, cancer, inflammatory bowel disease, Cancer History, Rheumatic Diseases, Obesity, Heart failure, Injury or surgery such as Hip Fracture, Femoral or Double leg fracture, Spinal Cord Injury, TBI, and GCS<8. Lower extremity fracture, head injury and pelvic fracture have been considered risk factors for VTE [15]. Acute spinal cord injury patients are at a considerable risk for developing DVT [16-18]. Spinella et al., [19] found that in trauma patients who transfused by 5 or more unit of RBC, DVT was increased with the transfusion of old RBC’s. Despite these numerous risk factors associated with DVT, the high risk group is unclear [20].
Mechanical Thromboprophylaxis
Mechanical method reduce the pooling of blood in the deep venous system that is increases the blood flow of venous and return the venous to the heart. The method also prevents microvascular damage of the veins caused by stretching during venous pooling. This method includes Intermittent pneumatic compression (IPC) sleeves and Anti-embolism stockings (AES). The advantage of the method is the absence of the effect on coagulation. Therefore, there is no increased risk of bleeding. The disadvantages include poor compliance, cost, exacerbation of arterial insufficiency in patients with peripheral arterial disease and lower efficacy than pharmacological method.
Pharmacologic thromboprophylaxis
This method depends on producing a low level of anticoagulation. Pharmacological method includes Low dose unfractionated heparin (UFH), Low dose low molecular weight heparin (LMWH) and Oral direct thrombin or Xa inhibitors. The advantages of this method are efficacy and compliance that based on the dose given to the patients. The disadvantages are bleeding due to the effect of coagulation and drug reactions. Drug reactions with heparin are rare but includes of allergy to heparin, skin necrosis and Heparin Induced Thrombocytopenia and Thrombosis (HITT). Drug reactions are less common by oral direct thrombin and Xa inhibitors. To prevent the thrombin in hospitalized patients, warfarin should not be used.
How is mechanical and pharmacologic prophylaxis used in prevention?
The risk of VTE can be reduced at the time of surgery with administration of appropriate prophylaxis regimen. Mechanical methods are usually used in combination with other methods. The types of mechanical prophylaxis include Stockings which are more effective in preventing DVT in the calf than in legs; of lower extremities such as elevating the foot, active and passive ankle motion that increasing blood flow through the femoral vein. External pneumatic devices are other mechanical prophylaxis of DVT which could be used in combination with other methods. In high risk patients pneumatic compression devices are the most effective route of DVT prophylaxis. These devices are expensive and not available in all the centers. Inferior vena cava (IVC) filters are among the mechanical prophylaxis of VTE devices which are used in those with extensive DVT and high risk of PE and have also contraindication of anticoagulation therapy. Application of pharmacological prophylaxis is associated with increased risk of bleeding. The most common anticoagulant is aspirin and warfarin.
Aspirin: it is easy to prescribe and use, costs little, has few complications of bleeding, and there is no need to monitoring. Therefore, it is not been proven to be more effective than other methods and may not be advisable for all patients.
Warfarin: Also called Coumadin and is most commonly used for the hip and knee of patient’s replacement. It will interfere with vitamin K metabolism in liver to clot formation of DVT. 4 to 5 days need to gain maximum effectiveness because it takes at least 36 hours to start working. Warfarin normally use at low doses because higher doses can cause bleeding. Also, it can cause fatal damage.
Comparative effectiveness of mechanical and pharmaceutical prophylaxis
There are two non-invasive mechanical methods of DVT prophylaxis that includes Intermittent Pneumatic Compression (IPC) and Anti-embolic stockings (AES). These two methods are both proven and effective when used alone or used in combination with pharmacologic prophylaxis for higher risk patients. Mechanical methods have an advantage and are not with the risk of bleeding. Both IPC and AES work to derogate the risk factor associated with VTE, unlike pharmacologic prophylaxis. These mechanical methods of VTE prophylaxis has no risk of bleeding when used as a monotherapy and can be used as an adjunct to pharmacological prophylaxis to increase the effectiveness in high risk patients.
