Abstract
Adolescent depression is a growing public health concern with an increased risk of negative health outcomes, including suicide. The use of antidepressants and psychotherapy has not halted its increasing prevalence, and there is a critical need for effective prevention and treatment. We reviewed the neuroscience of adolescent depression, with a focus on the neurocircuitry of sustained threat and summarised contextual factors that have an impact on brain development and the pathophysiology of depression. We also reviewed novel treatment models.
Conclusion
Attention to the relevant neurocircuitry and contextual factors implicated in adolescent depression is necessary to advance prevention and treatment development.
Keywords: Adolescent depression, Contextual factors, Neuroscience, Review, Sustained threat
Abbreviations
- ADHD
Attention deficit hyperactivity disorder
- ASD
Autism spectrum disorder
- CBT
Cognitive behavioural therapy
- DSM
The diagnostic and statistical manual of mental disorders
- fMRI
Functional magnetic resonance imaging
- MDD
Major depressive disorder
- RSFC
Resting‐state functional connectivity
- sgACC
Subgenual anterior cingulate cortex
- SSRI
Selective serotonin reuptake inhibitor
- TARA
Training for awareness resilience and action
Key notes.
Adolescent depression is a growing public health concern with an increased risk of negative health outcomes, including suicide.
We reviewed the neuroscience of adolescent depression, summarised contextual factors that have an impact on brain development and the pathophysiology of depression, and reviewed novel treatment models.
Our conclusion is that attention to the relevant neurocircuitry and contextual factors implicated in adolescent depression is necessary to advance prevention and treatment development.
Introduction
Adolescent major depressive disorder (MDD) is an important public health concern because of its prevalence, early onset and impact on the individual, family and community 1. In Sweden, during the period between 1997 and 2007, the number of teenagers between 16 and 19 years old who received in‐patient medical care for anxiety and depression increased by 400% 2. During the same time period, the prevalence of suicide attempts by young women aged 16–24 years increased by 60% in Sweden 2. Furthermore, in the USA, suicide was the second leading cause of death in children aged 12–17 years in 2011 1. The risk of the onset of MDD increases sharply during the teenage years, with a lifetime prevalence of 11.0% and 12‐month prevalence of 7.5% for teenagers 3. In addition, adolescent MDD often has a recurrent course that persists into adulthood and afflicted adolescents are at a higher risk of future negative outcomes, such as the loss of social, cognitive and interpersonal skills; poor school performance; increased treatment use; future psychiatric comorbidity 4, 5; and significantly increased risks of self‐harm and suicide 6. MDD is also associated with medical complications later in life, such as cardiovascular disease, stroke, osteoporosis and diabetes 7. It should be noted that other paediatric mental health disorders have also shown an increasing prevalence in the USA, with a 21.8% increase in attention deficit hyperactivity disorder (ADHD) from 2003 to 2007 and a nearly fourfold increase in autism spectrum disorder (ASD) during the last decade 1, now reaching a parent‐reported prevalence of 6.8% for ADHD and 1.1% for ASD among children between three and 17 years of age 1. Adolescent MDD is often associated with other mental disorders, most frequently with generalised anxiety disorder, behavioural disorders and substance abuse 3. Children and adolescents with ADHD and ASD also show increased risks of comorbid depression 3. Assessing comorbidity is important, as MDD may be secondary to the functional limitation of, for example, ADHD or ASD, which will inform the choice of treatment.
The reasons for the increased prevalence of the diagnosis of MDD in adolescents are likely to be complex and include several mechanisms, such as classification bias, financial incentives and social and cultural factors in addition to the actual increase of depressive problems in this age group 8. During the last few decades, we have witnessed a tendency to medicalise depressive symptoms in adolescents by defining depressive symptoms as a medical disease or disorder. This trend has been driven by symptom‐based categorical psychiatric diagnoses defined in the diagnostic and statistical manual of mental disorders (DSM), which has become the foundation on which treatment is considered 9. The DSM symptom criteria are not adapted for age and gender, which leads to low diagnostic validity, especially for adolescent MDD, as symptoms of MDD change across the lifespan, as opposed to other psychiatric disorders, where symptoms remain more constant over time 10. Also, as the DSM system defines depressive symptoms as a medical disorder without considering that depressive pathophysiology develops in the interface between biology and the environmental context, there is a risk that a medical treatment approach is over‐emphasised rather than a well‐balanced approach in which important contextual risk factors are also addressed. Furthermore, as implied in Research Domain Criteria, the new diagnostic mental health approach launched by the National Institute of Mental Health in the USA, depressive symptomatology may constitute dimensional rather than categorical constructs 10 and consist of different combinations of transdiagnostic dimensions of psychopathology 11. The Research Domain Criteria emphasise neurobiological mechanisms, the impact of contextual factors and the importance of a developmental perspective in mental health 12.
