Abstract
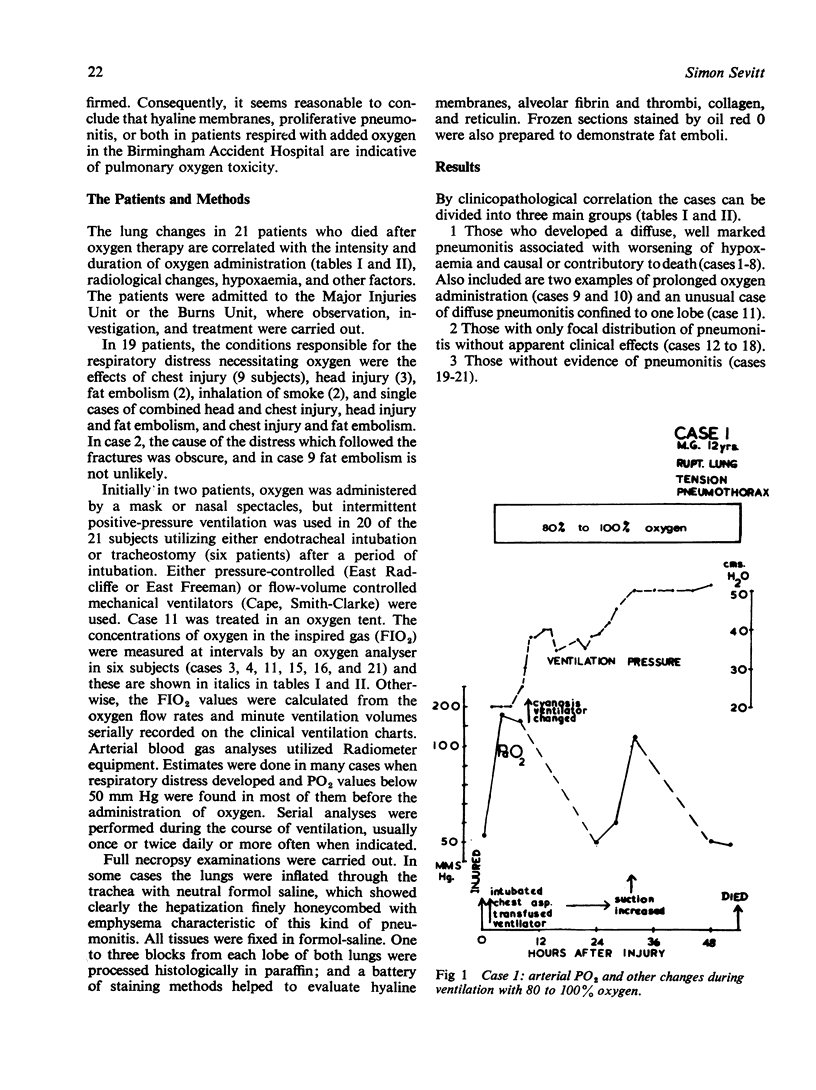
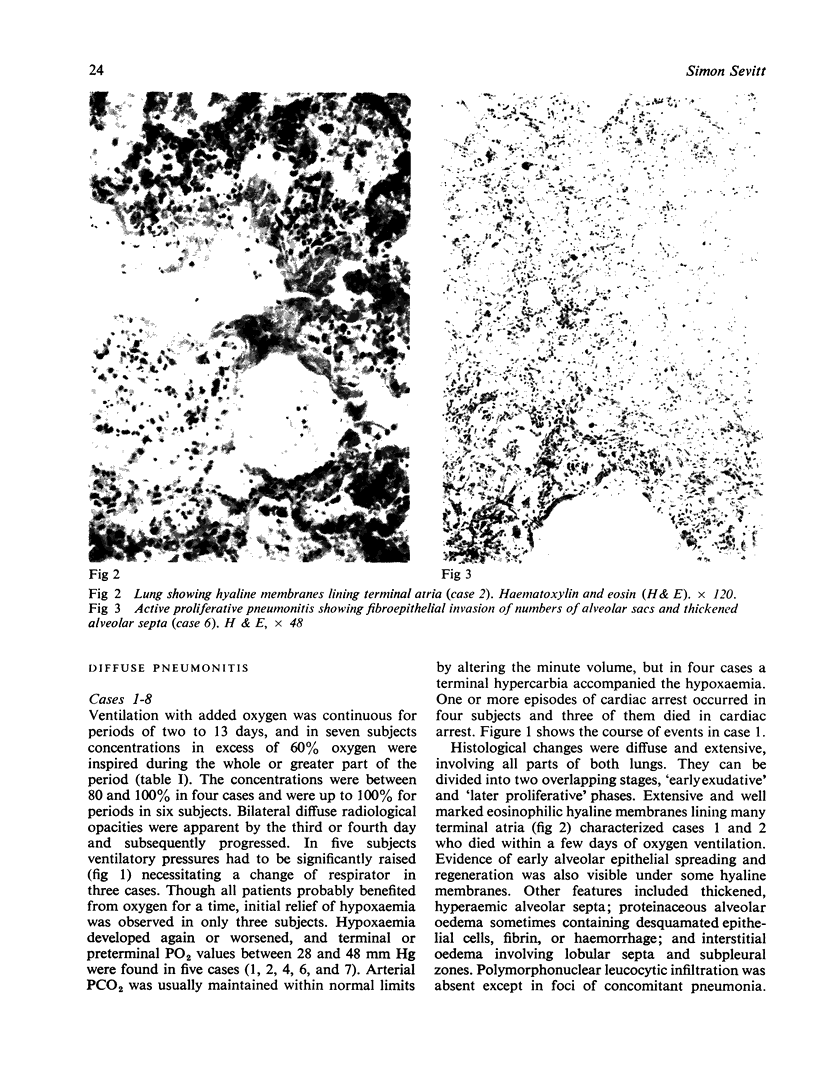
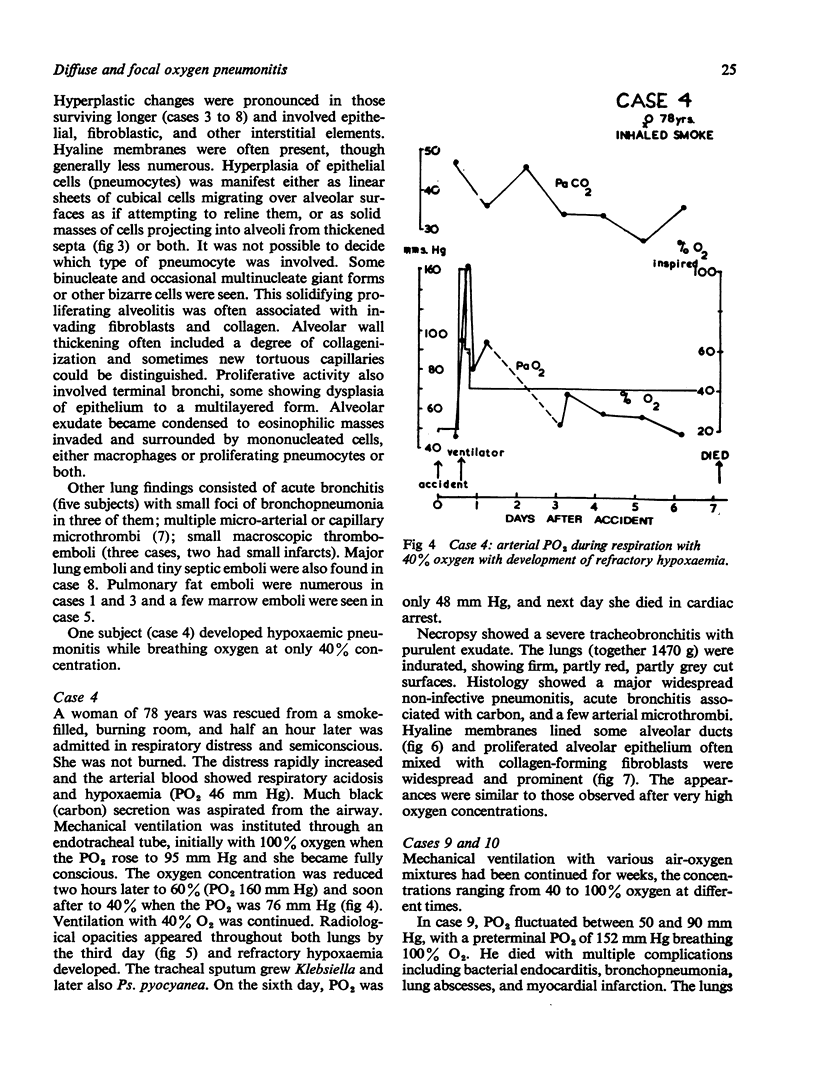
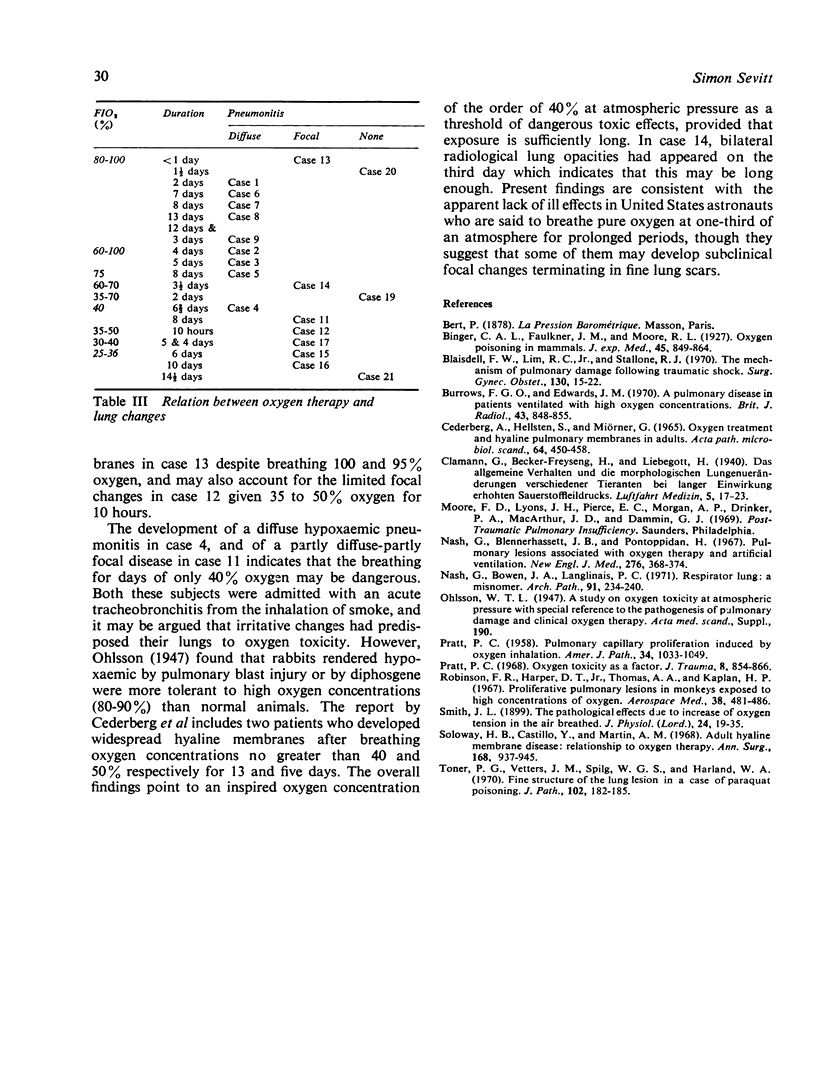
Utilizing hyaline membranes and proliferative pneumonitis as evidence of pulmonary oxygen toxicity, the lung changes in 21 patients (19 injured, two inhaled smoke) who died after oxygen therapy are correlated with the intensity and duration of oxygen administration. Diffuse pneumonitis inducing hypoxaemia was found in 10 (or 11) subjects, and in nine of them it was associated with the breathing of high concentrations of oxygen (60 to 100%) for at least two days. In at least eight subjects the pneumonitis contributed to death, and two others who survived for weeks had extensively fibrosed lungs. The breathing of 40% oxygen for a sufficient time seems to be a threshold for dangerous lung effects, since one patient developed a diffuse pneumonitis and another a partly-diffuse partly-focal pneumonitis while exposed to this concentration. Those respiring oxygen concentrations between 25 and 40% for days developed either subclinical focal lung lesions or had no relevant lung changes.