Internal Bleeding
DVT is a blood clot which develops in the deep veins in one or both legs. It can be dangerous because the clot may become large and deep and go through blood vessels and lodge in the lungs. Anticoagulants such as heparin, Low Molecular Weight Heparin (LMWH), or coumadin have been the main treatment for DVT. IV thromboembolic is no longer recommended for treating DVT because it will increase the chance of bleeding. Study of Joseph et al., [21] showed no significant correlation between early anticoagulation and development of bleeding complications. It says using of early enoxaparin anticoagulation maybe a safe option in trauma patients.
Spinal Injuries
Patients with spinal cord injury are at the high risk of VTE. Using mechanical prophylaxis recommended when anticoagulant prophylaxis is contraindicated but no evidence exist to support the use of mechanical prophylaxis as a single prophylaxis method [22,23]. The risk of VTE in spinal cord patients will increase during their rehabilitation phase and should continue the thromboembolic prophylaxis [24].
Patients with spinal cord injuries are at a high risk of gastrointestinal hemorrhage or bleeding even during periods of rehabilitation [25,26]. All acute spinal cord injured patients and patients with rehabilitations may benefit from receiving chemical prophylaxis for ulceration [27]. Prevention could be the basis in the management of this problem.
Pelvis Fractures
In a trauma patients who have sustained pelvic or acetabular fractures, proximal vein thrombosis frequently occurs. For these patients, LMWH is recommended as a mean of thromboembolic prophylaxis after hemostasis [28]. When LMWH is contraindicated, mechanical thromboembolic prophylaxis is recommended [22,23,29]
Hip Fractures
The complications of thromboembolic events remain an important cause of mortality and morbidity associated with hip fractures.
Patients with hip fractures are at very high risk of VTE. In a study of Marsland et al., [30] aspirin is reduces the risk of VTE but does not provide protection compared with other pharmacological prophylaxis. Therefore, it is not recommended. Warfarin, LMWH, and Fondaparinx reduce the risk of DVT. The study showed that chemical VTE prophylaxis should be used for all patients with hip fractures.
Studies showed that without prophylaxis the rate of DVT in patients with hip fracture ranges from 46%-75% [31-34]. Therefore, all patients with hip fracture need prophylaxis against VTE. Another studies showed that the risk of VTE in hip fracture patients starts at the time of surgery [35,36]. The study of Niikura et al., [37] evaluates the rate of VTE after complex lower limb fracture surgery without pharmacological prophylaxis. The study showed that VTE was high in patients undergoing this surgery. Also, study of Chu et al., [38] showed that major trauma patients have an approximate six fold increased risk of developing VTE during admission compared with minor trauma patients. This study supports the use of prophylaxis to treat minor trauma patients.
Traumatic Brain Injury
TBI are at increased risk of DVT [39] and it is because of hypercoagulability which is happen in TBI patients from a variety of mechanisms such as tissue factor [40]. All TBI patients should receive Intermittent Pneumatic Compression Devises (IPC) at the time of admission to hospital [41]. Also a head CT should be obtained to find about the lack of progression of further bleeding. The CT scan should be performed at 24 hours of intervals. Chemical thromboprophylaxis should be started in 24-48 hours after head CT and found about progression of bleeding [42-44].
Prevention of Venous Thromboembolism
Although mechanical methods have been shown to reduce the risk of DVT, they have been studied less than pharmacological treatment methods [45]. Mechanical methods of prophylaxis include IPC and AES and Venous foot pump. Mechanical prophylaxis should be used in patients who are in high risk of bleeding or as an adjunct with pharmacological methods.Comparison stocking have been shown to reduce DVT, but their use is associated with an increase in skin complications [46].
The DVT management includes PE prevention. Study of Clark-pearson suggests that IPC is as an option for VTE prophylaxis in patients undergoing gynecologic surgery. Clinicians who are treating women with more than one risk factor should use pharmacologic rather than mechanical methods to prevent VTE [47].
DVT and PE are clinically important complications of strock. The study of Mazzone et al., [48] showed that mechanical prophylaxis appears safe in patients with strock.
