Abstract
It has long been recognized that an increase of reactive oxygen species (ROS) can modify the cell-signaling proteins and have functional consequences, which successively mediate pathological processes such as atherosclerosis, diabetes, unchecked growth, neurodegeneration, inflammation, and aging. While numerous articles have demonstrated the impacts of ROS on various signaling pathways and clarify the mechanism of action of cell-signaling proteins, their influence on the level of intracellular ROS, and their complex interactions among multiple ROS associated signaling pathways, the systemic summary is necessary. In this review paper, we particularly focus on the pattern of the generation and homeostasis of intracellular ROS, the mechanisms and targets of ROS impacting on cell-signaling proteins (NF-κB, MAPKs, Keap1-Nrf2-ARE, and PI3K-Akt), ion channels and transporters (Ca2+ and mPTP), and modifying protein kinase and Ubiquitination/Proteasome System.
1. Introduction
Reactive oxygen species (ROS), generated through a variety of extracellular and intracellular actions, have drawn attention as novel signal mediators which are involved in growth, differentiation, progression, and death of the cell [1, 2]. As a group of chemical species that include at least one oxygen atom in each molecule but display stronger reactivity than molecular oxygen, ROS comprise free radicals such as superoxide, hydroxyl radical, and singlet oxygen, as well as nonradical species such as hydrogen peroxide formed by the partial reduction of oxygen [3–5]. Oxygen free radicals are highly reactive and have the capacity to damage cellular components such as proteins, lipids, and nucleic acids. Classically, ROS were regarded as host defending molecule released by neutrophil for destructing exogenous pathogens such as bacteria; however, accumulated evidence indicates that ROS play central roles in determination of cell fate as second messengers and modifying of various signaling molecules [6–9].
It has been demonstrated that ROS have impacts on several signaling pathways and the mechanisms of how ROS act on cell-signaling proteins, how the cell-signaling proteins influence the level of intracellular ROS in turn, and if there are complex interactions between different ROS associated signaling pathways have been clarified, but the systemic summary is necessary. In this review, we focus on the pattern of the generation and homeostasis of intracellular ROS, the mechanisms and targets of ROS impacting on cell-signaling proteins, ion channels and transporters, and modifying kinases and Ubiquitination/Proteasome System.
2. The Homeostasis of ROS
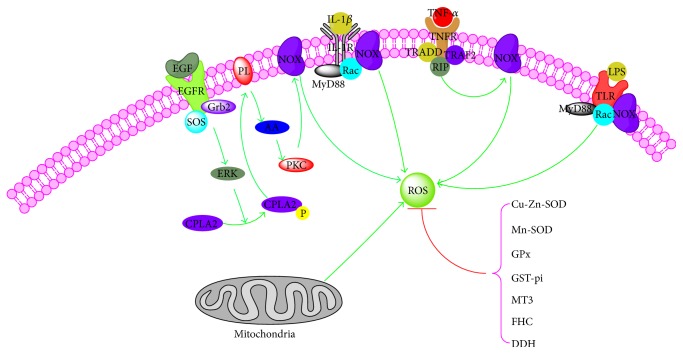
Under a physiological state, the level of cellular ROS is stable in a dynamic equilibrium, and this balance is modulated by cellular processes that produce ROS and eliminate them (Figure 1).
Figure 1.
Homeostasis of intracellular reactive oxygen species. NOX, NADPH oxidases; TNF-α, tumor necrosis factor-α; EGF, epidermal growth factor; IL-1β, Interleukin-1β; SOD, superoxide dismutase; GPx, glutathione peroxidase; GST-pi, glutathione S-transferase pi; MT3, metallothionein-3; FHC, ferritin heavy chain; DDH1, dihydrodiol dehydrogenase; TNFR, tumor necrosis factor receptor; TRADD, TNFRSF1A-associated via death domain; MyD88, myeloid differentiation factor 88; TLR, Toll-like receptor; cPLA2, cytosolic phospholipases A2.
The resource of cellular ROS could be broadly divided into two main categories: firstly, there are those biological processes, mainly the mitochondrial oxidative metabolism, that release ROS as a byproduct, or a waste product, of various other necessary reactions and, secondly, there are those processes, in cellular response to xenobiotics, cytokines, and bacterial invasion, that generate ROS intentionally, either in molecular synthesis or in breakdown, as part of a signal transduction pathway, or as part of a cell defense mechanism [10–12]. The initial product of the mitochondrial respiratory chain is O2 −∙ mainly generated by complexes I and III and could be quickly transformed into H2O2 by the enzyme superoxide dismutase (SOD) and then could be reduced to water by catalase or glutathione peroxidase [13–16]. NADPH oxidases (Nox) including Nox1 to Nox5 and Duox1 and Duox2, which are classified into three groups, according to the presence of domains in addition to the gp91phox (NOX2) domain, are another important source of cellular ROS [17, 18]: NOX1, NOX3, and NOX4 are similar in size and domain structure to NOX2, catalyzing the NADPH-dependent reduction of oxygen to form superoxide, which can react with itself to form H2O2; NOX5 is slightly different in domain structure to NOX2 but with similar process of superoxide formation; Duox1 and Duox2 contain a peroxidase-homology domain, utilizing ROS generated by the catalytic core to generate more powerful oxidant species that then oxidize extracellular substrates [19]. Meanwhile, external stimuli including tumor necrosis factor-α (TNF-α), epidermal growth factor (EGF), Interleukin-1β (IL-1β), and hypoxia and irradiation also stimulate the formation of ROS [20–24].
And, as a critical role to withstand the excessive formation of intracellular ROS, series of antioxidant proteins have been found. The main category of these antioxidant proteins is superoxide dismutases (SOD) which contain Cu-Zn-SOD (SOD1) and Mn-SOD (SOD2) [25]. SOD2, in the matrix, converts superoxide, which cannot diffuse across membranes, to H2O2 which then is reduced to water by catalase. Compared to SOD2, SOD1 mainly reduces the superoxide of intermembrane space and cytosol to H2O2. Besides, glutathione peroxidase (GPx), glutathione S-transferase pi (GST-pi), metallothionein-3 (MT3), ferritin heavy chain (FHC), and dihydrodiol dehydrogenase (DDH1 or AKR1C1) and so on also play decisive roles in the process of antioxidant [26–29].
3. ROS and NF-κB Signaling Pathway
The transcription factor NF-κB is crucial in a series of cellular processes, including immune, inflammatory response, cellular adhesion, differentiation, proliferation, autophagy, senescence, and apoptosis [30]. Likewise, the disorder of NF-κB has already been confirmed to be associated with cancer, arthritis, inflammation, asthma, neurodegenerative diseases, and heart disease [31]. The family of NF-κB consists of Rel (c-Rel), RelA (p65), RelB, p50/p105 (NF-κB1), and p52/p100 (NF-κB2). NF-κB pathway may be activated by at least two distinct pathways named the canonical and noncanonical pathways. The canonical NF-κB-activating pathway is triggered in response to microbial products, stress, and proinflammatory cytokines and it depends on the phosphorylation of IκB-kinase (IKK) β and the phosphorylation and ubiquitination of IκBa and its degradation by the proteasome, and then NF-κB translocates into the nucleus where it activates the transcription of target genes [32–34]. In contrast, the noncanonical NF-κB-activating pathway is activated by B-cell activating factor (BAFF) [35], lymphotoxin β (LTβ) [36], CD40 ligand [37], CD27 ligand [38], human T-cell leukemia virus (HTLV) [39], and Epstein-Barr virus (EBV) [40] and it relies on IKKα and causes activation of NF-κB2/RelB complexes by inducing the proteolytic processing of the NF-κB2/p100 precursor.