Another reason to reconsider the DSM diagnosis of adolescent MDD is that, in general, psychiatric diagnoses are only meaningful when linked to evidence‐based treatment, and a Cochrane meta‐analysis that included more than 1300 participants concluded that ‘there is very limited evidence upon which to base conclusions about the relative effectiveness of psychological interventions, antidepressant medication and a combination of these interventions in children and adolescents’ 13. Importantly, this meta‐analysis included individual studies that are often used to advocate for cognitive behavioural therapy (CBT) and antidepressant medication for treating adolescent depression, such as the Treatment for Adolescents with Depression Study 14, funded by the National Institute of Mental Health.
Cognitive behavioural therapy is currently the most common psychological treatment for adolescent depression, but even though it is considered evidence‐based in adult MDD, it has not shown reliable longstanding effects in adolescents 13. It has been speculated that CBT, which was originally developed for adults, may not be as effective for adolescents with MDD due to differences in cognitive control 15 and reward sensitivity 16. Selective serotonin reuptake inhibitors (SSRIs), which were also originally developed for adult MDD, are now the most commonly used antidepressants for adolescents, even though the effects of SSRIs on brain development are not fully known 17. Several SSRI side effects may be especially problematic for teenagers, such as weight gain, sexual dysfunction and sleep disturbances, which may impede both social functioning and overall health 18. Paradoxically, cognitive impairment is not only one of the most common symptoms of adolescent depression 19, but also a common side effect of SSRIs. Studies comparing adults treated with SSRIs for either MDD or anxiety disorders have demonstrated that these patient groups showed similar patterns of cognitive decline, including fatigue, attention deficit, concentration difficulties and memory impairment, after six months of SSRI treatment, suggesting that the symptoms of cognitive decline represent side effects of SSRIs rather than residual depressive symptoms 20. Emotional blunting and indifference 21, as well as increased violent behaviour 22, have also recently been described as SSRI side effects. SSRIs may also cause withdrawal symptoms at discontinuation, tolerance and resistance phenomena and paradoxical effects, including depression induction and symptomatic worsening 23. A meta‐analysis has shown that SSRIs are less effective in paediatric than in adult MDD, with minimal gains after four weeks of treatment 24. It is generally believed that the antidepressant efficacy of SSRIs increases as a function of baseline depression severity, but it is also hypothesised that this may be due to decreased responsiveness to the placebo effect of SSRIs, rather than to increased responsiveness to medication 25. It is notable that previously published data that supported the efficacy and safety of SSRIs in paediatric populations have shown to be incorrect when reanalysed 26. SSRIs have become one of the most frequently prescribed pharmaceutical substances in the world, and one consequence, which is seldom highlighted in the psychiatric literature, is the acute and chronic ecotoxic and bio‐accumulative effects of SSRIs, especially on marine life 27. This further emphasises the need to develop new and environmentally sustainable treatment methods of adolescent depression.
It is important to state that we do not claim to have fully covered the vast research field of adolescent depression in this study. Here we review the literature with the goal of extending our understanding of adolescent depression beyond the medicalised paradigm, to better succeed in the development of preventative and treatment measures. We summarise recent articles on prevalence and current treatment modalities. We then review the most robust neuroimaging findings of adolescent depression, focusing on the neurocircuitry of sustained threat, which may be helpful in understanding how future treatments can be designed. We summarise how contextual factors are mediated through epigenetic, endocrinal and immunological mechanisms and we then review the literature on the contextual factors related to adolescent depression. Finally, we report on a few new prevention and treatment initiatives and the importance of an alignment with both developmental and depression neuroscience and a contextualised understanding of adolescent depression.
The aberrant neurocircuitry of adolescent depression
An increasing body of research supports the hypothesis that exposure to increased early life stress and, or increased vulnerability to stress through lack of social bonding, care and support, have a detrimental impact on the developing central nervous system 28. This adverse effect on neurodevelopment leads to increased risk for adolescent depression onset, fewer opportunities for neural recovery and more frequent recurrence throughout life 29.
Replicated findings from task‐based functional magnetic resonance imaging (fMRI) support the hypothesis of increased sensitivity to stress in adolescent depression and show that adolescent depression is associated with hyperactivation of the amygdala 30. The amygdala has reciprocal connections with the subgenual anterior cingulate cortex (sgACC), an area that interfaces between affective and cognitive processing, which has also been shown to exhibit hyperactivation in depressed adolescents when compared to well‐matched controls 31, 32. These results suggest that adolescent depression is characterised by an enhanced amygdala response to emotional stimuli, which may further impede the frontolimbic development of cognitive control mechanisms and contribute to increased emotional and social reactivity in depressed teenagers 33.