Full text
PDF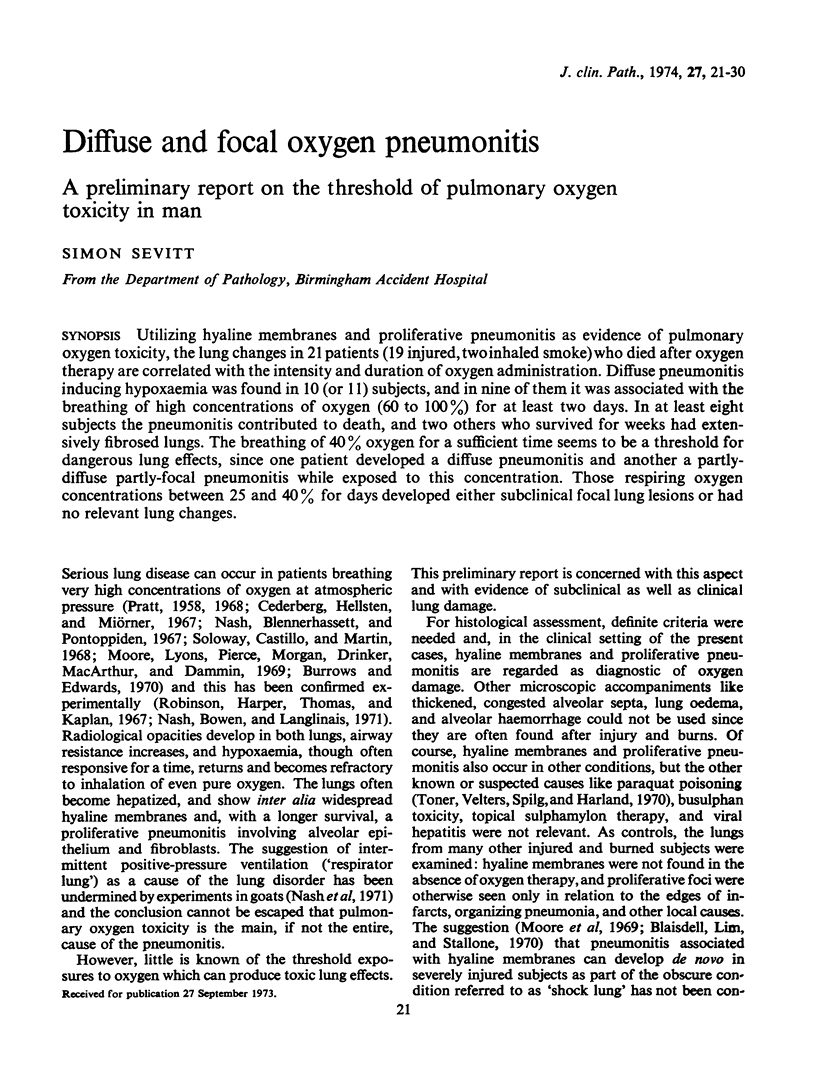

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blaisdell F. W., Stallone R. J. The mechanism of pulmonary damage following traumatic shock. Surg Gynecol Obstet. 1970 Jan;130(1):15–22. [PubMed] [Google Scholar]
- Burrows F. G., Edwards J. M. A pulmonary disease in patients ventilated with high oxygen concentrations. Br J Radiol. 1970 Dec;43(516):848–855. doi: 10.1259/0007-1285-43-516-848. [DOI] [PubMed] [Google Scholar]
- Cederberg A., Hellsten S., Miörner G. Oxygen treatment and hyaline pulmonary membranes in adults. Acta Pathol Microbiol Scand. 1965;64(4):450–458. doi: 10.1111/apm.1965.64.4.450. [DOI] [PubMed] [Google Scholar]
- Nash G., Blennerhassett J. B., Pontoppidan H. Pulmonary lesions associated with oxygen therapy and artifical ventilation. N Engl J Med. 1967 Feb 16;276(7):368–374. doi: 10.1056/NEJM196702162760702. [DOI] [PubMed] [Google Scholar]
- Nash G., Bowen J. A., Langlinais P. C. "Respirator lung": a misnomer. Arch Pathol. 1971 Mar;91(3):234–240. [PubMed] [Google Scholar]
- PRATT P. C. Pulmonary capillary proliferation induced by oxygen inhalation. Am J Pathol. 1958 Nov-Dec;34(6):1033–1049. [PMC free article] [PubMed] [Google Scholar]
- Pratt P. C. Oxygen toxicity as a factor. J Trauma. 1968 Sep;8(5):854–866. doi: 10.1097/00005373-196809000-00033. [DOI] [PubMed] [Google Scholar]
- Robinson F. R., Harper D. T., Jr, Thomas A. A., Kaplan H. P. Proliferative pulmonary lesions in monkeys exposed to high concentrations of oxygen. Aerosp Med. 1967 May;38(5):481–486. [PubMed] [Google Scholar]
- Soloway H. B., Castillo Y., Martin A. M., Jr Adult hyaline membrane disese: relationship to oxygen therapy. Ann Surg. 1968 Dec;168(6):937–945. doi: 10.1097/00000658-196812000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toner P. G., Vetters J. M., Spilg W. G., Harland W. A. Fine structure of the lung lesion in a case of paraquat poisoning. J Pathol. 1970 Nov;102(3):182–185. doi: 10.1002/path.1711020311. [DOI] [PubMed] [Google Scholar]