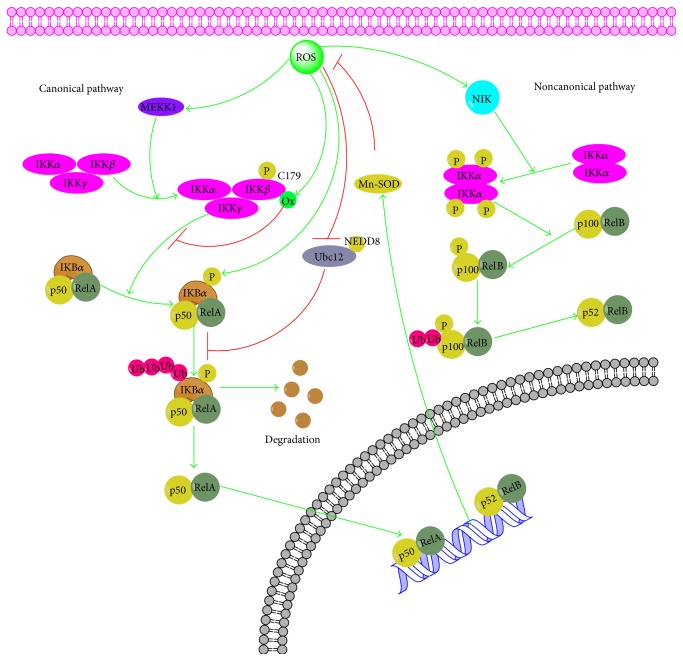
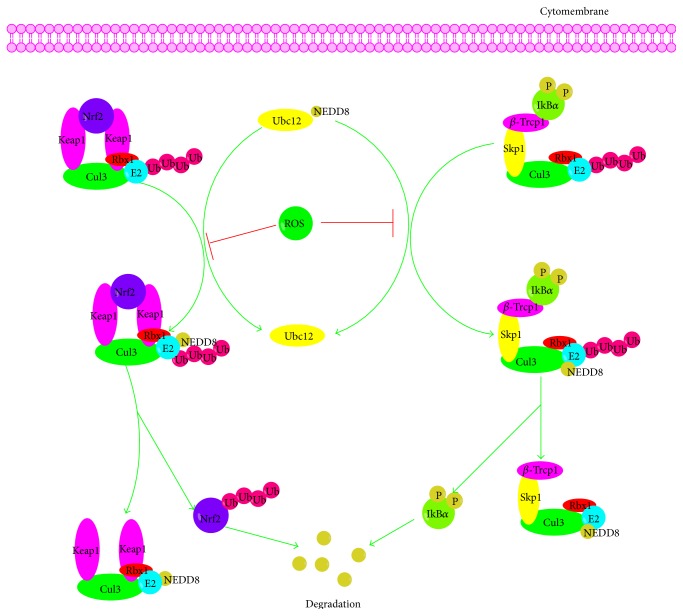
Recently, cumulative evidence has indicated that there is an interrelation between ROS and NF-κB. Firstly, ROS influence the activation of NF-κB pathway mainly by inhibiting the phosphorylation of IκBα. A series of studies has testified that IκBα is usually phosphorylated on serines 32 and 36 by IKK leading to its ubiquitination and degradation and exogenously added H2O2 affects the phosphorylation of IκBα on Tyr42 or other tyrosine residues and subsequent degradation of IκBα and activation of NF-κB pathway [41, 42]. In addition, IKK is also the primary target for ROS in influencing NF-κB and the S-glutathionylation of IKKβ on cysteine 179 by ROS results in the inhibition of IKKβ activity [43]. Then, MEKK1, the kinases upstream of IKK, may be potentially regulated by ROS. MEKK1 is a redox-sensitive kinase that could be glutathionylated at C1238 leading to its inactivation [44]. Thirdly, ROS also could disturb the ubiquitination and degradation of IκB and then the activation of NF-κB by inactivating Ubc12. Furthermore, NIK, the upstream kinase in the noncanonical pathway, is believed to be activated by ROS through inhibition of phosphatases and oxidation of cysteine residues [45, 46]. Meanwhile, NF-κB pathway also can influence the ROS levels by increasing expression of antioxidant proteins such as Cu-Zn-SOD, Mn-SOD, GPx, GST-pi, MT3, and FHC (Figure 2).
Figure 2.
Cross talk between ROS and NF-κB signaling pathway. MEKK1, mitogen-activated protein kinase kinase kinase 1; PKC, protein kinase C; NIK, NF-κB inducing kinase; NEDD8, neural precursor cell expressed developmentally downregulated 8.
4. ROS and MAPKs Signaling Pathway
The mitogen-activated protein kinase (MAPK) cascades, consisting of the extracellular signal-related kinases (ERK1/2), the c-Jun N-terminal kinases (JNK), the p38 kinase (p38), and the big MAP kinase 1 (BMK1/ERK5) pathway [47], are major intracellular signal transduction pathways that play an important role in various cellular processes such as cell growth, differentiation, development, cell cycle, survival, and cell death [48]. Similarly, ERK, JNK, p38, and BMK1 are all serine/threonine kinases that are directed by a proline residue. Along with the pathways in which these four MAP kinases are activated share similarity by extracellular or intracellular stimuli, a MAP kinase kinase kinase (MAPKKK) is activated and then phosphorylating and activating a MAP kinase kinase (MAPKK) and the MAPKK phosphorylating and activating a MAP kinase (MAPK) and activated MAPKs phosphorylate various substrate proteins, resulting in regulation of various cellular activities [49–51].
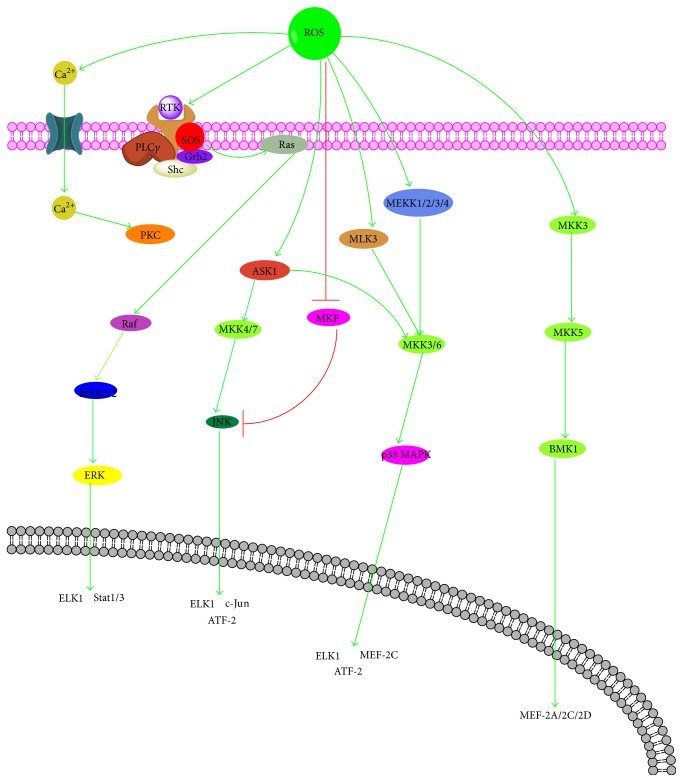
The ERK pathway is activated mainly by growth factors (epidermal growth factor, EGF, and platelet-derived growth factor, PDGF) and cytokines (IL-1β and TNF-α), and its activation is related to the stimulation of tyrosine kinase receptors [52, 53]. When these receptors of growth factors and cytokines are bound with their ligands, the GDP bound Ras is converted to GTP that in turn activates Ras. Subsequently activated Ras recruits cytoplasmic Raf (MAPKKK) to the cell membrane for activation. Activated Raf phosphorylates MEK1/2 (MAPKK), which then phosphorylates ERK1/2 (MAPK) that translocate to the nucleus and activates several transcription factors [54, 55]. ROS have been shown to activate the receptors of EGF and PDGF, though without corresponding ligands, which can stimulate Ras and the subsequent activation of ERK pathway [56, 57]. In addition, it has been demonstrated that ROS generated by commensal bacteria inactivated dual-specific phosphatase 3 (DUSP3) by oxidation on Cys-124 results in ERK activation [58]. Meanwhile, in some cells, treatment with H2O2 leads to the phosphorylation and activation of phospholipase C- (PLC-) gamma which results in the generation of inositol trisphosphate (IP3) and diacylglycerol (DAG) [59]. IP3 could increase the intracellular calcium by inducing the release of calcium from intracellular stores that can mediate activation of ERK pathway and generation of DAG and increases in intracellular calcium which results in the activation of several forms of protein kinase C (PKC) leading to Ras and Raf activation [60, 61].
The JNK pathway is activated by environmental stress (oxidative stress) and cytokines (tumor necrosis factor, TNF, and FAS) and involves a kinase cascade similar to the ERK pathway with a MAPKKK activating a MAPKK and the MAPKK subsequently phosphorylating JNK on critical threonine and tyrosine residues resulting in the activation of JNK; afterwards JNK translocate to the nucleus and regulate the activity of multiple transcription factors. The MAPKKK in JNK pathway includes MEKK1, MEKK2, MEKK3, and MEKK4, MLK, and ASK1 and MAPKK contain MKK4, MKK3, MKK6, and MKK7 [62, 63]. ROS could act on TRX and glutaredoxin, a kind of redox-sensitive proteins, to dissociate from ASK-1 for its activation, resulting in the activation of JNK [64]. Also, ROS could trigger the detachment of JNK from glutathione S-transferase pi (GSTp), which can interact with JNK to suppress its activation, thereby facilitating JNK activation [65]. ROS could be able to allow ASK1 to be oligomerized and autophosphorylated and become activated by oxidizing thioredoxin, which inhibits the activation of ASK1 via binding to the N-terminal of ASK1 [66]. TNF receptor-associated JNK activation is thought to be mediated in part by oxygen radicals because superoxide anion and lipid peroxide-scavengers inhibit JNK activation. Furthermore, it is possible that low levels of ROS intermediates leave phosphatase activity intact, leading to a transient activation of JNK. Higher levels of ROS may activate JNK pathway and inactivate the phosphatases resulting in a prolonged activation of JNK (Figure 3).
Figure 3.
Cross talk between ROS and MAPKs signaling pathway. MAPK, mitogen-activated protein kinase; ERK, extracellular signal-related kinases; JNK, c-Jun N-terminal kinases; p38, p38 kinase; BMK1/ERK5, big MAP kinase 1; MAPKKK, MAP kinase kinase kinase; MAPKK, MAP kinase kinase; MAPK, MAP kinase; PLC, phospholipase C; IP3, inositol trisphosphate; DAG, diacylglycerol.
The p38 pathway is activated by extracellular stresses, growth factor, and cytokines, such as tumor necrosis factor-a (TNF-a) and IL-1β. The TNF receptors switch on the p38 pathway via the activation of cdc42, whereas growth factor receptors switch on the p38 pathway by the sequential activation of Ras and Rac1 [67]. Small G-proteins Rac1 and cdc42 activate ASK1, MLK3, and MLK3 that directly activate MKK3 and MKK6 which phosphorylates p38 on both tyrosine and threonine residue resulting in the activation of p38 pathway [68, 69]. Some initial proteins, such as ASK-1, in the JNK pathway, are also involved in the activation of the p38 pathway. Oxidative stress directly or indirectly affects ASK1, MEKK1, MEKK2, MEKK3, MEKK4, and MLK3 and subsequently activates p38 pathway (Figure 3).