Resting‐state functional connectivity (RSFC) has also been investigated in adolescent depression and has been used to assess the connectivity of a variety of brain regions in adolescent MDD, including the amygdala and the sgACC 34. The onset of depression in adolescents has been associated with an increase in amygdala RSFC to the sgACC, which has been suggested to represent heightened reactivity to emotional and social stimuli 35. This finding is consistent with previously described task‐based fMRI findings of limbic hyperactivation 30, 31, 32. RSFC between the amygdala and hippocampus has also been shown to be impaired 36. These connections are important for memory, self‐processing and for modulation of physiologic responses to emotion 36. Reward‐related processes and striatum‐based neurocircuitry have also been well studied in the context of adolescent depression 37, but little is yet known about how contextual factors shape reward processing during brain development. In addition, several other neurocircuits are involved in the complex pathophysiology of adolescent depression, and a detailed description is beyond the scope of this study and reviewed elsewhere 38. Importantly, whether they are depressed or not, teenagers have incomplete development of the frontal cortex and underdeveloped frontolimbic connections have been shown to have implications for emotion regulation, impulse control and capacity for foresight and planning, which may contribute to the increased risk for depression in this age group 39.
In summary, converging fMRI findings suggest that adolescent MDD is characterised by significant hyperactivation of the amygdala and sgACC and aberrant functional connectivity between these regions and other regions involved in emotion processing and regulation. This aberrant neurocircuitry should be systematically addressed in future neuroscience‐based interventions.
Genetic and epigenetic mechanisms
Even though depression is moderately heritable, the pathogenesis of depression seems to involve environmentally mediated modifications of gene expression in a multitude of small susceptibility genes rather than specific depression genes 40. Importantly, stress‐related pathology can be transgenerationally transmitted through epigenetic phenomena, and changes in gene expression have been shown to persist long after the initial stress exposure, which may predispose the individual for disease in later life 41. The effects of high maternal stress levels during pregnancy appear to be transmitted to one or two subsequent generations, which may result in an accumulative increase in vulnerability to depression in future generations 42. As complex gene–environment interactions seem to contribute to the vulnerability to depression, contextual considerations are increasingly relevant from this traditionally more deterministic perspective.
Endocrinal, metabolic and immunological mechanisms
As previously described, the trajectory of depressive illness seems to start early, often through relational and contextual impact, which is hypothesised to cause increased limbic sensitivity to emotional stress 28. This situation causes a tendency to perceive the environment as more threatening, with chronic systemic consequences that include increased inflammation 43, oxidative stress, and dysregulation of telomerase activity, neurotrophic factors and neurosteroids, all of which have been implicated in the systemic effects of depression 44. Related persistent hypersecretion of corticotropin‐releasing factor, overproduction of adrenocorticotropic hormone and increased glucocorticoid secretion cause reduced neurogenesis in the hippocampus, which has been related to adolescent and adult depression 45. In females, the effect of cortisol reactivity on the subsequent onset of MDD is influenced by the levels of gonadal steroid hormones associated with pubertal development 46, and early puberty seems to increase the risk of depression in girls 29, 47. Importantly, the earlier onset of puberty, which has been observed, first in USA and now in Europe, coincides with the increasing prevalence of adolescent depression 48.
Contextual considerations
From a prevention and treatment perspective, several contextual considerations may be relevant and important to consider when expanding the analysis of adolescent depression beyond the medicalised paradigm. These include perceived stress, early life adversity, suboptimal attachment, the increased use of technology and exposure to media, and the direct and indirect psychological impact of climate change on adolescent mental health. These contextual factors all have a common denominator in creating a situation of sustained threat for the individual, thereby predisposing an adolescent to developing depression 49.
As a general reflection, the modern world's accelerated pace of living has coincided with an increase in the prevalence of chronic stress‐related mental health problems, such as insomnia, anxiety and depression, especially in young women 1. This stress of modern lifestyles may limit a parent's capacity to bond with his/her children and support their emotional development. It is well know that inconsistent, unreliable or insensitive attachment figures during childhood and adolescence may interfere with the development of a secure, stable mental foundation. This subsequently reduces the child's capacity to cope with stressful life events, thus increasing the risk for adolescent depression 50. A meta‐analysis has reported that neglect and emotional abuse, in particular, are related to depression 51. This should be viewed in the light of data showing that 10% of children in high‐income countries were found to be neglected or psychologically abused, 4–16% were physically abused and 15–30% had been exposed to sexual abuse each year 52.
Social support targeting young people directly seems to partially buffer the effects of current stressors on mental health 53, and when parenting capacity is insufficient, opportunities for potential resilience through secondary attachment persons have shown to be protective 54. Unfortunately, modern facets of society, including lack of supporting care from extended families and friends and the large‐scale, nonparental day care centres that are common in urban environments, seem to undermine such efforts 54.
Media and technology are additional contextual factors that have shown a massive increase during the last decades. On average, American teenagers spend 6.75 hours a day engaging with media, with television as the dominant medium, which is more than any other waking activity 55. When the simultaneous use of multiple media is included, this figure increases to eight hours daily 55. Total media exposure in adolescence has been associated with an increased risk of depressive symptoms in young adulthood, especially for males 56, and more than two hours of Internet use per day has been related to increased self‐reported depression scores 57. The use of technology seems to have a negative effect on adolescent mental health that is independent of sedentariness, lack of sleep or poor eating habits 58. Cultural messages transmitted through media may drive depressive symptomatology by repeating the exposure of highly idealised and simplified characters and situations, leading to increased comparison of one's self with unrealistic images 56. This may also affect body image and increase the risks of eating disturbances and depression 59. Market‐driven values are often communicated through media and lead to consistent negative associations with overall well‐being 60.
