Abstract
Purpose
This study examines differences in prescription opioid misuse (POM) among adolescents in rural, small urban and large urban areas of the US and identifies several individual, social, and community risk factors contributing to those differences.
Methods
We used nationally representative data from the 2011 and 2012 National Survey on Drug Use and Health (NSDUH) and estimated binary logistic regression and formal mediation models to assess past-year POM among 32,036 adolescents aged 12–17.
Results
Among adolescents, 6.8% of rural, 6.0% of small urban, and 5.3% of large urban engaged in past-year POM. Net of multiple risk and protective factors, rural adolescents have 35% greater odds and small urban adolescents have 21% greater odds of past-year POM compared to large urban adolescents. The difference between rural and small urban adolescents was not significant. Criminal activity, lower perceived substance use risk, and greater use of emergency medical treatment partially contribute to higher odds among rural adolescents, but they are also partially buffered by less peer substance use, less illicit drug access, and stronger religious beliefs.
Conclusions
Researchers, policy makers, and treatment providers must consider the complex array of individual, social, and community risk and protective factors to understand rural/urban differences in adolescent POM. Potential points of intervention to prevent POM in general and reduce rural disparities include early education about addiction risks, use of family drug courts to link criminal offenders to treatment, and access to non-emergency medical services to reduce rural residents’ reliance on emergency departments where opioid prescribing is more likely.
Keywords: demography, drug abuse, epidemiology, geography, sociology
Prescription opioid misuse (POM) is a critical United States (US) public health issue. POM is responsible for over 16,000 US deaths annually1 and has an estimated annual cost of nearly $56 billion (2009 USD).2 For every opioid-related death, there are 10 treatment admissions and 32 emergency department (ED) visits.3 Of particular concern is the substantial increase in adolescent POM since the 1960s (0.4% in 1965 to 8% by 2012),4,5 partly due to the almost doubling of opioid prescriptions written for adolescents and young adults since 1994.6
Adolescence is a critical time to study POM because most substance use begins during this period,7 and individuals who initiate use before age 18 are more likely to develop a POM disorder than those who initiate later in life.8 Studies on risk factors for adolescent POM find risky attitudes and misconceptions regarding the illegality and safety of prescription opioids make experimenting with opioids more attractive compared to illicit drugs.9 In a systematic review of nationally representative studies,10 low family income, poor mental health, receipt of mental health treatment, illicit drug use, delinquency, residentially instability, ED use, peer norms, parental factors, and weaker bonds to school were all positively associated with adolescent POM. Although these risk factors differ between rural and urban areas, research on rural/urban differences in adolescent POM, and particularly the role of different risk and protective factors in explaining those differences, remains sparse.
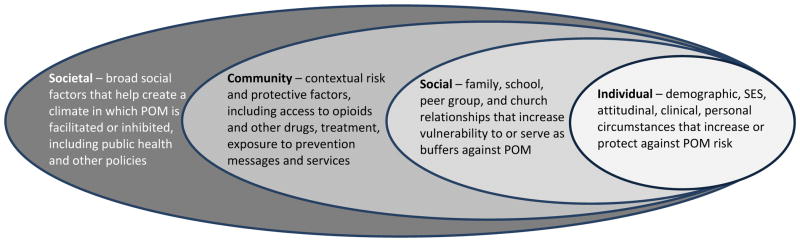
Spatial variation in POM is of great interest to researchers and policy makers. Indeed, the origins of the POM epidemic can be traced to rural America, where reports of OxyContin® abuse first surfaced.11 Communities along the rural-urban continuum now struggle with high rates of opioid overdose deaths, excessive opioid diversion, and increased treatment admissions.12–15 Yet, there is scant nationally representative research that includes rural/urban status in models predicting adolescent POM,16–19 and only Havens et al16 explicitly examine rurality as a main independent variable of interest, finding rural adolescents to be at greater risk than their urban counterparts, even after controlling for multiple confounders. Though informative, this study assessed lifetime rather than recent POM, and a focus on the specific risk and protective factors that contribute to rural/urban differences was beyond the scope of the paper. Dew and colleagues20 propose a multidimensional approach to understanding substance use that accounts not only for individual circumstances, but also integrates social factors and community risk and prevention influences. This social-ecological model (see Figure 1), popularized in sociological research on neighborhood effects21–24 and increasingly employed in public health research,20,25 allows us to consider the complex interplay between the multiple factors that put adolescents at risk of or buffer against substance abuse within rural and urban communities. To our knowledge, no existing research applies this framework to try to understand rural/urban differences in adolescent POM.
Figure 1.
A Social-Ecological Model for Understanding Rural/Urban Differences in Adolescent POM
Broad societal trends, including deteriorating rural economic and employment conditions over the past 30 years,26,27 historically high rates of opioid prescribing,28 and expanded trafficking networks and Internet availability of opioids20 have led to increased demand for and access to opiates in rural areas. Rural and urban social and community contexts vary in significant ways that may exacerbate the effects of these societal trends. Dew et al20 suggest distinctive features of rural areas increase the likelihood of substance abuse, including higher poverty rates,26,27,29 peer norms,30,31 lack of recreational activities, family and community denial about substance abuse, and an emphasis on self-reliance that leads to lack of treatment services and prevention efforts.20 On the other hand, rural adolescents may be buffered by traditional family values that emphasize interpersonal support, organized religion,32 and greater school involvement.33 Rural adolescents also may be at reduced risk of POM due to greater isolation from drug markets.34 Ultimately, the complexities of multiple intersecting risk and protective factors suggest rural adolescents may be simultaneously buffered by certain aspects of their families, schools, and communities and at increased risk of POM relative to urban adolescents as a result of other factors.
Understanding the factors that influence rural/urban differences in POM is important for tailoring interventions to the unique needs of adolescents in these different spatial environments. The current study builds on previous research on rural/urban differences in POM by a) using a large nationally representative sample of US adolescents; b) conceptualizing rural/urban status as a “trichotomy” (ie, large urban, small urban, rural) rather than the dichotomy commonly found in the literature; c) employing a social-ecological framework that accounts for multiple individual, social, and community conditions that may contribute to rural/urban differences in POM; and d) conducting formal mediation analyses to identify the specific contributions of each factor to rural/urban differences in POM.
Methods
Data
Data are from the 2011 and 2012 National Survey on Drug Use and Health (NSDUH), i,35,36 an annual household survey of the US population aged 12 and older. The NSDUH includes a section on “youth experiences” making it ideal for studying risk factors for adolescent POM. Our analytic sample included 32,036 respondents ages 12–17.
Measures
Our outcome was past-year prescription opioid misuse (POM). The NSDUH defines POM as use without a prescription from a doctor or use for the feeling or experience it causes. The independent variable was rural/urban trichotomy: lives in a Core Based Statistical Area (CBSA) with 1 million or more persons (large CBSA), lives in a CBSA with fewer than 1 million persons (small CBSA), and does not live in a CBSA (rural).ii Suburban areas are included within both large and small CBSAs.
We examined the contributions of individual, social, and community factors to rural/urban differences in adolescent POM. Individual circumstances included demographic characteristics (age, gender, race/ethnicity, number of people in the household), socioeconomic status (annual family income, family receipt of public assistance [SNAP and/or cash assistance], adolescent health insurance), history of delinquency/substance use (committed crime in past year [gang fighting, carried handgun, sold illegal drugs, stole/tried to steal item worth $50+, attacked someone with intent to seriously harm]; ever been arrested and booked; perceived substance use risk index; smoked average of 1+ cigarettes/day in past year; past-year binge drinking, marijuana use, other illicit drug use [powder cocaine, crack, heroin, hallucinogens, LSD, PCP, ecstasy, inhalants, methamphetamine]; and misuse of non-opioid medications [tranquilizers, sedatives, and stimulants]), and clinical characteristics (poor/fair self-rated health and past-year major depressive episode, doctor’s diagnosis of anxiety, ED treatment, and overnight hospitalization for emotional treatment). Age of first substance use was strongly correlated with age, so we excluded it from our models. Statistical tests for multicollinearity (VIF, TOL) revealed no problems with any other predictors.