The BMK1 (also known as ERK5) pathway, which has been involved in cell survival, antiapoptotic signaling, angiogenesis, cell motility, differentiation, and cell proliferation, is one of the least studied members of the MAPK family [70]. Oxidative stress (H2O2) could influence BMK1 pathway by activating MEKK2 and MEKK3 directly. Then MEK5 and BMK1 are activated sequentially and BMK1 acts on its downstream targets including Mef2C, c-Myc, and possibly Nrf2 (Figure 3).
5. ROS and Keap1-Nrf2-ARE Signaling Pathway
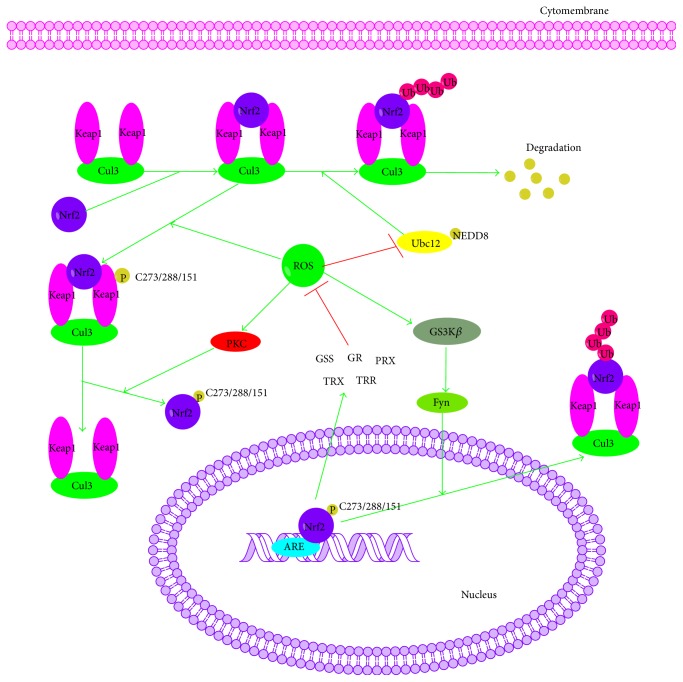
Another signaling pathway, Keap1-Nrf2-ARE, performs critical role in maintaining the cellular redox balance and metabolism and inducing an adaptive response for oxidative stress that can otherwise lead to many inflammatory diseases including cancer, Alzheimer's disease (AD), Parkinson's disease (PD), and diabetes. This pathway consists of three main cellular components: Kelch-like ECH-associated protein 1 (Keap1), nuclear factor erythroid 2-related factor 2 (Nrf2), and antioxidant response elements (ARE) [71–76]. Under normal physiological conditions, Keap1, which is also called an inhibitor of Nrf2 (INrf2), is associated with Nrf2 (the majority of which resides in the cytoplasm) and recruits and interacts with the cullin-3 E3-ubiquitin ligase (Cul3) [77]. And the ubiquitination of Nrf2 is stimulated that targeted Nrf2 for degradation by the 26S proteasome (more related information has been provided in “ROS and Ubiquitination/Proteasome System” section) [78].
However, under oxidizing conditions, the increased level of intracellular ROS promotes the dissociation of Nrf2 and Keap1, either by the oxidization of key reactive cysteine residues (Cys273, Cys288, and Cys151) that govern Keap1 activity or via the activation of kinases, such as protein kinase C (PKC), MAPK, phosphatidylinositide 3-kinases (PI3Ks), and protein kinase-like endoplasmic reticulum kinase (PERK) that phosphorylate Nrf2 [79–81]. After that the dissociated Nrf2 is transferred to the nucleus where it dimerizes with members of another b-zip family, the small Maf proteins (Maf-F, Maf-G, and Maf-K), binds to ARE of phase II genes, and translates detoxification enzymes such as glutathione synthetase (GSS), glutathione reductase (GR), Gpx, thioredoxin (TRX), thioredoxin reductase (TRR), and peroxiredoxin (PRX) to prevent the oxidative stress [73, 82]. Meanwhile, oxidative stress activates GSK3β leading to nuclear import of Src kinases such as Src, Yes, Fyn, and Fgr, which phosphorylates Nrf2 (Tyr568) followed by the nuclear export with Keap1 and degradation of Nrf2 [83, 84] (Figure 4).
Figure 4.
Cross talk between ROS and Keap1-Nrf2-ARE signaling pathway. Keap1, Kelch-like ECH-associated protein 1; Nrf2, nuclear factor erythroid 2-related factor 2; ARE, antioxidant response elements; Cul3, cullin-3 E3-ubiquitin ligase; GSK3β, glycogen synthase kinase 3; Ubc, E2-ubiquitin conjugating enzyme.
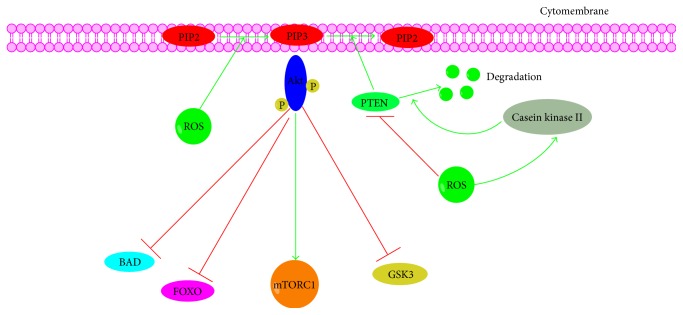
6. ROS and PI3K-Akt Signaling Pathway
The phosphoinositide-3-kinase- (PI3K-) Akt pathway has been involved in many critical cellular functions, including protein synthesis, cell cycle progression, proliferation, apoptosis, autophagy, and drug resistance in response to growth factor (EGF, PDGF, NGF, and VEGF), hormone (prostaglandin, PGE2), and cytokine (IL-17, IL-6, and IL-2) stimulation [85–87]. The binding of growth factor to its receptors directly stimulates class 1A PI3Ks bound via their regulatory subunit or adapter molecules such as the insulin receptor substrate (IRS) proteins, which subsequently triggers the activation of PI3K. Afterwards, the activated PI3K catalyzes the synthesis of phosphatidylinositol 3,4,5-triphosphate (PIP3), from phosphatidylinositol 4,5-bisphosphate (PIP2) [88]. The membranal PIP3, a signaling molecule, recruits and activates proteins that contain the pleckstrin homology (PH) domain such as the phosphoinositide-dependent protein kinase (PDK) and protein kinase B (Akt) serine/threonine kinases and the activation of PDK and Akt successively promotes the activation and transcription of their target genes (GSK3, FOXO, BAD, mTOR1, and p53) [89–92].
ROS not only activate PI3K directly to amplify its downstream signaling but also concurrently inactivate phosphatase and tensin homolog (PTEN), which negatively regulates the synthesis of PIP3 and thereby inhibits the activation of Akt, via oxidizing cysteine residues within the active center [93]. In addition, ROS is able to promote the phosphorylation by casein kinase II on PTEN which urges PTEN to enter the proteolytic degradation pathway [93]. Furthermore, protein phosphatase 2A (PP2A), which might be deactivated by ROS, could inhibit Akt/PKB. However, it seems that, at lower levels, ROS oxidize the disulfide bridges in Akt/PKB, leading to the association of Akt/PKB with PP2A and thus short-term activation of Akt/PKB [46, 94, 95] (Figure 5).
Figure 5.
Cross talk between ROS and PI3K-Akt signaling pathway. PI3K, phosphoinositide-3-kinase; Akt, protein kinase B; PTEN, phosphatase and tensin homolog; FOXO, forkhead box protein O; mTOR1, mechanistic target of rapamycin 1.
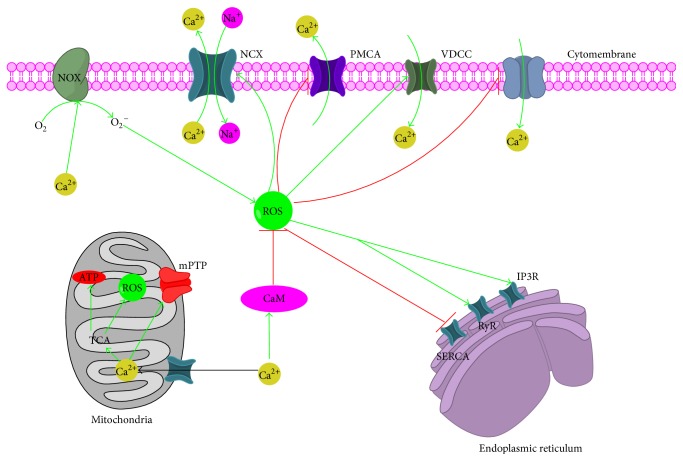
7. Cross Talk between ROS and Ca2+
In eukaryotic cells, Ca2+ is one of the most versatile signals involved in the control cellular processes and functions, such as contraction, secretion, metabolism, gene expression, cell survival, and cell death [96, 97]. Cytosolic Ca2+ concentration ([Ca2+]c) is determined by a dynamic balance between the mechanisms that pour Ca2+ into the cytoplasm, including Ca2+ influx from the extracellular medium and intracellular stores such as endoplasmic reticulum (ER) or sarcoplasmic reticulum (SR), and those processes that remove it out, involving Ca2+ efflux across the plasma membrane and sequestration into mitochondria [98, 99]. The uptake mechanisms of Ca2+ into the cytoplasm refer to the inositol 1,4,5-trisphosphate receptor (IP3R), the ryanodine receptor (RyR), and the nicotinic acid-adenine dinucleotide phosphate (NAADP) that are responsible for Ca2+ release from ER and SR, as well as voltage-dependent Ca2+ channels (VDCC) and store-operated Ca2+ channel (SOC), which are in charge of Ca2+ influx from extracellular matrix [100–102]. Meanwhile, the mechanisms of removing Ca2+ are determined by the plasma membrane Ca2+ ATPase (PMCA), which mediates Ca2+ extrusion across the plasma membrane into the cytoplasm, the sarcoplasmic/endoplasmic reticulum Ca2+ ATPase (SERCA), which reintroduces Ca2+ into the ER/SR, Na+/Ca2+ exchanger (NCX) that involves the clearance of Ca2+ through its exchange by Na+, and the mitochondrial Ca2+ uniporter (MCU) that transports Ca2+ into the mitochondria [103, 104]. Recent studies have demonstrated that the ROS and Ca2+ signaling systems influence each other in various ways (Figure 6).