Peer victimisation is related to both suicidal ideation and suicide attempts 61, and cyberbullying is more strongly linked than traditional bullying to emotional distress and suicidal ideas 61. Between 20% and 40% of American children and adolescents have been victims of cyberbullying, with females and sexual minorities facing a higher risk 62. Social media, such as Facebook, creates high incentives for adolescents to grow extensive online networks, and this increases the risks of exploitation and amplification of aggressive behaviour 61. These mechanisms increase risk and susceptibility to peer victimisation and social rejection, which are among the strongest proximal risk factors for depression 63. A more comprehensive review of the impact of social media on mental health has been published elsewhere 64.
Over the last few decades, as depressive symptoms in adolescents have been increasing, scientists have come to a consensus about climate change and approaching ecological tipping points. These have severe consequences for human life, such as increased carbon dioxide emissions, rising temperatures, mass extinction of species, air, earth and water pollution, and the unravelling of ecosystems 65. An emerging body of literature has addressed the effects of climate change on mental health 66. Climate change has a direct psychological impact in terms of perceived threat, stress, trauma, anxiety and depression and also indirectly through increases in violence and aggression, loss of autonomy and community identity and increasing social inequality 67. Children and adolescents are particularly vulnerable to the impact of climate change 66. A recent Swedish survey showed that 80% of 15–25 years old had climate‐related anxiety and that 78% felt that they had been left to cope with their parents’ generation's failure to take responsibility and to respond adequately to climate change 68. The adult generation's individual and collective emotional avoidance of the consequences of climate change may be an important risk factor for maladaptive behaviour and depression in adolescents, who are left with insufficient support to cope with their own emotional reactions such as fear, anger, complex grief, a sense of loss, lack of control and helplessness 69.
Implications for novel treatment strategies
A few theoretically sound psychological treatment strategies have emerged and are showing preliminary promising results. These treatments include attachment‐based family therapy 70, interpersonal psychotherapy 71, acceptance commitment therapy 72, thinking about reward in young people 16, game‐based digital interventions 73 and Internet and computer‐based therapy 74. However, on the basis of the findings reviewed in this paper, we promote the development of neuroscientifically informed, contextually aware and ecologically sustainable ways to treat adolescent depression in a manner that simultaneously empowers, informs and prepares the young generation for a future with rapidly changing living conditions. Training for awareness resilience and action (TARA) is based on neuroscientifically informed training and targets the neurocircuitry of sustained threat, as shown in Figure 1. Skills training inspired by yoga‐based practices, including breathing techniques and slow, focused movement, is applied to calm limbic hyperactivity and to improve emotion regulation through vagal and sensory afferent connections 15, potentially normalising the functional connectivity between the amygdala and key areas of emotion regulation. The TARA program also includes an extended social and systemic perspective of adolescent depression 15.
Figure 1.
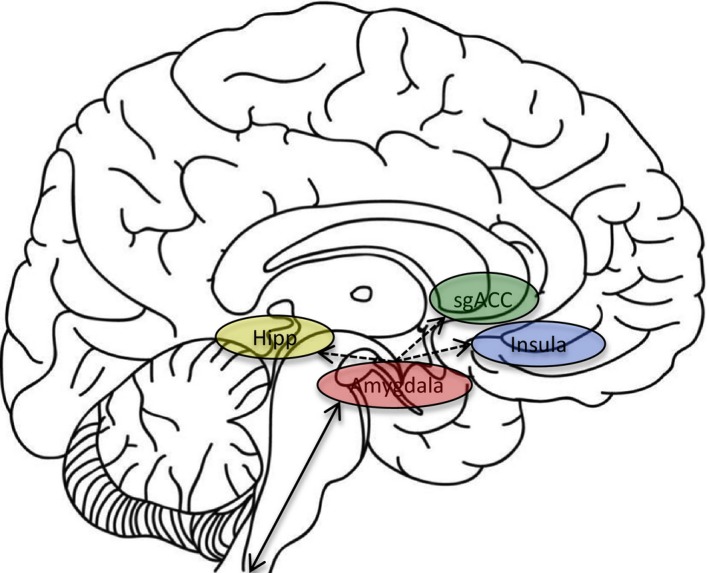
Schematic illustration of a possible neurocircuitry to be targeted in a brain‐based intervention for adolescent depression: reducing amygdala hyper‐reactivity through practice of vagal afference and potentially normalising functional connectivity between the amygdala and key areas of emotion processing such as the hippocampus (Hipp), the subgenual anterior cingulate cortex (sgACC) and the insula.