Social factors included family characteristics (both parents living in household, parent involvement index, parents’ attitudes toward substance use index), school factors (school connectedness index, past-year exposure to school-based prevention classes/activities), peer influences (peer substance use index, friends’ attitudes toward substance use index), religiosity (past-year religious service attendance, religious beliefs index), and characteristics encompassing all 3 social domains (past-year participation in school, community, or faith-based activities; lack of social/emotional support; and residential instability [moved in past 5 years]). Consistent with Ford,18 respondents who were not attending school were assigned a score of 0 on school-specific items so we could include this important at-risk group.
Community and environmental influences included being approached by somebody selling illicit drugs in the past 30 days; drug access index; past-year participation in non-school-based self-help, counseling, or prevention (including AA/substance abuse prevention); and past-year exposure to non-school-based substance abuse prevention messages.
Specific variables included in each index, their anchors, and Cronbach’s alphas are shown in Table 1.
Table 1.
Items Included in Indices
| Items | Anchors |
|---|---|
| Perceived Substance Use Risk Index (α = .86) | |
| How much do people risk harming themselves physically and in other ways: Risk of smoking 1 or more packs of cigarettes per day Risk of smoking marijuana once a month Risk of smoking marijuana once or twice a week Risk of trying LSD once or twice Risk of using LSD once or twice per week Risk of trying heroin once or twice Risk of using heroin once or twice a week Risk of using cocaine once a month Risk of using cocaine once or twice a week Risk of having 4 or 5 drinks nearly every day Risk of having 5 or more drinks once or twice a week |
0=no risk 1=slight risk 2=moderate risk 3=great risk |
| Parent Involvement Index (α = .71) | |
| During the past 12 months how often did parents: Check if you’ve done your homework Help you with homework Make you do work/chores Limit your amount of TV time Limit your time out with friends on school nights Let you know you did a good job Tell you they’re proud of something you had done |
0=never 1=seldom 2=sometimes 3=always |
| Parents’ Disapproval toward Substance Use Index (α = .85) | |
| How do you think parents would feel about you: Smoking 1+ pack of cigarettes per day Trying marijuana/hashish Using marijuana/hashish monthly Drinking alcohol daily |
0=neither approve nor disapprove 1=somewhat disapprove 2=strongly disapprove |
| School Connectedness Index (α = .77) | |
| During the past 12 months: How did you feel overall about going to school? |
0=hated going to school 1=didn’t like going to school 2=kind of liked going to school 3=liked going to school a lot |
| How often did you feel school work was meaningful? | 0=never 1=seldom 2=sometimes 3=always |
| How important do you think the things you have learned in school will be later in life? | 0=very unimportant 1=somewhat unimportant 2=somewhat important 3=very important |
| How interesting are courses at school? | 0=very boring 1=somewhat boring 2=somewhat interesting 3=very interesting |
| How often did teacher say you were doing a good job? | 0=never 1=seldom 2=sometimes 3=always |
| Peer Substance Abuse Index (α = .89) | |
| How many students you know in grade smoke cigarettes? How many students you know in grade use marijuana/hashish? How many students you know in grade drink alcohol? How many students you know in grade get drunk weekly? |
0=none of them 1=a few of them 2=most of them 3=all of them |
| Friends’ Disapproval toward Substance Use Index (α = .89) | |
| How do you think your friends would feel about you: Smoking 1+ pack of cigarettes per day Trying marijuana/hashish Using marijuana/hashish monthly Drinking alcohol daily |
0=neither approve nor disapprove 1=somewhat disapprove 2=strongly disapprove |
| Religious Beliefs Importance Index (α = .84) | |
| My religious beliefs are very important My religious beliefs influence my decisions It is important that my friends share my religious beliefs |
0=strongly disagree 1=disagree 2=agree 3=strongly agree |
| Illicit Drug Access Index (α = .91) | |
| How easy or difficult to get marijuana? How easy or difficult to get LSD? How easy or difficult to get cocaine? How easy or difficult to get crack? How easy or difficult to get heroin? |
0=probably impossible 1=very difficult 2=fairly difficult 3=fairly easy 4=very easy |
Note: α = standardized Cronbach’s alpha
Data Analysis
We conducted all analyses using the SVYSET and SVY commands in Stata (StataCorp LLP, College Station, Texas) to account for the complex multistage sampling design of the NSDUH, including strata, cluster, and survey weight. We first examined descriptive statistics for all variables across the rural/small urban/large urban trichotomy and conducted adjusted Wald tests to determine whether there were significant differences in characteristics across the 3 categories. We estimated unadjusted binary logistic regression models for all predictors, identifying the characteristics associated with POM for the full sample. We then estimated an adjusted model accounting for all predictors. Finally, we present results from formal mediation analyses conducted with the KHB method in Stata.40 This method enables us to identify the degree to which specific factors mediate rural/urban differences in POM while adjusting for the rescaling/attenuation bias that arises in cross-model comparisons of nonlinear models. Using this method, we identify both positive and negative (suppressor) mediators41 and disentangle the unique contribution of each mediator while controlling for confounders.iii We identify which characteristics are contributing the most to rural/urban differences in POM, and specifically, which characteristics of rural adolescents and their contexts serve as the most influential buffers against POM (compared to their urban peers) and which characteristics serve as the most influential risk factors for POM (compared to their urban peers).
Results
Descriptive statistics by rural/urban status are displayed in Table 2. A significantly greater percentage of rural adolescents (6.7%) reported past-year POM compared with adolescents in large urban areas (5.3%, P = .042). The difference between small urban (6.0%) and rural was not statistically significant (P = .269). Rural adolescents had lower family incomes than small and large urban adolescents and were significantly more likely to live in families receiving public assistance and less likely to have health insurance than adolescents in large urban areas. Rural adolescents had lower perceptions of substance use risk and were significantly more likely than urban adolescents to regularly smoke and engage in binge drinking but less likely to use marijuana. Although rural adolescents were more likely than urban teens to report poor/fair health and needing treatment at an ED in the past year, they were less likely to report a major depressive episode. There were also important differences in social factors. Rural adolescents reported significantly lower school connectedness and were less likely to be exposed to school-based or out-of-school prevention education activities or messages. However, rural adolescents reported significantly less peer substance use, stronger importance of religious beliefs, and less residential instability. Finally, rural adolescents were significantly less likely than urban adolescents to report being approached by someone selling drugs in the past 30 days and reported overall lower access to illicit drugs.
Table 2.