Current Status
Existing guidelines of trauma usually cannot speak in detail about the harsh conditions of traumatic injuries because of trauma conditions elaboration and there is no evidence of levels I and II in the field and there are no other evidences. In a guideline of American College of Chest physician (ACCP) recommends the use of LMWH for major trauma patients. [49] An acceptable recommendation is using LMWH and the optimal use of the mechanical prophylaxis. ACCP also recommends thromboprophylaxis for major trauma patients with impaired mobility until they discharged [49]. Using of Kaprini disk should also be reviewed for the trauma victims [39].The Eastern Association for the Surgery of Trauma (EAST) guideline also shows several important points about patient’s management with bleeding and cerebral hemorrhage [50]. EAST guideline has no level I recommendation for LMWH. According to Level II, LMWH can use for the pelvic fractures, lower extremity fractures and spinal cord injury. According to level III, patients with ISS> 9 should receive LMWH [51]. At the start of DVT prophylaxis for patients with brain problems levels of cc reflects to start the DVT prophylaxis treatment. The onset and rate of treatment is only the evidence of level III that indicating the safety of starting mechanical prophylaxis from the beginning of hospitalization and pharmacological prophylaxis starting from 24-48 hours after the stability of brain injury.
Recommendations
All patients should receive mechanical prophylaxis or pharmacologic prophylaxis
Risk of bleeding and thromboembolism should be assessed in all patients at admission.
For the majority of inpatients who do not have contraindications, pharmacologic prophylaxis has been the default mode of prophylaxis [52,53]
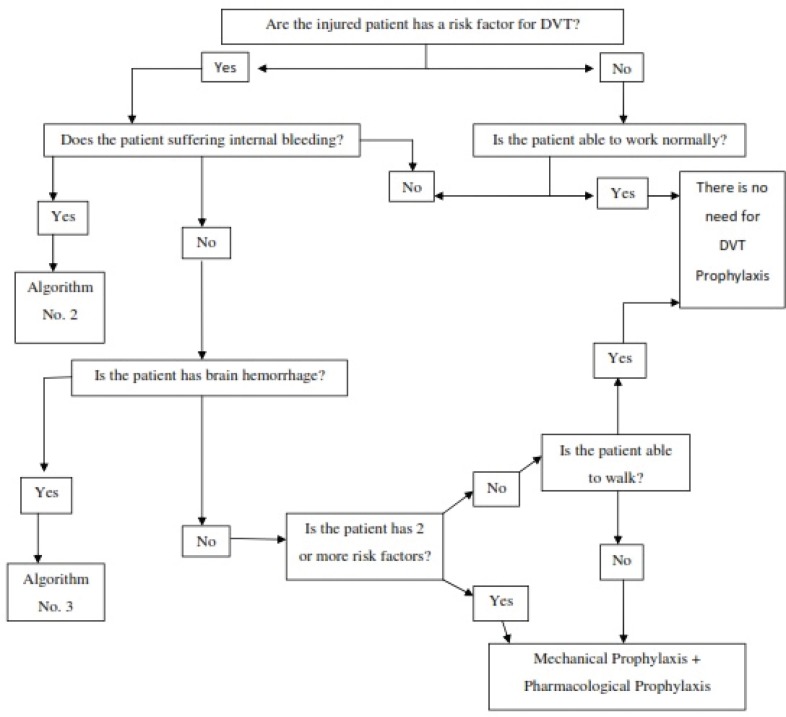
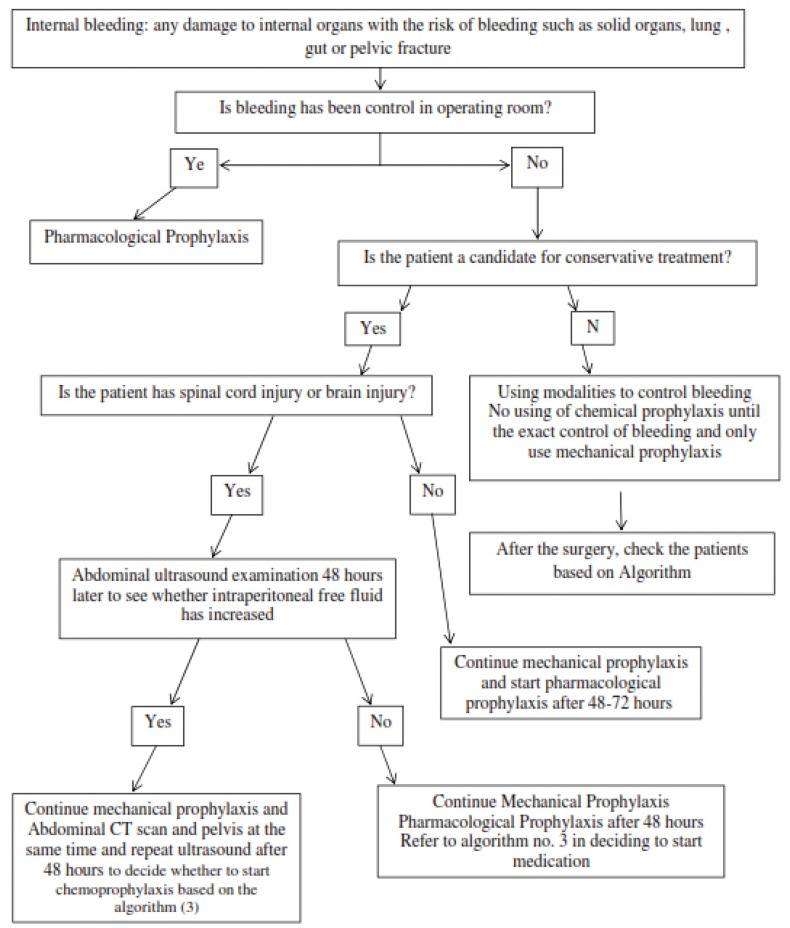
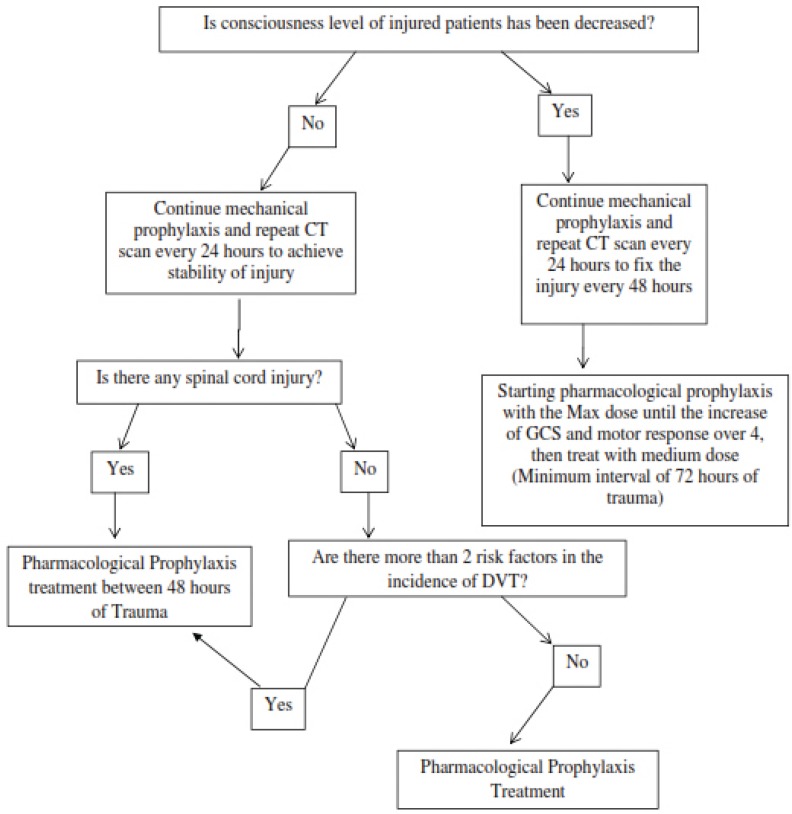
Internal bleeding means any damage to internal organs with the risk of bleeding such as solid organs, lung, gut or pelvic fracture. Algorithm 1-3 shows the decision for starting DVT prophylaxis in trauma patients (Figure 1, 2 and 3).