As it is increasingly clear that the root cause of depressive illness often originates early in life, more prevention efforts are also warranted. Transdisciplinary collaboration, especially with the growing research field of prevention science, may increase our ability to reduce morbidity and mortality in adolescent depression 75. Minimising exposure to early life stress and, or decreasing vulnerability to stress through improved social bonding, care and support could help improve the regulation of limbic function and optimise the development of the central nervous system 76. Several evidence‐based school and family programmes have been developed, but unfortunately sporadic and inconsistent implementation remains a persistent challenge to realising the potential benefits of these interventions 77. Improved knowledge on how to successfully and sustainably finance, disseminate and implement evidence‐based programmes for paediatric mental health in schools and in public service systems is needed 78, as well as an intentional paradigm shift to an ecological public health model where the local norms in diverse settings are considered 79. To minimise the detrimental impact of media, technology and cyberbullying on the developing brain, a multipronged approach is suggested, including school‐based programmes, educational media campaigns, parental involvement as well as new policies and legislative action to achieve system‐level changes 62.
Finally, an increasingly acute and impactful stressor that adolescents now have to contend with is climate change, which may also have an impact on the core structures of society in ways that drive the psychopathology of adolescent depression 80, for example through decreased social cohesion and loss of trust both between community members and in relation to institutions 80. In a larger contextual framework, it is evident that building collective resilience is a key factor in preventing adolescent depression, which includes addressing social inequality, creating organisational collaboration, protecting social support initiatives and engaging adolescents in mitigation of the effects of climate change 80. It has been suggested that talking about the psychological impact of climate change in general will help to better process and accept potentially overwhelming climate information and thus prevent more longstanding climate‐related depression 74. Providing forums where young people can inspire and support each other to committed action for the climate or other values they care about may contribute to the creation of new social norms and be part of the prevention and treatment of adolescent depression 66. This approach is currently being integrated into the novel TARA model for group treatment of adolescent depression 15.
Conclusion
In this study, we reviewed the literature explaining how contextual factors such as early life adversity and stress, insecure attachment, extensive use of technology and social media and the consequences of climate change all contribute to perceptions of sustained threat for the individual. The perception of sustained threat is related to amygdala hyper‐reactivity and aberrant functional connectivity between the amygdala and key emotion regulation areas, which increases the risk for adolescent depression. The neurocircuitry dysfunction is mediated and maintained through epigenetic, hormonal, metabolic and immunological mechanisms that include hypothalamic–pituitary–adrenal axis overdrive. The critical issue is that contextual factors that increase the child's perception of sustained threat and contribute to the increased prevalence of adolescent depression that we currently witness cannot be successfully addressed just within a limited medicalised treatment paradigm. It is therefore time to consider how to effectively prevent adolescent depression and suicide from an integrated transdisciplinary research platform.
The development of theoretically well‐grounded new psychological treatment strategies that adequately target the implicated neurocircuitry of sustained threat in developmentally appropriate ways is warranted. Bringing an understanding of stress‐mediated effects on neurodevelopment, the impact of technology and social media on social emotional regulation and the effect of environmental degradation on individual and community resilience into the equation will contribute to the emergence of new prevention and treatment targets. It is hoped that this critical review of adolescent depression will inspire continued discussion and progress in preventing and treating depression in young people.
Funding statement
This work was supported by the Swedish Research Council (Grant number 350‐2012‐303); the Swedish Society of Medicine (Grant number SLS244671 and 499411); the Brain and Behavior Research Foundation (formerly NARSAD); the National Institute of Mental Health (Grant numbers 7R01MH085734, R01MH085734‐02S1, R01MH085734‐05S1 and K01MH097978); and the American Foundation for Suicide Prevention (PDF‐1‐064‐13). The funding agencies played no role in the interpretation or review of the data.
Conflict of interest
None of the authors declared any conflict of interest.
Acknowledgement
We would like to thank David Vago for providing illustrative material.
References
- 1. Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, et al. Mental health surveillance among children–United States, 2005–2011. Morbidity and mortality weekly report. MMWR Surveill Summ 2013; 62(Suppl 2): 1–35. [PubMed] [Google Scholar]
- 2. The Swedish National Board of Health and Welfare . F. Folkhälsorapporten 2009. 2009.