Sample Characteristics by Metropolitan Status
| Rural (N=2,747) | Small Urban (N=16,014) | Large Urban (13,275) | Pa | Pb | Pc | ||||
|---|---|---|---|---|---|---|---|---|---|
| Non-medical prescription opioid use (past year) | 6.68 | (.627) | 5.97 | (.250) | 5.29 | (.276) | .269 | .042 | .073 |
| INDIVIDUAL CIRCUMSTANCES | |||||||||
| Demographic Characteristics | |||||||||
| Age | 14.69 | (.044) | 14.62 | (1.839) | 14.65 | (.017) | .166 | .423 | .265 |
| Sex (Female) | 49.08 | (1.336) | 50.22 | (.624) | 48.72 | (.567) | .487 | .800 | .048 |
| Race/Ethnicity | |||||||||
| Non-Hispanic white | 77.07 | (1.691) | 64.91 | (.775) | 48.52 | (.698) | <.001 | <.001 | <.001 |
| Non-Hispanic black | 9.27 | (1.304) | 10.94 | (.579) | 15.82 | (.476) | .217 | <.001 | <.001 |
| Hispanic | 8.17 | (1.176) | 17.24 | (.711) | 25.59 | (.575) | <.001 | <.001 | <.001 |
| Other Race | 5.49 | (.670) | 6.91 | (.283) | 10.07 | (.355) | .052 | <.001 | <.001 |
| Number of people in household | 4.25 | (.040) | 4.31 | (.013) | 4.32 | (.014) | .151 | .067 | .452 |
| Socioeconomic Status | |||||||||
| Family Income (annual) | |||||||||
| < $20,000 | 21.12 | (1.451) | 16.79 | (.474) | 15.91 | (.483) | .004 | .002 | .158 |
| $20,000 < $40,000 | 23.93 | (1.336) | 21.22 | (.504) | 18.82 | (.489) | .043 | .001 | <.001 |
| $40,000 < $75,000 | 34.61 | (1.288) | 28.19 | (.518) | 25.06 | (.651) | <.001 | <.001 | <.001 |
| ≥ $75,000 | 20.34 | (1.206) | 33.79 | (.738) | 40.22 | (.705) | <.001 | <.001 | <.001 |
| Family receives public assistance | 24.39 | (1.429) | 22.13 | (.643) | 19.88 | (.489) | .119 | .005 | .007 |
| Adolescent has health insurance | 91.57 | (.947) | 93.51 | (.338) | 93.69 | (.347) | .072 | .036 | .719 |
| Delinquency and Substance Use History | |||||||||
| Ever been arrested and booked | 6.22 | (.569) | 5.24 | (.231) | 5.93 | (.262) | .104 | .611 | .065 |
| Committed crime past year | 20.37 | (1.080) | 18.96 | (.426) | 18.95 | (.441) | .213 | .215 | .988 |
| Perceived substance use risk index (higher score=greater risk) | 25.88 | (.162) | 26.20 | (.055) | 26.20 | (.060) | .074 | .088 | .959 |
| Regular cigarette smoker (avg. 1+ cig per day) | 8.28 | (.712) | 6.07 | (.283) | 4.48 | (.204) | .005 | <.001 | <.001 |
| Binge drinking in past year | 9.97 | (.851) | 7.29 | (.243) | 7.15 | (.266) | .002 | .004 | .724 |
| Marijuana use in past year | 12.40 | (.925) | 14.24 | (.411) | 14.45 | (.303) | .066 | .031 | .679 |
| Illicit drug use in past year (except marijuana) | 5.66 | (.631) | 5.04 | (.251) | 5.46 | (.273) | .363 | .778 | .246 |
| Misuse of non-opioid medications in past-year | 3.24 | (.468) | 2.86 | (.166) | 2.95 | (.184) | .461 | .543 | .671 |
| Clinical Characteristics | |||||||||
| Poor/fair self-rated health | 4.56 | (.458) | 3.66 | (.231) | 3.34 | (.167) | .063 | .012 | .280 |
| Major depressive episode in past year | 7.61 | (.776) | 9.28 | (.324) | 9.13 | (.345) | .059 | .082 | .746 |
| Physician diagnosed anxiety in past year | 2.66 | (.391) | 3.06 | (.181) | 2.39 | (.160) | .350 | .490 | .011 |
| Treated in ER at least once in past year | 36.03 | (1.353) | 32.19 | (.528) | 29.75 | (.472) | .002 | <.001 | <.001 |
| Overnight hosp. for emotional prob. in past year | 2.09 | (.297) | 1.76 | (.130) | 1.58 | (.135) | .310 | .098 | .332 |
| SOCIAL FACTORS | |||||||||
| Both parents living in household | 70.14 | (1.316) | 69.36 | (.467) | 70.69 | (.531) | .566 | .697 | .057 |
| Parent involvement index (higher score=more involvement) | 14.34 | (.108) | 14.41 | (.043) | 14.46 | (.046) | .534 | .299 | .320 |
| Parent disapproval toward substance use index (higher score=greater disapproval) | 7.46 | (.043) | 7.49 | (.014) | 7.51 | (.016) | .466 | .206 | .314 |
| School connectedness index (higher score=stronger connection) | 9.73 | (.104) | 10.05 | (.040) | 10.13 | (.041) | .008 | <.001 | .096 |
| School, comm., faith-based act. in past year | 93.03 | (.812) | 93.39 | (.226) | 94.21 | (.312) | .674 | .153 | .050 |
| School-based prev. classes/activities in past year | 68.19 | (1.373) | 70.91 | (.546) | 71.96 | (.505) | .083 | .011 | .136 |
| Peer substance use index (higher score=greater peer substance use) | 3.55 | (.072) | 3.92 | (.028) | 3.95 | (.035) | <.001 | <.001 | .548 |
| Friends’ disapproval toward substance use index (higher score=greater disapproval) | 6.11 | (.083) | 6.07 | (.028) | 6.06 | (.032) | .615 | .539 | .807 |
| Religious service attendance in past year | |||||||||
| ≤ 2 times | 44.58 | (1.410) | 45.73 | (.643) | 47.08 | (.669) | .466 | .115 | .137 |
| 3 ≤ 24 times | 19.83 | (.915) | 20.76 | (.433) | 23.02 | (.501) | .401 | .004 | <.001 |
| ≥ 25 times | 35.58 | (1.389) | 33.51 | (.639) | 29.91 | (.518) | .205 | <.001 | <.001 |
| Religious beliefs importance index (higher score=more imp) | 5.34 | (.078) | 5.00 | (.028) | 4.79 | (.027) | <.001 | <.001 | <.001 |
| Lack of social/emotional support | 4.30 | (.703) | 3.48 | (.197) | 4.04 | (.253) | .283 | .720 | .089 |
| Moved in past 5 years | 39.89 | (1.538) | 45.89 | (.530) | 44.15 | (.620) | <.001 | .016 | .033 |
| COMMUNITY AND ENVIRONMENTAL INFLUENCES | |||||||||
| App. by person selling illicit drugs, past 30 days | 9.65 | (.770) | 12.83 | (.381) | 15.20 | (.445) | <.001 | <.001 | <.001 |
| Illicit drug access index (higher score=greater access) | 5.92 | (.136) | 6.54 | (.061) | 6.63 | (.063) | <.001 | <.001 | 0.260 |
| Part. non-school prev./counseling past year | 37.65 | (1.394) | 36.28 | (.563) | 36.12 | (.592) | .346 | .335 | .853 |
| Exposed to non-school drug/alcohol prevention messages past year | 72.26 | (1.174) | 76.12 | (.427) | 77.10 | (.379) | .003 | <.001 | .087 |
N=32,036; percentages/means and standard errors reported; weighted
P value for adjusted Wald test of difference between rural and small urban; 2-tailed tests
P value for adjusted Wald test of difference between rural and large urban; 2-tailed tests
P value for adjusted Wald test of difference between small urban and large urban; 2-tailed tests
Results from unadjusted binary logistic regression models are presented in the first column of Table 3. Adolescents in large urban areas have 22% lower odds of POM relative to rural adolescents (Unadjusted Odds Ratio [UOR] = 0.78, P = .026). The difference between small urban and rural adolescents was not statistically significant (UOR = 0.89, P = .261). When large urban is the referent, rural adolescents have 28% greater odds of POM (UOR = 1.28, P = .026), and small urban adolescents have 14% greater odds of POM, but that difference is only marginally significant (UOR = 1.14, P = .078).
Table 3.