Figure 6.
Cross talk between ROS and Ca2+. IP3R, inositol 1,4,5-trisphosphate receptor; RyR, the ryanodine receptor; VDCC, voltage-dependent Ca2+ channels; SOC, store-operated Ca2+ channel; SERCA, sarcoplasmic/endoplasmic reticulum Ca2+ ATPase; PMCA, plasma membrane Ca2+ ATPase; MCU, mitochondrial Ca2+ uniporter; TCA cycle, tricarboxylic acid cycle; NCX, Na+/ Ca2+ exchanger.
Numerous evidences indicate that intracellular Ca2+ modulates both ROS generation and ROS clearance processes and thereby shift the redox state to either more oxidized or reduced state. The primary role of Ca2+ is the promotion of ATP synthesis and ROS generation in mitochondria via stimulating the Krebs cycle enzymes and oxidative phosphorylation [105]. The mitochondrial respiratory chain provides the main source of physiological ROS production (O2 −∙), which is either converted to H2O2 by spontaneous dismutation or catalyzed by SOD. Mitochondrial Ca2+ could activate three dehydrogenases of the TCA cycle (pyruvate dehydrogenase, isocitrate dehydrogenase, and oxoglutarate dehydrogenase), the ATP synthase (complex V), and the adenine nucleotide translocase and then increase the generation of ROS [106–108]. Along with that, Ca2+ regulates multiple extramitochondrial ROS generating enzymes, including NOX [109] and nitric oxide synthase (NOS) [110], both in physiological and in pathological processes. Meanwhile, Ca2+ modulates ROS clearance processes via regulating the antioxidant defense system: on one hand, Ca2+ can directly activate antioxidant enzymes (catalase and GSH reductase), increase the level of SOD, and induce mitochondrial GSH release early in Ca2+-induced mitochondrial permeability transition pore (mPTP) opening; on the other hand, calmodulin (CaM), ubiquitous Ca2+-binding protein, could activate catalases in the presence of Ca2+ and downregulates H2O2 levels [111–113].
Furthermore, ROS also influences Ca2+ signaling via oxidizing Cys thiol of Ca2+ channels/pumps/exchangers involving RyR, IP3R, SERCA, PMCA, and NCX. RyR/IP3R, as well as many of the regulatory proteins that form complex with the RyR/IP3R, contains multiple reactive Cys thiols that influence channel gating or assembly [114]. Thiol oxidation of RyR/IP3R by ROS in general increases channel activity and thereby promotes Ca2+ efflux via enhancing intersubunit binding and preventing the binding of the negative regulator calmodulin to the receptor [115]. As with RyR/IP3R, SERCA pumps also contain numerous free Cys residues which are oxidized by ROS in the context of oxidation state which inhibits the activity of SERCA and decreases Ca2+ influx from the cytoplasm to ER [116]. Additionally, although PMCA is a slower pump than SERCA, it can be reversibly inactivated by ROS by altering the Tyr589, Met622, and Met831 residues [117]. And ROS both stimulate and decrease NCX activity: H2O2 generated from the xanthine/xanthine oxidase system enhances NCX activity and oxidants from hypoxanthine/xanthine oxidase depress NCX activity. Moreover, ROS also alter the activity of VDCC, especially the activity of L-type Ca2+ channels, which has been associated with the oxidation of -SH groups resulting in altered Ca2+ entry in the cytoplasm [118].
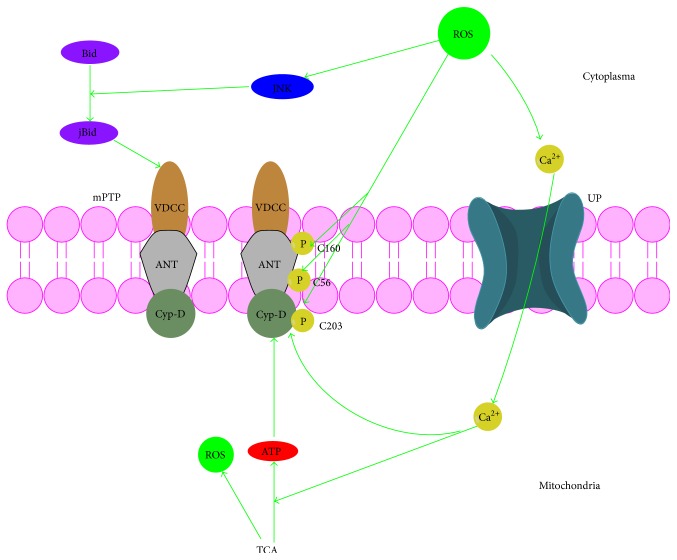
8. ROS and mPTP
Several studies, lasting for decades, have showed that mPTP, a large, nonspecific channel spanning the inner mitochondrial membrane (IMM) and outer mitochondrial membrane (OMM) [119, 120], mediates the lethal permeability changes that initiate mitochondrial-driven death. Hitherto, the putative components include the voltage-dependent anion channel (VDAC) or porin, localized in the OMM; the adenine nucleotide translocator (ANT) in the IMM; the peripheral benzodiazepine receptor and the Bcl-2 family proteins; the hexokinase bound to porin; the cyclophilin-D (Cyp-D), a regulatory element in the matrix; glycogen synthase kinase-3b (GSK-3b); and cytochrome c [121–123]. It has been described that when mPTP opens by the activation of various signals, mitochondrial permeability is changed which dissipates the proton electrochemical gradient (ΔΨm), which drives multiple mitochondrial functions, leading to ATP depletion, further reactive oxygen species production, and ultimately swelling and rupture of the organelle. This in turn releases proapoptotic proteins: cytochrome c (Cyt C) [124] binds to apoptotic protease activating factor-1 (Apaf1) and then forms apoptosome that activates the caspase-9 and caspase-3 protease system and induces apoptosis, Smac/DIABLO [125] activates caspases by sequestering caspase-inhibitory proteins, and endonuclease-G (endoG) [126] mediates DNA fragmentation. Factors like the changes of intracellular Ca2+, the level of ATP/ADP, the release of Cyt C, regulation in mitochondrial morphology, and ROS generation often influence the mPTP opening [127] (Figure 7).
Figure 7.
Cross talk between ROS and mPTP. VDAC, voltage-dependent anion channel; ANT, adenine nucleotide translocator; Cyp-D, cyclophilin-D.
The mechanism of ROS mediating the mPTP formation involves several pathways. Firstly, ROS directly modulate mPTP opening by oxidizing four different sites: Cys160 of ANT, regulated by glutathione oxidation and protected by low concentration of N-ethylmaleimide (NEM) or monobromobimane [128]; Cys56 of ANT, sensitive to the redox state of the matricial pyridine nucleotides perhaps with the mediation of thioredoxin or lipoamide and also protected by NEM, not by monobromobimane [129]; external thiol groups (SH), promoting PTP opening by reaction with NEM or copper-orthophenanthroline; and Cys203 of Cyp-D, S-glutathionylation of which prevents Cyp-D binding to ANT which blocks MPT [130]. Besides, ROS indirectly modulate the opening of mPTP via increasing the mitochondrial Ca2+ concentration ([Ca2+]m): ROS promotes Ca2+ efflux from ER/SR to cytoplasm and from cytoplasm to mitochondria. The increase of Ca2+ concentration in turn favors ATP production and ROS generation during oxidative phosphorylation and promotes the opening of mPTP [131, 132]. In addition, ROS also may translocate Bid to jBid via activating the JNK pathway, which leads to the opening of mPTP [133–135].
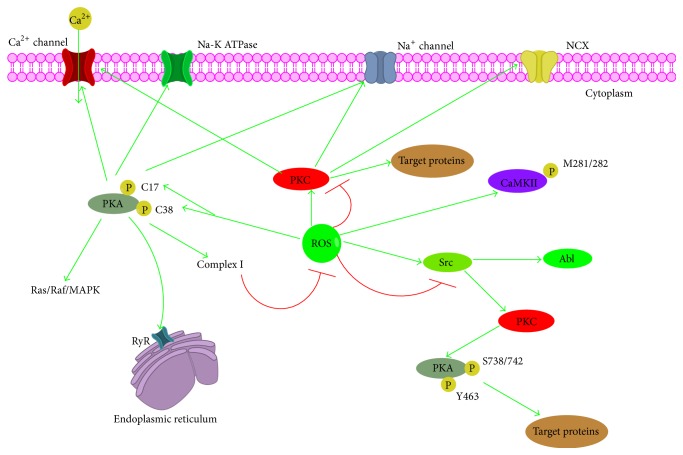
9. ROS and Protein Kinase
Recently, it is becoming increasingly apparent that, like physiological second messengers in signal transduction, ROS function in various cellular processes via oxidating sulfhydryl (SH) groups of cysteine residues in protein kinases including protein kinase A (PKA) [136], protein kinase C (PKC) [137], protein kinase D (PKD) [138], receptor tyrosine kinase (RTK) [139], and Ca/calmodulin independent protein kinase II (CaMKII) [140] and then activated protein kinases phosphorylate their target proteins which are involved in different cellular signaling mechanisms (Figure 8).