- 3. Avenevoli S, Swendsen J, He JP, Burstein M, Merikangas KR. Major depression in the national comorbidity survey‐adolescent supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry 2015; 54: 37–44.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Korczak DJ, Goldstein BI. Childhood onset major depressive disorder: course of illness and psychiatric comorbidity in a community sample. J Pediatr 2009; 155: 118–23. [DOI] [PubMed] [Google Scholar]
- 5. Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child Adolesc Psychiatr Clin N Am 2002; 11: 619–37. [DOI] [PubMed] [Google Scholar]
- 6. Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, et al. Childhood and adolescent depression: a review of the past 10 years. Part I. J Am Acad Child Adolesc Psychiatry 1996; 35: 1427–39. [DOI] [PubMed] [Google Scholar]
- 7. Wolkowitz OM, Reus VI, Mellon SH. Of sound mind and body: depression, disease, and accelerated aging. Dialogues Clin Neurosci 2011; 13: 25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mulder RT. An epidemic of depression or the medicalization of distress? Perspect Biol Med 2008; 51: 238–50. [DOI] [PubMed] [Google Scholar]
- 9. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders DSM‐IV‐TR Fourth Edition: American Psychiatric Association; 2000. [Google Scholar]
- 10. Henje Blom E, Forsman M, Yang TT, Serlachius E, Larsson JO. Latent classes of symptoms related to clinically depressed mood in adolescents. Scand J Child Adolesc Psychiatr Psychol 2014; 2: 19–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry 2010; 167: 748–51. [DOI] [PubMed] [Google Scholar]
- 12. Casey BJ, Oliveri ME, Insel T. A neurodevelopmental perspective on the research domain criteria (RDoC) framework. Biol Psychiatry 2014; 76: 350–3. [DOI] [PubMed] [Google Scholar]
- 13. Cox GR, Callahan P, Churchill R, Hunot V, Merry SN, Parker AG, et al. Psychological therapies versus antidepressant medication, alone and in combination for depression in children and adolescents. Cochrane Database Syst Rev 2014; 11: CD008324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reinecke MA, Curry JF, March JS. Findings from the Treatment for Adolescents with Depression Study (TADS): what have we learned? What do we need to know? J Clin Child Adolesc Psychol 2009; 38: 761–7. [DOI] [PubMed] [Google Scholar]
- 15. Henje Blom E, Duncan LG, Ho TC, Connolly CG, LeWinn KZ, Chesney M, et al. The development of an RDoC‐based treatment program for adolescent depression: “Training for Awareness, Resilience, and Action” (TARA). Front Hum Neurosci 2014; 8: 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rice F, Rawal A, Riglin L, Lewis G, Lewis G, Dunsmuir S. Examining reward‐seeking, negative self‐beliefs and over‐general autobiographical memory as mechanisms of change in classroom prevention programs for adolescent depression. J Affect Disord 2015; 186: 320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cousins L, Goodyer IM. Antidepressants and the adolescent brain. J Psychopharmacol 2015; 29: 545–55. [DOI] [PubMed] [Google Scholar]
- 18. Ferguson JM. SSRI antidepressant medications: adverse effects and tolerability. Prim Care Companion J Clin Psychiatry 2001; 3: 22–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jaycox LH, Stein BD, Paddock S, Miles JN, Chandra A, Meredith LS, et al. Impact of teen depression on academic, social, and physical functioning. Pediatrics 2009; 124: e596–605. [DOI] [PubMed] [Google Scholar]
- 20. Popovic D, Vieta E, Fornaro M, Perugi G. Cognitive tolerability following successful long term treatment of major depression and anxiety disorders with SSRi antidepressants. J Affect Disord 2015; 173: 211–5. [DOI] [PubMed] [Google Scholar]
- 21. Sansone RA, Sansone LA. SSRI‐induced indifference. Psychiatry 2010; 7: 14–8. [PMC free article] [PubMed] [Google Scholar]
- 22. Molero Y, Lichtenstein P, Zetterqvist J, Gumpert CH, Fazel S. Selective serotonin reuptake inhibitors and violent crime: a cohort study. PLoS Med 2015; 12: e1001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fava GA, Offidani E. The mechanisms of tolerance in antidepressant action. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35: 1593–602. [DOI] [PubMed] [Google Scholar]
- 24. Varigonda AL, Jakubovski E, Taylor MJ, Freemantle N, Coughlin C, Bloch MH. Systematic review and meta‐analysis: early treatment responses of selective serotonin reuptake inhibitors in pediatric major depressive disorder. J Am Acad Child Adolesc Psychiatry 2015; 54: 557–64. [DOI] [PubMed] [Google Scholar]
- 25. Kirsch I, Deacon BJ, Huedo‐Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: a meta‐analysis of data submitted to the food and drug administration. PLoS Med 2008; 5: e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Le Noury J, Nardo JM, Healy D, Jureidini J, Raven M, Tufanaru C, et al. Restoring study 329: efficacy and harms of paroxetine and imipramine in treatment of major depression in adolescence. BMJ 2015; 351: h4320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Silva LJ, Pereira AM, Meisel LM, Lino CM, Pena A. Reviewing the serotonin reuptake inhibitors (SSRIs) footprint in the aquatic biota: uptake, bioaccumulation and ecotoxicology. Environ Pollut 2015; 197: 127–43. [DOI] [PubMed] [Google Scholar]