Odds Ratios and 95% Confidence Intervals From Binary Logistic Regression Models Predicting Past-Year POM
| Unadjusted Models | Fully Adjusted Model | Excluding Other Substance Use | |||||||
|---|---|---|---|---|---|---|---|---|---|
| UOR | 95% CI | P | AOR | 95% CI | P | AOR | 95% CI | P | |
| Metropolitan Status (rural=ref) | |||||||||
| Small Urban | 0.888 | (0.721–1.094) | .261 | 0.898 | (0.694–1.161) | .408 | 0.877 | (0.699–1.100) | .254 |
| Large Urban | 0.782 | (0.629–0.971) | .026 | 0.742 | (0.571–0.963) | .025 | 0.758 | (0.604–0.950) | .017 |
| INDIVIDUAL CIRCUMSTANCES | |||||||||
| Demographic Characteristics | |||||||||
| Age | 1.378 | (1.323–1.434) | <.001 | 1.024 | (0.963–1.088) | .449 | 1.109 | (1.050–1.172) | <.001 |
| Sex (Female) | 1.137 | (1.005–1.286) | .041 | 1.180 | (1.016–1.371) | .030 | 1.313 | (1.137–1.517) | <.001 |
| Race/Ethnicity (white=ref) | |||||||||
| Non-Hispanic black | 0.937 | (0.781–1.124) | .481 | 1.272 | (1.038–1.559) | .021 | 0.858 | (0.699–1.053) | .141 |
| Hispanic | 0.945 | (0.790–1.131) | .535 | 1.015 | (0.798–1.293) | .900 | 0.855 | (0.699–1.060) | .152 |
| Other Race | 0.641 | (0.467–0.881) | .007 | 0.780 | (0.571–1.065) | .117 | 0.733 | (0.536–1.002) | .051 |
| Number of people in household | 0.924 | (0.068–0.983) | .013 | 1.031 | (0.957–1.112) | .420 | 1.015 | (0.948–1.086) | .675 |
| Socioeconomic Status | |||||||||
| Family Income (annual) (> $75,000=ref) | |||||||||
| < $20,000 | 1.590 | (1.347–1.977) | <.001 | 1.082 | (0.802–1.460) | .604 | 1.030 | (0.787–1.348) | .829 |
| $20,000 < $40,000 | 1.478 | (1.259–1.735) | <.001 | 1.077 | (0.846–1.371) | .543 | 1.078 | (0.876–1.327) | .475 |
| $40,000 < $75,000 | 1.320 | (1.117–1.560) | .001 | 1.092 | (0.883–1.350) | .413 | 1.107 | (0.915–1.339) | .293 |
| Family receives public assistance | 1.313 | (1.150–1.499) | <.001 | 0.984 | (0.792–1.223) | .883 | 0.994 | (0.816–1.211) | .952 |
| Has health insurance | 0.775 | (0.593–1.012) | .061 | 0.937 | (0.661–1.330) | .714 | 0.942 | (0.680–1.305) | .717 |
| Delinquency and other Substance Use | |||||||||
| Ever been arrested and booked | 5.056 | (4.224–6.051) | <.001 | 1.202 | (0.950–1.521) | .123 | 1.703 | (1.369–2.118) | <.001 |
| Criminal behavior in past year | 4.738 | (4.151–5.409) | <.001 | 1.761 | (1.484–2.090) | <.001 | 2.321 | (1.978–2.723) | <.001 |
| Perceived substance use risk | 0.923 | (0.914–0.931) | <.001 | 0.979 | (0.965–0.993) | .005 | 0.953 | (0.942–0.965) | <.001 |
| Smokes avg. of 1+ cig/day | 11.130 | (9.429–13.139) | <.001 | 1.521 | (1.197–1.933) | .001 | ----- | ----- | ----- |
| Binge drinker in past year | 7.743 | (6.551–9.153) | <.001 | 1.445 | (1.142–1.829) | .002 | ----- | ----- | ----- |
| Marijuana use in past year | 10.548 | (9.334–11.919) | <.001 | 2.462 | (2.022–2.999) | <.001 | ----- | ----- | ----- |
| Illicit drug use in past year | 13.528 | (11.48–15.94) | <.001 | 2.224 | (1.770–2.793) | <.001 | ----- | ----- | ----- |
| Misuse of non-opioid medications in past-year | 36.560 | (29.83–44.80) | <.001 | 6.992 | (5.598–8.733) | <.001 | ----- | ----- | ----- |
| Clinical Characteristics | |||||||||
| Poor/fair self-rated health | 2.118 | (1.619–2.771) | <.001 | 1.299 | (0.925–1.826) | .130 | 1.302 | (0.952–1.779) | .098 |
| Depressive episode past year | 3.036 | (2.589–3.560) | <.001 | 1.469 | (1.191–1.812) | <.001 | 1.615 | (1.332–1.959) | <.001 |
| Anxiety in past year | 3.690 | (2.957–4.605) | <.001 | 0.967 | (0.698–1.338) | .838 | 1.311 | (1.021–1.684) | .034 |
| Treated in ER in past year | 1.703 | (1.503–1.930) | <.001 | 1.259 | (1.068–1.485) | .007 | 1.210 | (1.046–1.401) | .011 |
| Hospitalized for emotional treatment in past year | 3.713 | (2.688–5.130) | <.001 | 1.480 | (1.009–2.172) | .045 | 1.566 | (1.087–2.257) | .017 |
| SOCIAL FACTORS | |||||||||
| Both parents living in household | 0.688 | (0.595–0.796) | <.001 | 0.953 | (0.770–1.180) | .658 | 0.934 | (0.762–1.144) | .507 |
| Parenting involvement index | 0.891 | (0.877–0.905) | <.001 | 0.985 | (0.964–1.006) | .165 | 0.981 | (0.963–1.000) | .051 |
| Parents’ attitudes toward substance use index | 0.743 | (0.721–0.764) | <.001 | 0.970 | (0.932–1.010) | .135 | 0.916 | (0.887–0.947) | <.001 |
| School connectedness index | 0.926 | (0.914–0.939) | <.001 | 1.005 | (0.983–1.029) | .643 | 1.006 | (0.985–1.027) | .578 |
| Participation in school, comm, faith-based act. in past year | 0.550 | (0.445–0.681) | <.001 | 1.360 | (0.993–1.861) | .055 | 1.092 | (0.848–1.407) | .492 |
| School-based prevention classes or activities in past year | 0.784 | (0.677–0.909) | .001 | 0.921 | (0.770–1.101) | .361 | 0.940 | (0.793–1.114) | .471 |
| Peer substance use index | 1.322 | (1.282–1.362) | <.001 | 1.055 | (1.013–1.099) | .010 | 1.077 | (1.040–1.116) | <.001 |
| Friends’ attitudes toward substance use index | 0.755 | (0.739–0.771) | <.001 | 0.978 | (0.948–1.010) | .175 | 0.916 | (0.891–0.943) | <.001 |
| Religious service attendance in past year (≥ 25 times=ref) | |||||||||
| ≤ 2 times | 1.882 | (1.564–2.265) | <.001 | 1.024 | (0.817–1.283) | .837 | 1.078 | (0.867–1.341) | .496 |
| 3 ≤ 24 times | 1.608 | (1.294–1.998) | <.001 | 1.034 | (0.808–1.322) | .790 | 1.150 | (0.908–1.458) | .244 |
| Religious belief importance index | 0.849 | (0.828–0.870) | <.001 | 0.987 | (0.956–1.018) | .396 | 0.971 | (0.944–0.999) | .042 |
| Lack of social/emotional support | 2.414 | (1.896–3.074) | <.001 | 1.139 | (0.816–1.590) | .441 | 1.093 | (0.832–1.435) | .520 |
| Moved in past 5 years | 1.409 | (1.247–1.592) | <.001 | 1.011 | (0.872–1.173) | .881 | 1.044 | (0.902–1.210) | .558 |
| COMMUNITY AND ENVIRONMENTAL INFLUENCES | |||||||||
| Approached by someone selling illicit drugs in past 30 days | 5.605 | (4.860–6.463) | <.001 | 1.114 | (0.916–1.356) | .278 | 1.953 | (1.657–2.302) | <.001 |
| Illicit drug access index | 1.124 | (1.111–1.138) | <.001 | 1.025 | (1.008–1.042) | .005 | 1.034 | (1.019–1.049) | <.001 |
| Participated in prevention/counseling prog past year | 0.966 | (0.848–1.100) | .848 | 1.025 | (0.876–1.198) | .756 | 0.971 | (0.839–1.244) | .695 |
| Exposure to drug/alcohol prevention messages outside of school in past year | 0.835 | (0.706–0.988) | .036 | 0.883 | (0.726–1.074) | .210 | 0.931 | (0.773–1.121) | .448 |
N=32,036; weighted
UOR = Unadjusted Odds Ratio; AOR = Adjusted Odds Ratio; CI = Confidence Interval; 2-tailed tests
Unadjusted models find most predictors to be significantly associated with adolescent POM. Age, being female, low family income, public assistance receipt, delinquency, other substance use, poor physical and mental health, peer substance use, lack of social/emotional support, residential instability, and drug access are all significantly and positively associated with POM. Being “other race” versus white, presence of both parents and more people in one’s household, perceptions of substance use risk, parental involvement, parent and friend disapproval of substance use, school connectedness, participation in school, community or faith-based activities, exposure to prevention activities and messages, and religiosity are all associated with significantly reduced odds of POM.