Figure 8.
Cross talk between ROS and protein kinase. CaMKII, calcium/calmodulin-dependent protein kinase II; RyR, the ryanodine receptor.
PKA, also called cAMP-dependent protein kinase A, is organized as tetramers comprising two catalytic and two regulatory subunits. The activation of PKA can occur by binding of two molecules of cAMP to each regulatory subunit and then this activated PKA phosphorylates its targeting proteins, including RyR and L-type Ca2+ channel and phospholamban (PLN) [141, 142]. Recently, it has been shown that type I regulatory subunit I of PKA is subjected to oxidation by ROS on Cys 17 and 38, which leads to the intersubunit disulfide bond formation (between two regulatory subunits) and dissociation of the PKA holoenzyme complex. And the translocation (from cytosol to membrane and myofilaments) and activation of type I PKA result in increased cellular contractility without elevations in cAMP [143]. Meanwhile, not only do ROS influence the phosphorylation of PKA, but phosphorylation of PKA also has an impact on the ROS homeostasis. In mammalian cells, the cAMP/PKA pathway regulates the expression, assembly, and catalytic activity of complex I of the mitochondrial respiratory chain and subsequently determines the synthesis and accumulation of ROS [144, 145].
Protein kinase C (PKC), containing four homologous domains termed C1, C2, C3, and C4, is a superfamily of structurally correlated serine-threonine kinases that catalyze numerous critical biochemical reactions, like cellular responses, gene expression, cell proliferation, survival, and migration [146]. In an inactive state, PKC is loosely associated with membrane lipids and chiefly isolated in the cytosolic fraction, whereas activation of PKC increases the affinity of the enzyme for membrane lipids and consequently stabilizes its membrane association, which causes a conformational change to a catalytically competent form of PKC [147–149]. Both the regulatory and catalytic domains of PKC contain cysteine-rich regions, thus making it a highly susceptible direct target for redox regulation. Oxidants play a dual role in both stimulation and inactivation of PKC with relation to the concentration: higher doses of oxidants react with catalytically important cysteine residues inactivating PKC; however, low doses induce stimulation of PKC activity. It has been found that H2O2 stimulated the activation of tyrosine kinases and was able to indirectly regulate the tyrosine phosphorylation of PKC-δ at residues 512 and 523 [150].
PKD isoforms (PKD1, PKD2, and PKD3), the effectors of diacylglycerol (DAG), and protein kinase c (PKC) effectors have been described as vital regulators of diverse cellular pathways and mediate the actions of growth factors, neurotransmitters, hormones, and other stimuli that activate PLCβ and PLCγ [151–153]. The binding of the corresponding ligand to G-protein coupled receptors (GPCRs) or tyrosine kinase receptors activates PLCβ and PLCγ. Then PLCβ cleave PI (4, 5) P2 that generates DAG and IP3. Subsequently, membranal DAG binds to and activates PKC and recruits PKD, which then is phosphorylated and activated by PKC on Ser744 and Ser748 residues [154, 155]. ROS influence the activation of PKD in a various manner: ROS trigger PLD1 and phosphatidic acid phosphatase- (PAP-) catalyzed DAG synthesis and concomitant recruitment of PKD1 and PKCδ at the outer mitochondrial membrane [156]; ROS promotes phosphorylation of PKD on its Tyr93 residue by Src that creates a binding site for the PKCδ C2 domain which facilitates the binding between PKCδ with PKD and the activation of PKD [157]; ROS also could lead to the activation of PKD via the phosphorylation at Tyr463 residue by the tyrosine kinase Abl. Additionally, expression of mitochondrial Mn-SOD induced by PKD1-NF-κB signaling removes toxic ROS [158].
Moreover, the activation of RTK and CaMKII could be affected by the level of intracellular ROS. The oxidation on Met281 and Met282 residues in the regulatory domain results in the activation of CaMKII [159]. And RTKs such as the insulin receptor, EGFR, platelet-derived growth factor receptor (PGFR), and c-Ret have all been reported to undergo direct oxidation on their cysteine residue.
10. ROS and Ubiquitination/Proteasome System
Ubiquitination/Proteasome System (UPS) includes four components: proteasome, ubiquitin, the ubiquitination machinery, and the deubiquitinases (DUBs) [160]. UPS play indispensable roles in variety of biological processes such as regulation of the cell cycle, inflammatory responses, immune response, protein misfolding, and endoplasmic reticulum-associated degradation of proteins. Initially, ubiquitin gets activated by an ATP-dependent E1 ubiquitin-activating enzyme which results in the transient adenylation of ubiquitin and the transference of ubiquitin from E1 to a cysteine residue of E2-ubiquitin conjugating enzyme (Ubc); then E3 transfers ubiquitin from E2-ubiquitin to the lysine residue of a substrate protein by catalyzing the peptidyl bond formation between ubiquitin and the target protein and subsequently the elongation of the polyubiquitin chain which transfers the client protein to the proteasome for degradation through specific proteolytic activities [161–163]. Concurrently, DUBs can remove ubiquitin from substrates and disassemble polyubiquitin chains which may lead to protein stabilization [164].
Recently, an increasing number of studies have documented the interactions between ROS and UPS [165–168]. The susceptibility of the UPP to oxidative stress may have been anticipated, because E1, E2, some E3 enzymes, and DUBs have a cysteine residue, which are sensitive to ROS, in their active sites (Figure 9). The rapid depletion of reduced glutathione (GSH) and improvement of the levels of oxidized glutathione (GSSG) upon exposure to oxidative stress result in the oxidation of cysteine residues in the active sites of E1 and E2 and the generation of mixed disulfide bonds which blocks their binding to ubiquitin [169, 170]. It has also been reported that bacteria elicit ROS generation in epithelial cells that inactivate the Ubc12 enzyme, preventing the neddylation of cullin-1. Unneddylated cullin in E3-SCFβ-TrCP complex renders it unable to carry out ubiquitination and is thus making it inactive [171]. Additionally, numerous reports have suggested that Kelch-like ECH-associated protein-1 (Keap1), a substrate adaptor protein for a cullin-3 E3-ubiquitin ligase (Cul3)/Ring-Box1 (Rbx1) dependent complex, plays a critical role in the ubiquitination and degradation of Nrf2, IKKβ, and Bcl-2/Bcl-xL, also being disturbed by ROS via modifying the reactive cysteines (Cys273, Cys288, and Cys151) and then inducing a conformational change that leads to the release of Nrf2, IKKβ, and Bcl-2/Bcl-xL from Keap1 and the suspending of their ubiquitination and degradation [172–174]. Meanwhile, the proteasome is also a target of oxidative stress and the 26S proteasome was more susceptible than the 20S proteasome to oxidative inactivation [175].
Figure 9.
Regulation of Ubiquitination/Proteasome System by ROS. Ubc, E2-ubiquitin conjugating enzyme.
In turn, UPS regulates cellular redox status via the degradation of Nrf2 and the activation of NF-κB and both could mediate the level of ROS by their downstream antioxidative proteins [176]. In addition, accumulating evidences made it evident that the UPS plays essential roles in regulating mitochondrial processes: oxidative phosphorylation, TCA cycle, and mitochondrial dynamics which subsequently regulate ROS generation [177–179].
11. Conclusions
It has been clearly demonstrated that redox equilibrium plays pivotal roles in cells' physiological and pathological events due to ROS's ability to activate or deactivate a variety of receptors, proteins, ions, and other signaling molecules. When the redox equilibrium is disturbed due to the excessive accumulation or depletion of ROS, many cellular signaling pathways are influenced which confers to the cellular dysfunction and subsequently the development of various pathologies. Therefore, unveiling the mechanisms of ROS regulating redox-associated signaling pathways is essential in providing relevant targets in order to develop innovative and effective therapeutic strategies. However, due to numerous signaling pathways which are sensitive to ROS and the high degree of complexity in simultaneous actions of ROS, even though we have learnt much about the mechanisms by which ROS influences signaling, in particular, the interactions between different ROS associated signaling pathways are yet to be elucidated.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Jixiang Zhang and Xiaoli Wang contributed equally to this work.