Fig. 1.
Algorithm 1: Decision for Starting DVT Prophylaxis in Trauma Patients
Fig. 2.
Algorithm 2: Starting DVT prophylaxis in patients with damage to internal organs or internal bleeding and pelvic fractures
Fig. 3.
Algorithm 3: Starting prophylaxis in trauma patients with cerebral hemorrhage
Conclusion
The detection of both PE and DVT are difficult. Therefore, it is good to concentrate on preventing their development by using mechanical or pharmacological methods. Combining vascular compression stockings with low-dose heparin is an effective strategy for patients at high or very high risk of venous thromboembolism [54].
Conflict of Interest: None declared.
References
- 1.Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87(4):246–a. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Modarres SR, Shokrollahi MH, Yaserian M, Rahimi M, Amani N, Manouchehri AA. Epidemiological Characteristics of Fatal Traumatic Accidents in Babol, Iran: A Hospital-Based Survey. Bull Emerg Trauma. 2014;2(4):146–150. [PMC free article] [PubMed] [Google Scholar]
- 3.In: U.S. Department of Health and Human Services. The surgeon general’s call to action to prevent deep vein thrombosis and pulmonary embolism. 2008. Available from: http://www.ncbi.nlm.nih.gov/books/NBK44178/pdf/TOC.pdf. [PubMed]
- 4.Prevention of venous thrombosis, pulmonary embolism. NIH Consensus Development. JAMA. 1986;256(6):744–9. [PubMed] [Google Scholar]
- 5.Shackford SR, Moser KM. Deep venous thrombosis and pulmonary embolism in trauma patients. Journal of Intensive Care Medicine. 1988;3(2):87–98. [Google Scholar]
- 6.Sevitt S. Fatal road accidents. Injuries, complications, and causes of death in 250 subjects. Br J Surg. 1968;55(7):481–505. doi: 10.1002/bjs.1800550702. [DOI] [PubMed] [Google Scholar]
- 7.Spyropoulos AC, Lin J. Direct medical costs of venous thromboembolism and subsequent hospital readmission rates: an administrative claims analysis from 30 managed care organizations. J Manag Care Pharm. 2007;13(6):475–86. doi: 10.18553/jmcp.2007.13.6.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piotrowski JJ, Alexander JJ, Brandt CP, McHenry CR, Yuhas JP, Jacobs D. Is deep vein thrombosis surveillance warranted in high-risk trauma patients? Am J Surg. 1996;172(2):210–3. doi: 10.1016/s0002-9610(96)00154-7. [DOI] [PubMed] [Google Scholar]
- 9.Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. New England Journal of Medicine. 1994;331(24):1601–6. doi: 10.1056/NEJM199412153312401. [DOI] [PubMed] [Google Scholar]
- 10.Hill SL, Berry RE, Ruiz AJ. Deep venous thrombosis in the trauma patient. Am Surg. 1994;60(6):405–8. [PubMed] [Google Scholar]
- 11.Sevitt S, Gallagher N. Venous thrombosis and pulmonary embolism. A clinico-pathological study in injured and burned patients. Br J Surg. 1961;48:475–89. doi: 10.1002/bjs.18004821103. [DOI] [PubMed] [Google Scholar]
- 12.Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, et al. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis: American College of Chest Physicians evidence-based clinical practice guidelines. CHEST Journal. 2012;141(2_suppl):e227S–e77S. doi: 10.1378/chest.11-2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laporte S, Mismetti P, Decousus H, Uresandi F, Otero R, Lobo JL, et al. Clinical predictors for fatal pulmonary embolism in 15,520 patients with venous thromboembolism: findings from the Registro Informatizado de la Enfermedad TromboEmbolica venosa (RIETE) Registry. Circulation. 2008;117(13):1711–6. doi: 10.1161/CIRCULATIONAHA.107.726232. [DOI] [PubMed] [Google Scholar]