Results from the fully adjusted model are presented in the middle column of Table 3. Net of multiple individual, social, and community factors, large urban adolescents have 26% lower odds of POM versus rural adolescents (AOR = 0.74, P = .025), but there are not significant differences between small urban and rural adolescents. When large urban is the referent, rural adolescents have 35% greater odds (AOR = 1.35, P = .025) and small urban adolescents have 21% greater odds of POM (AOR = 1.21; P = .021) versus adolescents in large urban areas.
A number of other factors remained significantly associated with POM in the adjusted model. Odds of POM are greater among females (AOR = 1.180); blacks versus whites (AOR = 1.272); and among those who committed a crime (AOR = 1.761), used other substances (especially other medications), experienced a major depressive episode (AOR = 1.469), were treated in the ED (AOR = 1.259), or hospitalized for emotional treatment (AOR = 1.480). Peer substance use (AOR = 1.055) and perceptions of ease of illicit drug access (AOR = 1.025) were also positively associated with POM.
Adolescent age, socioeconomic status (SES), anxiety, parenting factors, school connectedness and prevention activities, friends’ disapproval of substance use, and religious involvement and belief were not associated with POM in the adjusted model. However, changes in the magnitude of the coefficients and elimination of statistical significance for many of these factors were the result of including other substance use variables in the model. When other substance use variables are excluded from the model (see third results column in Table 3), age, being arrested, anxiety, and being approached by someone selling drugs are significantly associated with increased odds of POM, and parent and friend disapproval of substance use and strength of religious beliefs are significantly associated with reduced odds of POM. This change occurs because many of the same characteristics that predict POM also predict use of other substances. Compared to those who are not misusing opioids, adolescents who engage in POM are significantly and substantively more likely to regularly smoke (30.8% vs 3.8%, P < .001), binge drink (32.5% vs 5.9%, P < .001), use marijuana (58.1% vs 11.6%, P < .001), use other illicit drugs (33.6% vs 3.6%, P < .001), and misuse other prescription medications (31.3% vs 1.2%, P < .001).iv As a result, including them as predictors in the regression model masks many of the important factors that increase risk of or buffer against POM.
We present the results from formal mediation analyses in Table 4. Because the rural/small urban difference was not statistically significant in any models, we present only the mediation effects on the rural versus large urban difference. All mediation results are available from the authors upon request. We present results from 3 sets of mediation analyses. The first treats all variables in the table as mediators (ie, the conditions through which rurality may partially operate to influence POM). The second includes other substance use indicators as control variables but does not test them as mediators. The third excludes other substance use indicators from the model altogether for the same reasons discussed above. All 3 models control for the demographic and SES characteristics included in the adjusted model in Table 3.
Table 4.
Results of KHB Mediation Analyses for Large Urban vs Rural Difference in Past-Year Adolescent POM
| Model 1a | Model 2b | Model 3c | ||||
|---|---|---|---|---|---|---|
| A | B | A | B | A | B | |
| Delinquency and other Substance Use | ||||||
| Ever been arrested and booked | 0.48 | −0.16 | 0.51 | −0.07 | 0.82 | −0.68 |
| Criminal behavior in past year | −0.77 | 2.56 | −18.34 | 2.64 | −6.80 | 5.64 |
| Perceived substance use risk index | −6.59 | 2.18 | −15.36 | 2.21 | −8.86 | 7.36 |
| Smokes avg. of at least 1 cigarette per day | −10.16 | 3.36 | ----- | ----- | ----- | ----- |
| Binge drinker in past year | −8.65 | 2.86 | ----- | ----- | ----- | ----- |
| Marijuana use in past year | 44.11 | −14.59 | ----- | ----- | ----- | ----- |
| Illicit drug use in past year | 1.22 | −0.40 | ----- | ----- | ----- | ----- |
| Misuse of non-opioid medications in past-year | 14.05 | −4.65 | ----- | ----- | ----- | ----- |
| Clinical Characteristics | ||||||
| Poor/fair self-rated health | −4.67 | 1.55 | −9.26 | 1.33 | −2.77 | 2.30 |
| Major depressive episode in past year | 12.17 | −4.02 | 22.53 | −3.24 | 8.95 | −7.43 |
| Anxiety in past year | −0.17 | 0.06 | −0.32 | 0.05 | 0.82 | −0.68 |
| Treated in ER at least once in past year | −13.07 | 4.32 | −25.00 | 3.59 | −6.39 | 5.30 |
| Hospitalized for emotional treatment in past year | −1.60 | 0.53 | −3.37 | 0.48 | −1.08 | 0.90 |
| SOCIAL FACTORS | ||||||
| Both parents living in household | 2.63 | −0.87 | 5.13 | −0.74 | 2.22 | −1.84 |
| Parent involvement scale | −0.01 | 0.00 | −0.80 | 0.12 | 0.00 | 0.00 |
| Parents’ attitudes toward substance use index | 1.40 | −0.46 | 2.74 | −0.39 | 2.37 | −1.97 |
| School connectedness index | 1.65 | −0.54 | 3.25 | −0.47 | 1.04 | −0.86 |
| Any participation in school, community, faith-based activities in past year | −0.29 | 0.10 | −0.63 | 0.09 | −0.05 | 0.04 |
| School-based prevention classes or activities in past year | −2.88 | 0.95 | −5.61 | 0.81 | −1.28 | 1.06 |
| Peer substance use index | 32.02 | −10.59 | 60.25 | −8.66 | 26.19 | −21.74 |
| Friends’ attitudes toward substance use index | 4.63 | −1.53 | 6.49 | −0.93 | 10.87 | −9.02 |
| Religious service attendance in past year | ||||||
| ≤ 2 times | 1.36 | −0.45 | 2.61 | −0.38 | 2.58 | −2.14 |
| 3 ≤ 24 times | 1.10 | −0.37 | 2.14 | −0.31 | 2.76 | −2.29 |
| ≥ 25 times (ref) | ||||||
| Religious belief importance index | 11.90 | −3.93 | 22.62 | −3.25 | 15.23 | −12.64 |
| Lack of social/emotional support | −0.73 | 0.24 | −1.75 | 0.25 | −0.30 | 0.25 |
| Moved in past 5 years | 0.91 | −0.30 | 1.77 | −0.25 | 2.09 | −1.73 |
| COMMUNITY AND ENVIRONMENTAL INFLUENCES | ||||||
| Approached by someone selling illicit drugs in past 30 days | 8.93 | −2.95 | 16.29 | −2.34 | 32.77 | −27.20 |
| Illicit drug access index | 24.64 | −8.15 | 46.65 | −6.70 | 20.08 | −16.67 |
| Participated in non-school based prevention or counseling program in past year | −0.95 | 0.31 | −1.86 | 0.27 | 0.67 | −0.55 |
| Exposure to drug/alcohol prevention messages outside of school in past year | −5.68 | 1.88 | −10.68 | 1.53 | −1.92 | 1.60 |
|
| ||||||
| Total Effect | −0.225 | −0.261 | −0.152 | |||
| Direct Effect | −0.299 | −0.299 | −0.278 | |||
| Indirect Effect | 0.074 | 0.038 | 0.126 | |||
Note: All models control for demographic and socioeconomic characteristics from fully adjusted model. A negative value in column A and positive value in column B indicate that including that variable in the model reduces (attenuates) the rural/large urban difference in POM. A positive value in column A and negative value in column B indicate that the inclusion of that variable in the model increases the rural/large urban difference in POM (ie, serves as a suppressor).