References
- 1.Zhang H., Gomez A. M., Wang X., Yan Y., Zheng M., Cheng H. ROS regulation of microdomain Ca2+ signalling at the dyads. Cardiovascular Research. 2013;98(2):248–258. doi: 10.1093/cvr/cvt050. [DOI] [PubMed] [Google Scholar]
- 2.Sena L. A., Chandel N. S. Physiological roles of mitochondrial reactive oxygen species. Molecular Cell. 2012;48(2):158–166. doi: 10.1016/j.molcel.2012.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giorgio M., Trinei M., Migliaccio E., Pelicci P. G. Hydrogen peroxide: a metabolic by-product or a common mediator of ageing signals? Nature Reviews Molecular Cell Biology. 2007;8(9):722–728. doi: 10.1038/nrm2240. [DOI] [PubMed] [Google Scholar]
- 4.Liochev S. I. Reactive oxygen species and the free radical theory of aging. Free Radical Biology and Medicine. 2013;60:1–4. doi: 10.1016/j.freeradbiomed.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Rhee S. G. Cell signaling. H2O2, a necessary evil for cell signaling. Science. 2006;312(5782):1882–1883. doi: 10.1126/science.1130481. [DOI] [PubMed] [Google Scholar]
- 6.Bae Y. S., Oh H., Rhee S. G., Yoo Y. D. Regulation of reactive oxygen species generation in cell signaling. Molecules and Cells. 2011;32(6):491–509. doi: 10.1007/s10059-011-0276-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alfadda A. A., Sallam R. M. Reactive oxygen species in health and disease. Journal of Biomedicine and Biotechnology. 2012;2012:14. doi: 10.1155/2012/936486.936486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsuzawa A., Ichijo H. Stress-responsive protein kinases in redox-regulated apoptosis signaling. Antioxidants and Redox Signaling. 2005;7(3-4):472–481. doi: 10.1089/ars.2005.7.472. [DOI] [PubMed] [Google Scholar]
- 9.Dröge W. Free radicals in the physiological control of cell function. Physiological Reviews. 2002;82(1):47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 10.Finkel T. Signal transduction by reactive oxygen species. Journal of Cell Biology. 2011;194(1):7–15. doi: 10.1083/jcb.201102095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grivennikova V. G., Vinogradov A. D. Mitochondrial production of reactive oxygen species. Biochemistry. 2013;78(13):1490–1511. doi: 10.1134/s0006297913130087. [DOI] [PubMed] [Google Scholar]
- 12.Starkov A. A. The role of mitochondria in reactive oxygen species metabolism and signaling. Annals of the New York Academy of Sciences. 2008;1147:37–52. doi: 10.1196/annals.1427.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galluzzi L., Morselli E., Kepp O., et al. Mitochondrial gateways to cancer. Molecular Aspects of Medicine. 2010;31(1):1–20. doi: 10.1016/j.mam.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 14.Chen Q., Vazquez E. J., Moghaddas S., Hoppel C. L., Lesnefsky E. J. Production of reactive oxygen species by mitochondria: central role of complex III. The Journal of Biological Chemistry. 2003;278(38):36027–36031. doi: 10.1074/jbc.m304854200. [DOI] [PubMed] [Google Scholar]
- 15.Nicholls D. G., Budd S. L. Mitochondria and neuronal survival. Physiological Reviews. 2000;80(1):315–360. doi: 10.1152/physrev.2000.80.1.315. [DOI] [PubMed] [Google Scholar]
- 16.Turrens J. F. Mitochondrial formation of reactive oxygen species. The Journal of Physiology. 2003;552, part 2:335–344. doi: 10.1113/jphysiol.2003.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown D. I., Griendling K. K. Nox proteins in signal transduction. Free Radical Biology and Medicine. 2009;47(9):1239–1253. doi: 10.1016/j.freeradbiomed.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison I. P., Selemidis S. Understanding the biology of reactive oxygen species and their link to cancer: NADPH oxidases as novel pharmacological targets. Clinical and Experimental Pharmacology and Physiology. 2014;41(8):533–542. doi: 10.1111/1440-1681.12238. [DOI] [PubMed] [Google Scholar]
- 19.Lambeth J. D. NOX enzymes and the biology of reactive oxygen. Nature Reviews Immunology. 2004;4(3):181–189. doi: 10.1038/nri1312. [DOI] [PubMed] [Google Scholar]
- 20.Brand M. D. The sites and topology of mitochondrial superoxide production. Experimental Gerontology. 2010;45(7-8):466–472. doi: 10.1016/j.exger.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberge S., Roussel J., Andersson D. C., et al. TNF-α-mediated caspase-8 activation induces ROS production and TRPM2 activation in adult ventricular myocytes. Cardiovascular Research. 2014;103(1):90–99. doi: 10.1093/cvr/cvu112. [DOI] [PubMed] [Google Scholar]
- 22.Ilatovskaya D. V., Pavlov T. S., Levchenko V., Staruschenko A. ROS production as a common mechanism of ENaC regulation by EGF, insulin, and IGF-1. The American Journal of Physiology—Cell Physiology. 2013;304(1):C102–C111. doi: 10.1152/ajpcell.00231.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clauzure M., Valdivieso A. G., Massip Copiz M. M., Schulman G., Teiber M. L., Santa-Coloma T. A. Disruption of interleukin-1β autocrine signaling rescues complex I activity and improves ROS levels in immortalized epithelial cells with impaired cystic fibrosis transmembrane conductance regulator (CFTR) function. PLoS ONE. 2014;9(6) doi: 10.1371/journal.pone.0099257.e99257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Large M., Reichert S., Hehlgans S., Fournier C., Rödel C., Rödel F. A non-linear detection of phospho-histone H2AX in EA.hy926 endothelial cells following low-dose X-irradiation is modulated by reactive oxygen species. Radiation Oncology. 2014;9, article 80 doi: 10.1186/1748-717x-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller A.-F. Superoxide dismutases: ancient enzymes and new insights. FEBS Letters. 2012;586(5):585–595. doi: 10.1016/j.febslet.2011.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marí M., Morales A., Colell A., García-Ruiz C., Fernández-Checa J. C. Mitochondrial glutathione, a key survival antioxidant. Antioxidants and Redox Signaling. 2009;11(11):2685–2700. doi: 10.1089/ars.2009.2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanwal R., Pandey M., Bhaskaran N., et al. Protection against oxidative DNA damage and stress in human prostate by glutathione S-transferase P1. Molecular Carcinogenesis. 2014;53(1):8–18. doi: 10.1002/mc.21939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meloni G., Vašák M. Redox activity of α-synuclein-Cu is silenced by Zn7-metallothionein-3. Free Radical Biology and Medicine. 2011;50(11):1471–1479. doi: 10.1016/j.freeradbiomed.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 29.Chen J., Adikari M., Pallai R., Parekh H. K., Simpkins H. Dihydrodiol dehydrogenases regulate the generation of reactive oxygen species and the development of cisplatin resistance in human ovarian carcinoma cells. Cancer Chemotherapy and Pharmacology. 2008;61(6):979–987. doi: 10.1007/s00280-007-0554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bonizzi G., Karin M. The two NF-κB activation pathways and their role in innate and adaptive immunity. Trends in Immunology. 2004;25(6):280–288. doi: 10.1016/j.it.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Baldwin A. S. Regulation of cell death and autophagy by IKK and NF-κB: critical mechanisms in immune function and cancer. Immunological Reviews. 2012;246(1):327–345. doi: 10.1111/j.1600-065x.2012.01095.x. [DOI] [PubMed] [Google Scholar]
- 32.Devin A., Cook A., Lin Y., Rodriguez Y., Kelliher M., Liu Z.-G. The distinct roles of TRAF2 and RIP in IKK activation by TNF-R1: TRAF2 recruits IKK to TNF-R1 while RIP mediates IKK activation. Immunity. 2000;12(4):419–429. doi: 10.1016/s1074-7613(00)80194-6. [DOI] [PubMed] [Google Scholar]
- 33.Gloire G., Piette J. Redox regulation of nuclear post-translational modifications during NF-κB activation. Antioxidants and Redox Signaling. 2009;11(9):2209–2222. doi: 10.1089/ars.2009.2463. [DOI] [PubMed] [Google Scholar]
- 34.Basak S., Hoffmann A. Crosstalk via the NF-κB signaling system. Cytokine and Growth Factor Reviews. 2008;19(3-4):187–197. doi: 10.1016/j.cytogfr.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gardam S., Brink R. Non-canonical NF-κB signaling initiated by BAFF influences B cell biology at multiple junctures. Frontiers in Immunology. 2014;4, article 509 doi: 10.3389/fimmu.2013.00509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bauer J., Namineni S., Reisinger F., Zöller J., Yuan D., Heikenwälder M. Lymphotoxin, NF-κB, and cancer: the dark side of cytokines. Digestive Diseases. 2012;30(5):453–468. doi: 10.1159/000341690. [DOI] [PubMed] [Google Scholar]
- 37.Elmetwali T., Young L. S., Palmer D. H. Fas-associated factor (Faf1) is a novel CD40 interactor that regulates CD40-induced NF-κB activation via a negative feedback loop. Cell Death and Disease. 2014;5(5) doi: 10.1038/cddis.2014.172.e1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramakrishnan P., Wang W., Wallach D. Receptor-specific signaling for both the alternative and the canonical NF-κB activation pathways by NF-κB-inducing kinase. Immunity. 2004;21(4):477–489. doi: 10.1016/j.immuni.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 39.Journo C., Bonnet A., Favre-bonvin A., et al. Human T cell leukemia virus type 2 tax-mediated NF-κB activation involves a mechanism independent of tax conjugation to ubiquitin and SUMO. Journal of Virology. 2013;87(2):1123–1136. doi: 10.1128/jvi.01792-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song Y.-J., Kang M.-S. Roles of TRAF2 and TRAF3 in Epstein-Barr virus latent membrane protein 1-induced alternative NF-κB activation. Virus Genes. 2010;41(2):174–180. doi: 10.1007/s11262-010-0505-4. [DOI] [PubMed] [Google Scholar]