- 28. Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D, et al. Limbic scars: long‐term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatry 2012; 71: 286–93. [DOI] [PubMed] [Google Scholar]
- 29. Sisk CL, Zehr JL. Pubertal hormones organize the adolescent brain and behavior. Front Neuroendocrinol 2005; 26: 163–74. [DOI] [PubMed] [Google Scholar]
- 30. Yang TT, Simmons AN, Matthews SC, Tapert SF, Frank GK, Max JE, et al. Adolescents with major depression demonstrate increased amygdala activation. J Am Acad Child Adolesc Psychiatry 2010; 49: 42–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yang TT, Simmons AN, Matthews SC, Tapert SF, Frank GK, Bischoff‐Grethe A, et al. Depressed adolescents demonstrate greater subgenual anterior cingulate activity. NeuroReport 2009; 20: 440–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ho TC, Yang G, Wu J, Cassey P, Brown SD, Hoang N, et al. Functional connectivity of negative emotional processing in adolescent depression. J Affect Disord 2014; 155: 65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Michl LC, McLaughlin KA, Shepherd K, Nolen‐Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: longitudinal evidence in early adolescents and adults. J Abnorm Psychol 2013; 122: 339–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kerestes R, Davey CG, Stephanou K, Whittle S, Harrison BJ. Functional brain imaging studies of youth depression: a systematic review. Neuroimage Clin 2013; 4: 209–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Davey CG, Whittle S, Harrison BJ, Simmons JG, Byrne ML, Schwartz OS, et al. Functional brain‐imaging correlates of negative affectivity and the onset of first‐episode depression. Psychol Med 2015; 45: 1001–9. [DOI] [PubMed] [Google Scholar]
- 36. Cullen KR, Westlund MK, Klimes‐Dougan B, Mueller BA, Houri A, Eberly LE, et al. Abnormal amygdala resting‐state functional connectivity in adolescent depression. JAMA Psychiatry 2014; 71: 1138–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Forbes EE, Dahl RE. Research review: altered reward function in adolescent depression: what, when and how? J Child Psychol Psychiatry 2012; 53: 3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hulvershorn LA, Cullen K, Anand A. Toward dysfunctional connectivity: a review of neuroimaging findings in pediatric major depressive disorder. Brain Imaging Behav 2011; 5: 307–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Andrews‐Hanna JR, Mackiewicz Seghete KL, Claus ED, Burgess GC, Ruzic L, Banich MT. Cognitive control in adolescence: neural underpinnings and relation to self‐report behaviors. PLoS One 2011; 6: e21598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Levinson DF. The genetics of depression: a review. Biol Psychiatry 2006; 60: 84–92. [DOI] [PubMed] [Google Scholar]
- 41. Kim DR, Bale TL, Epperson CN. Prenatal programming of mental illness: current understanding of relationship and mechanisms. Curr Psychiatry Rep 2015; 17: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Harris A, Seckl J. Glucocorticoids, prenatal stress and the programming of disease. Horm Behav 2011; 59: 279–89. [DOI] [PubMed] [Google Scholar]
- 43. Henje Blom E, Lekander M, Ingvar M, Asberg M, Mobarrez F, Serlachius E. Pro‐inflammatory cytokines are elevated in adolescent females with emotional disorders not treated with SSRIs. J Affect Disord 2012; 136: 716–23. [DOI] [PubMed] [Google Scholar]
- 44. Taylor SE, Way BM, Seeman TE. Early adversity and adult health outcomes. Dev Psychopathol 2011; 23: 939–54. [DOI] [PubMed] [Google Scholar]
- 45. Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci 2008; 31: 183–91. [DOI] [PubMed] [Google Scholar]
- 46. Colich NL, Kircanski K, Foland‐Ross LC, Gotlib IH. HPA‐axis reactivity interacts with stage of pubertal development to predict the onset of depression. Psychoneuroendocrinology 2015; 55: 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Galvao TF, Silva MT, Zimmermann IR, Souza KM, Martins SS, Pereira MG. Pubertal timing in girls and depression: a systematic review. J Affect Disord 2014; 155: 13–9. [DOI] [PubMed] [Google Scholar]
- 48. Mouritsen A, Aksglaede L, Sorensen K, Mogensen SS, Leffers H, Main KM, et al. Hypothesis: exposure to endocrine‐disrupting chemicals may interfere with timing of puberty. Int J Androl 2010; 33: 346–59. [DOI] [PubMed] [Google Scholar]
- 49. Perlman G, Simmons AN, Wu J, Hahn KS, Tapert SF, Max JE, et al. Amygdala response and functional connectivity during emotion regulation: a study of 14 depressed adolescents. J Affect Disord 2012; 139: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Malik S, Wells A, Wittkowski A. Emotion regulation as a mediator in the relationship between attachment and depressive symptomatology: a systematic review. J Affect Disord 2014; 172C: 428–44. [DOI] [PubMed] [Google Scholar]
- 51. Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: a meta‐analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry 2015; 30: 665–80. [DOI] [PubMed] [Google Scholar]
- 52. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high‐income countries. Lancet 2009; 373: 68–81. [DOI] [PubMed] [Google Scholar]