Model 1 includes substance use history variables as formal mediators
Model 2 includes substance use history variables as controls, but not mediators
Model 3 excludes substance use history variables
A=percent the mediator contributes to indirect effect of large urban versus rural difference on POM
B=percent of total large urban versus rural difference due to positive/negative confounding of respective mediator
The magnitude of the rural/large urban difference in POM did not dramatically change between the unadjusted and adjusted models in Table 3. Our mediation results suggest this is because positive and negative mediators cancel each other out in their influence in rural/large urban differences in the full model. That is, there are certain individual POM risk factors that are more pronounced among rural adolescents than their large urban peers that explain part of the higher odds of POM among rural adolescents. At the same time, however, there are certain individual, social, and community protective factors that are more pronounced among rural adolescents than their large urban peers that increase the magnitude of the rural/urban difference once they are included in the model (ie, once those conditions are held constant between large urban and rural adolescents). In the interest of space, we will discuss the mediation results only from Model 2.
Most of the mediation effects are quite small.v However, criminal behavior, lower perceived substance use risk, and past-year ED treatment are robust positive mediators; each of these are more likely among rural versus large urban adolescents, and each of these factors are significantly and positively associated with POM. Conversely, past-year major depressive episode, peer substance use, importance of religious beliefs, and drug access are robust negative mediators. Depression, peer substance use, lower scores on the religious importance index, and greater drug access are all associated with greater odds of POM, and rural adolescents are less likely than their large urban peers to report these conditions. Accordingly, these factors serve as buffers against POM among rural adolescents relative to those in large urban areas. Ultimately, these results suggest a complex interplay of concomitantly existing risk and protective factors that influence rural/urban differences in adolescent POM. Moreover, even when accounting for all of these factors, rural adolescents continue to have significantly greater odds of POM relative to adolescents in large urban areas.
Discussion
This study provides the most recent nationally representative examination of rural/urban differences in adolescent past-year POM and is the first to use the social-ecological framework to identify specific individual, social and community characteristics through which rurality indirectly operates to influence POM. In research using the 2008 NSDUH, Havens and colleagues16 found rural adolescents were significantly more likely than adolescents in large urban areas to report lifetime POM. Using the 2011–2012 NSDUH, we found similar rural/large urban differences in past-year POM, suggesting the rural disadvantage has not decreased over time.vi Higher POM among rural adolescents is concerning because of inadequate treatment services in rural areas20 already overwhelmed with increasing treatment demand, long distances to providers, and transportation barriers that are burdensome for accessing regular opioid outpatient treatment.42 In addition to increasing the supply of community-based treatment facilities, innovative programs (eg, Empower for Recovery43) providing home-based intervention and case management services to rural teens and families may help reduce adolescent POM in rural areas.
Our findings demonstrate the importance of considering social and community environment factors, above and beyond adolescents’ own individual circumstances, when examining rural/urban differences in POM. Results of formal mediation analyses suggest that although rural adolescents are partially buffered by distinctive features of rural life (less peer substance use, less access to illicit drugs), they are simultaneously at increased risk of POM relative to their large urban peers due at least partly to more criminal involvement, less risky attitudes about substance use, and higher ED utilization. To mitigate these risk factors, intervention efforts should focus on greater use of family drug courts to link teen criminal offenders to prevention and treatment services, better education on the highly addictive nature and consequences of POM, and increased access to standard (non-emergency) health services to reduce rural residents’ reliance on EDs44 where opioid prescribing is more prevalent.45
Despite lower availability of illicit drugs in rural versus urban areas, rural adolescents have greater prevalence of POM, suggesting they may be obtaining prescription opioids through legitimate means (ie, the health care system). In supplemental analyses (available from the authors upon request), we found the most common source for prescription opioids among adolescents (67%) was friends or family. This finding is consistent with other studies46,47 and suggests the need for interventions aimed at educating teens and parents about safeguarding their medication and more opportunities for safe disposal/return of unused prescriptions. However, in our analyses, rural adolescents were significantly less likely than urban adolescents to obtain opioids from friends or family (rural=62%; small urban=69%; large urban=67%) and significantly more likely than urban adolescents to obtain opioids from physicians (rural=23%; small urban=17%; large urban=19%). This is consistent with studies showing rural physicians prescribe opioids more liberally than their urban counterparts,45 suggesting provider-level interventions might be one route for reducing rural POM. We also found that rural adolescents are twice as likely as urban adolescents to obtain opioids from a dealer (rural=9%; small urban=2%; large urban=5%). This finding is not that surprising given recent journalistic accounts of increases in opiate drug trafficking in rural areas,48 but empirical research on rural prescription trafficking is sparse. Studies similar to ones conducted on urban prescription dealers15 could help illuminate how rural adolescents come into contact with dealers.
Consistent with findings from other studies,10,49–54 we also found past-year use of other substances are among the strongest predictors of POM. About half of prescription painkiller deaths involve the use of other substances.55 The positive association between age and POM, and research showing that age of first substance use is associated with greater odds of POM among adults,53,54 suggests the need for prevention efforts targeting early poly-substance abuse among all spatial groups. Our results suggest many of the same factors that increase risk of POM also increase risk of using other substances. Researchers should be aware that when they include other substance use variables in regression models, they are potentially masking the significance of many of the factors contributing to POM, including older age, being arrested, parent and friend disapproval of substance use, and strength of religious beliefs, because other substances serve as confounders in the associations between these factors and POM. From a policy standpoint, given that parents’ and friends’ attitudes toward teen substance use appear to influence both adolescent POM and use of other substances, parents and peers provide important points of intervention for reducing adolescent POM.
An important contribution of this paper is that whereas most research on rural/urban differences in adolescent POM combines small and large urban areas into one category (except Havens et al16), we examined metropolitan status as a trichotomy. This revealed that whereas rural adolescents have significantly greater odds of POM than their peers in large urban areas, there are no significant differences between adolescents in small urban versus rural areas. Adolescents in small urban areas, however, do have marginally greater odds of POM than those in large urban areas, net of individual, social, and community factors. Future research should explore how variation in contextual characteristics between large and small urban areas explains this finding. Unfortunately, the public-use NSDUH does not enable us to categorize respondents along a finer rural/urban continuum. “Rural” and “urban” represent heterogeneous geographic units where many outlying residents of an urban area may experience life that is more “rural” in character than residents living in a city center. In addition, because suburban areas are included in both small and large CBSAs, our results cannot speak to whether or how suburban POM differs from rural or urban POM.
Despite including a myriad of individual, social, and community factors, we were unable to account for the residual greater odds of POM among rural versus large urban adolescents. Differences in prescriber behaviors, types of employment (eg, manual labor), historical/cultural differences, overall community economic disadvantage, and other contextual characteristics unavailable from the data may explain the rural disparity.20 Because prescription drug misuse has historically been an embedded part of the culture in some of the most remote rural areas of the US,56,57 qualitative research exploring perceptions of painkiller risk among rural adolescents may help inform rural intervention strategies. Moreover, data sets that include geographic identifiers would enable merging contextual- and individual-level data to present a more nuanced portrait of the multilevel and multidimensional risk factors for adolescent POM.