- 41.Schoonbroodt S., Ferreira V., Best-Belpomme M., et al. Crucial role of the amino-terminal tyrosine residue 42 and the carboxyl-terminal PEST domain of IκBα in NF-κB activation by an oxidative stress. Journal of Immunology. 2000;164(8):4292–4300. doi: 10.4049/jimmunol.164.8.4292. [DOI] [PubMed] [Google Scholar]
- 42.Takada Y., Mukhopadhyay A., Kundu G. C., Mahabeleshwar G. H., Singh S., Aggarwal B. B. Hydrogen peroxide activates NF-κB through tyrosine phosphorylation of IκBα and serine phosphorylation of p65. Evidence for the involvement of IκBα kinase and Syk protein-tyrosine kinase. The Journal of Biological Chemistry. 2003;278(26):24233–24241. doi: 10.1074/jbc.m212389200. [DOI] [PubMed] [Google Scholar]
- 43.Reynaert N. L., van der Vliet A., Guala A. S., et al. Dynamic redox control of NF-κB through glutaredoxin-regulated S-glutathionylation of inhibitory κB kinase β . Proceedings of the National Academy of Sciences of the United States of America. 2006;103(35):13086–13091. doi: 10.1073/pnas.0603290103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cross J. V., Templeton D. J. Thiol oxidation of cell signaling proteins: controlling an apoptotic equilibrium. Journal of Cellular Biochemistry. 2004;93(1):104–111. doi: 10.1002/jcb.20202. [DOI] [PubMed] [Google Scholar]
- 45.Li Q., Engelhardt J. F. Interleukin-1β induction of NFκB is partially regulated by H2O2-mediated activation of NFκB-inducing kinase. The Journal of Biological Chemistry. 2006;281(3):1495–1505. doi: 10.1074/jbc.M511153200. [DOI] [PubMed] [Google Scholar]
- 46.Kim J.-H., Na H.-J., Kim C.-K., et al. The non-provitamin A carotenoid, lutein, inhibits NF-κB-dependent gene expression through redox-based regulation of the phosphatidylinositol 3-kinase/PTEN/Akt and NF-κB-inducing kinase pathways: role of H2O2 in NF-κB activation. Free Radical Biology and Medicine. 2008;45(6):885–896. doi: 10.1016/j.freeradbiomed.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 47.Junttila M. R., Li S.-P., Westermarck J. Phosphatase-mediated crosstalk between MAPK signaling pathways in the regulation of cell survival. The FASEB Journal. 2008;22(4):954–965. doi: 10.1096/fj.06-7859rev. [DOI] [PubMed] [Google Scholar]
- 48.Ravingerová T., Barančík M., Strnisková M. Mitogen-activated protein kinase: a new therapeutic target in cardiac pathology. Molecular and Cellular Biochemistry. 2003;247(1-2):127–138. doi: 10.1023/a:1024119224033. [DOI] [PubMed] [Google Scholar]
- 49.Pimienta G., Pascual J. Canonical and alternative MAPK signaling. Cell Cycle. 2007;6(21):2628–2632. doi: 10.4161/cc.6.21.4930. [DOI] [PubMed] [Google Scholar]
- 50.Kyriakis J. M., Avruch J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiological Reviews. 2001;81(2):807–869. doi: 10.1152/physrev.2001.81.2.807. [DOI] [PubMed] [Google Scholar]
- 51.Chen Z., Gibson T. B., Robinson F., et al. MAP kinases. Chemical Reviews. 2001;101(8):2449–2476. doi: 10.1021/cr000241p. [DOI] [PubMed] [Google Scholar]
- 52.Stadler W. M. Targeted agents for the treatment of advanced renal cell carcinoma. Cancer. 2005;104(11):2323–2333. doi: 10.1002/cncr.21453. [DOI] [PubMed] [Google Scholar]
- 53.Sproul E. P., Argraves W. S. A cytokine axis regulates elastin formation and degradation. Matrix Biology. 2013;32(2):86–94. doi: 10.1016/j.matbio.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Friday B. B., Adjei A. A. Advances in targeting the Ras/Raf/MEK/Erk mitogen-activated protein kinase cascade with MEK inhibitors for cancer therapy. Clinical Cancer Research. 2008;14(2):342–346. doi: 10.1158/1078-0432.ccr-07-4790. [DOI] [PubMed] [Google Scholar]
- 55.Plotnikov A., Zehorai E., Procaccia S., Seger R. The MAPK cascades: signaling components, nuclear roles and mechanisms of nuclear translocation. Biochimica et Biophysica Acta—Molecular Cell Research. 2011;1813(9):1619–1633. doi: 10.1016/j.bbamcr.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 56.León-Buitimea A., Rodríguez-Fragoso L., Lauer F. T., Bowles H., Thompson T. A., Burchiel S. W. Ethanol-induced oxidative stress is associated with EGF receptor phosphorylation in MCF-10A cells overexpressing CYP2E1. Toxicology Letters. 2012;209(2):161–165. doi: 10.1016/j.toxlet.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lei H., Kazlauskas A. Growth factors outside of the platelet-derived growth factor (PDGF) family employ reactive oxygen species/Src family kinases to activate PDGF receptor α and thereby promote proliferation and survival of cells. The Journal of Biological Chemistry. 2009;284(10):6329–6336. doi: 10.1074/jbc.m808426200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wentworth C. C., Alam A., Jones R. M., Nusrat A., Neish A. S. Enteric commensal bacteria induce extracellular signal-regulated kinase pathway signaling via formyl peptide receptor-dependent redox modulation of dual specific phosphatase 3. The Journal of Biological Chemistry. 2011;286(44):38448–38455. doi: 10.1074/jbc.m111.268938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Banan A., Fields J. Z., Zhang Y., Keshavarzian A. Phospholipase C-γ inhibition prevents EGF protection of intestinal cytoskeleton and barrier against oxidants. The American Journal of Physiology—Gastrointestinal and Liver Physiology. 2001;281(2):G412–G423. doi: 10.1152/ajpgi.2001.281.2.G412. [DOI] [PubMed] [Google Scholar]
- 60.Franklin R. A., Atherfold P. A., McCubrey J. A. Calcium-induced ERK activation in human T lymphocytes occurs via p56Lck and CaM-kinase. Molecular Immunology. 2000;37(11):675–683. doi: 10.1016/s0161-5890(00)00087-0. [DOI] [PubMed] [Google Scholar]
- 61.Dann S. G., Golas J., Miranda M., et al. P120 catenin is a key effector of a Ras-PKCε oncogenic signaling axis. Oncogene. 2014;33(11):1385–1394. doi: 10.1038/onc.2013.91. [DOI] [PubMed] [Google Scholar]
- 62.Davies C., Tournier C. Exploring the function of the JNK (c-Jun N-terminal kinase) signalling pathway in physiological and pathological processes to design novel therapeutic strategies. Biochemical Society Transactions. 2012;40(1):85–89. doi: 10.1042/bst20110641. [DOI] [PubMed] [Google Scholar]
- 63.Leonard S. S., Harris G. K., Shi X. Metal-induced oxidative stress and signal transduction. Free Radical Biology and Medicine. 2004;37(12):1921–1942. doi: 10.1016/j.freeradbiomed.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 64.Katagiri K., Matsuzawa A., Ichijo H. Regulation of apoptosis signal-regulating kinase 1 in redox signaling. Methods in Enzymology. 2010;474:277–288. doi: 10.1016/s0076-6879(10)74016-7. [DOI] [PubMed] [Google Scholar]
- 65.Castro-Caldas M., Carvalho A. N., Rodrigues E., Henderson C., Wolf C. R., Gama M. J. Glutathione S-transferase pi mediates MPTP-induced c-Jun N-terminal kinase activation in the nigrostriatal pathway. Molecular Neurobiology. 2012;45(3):466–477. doi: 10.1007/s12035-012-8266-9. [DOI] [PubMed] [Google Scholar]
- 66.Matsukawa J., Matsuzawa A., Takeda K., Ichijo H. The ASK1-MAP kinase cascades in mammalian stress response. The Journal of Biochemistry. 2004;136(3):261–265. doi: 10.1093/jb/mvh134. [DOI] [PubMed] [Google Scholar]
- 67.Grill B., Schrader J. W. Activation of Rac-1, Rac-2, and Cdc42 by hemopoietic growth factors or cross-linking of the B-lymphocyte receptor for antigen. Blood. 2002;100(9):3183–3192. doi: 10.1182/blood-2002-01-0154. [DOI] [PubMed] [Google Scholar]
- 68.Shin I., Kim S., Song H., Kim H.-R. C., Moon A. H-Ras-specific activation of Rac-MKK3/6-p38 pathway: its critical role in invasion and migration of breast epithelial cells. The Journal of Biological Chemistry. 2005;280(15):14675–14683. doi: 10.1074/jbc.m411625200. [DOI] [PubMed] [Google Scholar]
- 69.Cuadrado A., Nebreda A. R. Mechanisms and functions of p38 MAPK signalling. Biochemical Journal. 2010;429(3):403–417. doi: 10.1042/BJ20100323. [DOI] [PubMed] [Google Scholar]
- 70.Hayashi M., Fearns C., Eliceiri B., Yang Y., Lee J.-D. Big mitogen-activated protein kinase 1/extracellular signal-regulated kinase 5 signaling pathway is essential for tumor-associated angiogenesis. Cancer Research. 2005;65(17):7699–7706. doi: 10.1158/0008-5472.CAN-04-4540. [DOI] [PubMed] [Google Scholar]
- 71.Hayes J. D., McMahon M. NRF2 and KEAP1 mutations: permanent activation of an adaptive response in cancer. Trends in Biochemical Sciences. 2009;34(4):176–188. doi: 10.1016/j.tibs.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 72.Taguchi K., Motohashi H., Yamamoto M. Molecular mechanisms of the Keap1-Nrf2 pathway in stress response and cancer evolution. Genes to Cells. 2011;16(2):123–140. doi: 10.1111/j.1365-2443.2010.01473.x. [DOI] [PubMed] [Google Scholar]