- 14.Pasquale M, Fabian TC. Practice management guidelines for trauma from the Eastern Association for the Surgery of Trauma. Journal of Trauma and Acute Care Surgery. 1998;44(6):941–56. doi: 10.1097/00005373-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Fakhry S, Michetti C. Bleeding and coagulation complications. Trauma. 2004:1251–70. [Google Scholar]
- 16.Fujii Y, Mammen EF, Farag A, Muz J, Salciccioli GG, Weingarden ST. Thrombosis in spinal cord injury. Thrombosis research. 1992;68(4):357–68. doi: 10.1016/0049-3848(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 17.Velmahos GC, Kern J, Chan LS, Oder D, Murray JA, Shekelle P. Prevention of venous thromboembolism after injury: an evidence-based report--part II: analysis of risk factors and evaluation of the role of vena caval filters. J Trauma. 2000;49(1):140–4. doi: 10.1097/00005373-200007000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Myllynen P, Kammonen M, Rokkanen P, Bostman O, Lalla M, Laasonen E. Deep venous thrombosis and pulmonary embolism in patients with acute spinal cord injury: a comparison with nonparalyzed patients immobilized due to spinal fractures. J Trauma. 1985;25(6):541–3. doi: 10.1097/00005373-198506000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Spinella PC, Carroll CL, Staff I, Gross R, Mc Quay J, Keibel L, et al. Duration of red blood cell storage is associated with increased incidence of deep vein thrombosis and in hospital mortality in patients with traumatic injuries. Crit Care. 2009;13(5):R151. doi: 10.1186/cc8050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gearhart MM, Luchette FA, Proctor MC, Lutomski DM, Witsken C, James L, et al. The risk assessment profile score identifies trauma patients at risk for deep vein thrombosis. Surgery. 2000;128(4):631–40. doi: 10.1067/msy.2000.108224. [DOI] [PubMed] [Google Scholar]
- 21.Joseph B, Pandit V, Harrison C, Lubin D, Kulvatunyou N, Zangbar B, et al. Early thromboembolic prophylaxis in patients with blunt solid abdominal organ injuries undergoing nonoperative management: is it safe? Am J Surg. 2015;209(1):194–8. doi: 10.1016/j.amjsurg.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 Suppl):338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 23.Rogers FB, Cipolle MD, Velmahos G, Rozycki G, Luchette FA. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53(1):142–64. doi: 10.1097/00005373-200207000-00032. [DOI] [PubMed] [Google Scholar]
- 24.Prevention of venous thromboembolism in the acute treatment phase after spinal cord injury: a randomized, multicenter trial comparing low-dose heparin plus intermittent pneumatic compression with enoxaparin. J Trauma. 2003;54(6):1116–24. doi: 10.1097/01.TA.0000066385.10596.71. discussion 25-6. [DOI] [PubMed] [Google Scholar]
- 25.Charney KJ, Juler GL, Comarr AE. General surgery problems in patients with spinal cord injuries. Arch Surg. 1975;110(9):1083–8. doi: 10.1001/archsurg.1975.01360150027005. [DOI] [PubMed] [Google Scholar]
- 26.Tanaka M, Uchiyama M, Kitano M. Gastroduodenal disease in chronic spinal cord injuries. An endoscopic study. Arch Surg. 1979;114(2):185–7. doi: 10.1001/archsurg.1979.01370260075012. [DOI] [PubMed] [Google Scholar]