Our results should be interpreted within the context of additional limitations. First, the NSDUH is a household sample of the non-institutionalized population and may not represent adolescents not permanently attached to one household, including adolescents in substance abuse treatment and juvenile detention. Second, the cross-sectional data prohibit us from establishing causality. Third, the data are self-reported and may be subject to under-reporting due to recall and/or social desirability bias. Fourth, the variable assessing adolescents’ experiences of being approached by someone selling drugs is measured on a 30-day recall whereas our outcome is based on past-year use. Finally, the wording of the opioid misuse variable in the NSDUH (“use without a prescription from a doctor or use for the feeling or experience it causes”) does not allow us to disentangle the different types of use or motivations for use.
Despite these limitations, our findings encourage researchers, policy makers, and treatment providers to consider the complex ways in which individual, social, and community factors simultaneously increase risk of and buffer against POM in rural versus urban areas. Future research should identify whether the relationships between POM and the characteristics we considered vary spatially, and whether the rural/urban differences found here are more pronounced among different groups of adolescents (eg, low income, racial/ethnic minority) or different classes of controlled medications.
Acknowledgments
Funding: Dr. Monnat acknowledges support from the Population Research Institute at Penn State which receives core funding from the National Institute of Child Health and Human Development (Grant R24-HD041025). Dr. Monnat is also a current grantee (2014–2016) with the Robert Wood Johnson Foundation New Connections Junior Investigators Program.
Footnotes
In 2011 and 2012, the weighted screening response rates were 87.0% and 86.1%, respectively, and the weighted interview response rates were 74.4% and 73.0%, respectively. For information on how annual screening and interview response rates are calculated, please see the NSDUH documentation.37,38
Core based statistical areas are associated with at least one urbanized area with a population of at least 50,000, plus adjacent/outlying counties that have substantial social and economic integration with the central city containing the core area as measured by commuting patterns. For more information on how CBSAs are defined, see Census documentation.39 We use the terms “large urban,” “small urban,” and “rural” throughout the paper.
The introduction of positive mediators/confounders to the model results in the reduction of rural/urban differences in POM while the introduction of suppressors (negative mediators/confounders) to the model results in an increase in the magnitude of the rural/urban difference in POM.
Significance tests are from unadjusted Wald tests of mean differences.
The KHB method ensures that the coefficients are measured on the same scale and thus are not affected by scale mismatch issues.
We also conducted the same regression models substituting “lifetime” POM as the dependent variable. We did not present those results in this paper due to space constraints, but they are available from the authors upon request. Results were consistent with those of “past-year” POM, except that rural/large urban differences were even larger for “lifetime” POM than they were for “past-year” POM (large urban vs rural AOR = 0.647, P < .001).
Disclosures: Everyone who has contributed to this study has been acknowledged herein. The authors do not have any potential, perceived, or real conflicts of interests. No honorarium, grant, or other form of payment was given to anyone to produce this article. Funders played no role in the study design, collection, analysis, or interpretation of the data or the decision to submit this article for publication.
References
- 1.Dart RC, Surratt HL, Cicero TJ, et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372(3):241–248. doi: 10.1056/NEJMsa1406143. [DOI] [PubMed] [Google Scholar]
- 2.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011;12(4):657–667. doi: 10.1111/j.1526-4637.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. [Accessed June 23, 2015];Policy Impact: Prescription Painkiller Overdoses. 2011 Available from: http://www.cdc.gov/HomeandRecreationalSafety/pdf/PolicyImpact-PrescriptionPainkillerOD.pdf.
- 4.Sung HE, Richter L, Vaughan R, Johnson PB, Thom B. Nonmedical use of prescription opioids among teenagers in the United States: trends and correlates. J Adolesc Health. 2006;37(1):44–51. doi: 10.1016/j.jadohealth.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 5.National Institute on Drug Abuse. [Accessed June 24, 2015];Table: National Survey on Drug Use and Health: Trends in Prevalence of Various Drugs for Ages 12 or Older, Ages 12 to 17, Ages 18 to 25, and Ages 26 or Older; 2011–2013 (in percent) Available from: www.drugabuse.gov/national-survey-drug-use-health.
- 6.Fortuna RJ, Robbins BW, Caiola E, et al. Prescribing of controlled medications to adolescents and young adults in the United States. Pediatr. 2010;126:1108–1116. doi: 10.1542/peds.2010-0791. [DOI] [PubMed] [Google Scholar]
- 7.Kandel DB, Logan JA. Patterns of drug use from adolescence to young adulthood: periods of risk for initiation, continued use, and discontinuation. Am J Public Health. 1984;74(7):660–666. doi: 10.2105/ajph.74.7.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCabe SE, West BT, Morales M, et al. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction. 2007;102:1920–1930. doi: 10.1111/j.1360-0443.2007.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rigg KK, Murphy JW. Understanding the etiology of prescription opioid abuse: Implications for prevention and treatment. Qual Health Res. 2013;23(7):963–975. doi: 10.1177/1049732313488837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young AM, Glover N, Havens JR. Nonmedical use of prescription medications among adolescents in the United States: a systematic review. J Adolesc Health. 2012;51(1):6–17. doi: 10.1016/j.jadohealth.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Hays LR. A profile of OxyContin addiction. J Addict Dis. 2004;23(4):1–9. doi: 10.1300/J069v23n04_01. [DOI] [PubMed] [Google Scholar]
- 12.Florida Office of Attorney General. [Accessed December 30, 2014];Florida’s Prescription Drug Diversion and Abuse Roadmap, 2012–2015. 2012 Available from: http://myfloridalegal.com/webfiles.nsf/wf/kgrg-8t8l5k/$file/Prescriptiondrugdiversionandabuseroadmap.pdf.
- 13.New York City Mayor’s Office. [Accessed June 23, 2015];Mayor’s Task Force on Prescription Painkiller Abuse: Interim Report. 2013 Available from: http://www.nyc.gov/html/cjc/downloads/pdf/rx_stat_september_2013_report.pdf.