- 53. Moskowitz D, Vittinghoff E, Schmidt L. Reconsidering the effects of poverty and social support on health: a 5‐year longitudinal test of the stress‐buffering hypothesis. J Urban Health 2013; 90: 175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mikulincer M, Shaver PR. An attachment perspective on psychopathology. World Psychiatry 2012; 11: 11–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Roberts DF. Media and youth: access, exposure, and privatization. J Adolesc Health 2000; 27: 8–14. [DOI] [PubMed] [Google Scholar]
- 56. Primack BA, Swanier B, Georgiopoulos AM, Land SR, Fine MJ. Association between media use in adolescence and depression in young adulthood: a longitudinal study. Arch Gen Psychiatry 2009; 66: 181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bailin A, Milanaik R, Adesman A. Health implications of new age technologies for adolescents: a review of the research. Curr Opin Pediatr 2014; 26: 605–19. [DOI] [PubMed] [Google Scholar]
- 58. Rosen LD, Lim AF, Felt J, Carrier LM, Cheever NA, Lara‐Ruiz JM, et al. Media and technology use predicts ill‐being among children, preteens and teenagers independent of the negative health impacts of exercise and eating habits. Comput Hum Behav 2014; 35: 364–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Stice E, Hayward C, Cameron RP, Killen JD, Taylor CB. Body‐image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol 2000; 109: 438–44. [PubMed] [Google Scholar]
- 60. Dittmar H, Bond R, Hurst M, Kasser T. The relationship between materialism and personal well‐being: a meta‐analysis. J Pers Soc Psychol 2014; 107: 879–924. [DOI] [PubMed] [Google Scholar]
- 61. van Geel M, Vedder P, Tanilon J. Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: a meta‐analysis. JAMA Pediatr 2014; 168: 435–42. [DOI] [PubMed] [Google Scholar]
- 62. Aboujaoude E, Savage MW, Starcevic V, Salame WO. Cyberbullying: review of an old problem gone viral. J Adolesc Health 2015; 57: 10–8. [DOI] [PubMed] [Google Scholar]
- 63. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull 2014; 140: 774–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Toseeb U, Inkster B. Online social networking sites and mental health research. Front Psychiatry 2015; 6: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Shaftel HJA (editor). Global Climate Change, Vital Signs of the Planet. California Institute of Technology, Pasadena, CA: The Earth Science Communications Team at NASA's Jet Propulsion Laboratory, 2015. [Google Scholar]
- 66. Clayton S, Manning C, Hodge C. Beyond storms and droughts: The psychological impacts of climate change momentus. Available from URL http://ecoamerica.org/wp-content/uploads/2014/06/eA_Beyond_Storms_and_Droughts_Psych_Impacts_of_Climate_Change.pdf2014.
- 67. Kowalski RM, Giumetti GW, Schroeder AN, Lattanner MR. Bullying in the digital age: a critical review and meta‐analysis of cyberbullying research among youth. Psychol Bull 2014; 140: 1073–137. [DOI] [PubMed] [Google Scholar]
- 68. Wirtén HK, Klum M, Lakso J, Nyberg H, Holmgren P. 80 procent av Sveriges unga har klimatångest. Svenska Dagbladet, 2014. [Google Scholar]
- 69. Spinhoven P, Drost J, de Rooij M, van Hemert AM, Penninx BW. A longitudinal study of experiential avoidance in emotional disorders. Behav Ther 2014; 45: 840–50. [DOI] [PubMed] [Google Scholar]
- 70. Ewing ES, Diamond G, Levy S. Attachment‐based family therapy for depressed and suicidal adolescents: theory, clinical model and empirical support. Attach Hum Dev 2015; 17: 136–56. [DOI] [PubMed] [Google Scholar]
- 71. Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry 2004; 61: 577–84. [DOI] [PubMed] [Google Scholar]
- 72. Hayes L, Boyd CP, Sewell J. Acceptance and commitment therapy for the treatment of adolescent depression: a pilot study in a psychiatric outpatient setting. Mindfulness 2011; 2: 86–94. [Google Scholar]
- 73. Li J, Theng YL, Foo S. Game‐based digital interventions for depression therapy: a systematic review and meta‐analysis. Cyberpsychol Behav Soc Netw 2014; 17: 519–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ebert DD, Zarski AC, Christensen H, Stikkelbroek Y, Cuijpers P, Berking M, et al. Internet and computer‐based cognitive behavioral therapy for anxiety and depression in youth: a meta‐analysis of randomized controlled outcome trials. PLoS One 2015; 10: e0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE Jr, Ross DA, et al. Worldwide application of prevention science in adolescent health. Lancet 2012; 379: 1653–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci U S A 2012; 109(Suppl 2): 17180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Evans R, Murphy S, Scourfield J. Implementation of a school‐based social and emotional learning intervention: understanding diffusion processes within complex systems. Prev Sci 2015; 16: 754–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Greenberg MT, Lippold MA. Promoting healthy outcomes among youth with multiple risks: innovative approaches. Annu Rev Public Health 2013; 34: 253–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Atkins MS, Rusch D, Mehta TG, Lakind D. Future directions for dissemination and implementation science: aligning ecological theory and public health to close the research to practice gap. J Clin Child Adolesc Psychol 2015; 53: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Norris FH, Stevens SP, Pfefferbaum B, Wyche KF, Pfefferbaum RL. Community resilience as a metaphor, theory, set of capacities, and strategy for disaster readiness. Am J Community Psychol 2008; 41: 127–50. [DOI] [PubMed] [Google Scholar]