- 27.Anwar F, Al-Khayer A, El-Mahrouki H, Purcell M. Gastrointestinal bleeding in spinal injuries patient: Is prophylaxis essential? Alcohol. 2013;5:26.3. [Google Scholar]
- 28.Ginzburg E, Cohn SM, Lopez J, Jackowski J, Brown M, Hameed SM. Randomized clinical trial of intermittent pneumatic compression and low molecular weight heparin in trauma. Br J Surg. 2003;90(11):1338–44. doi: 10.1002/bjs.4309. [DOI] [PubMed] [Google Scholar]
- 29.Eastman AB. Venous thromboembolism prophylaxis in trauma patients. Techniques in Orthopaedics. 2004;19(4):293–9. [Google Scholar]
- 30.Marsland D, Mears SC, Kates SL. Venous thromboembolic prophylaxis for hip fractures. Osteoporos Int. 2010;21(Suppl 4):S593–604. doi: 10.1007/s00198-010-1403-2. [DOI] [PubMed] [Google Scholar]
- 31.Agnelli G, Cosmi B, Di Filippo P, Ranucci V, Veschi F, Longetti M, et al. A randomised, double-blind, placebo-controlled trial of dermatan sulphate for prevention of deep vein thrombosis in hip fracture. Thromb Haemost. 1992;67(2):203–8. [PubMed] [Google Scholar]
- 32.Lowe GD, Campbell AF, Meek DR, Forbes CD, Prentice CR. Subcutaneous ancrod in prevention of deep-vein thrombosis after operation for fractured neck of femur. Lancet. 1978;2(8092 Pt 1):698–700. doi: 10.1016/s0140-6736(78)92701-0. [DOI] [PubMed] [Google Scholar]
- 33.Powers PJ, Gent M, Jay RM, Julian DH, Turpie AG, Levine M, et al. A randomized trial of less intense postoperative warfarin or aspirin therapy in the prevention of venous thromboembolism after surgery for fractured hip. Arch Intern Med. 1989;149(4):771–4. [PubMed] [Google Scholar]
- 34.Rogers PH, Walsh PN, Marder VJ, Bosak GC, Lachman JW, Ritchie WG, et al. Controlled trial of low-dose heparin and sulfinpyrazone to prevent venous thromboembolism after operation on the hip. J Bone Joint Surg Am. 1978;60(6):758–62. [PubMed] [Google Scholar]
- 35.Hefley FG Jr, Nelson CL, Puskarich-May CL. Effect of delayed admission to the hospital on the preoperative prevalence of deep-vein thrombosis associated with fractures about the hip. J Bone Joint Surg Am. 1996;78(4):581–3. doi: 10.2106/00004623-199604000-00012. [DOI] [PubMed] [Google Scholar]
- 36.Zahn HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein thrombosis in patients with femoral neck fractures and delayed operation. Injury. 1999;30(9):605–7. doi: 10.1016/s0020-1383(99)00163-1. [DOI] [PubMed] [Google Scholar]
- 37.Niikura T, Sakai Y, Lee SY, Iwakura T, Kuroda R, Kurosaka M. Rate of venous thromboembolism after complex lower-limb fracture surgery without pharmacological prophylaxis. J Orthop Surg (Hong Kong) 2015;23(1):37–40. doi: 10.1177/230949901502300109. [DOI] [PubMed] [Google Scholar]
- 38.Chu CC, Haga H. Venous thromboembolism associated with lower limb fractures after trauma: dilemma and management. J Orthop Sci. 2015;20(2):364–72. doi: 10.1007/s00776-014-0690-4. [DOI] [PubMed] [Google Scholar]
- 39.Praeger AJ, Westbrook AJ, Nichol AD, Wijemunige R, Davies AR, Lyon SM, et al. Deep vein thrombosis and pulmonary embolus in patients with traumatic brain injury: a prospective observational study. Crit Care Resusc. 2012;14(1):10–3 3. [PubMed] [Google Scholar]
- 40.Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70(6):1334–45. doi: 10.1227/NEU.0b013e31824d179b. [DOI] [PubMed] [Google Scholar]
- 41.DeMuro JP, Hanna AF. Prophylaxis of Deep Venous Thrombosis in Trauma Patients: A Review. J Blood Disorders Transf. 2013;4(151):2. [Google Scholar]