- 14.Havens JR, Talbert JC, Walker R, Leedham C, Leukefeld CG. Trends in controlled-release oxycodone (Oxycontin®) prescribing among Medicaid recipients in Kentucky, 1998–2002. J Rural Health. 2006;22(3):276–278. doi: 10.1111/j.1748-0361.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 15.Rigg KK, Kurtz SP, Surratt HL. Patterns of prescription medication diversion among drug dealers. Drugs: Educ Prev Polic. 2012;19(2):145–155. doi: 10.3109/09687637.2011.631197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Havens JR, Young AM, Havens CE. Nonmedical prescription drug use in a nationally representative sample of adolescents: evidence of greater use among rural adolescents. JAMA Pediatr. 2011;165(3):250–255. doi: 10.1001/archpediatrics.2010.217. [DOI] [PubMed] [Google Scholar]
- 17.Wu L, Pilowsky DJ, Patkar AA. Non-prescribed use of pain relievers among adolescents in the United States. Drug Alcohol Depend. 2008;94:1–11. doi: 10.1016/j.drugalcdep.2007.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ford J. Nonmedical prescription drug use among adolescents: the influence of bonds to family and school. Youth Soc. 2009;40:336–352. [Google Scholar]
- 19.McCauley JL, Danielson CK, Amstadter AB, et al. The role of traumatic event history in non-medical use of prescription drugs among a nationally representative sample of U.S. adolescents. J Child Psychol Psychiatry. 2010;51(1):84–93. doi: 10.1111/j.1469-7610.2009.02134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dew B, Elifson K, Dozier M. Social and environmental factors and their influence on drug use vulnerability and resiliency in rural populations. J Rural Health. 2007;23(s1):16–21. doi: 10.1111/j.1748-0361.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 21.Park R. Suggestions for the investigations of human behaviors in the urban environment. Am J Sociol. 1916:577–612. [Google Scholar]
- 22.Brooks-Gunn J, Duncan GJ, Klebanov PK, Sealand N. Do neighborhoods influence child and adolescent development. Am J Sociol. 1993;99(2):353–395. [Google Scholar]
- 23.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing ‘neighborhood effects’: social processes and new directions in research. Annu Rev Sociol. 2002:443–478. [Google Scholar]
- 24.Raudenbush SW, Sampson RJ. ‘Ecometrics’: toward a science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociol Methodol. 1999;29:1–41. [Google Scholar]
- 25.Earls F, Carlson M. The social ecology of child health and well-being. Ann Rev Publ Health. 2001:143–66. doi: 10.1146/annurev.publhealth.22.1.143. [DOI] [PubMed] [Google Scholar]
- 26.Lichter DT, Graefe DR. Rural economic restructuring: implications for children, youth, and families. In: Smith KE, Tickamyer AR, editors. Economic Restructuring and Family Well-Being in Rural America. University Park, PA: Penn State University Press; 2011. pp. 25–39. [Google Scholar]
- 27.Sherman J. Those Who Work, Those Who Don’t: Poverty, Mobility, and Family in Rural America. Minneapolis, MN: University of Minnesota Press; 2009. [Google Scholar]
- 28.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13(10):988–996. doi: 10.1016/j.jpain.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United States Department of Agriculture. Rural America at a Glance, 2014 edition. Washington, DC: Economic Research Service; 2014. p. 26. [Google Scholar]
- 30.Brown EJ, Waite CD. Perceptions of risk and resiliency factors associated with rural African American adolescents’ substance abuse and HIV behaviors. J Am Psychiatr Nurses Assoc. 2005;11:88–100. [Google Scholar]
- 31.De Haan L, Trageton L. Relationships between substance abuse information and use prevalence and attitudes. Adolesc Fam Health. 2001;2:55–62. [Google Scholar]
- 32.Stylianou S. The role of religiosity in the opposition to drug use. Int J Offender Ther Comp Criminology. 2004;45:429–448. doi: 10.1177/0306624X03261253. [DOI] [PubMed] [Google Scholar]
- 33.Paige LZ, Kitzis SN, Wolfe J. Rural underpinnings for resiliency and linkages: a safe schools/healthy students project. Psychol Sch. 2003;40:531–547. [Google Scholar]
- 34.Schoeneberger ML, Leukefeld CG, Hiller ML, Godlaski T. Substance abuse among rural and very rural drug users at treatment entry. Am J Drug Alcohol Abuse. 2006;32:87–110. doi: 10.1080/00952990500328687. [DOI] [PubMed] [Google Scholar]
- 35.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health (NSDUH) Series. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [Accessed June 14, 2014]. Updated May 19, 2014. Available from: http://www.icpsr.umich.edu/icpsrweb/ICPSR/series/00064. [Google Scholar]
- 36.Substance Abuse and Mental Health Services Administration. [Accessed December 30, 2014];Substance Abuse & Mental Health Data Archive: How to combine NSDUH public-use file data and its use? Updated March, 2013. Available from: http://www.icpsr.umich.edu/icpsrweb/SAMHDA/support/faqs/2014/03/how-to-combine-nsduh-public-use-file.
- 37.Substance Abuse & Mental Health Data Archive. [Accessed June 23, 2015];National Survey on Drug Use and Health, 2012: Documentation. Available from: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34933.
- 38.Substance Abuse & Mental Health Data Archive. [Accessed June 23, 2015];National Survey on Drug Use and Health, 2011: Documentation. Available from: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/34481.
- 39.United States Census Bureau. Geographic Terms and Concepts - Core Based Statistical Areas and Related Statistical Areas. Washington, DC: 2012. [Accessed June 20, 2015]. Available from: http://www.census.gov/geo/reference/gtc/gtc_cbsa.html. [Google Scholar]
- 40.Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models. Stata J. 2011;11(3):420–438. [Google Scholar]
- 41.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppressor effect. Prev Sci. 2000;1(4):173. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roberton EB, Donnermeyer JF. Illegal drug use among rural adults: mental health consequences and treatment utilization. Am J Drug Alcohol Abuse. 1997;23:467–484. doi: 10.3109/00952999709016890. [DOI] [PubMed] [Google Scholar]
- 43.Rohlfs DK. US Department of Health and Human Services, editor. The National Rural Alcohol and Drug Abuse Network Awards for Excellence 2004, Technical Assistance Publication Series 28. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment; 2006. [Accessed June 23, 2015]. Empower for Recovery: an innovative approach to assist sustained recovery in rural Iowa. Available from: http://lib.adai.washington.edu/clearinghouse/downloads/TAP-28-The-National-Rural-Alcohol-and-Drug-Abuse-Network-Awards-for-Excellence-2004-119.pdf#page=25. [Google Scholar]
- 44.Haggerty JL, Roberge D, Lévesque JF, Gauthier J, Loignon C. An exploration of rural–urban differences in healthcare-seeking trajectories: Implications for measures of accessibility. Health Place. 2014;28:92–98. doi: 10.1016/j.healthplace.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Hoppe JA, Nelson LS, Perrone J, Weiner SG. Opioid prescribing in a cross section of US emergency departments. [Accessed June 25, 2015];Ann Emerg Med. 2015 doi: 10.1016/j.annemergmed.2015.03.026. (epub ahead of print) Available from: http://www.ncbi.nlm.nih.gov/pubmed/25952503. [DOI] [PMC free article] [PubMed]
- 46.Boyd CJ, McCabe SE, Cranford JA, Young A. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. JAMA Pediatr. 2007;161(3):276–281. doi: 10.1001/archpedi.161.3.276. [DOI] [PubMed] [Google Scholar]
- 47.McCabe SE, Boyd CJ. Sources of prescription drug for illicit use. Addict Behav. 2005;30(7):1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quinones S. Dreamland: The True Tale of America’s Opiate Epidemic. New York, NY: Bloomsbury Press; 2015. [Google Scholar]
- 49.Ford JA, Rigg KK. Racial/ethnic differences in factors that place adolescents at risk for prescription opioid misuse. Prev Sci. 2015;16(5):633–641. doi: 10.1007/s11121-014-0514-y. [DOI] [PubMed] [Google Scholar]
- 50.Fiellin LE, Tetrault JM, Becker, et al. Previous use of alcohol, cigarettes, and marijuana and subsequent abuse of prescription opioids in young adults. J Adolesc Health. 2013;52(2):158–163. doi: 10.1016/j.jadohealth.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Havens JR, Stoops WW, Leukefeld CG, et al. Prescription opiate misuse among rural stimulant users in a multistate community-based study. Am J Drug Alcohol Abuse. 2009;35:18–23. doi: 10.1080/00952990802326298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCabe SE, West BT, Teter CJ, Boyd CJ. Medical and nonmedical use of prescription opioids among high school seniors in the United States. JAMA Pediatr. 2012;166:797–802. doi: 10.1001/archpediatrics.2012.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang KH, Becker WC, Fiellin DA. Prevalence and correlates for nonmedical use of prescription opioids among urban and rural residents. Drug Alcohol Depend. 2013;127:156–62. doi: 10.1016/j.drugalcdep.2012.06.027. [DOI] [PubMed] [Google Scholar]
- 54.Rigg KK, Monnat SM. Urban vs. rural differences in prescription opioid misuse among adults in the United States: Informing region specific drug policies and interventions. Int J Drug Policy. 2015;26:484–491. doi: 10.1016/j.drugpo.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Warner M, Chen LH, Makuc DM. [Accessed June 23, 2015];Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. 2009 Available from: http://www.cdc.gov/nchs/data/databriefs/db22.pdf. [PubMed]
- 56.Keyes KM, Cerda M, Brady JE, Havens JR, Galea S. Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014;104:e52–59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leukefeld CG, Walker R, Havens JR, Leedham VT. What does the community say: key informant perceptions of rural prescription drug use. J Drug Issues. 2007;37(3):503–524. [Google Scholar]