- 42.Phelan HA, Wolf SE, Norwood SH, Aldy K, Brakenridge SC, Eastman AL, et al. A randomized, double-blinded, placebo-controlled pilot trial of anticoagulation in low-risk traumatic brain injury: The Delayed Versus Early Enoxaparin Prophylaxis I (DEEP I) study. J Trauma Acute Care Surg. 2012;73(6):1434–41. doi: 10.1097/TA.0b013e31825ac49e. [DOI] [PubMed] [Google Scholar]
- 43.Saadeh Y, Gohil K, Bill C, Smith C, Morrison C, Mosher B, et al. Chemical venous thromboembolic prophylaxis is safe and effective for patients with traumatic brain injury when started 24 hours after the absence of hemorrhage progression on head CT. J Trauma Acute Care Surg. 2012;73(2):426–30. doi: 10.1097/TA.0b013e31825a758b. [DOI] [PubMed] [Google Scholar]
- 44.Kim J, Gearhart MM, Zurick A, Zuccarello M, James L, Luchette FA. Preliminary report on the safety of heparin for deep venous thrombosis prophylaxis after severe head injury. J Trauma. 2002;53(1):38–42. doi: 10.1097/00005373-200207000-00008. discussion 3. [DOI] [PubMed] [Google Scholar]
- 45.Christie S, Thibault-Halman G, Casha S. Acute pharmacological DVT prophylaxis after spinal cord injury. J Neurotrauma. 2011;28(8):1509–14. doi: 10.1089/neu.2009.1155-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e278S–325S. doi: 10.1378/chest.11-2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clarke-Pearson DL, Dodge RK, Synan I, McClelland RC, Maxwell GL. Venous thromboembolism prophylaxis: patients at high risk to fail intermittent pneumatic compression. Obstet Gynecol. 2003;101(1):157–63. doi: 10.1016/s0029-7844(02)02444-4. [DOI] [PubMed] [Google Scholar]
- 48.Mazzone C, Chiodo GF, Sandercock P, Miccio M, Salvi R. Physical methods for preventing deep vein thrombosis in stroke. Cochrane Database Syst Rev. 2004;(4):CD001922. doi: 10.1002/14651858.CD001922.pub2. [DOI] [PubMed] [Google Scholar]
- 49.Hirsh J, Guyatt G, Lewis SZ. Reflecting on eight editions of the American College of Chest Physicians antithrombotic guidelines. Chest. 2008;133(6):1293–5. doi: 10.1378/chest.08-0782. [DOI] [PubMed] [Google Scholar]
- 50.Rogers FB, Cipolle MD, Velmahos G, Rozycki G, Luchette FA. Practice management guidelines for the prevention of venous thromboembolism in trauma patients: the EAST practice management guidelines work group. J Trauma. 2002;53(1):142–64. doi: 10.1097/00005373-200207000-00032. [DOI] [PubMed] [Google Scholar]
- 51.Cushman JG, Agarwal N, Fabian TC, Garcia V, Nagy KK, Pasquale MD, et al. Practice management guidelines for the management of mild traumatic brain injury: the EAST practice management guidelines work group. J Trauma. 2001;51(5):1016–26. doi: 10.1097/00005373-200111000-00034. [DOI] [PubMed] [Google Scholar]
- 52.Kakkar AK, Cimminiello C, Goldhaber SZ, Parakh R, Wang C, Bergmann JF. Low-molecular-weight heparin and mortality in acutely ill medical patients. N Engl J Med. 2011;365(26):2463–72. doi: 10.1056/NEJMoa1111288. [DOI] [PubMed] [Google Scholar]
- 53.Lederle FA, Zylla D, MacDonald R, Wilt TJ. Venous thromboembolism prophylaxis in hospitalized medical patients and those with stroke: a background review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2011;155(9):602–15. doi: 10.7326/0003-4819-155-9-201111010-00008. [DOI] [PubMed] [Google Scholar]
- 54.Goldhaber SZ, Fanikos J. Prevention of deep vein thrombosis and pulmonary embolism. Circulation. 2004;110(16):e445–e7. doi: 10.1161/01.CIR.0000145141.70264.C5. [DOI] [PubMed] [Google Scholar]