- 73.Kensler T. W., Wakabayashi N., Biswal S. Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annual Review of Pharmacology and Toxicology. 2007;47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046. [DOI] [PubMed] [Google Scholar]
- 74.Lee J.-M., Johnson J. A. An important role of Nrf2-ARE pathway in the cellular defense mechanism. Journal of Biochemistry and Molecular Biology. 2004;37(2):139–143. doi: 10.5483/bmbrep.2004.37.2.139. [DOI] [PubMed] [Google Scholar]
- 75.Jung K.-A., Kwak M.-K. The Nrf2 system as a potential target for the development of indirect antioxidants. Molecules. 2010;15(10):7266–7291. doi: 10.3390/molecules15107266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Furukawa M., Xiong Y. BTB protein keap1 targets antioxidant transcription factor Nrf2 for ubiquitination by the cullin 3-Roc1 ligase. Molecular and Cellular Biology. 2005;25(1):162–171. doi: 10.1128/MCB.25.1.162-171.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Villeneuve N. F., Lau A., Zhang D. D. Regulation of the Nrf2-Keap1 antioxidant response by the ubiquitin proteasome system: an insight into cullin-ring ubiquitin ligases. Antioxidants & Redox Signaling. 2010;13(11):1699–1712. doi: 10.1089/ars.2010.3211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dinkova-Kostova A. T., Holtzclaw W. D., Cole R. N., et al. Direct evidence that sulfhydryl groups of Keap1 are the sensors regulating induction of phase 2 enzymes that protect against carcinogens and oxidants. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(18):11908–11913. doi: 10.1073/pnas.172398899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim K. C., Kang K. A., Zhang R., et al. Up-regulation of Nrf2-mediated heme oxygenase-1 expression by eckol, a phlorotannin compound, through activation of Erk and PI3K/Akt. International Journal of Biochemistry and Cell Biology. 2010;42(2):297–305. doi: 10.1016/j.biocel.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 80.Kaspar J. W., Niture S. K., Jaiswal A. K. Nrf2:INrf2 (Keap1) signaling in oxidative stress. Free Radical Biology and Medicine. 2009;47(9):1304–1309. doi: 10.1016/j.freeradbiomed.2009.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nguyen T., Sherratt P. J., Pickett C. B. Regulatory mechanisms controlling gene expression mediated by the antioxidant response element. Annual Review of Pharmacology and Toxicology. 2003;43:233–260. doi: 10.1146/annurev.pharmtox.43.100901.140229. [DOI] [PubMed] [Google Scholar]
- 82.Jain A. K., Jaiswal A. K. GSK-3β acts upstream of Fyn kinase in regulation of nuclear export and degradation of NF-E2 related factor 2. The Journal of Biological Chemistry. 2007;282(22):16502–16510. doi: 10.1074/jbc.m611336200. [DOI] [PubMed] [Google Scholar]
- 83.Yip W. K., Seow H. F. Activation of phosphatidylinositol 3-kinase/Akt signaling by EGF downregulates membranous E-cadherin and β-catenin and enhances invasion in nasopharyngeal carcinoma cells. Cancer Letters. 2012;318(2):162–172. doi: 10.1016/j.canlet.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 84.Hong J., Qian T., Le Q., et al. NGF promotes cell cycle progression by regulating D-type cyclins via PI3K/Akt and MAPK/Erk activation in human corneal epithelial cells. Molecular Vision. 2012;18:758–764. [PMC free article] [PubMed] [Google Scholar]
- 85.Qiu X., Cheng J.-C., Chang H.-M., Leung P. C. K. COX2 and PGE2 mediate EGF-induced E-cadherin-independent human ovarian cancer cell invasion. Endocrine-Related Cancer. 2014;21(4):533–543. doi: 10.1530/erc-13-0450. [DOI] [PubMed] [Google Scholar]
- 86.Ahn I. E., Ju J. H., Lee S. Y., et al. Upregulation of stromal cell-derived factor by IL-17 and IL-18 via a phosphatidylinositol 3-kinase-dependent pathway. Scandinavian Journal of Immunology. 2012;76(4):433–439. doi: 10.1111/j.1365-3083.2012.02745.x. [DOI] [PubMed] [Google Scholar]
- 87.Cantrell D. A. Phosphoinositide 3-kinase signalling pathways. Journal of Cell Science. 2001;114, part 8:1439–1445. doi: 10.1242/jcs.114.8.1439. [DOI] [PubMed] [Google Scholar]
- 88.Sarbassov D. D., Guertin D. A., Ali S. M., Sabatini D. M. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307(5712):1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 89.Cohen P., Frame S. The renaissance of GSK3. Nature Reviews Molecular Cell Biology. 2001;2(10):769–776. doi: 10.1038/35096075. [DOI] [PubMed] [Google Scholar]
- 90.Zhang Y., Gan B., Liu D., Paik J.-H. FoxO family members in cancer. Cancer Biology and Therapy. 2011;12(4):253–259. doi: 10.4161/cbt.12.4.15954. [DOI] [PubMed] [Google Scholar]
- 91.Zhang X.-S., Zhang X., Wu Q., et al. Astaxanthin alleviates early brain injury following subarachnoid hemorrhage in rats: possible involvement of Akt/bad signaling. Marine Drugs. 2014;12(8):4291–4310. doi: 10.3390/md12084291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Abraham A. G., O'Neill E. PI3K/Akt-mediated regulation of p53 in cancer. Biochemical Society Transactions. 2014;42(4):798–803. doi: 10.1042/BST20140070. [DOI] [PubMed] [Google Scholar]
- 93.Leslie N. R., Downes C. P. PTEN: the down side of PI 3-kinase signalling. Cellular Signalling. 2002;14(4):285–295. doi: 10.1016/s0898-6568(01)00234-0. [DOI] [PubMed] [Google Scholar]
- 94.Lee S.-R., Yang K.-S., Kwon J., Lee C., Jeong W., Rhee S. G. Reversible inactivation of the tumor suppressor PTEN by H2O2 . The Journal of Biological Chemistry. 2002;277(23):20336–20342. doi: 10.1074/jbc.m111899200. [DOI] [PubMed] [Google Scholar]
- 95.Murata H., Ihara Y., Nakamura H., Yodoi J., Sumikawa K., Kondo T. Glutaredoxin exerts an antiapoptotic effect by regulating the redox state of Akt. The Journal of Biological Chemistry. 2003;278(50):50226–50233. doi: 10.1074/jbc.m310171200. [DOI] [PubMed] [Google Scholar]
- 96.Tarasov A. I., Griffiths E. J., Rutter G. A. Regulation of ATP production by mitochondrial Ca2+ . Cell Calcium. 2012;52(1):28–35. doi: 10.1016/j.ceca.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Naranjo J. R., Mellström B. Ca2+-dependent transcriptional control of Ca2+ homeostasis. The Journal of Biological Chemistry. 2012;287(38):31674–31680. doi: 10.1074/jbc.r112.384982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Berridge M. J., Bootman M. D., Roderick H. L. Calcium signalling: dynamics, homeostasis and remodelling. Nature Reviews Molecular Cell Biology. 2003;4(7):517–529. doi: 10.1038/nrm1155. [DOI] [PubMed] [Google Scholar]
- 99.Felsenfeld A., Rodriguez M., Levine B. New insights in regulation of calcium homeostasis. Current Opinion in Nephrology and Hypertension. 2013;22(4):371–376. doi: 10.1097/mnh.0b013e328362141e. [DOI] [PubMed] [Google Scholar]
- 100.Stathopulos P. B., Ikura M. Partial unfolding and oligomerization of stromal interaction molecules as an initiation mechanism of store operated calcium entry. Biochemistry and Cell Biology. 2010;88(2):175–183. doi: 10.1139/O09-125. [DOI] [PubMed] [Google Scholar]
- 101.Kurosaki T., Baba Y. Ca2+ signaling and STIM1. Progress in Biophysics and Molecular Biology. 2010;103(1):51–58. doi: 10.1016/j.pbiomolbio.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 102.Mándi M., Bak J. Nicotinic acid adenine dinucleotide phosphate (NAADP) and Ca2+ mobilization. Journal of Receptors and Signal Transduction. 2008;28(3):163–184. doi: 10.1080/10799890802084085. [DOI] [PubMed] [Google Scholar]
- 103.Brini M., Calì T., Ottolini D., Carafoli E. The plasma membrane calcium pump in health and disease. The FEBS Journal. 2013;280(21):5385–5397. doi: 10.1111/febs.12193. [DOI] [PubMed] [Google Scholar]
- 104.Samanta K., Douglas S., Parekh A. B. Mitochondrial calcium uniporter MCU supports cytoplasmic Ca2+ oscillations, store-operated Ca2+ entry and Ca2+-dependent gene expression in response to receptor stimulation. PLoS ONE. 2014;9(7) doi: 10.1371/journal.pone.0101188.e101188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lewis A., Hayashi T., Su T.-P., Betenbaugh M. J. Bcl-2 family in inter-organelle modulation of calcium signaling; roles in bioenergetics and cell survival. Journal of Bioenergetics and Biomembranes. 2014;46(1):1–15. doi: 10.1007/s10863-013-9527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hatano A., Okada J.-I., Washio T., Hisada T., Sugiura S. Mitochondrial colocalization with Ca2+ release sites is crucial to cardiac metabolism. Biophysical Journal. 2013;104(2):496–504. doi: 10.1016/j.bpj.2012.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Konràd C., Kiss G., Töröcsik B., et al. A distinct sequence in the adenine nucleotide translocase from Artemia franciscana embryos is associated with insensitivity to bongkrekate and atypical effects of adenine nucleotides on Ca2+ uptake and sequestration. The FEBS Journal. 2011;278(5):822–836. doi: 10.1111/j.1742-4658.2010.08001.x. [DOI] [PubMed] [Google Scholar]
- 108.Menzies K. J., Robinson B. H., Hood D. A. Effect of thyroid hormone on mitochondrial properties and oxidative stress in cells from patients with mtDNA defects. American Journal of Physiology—Cell Physiology. 2009;296(2):C355–C362. doi: 10.1152/ajpcell.00415.2007. [DOI] [PubMed] [Google Scholar]
- 109.Montezano A. C., Burger D., Ceravolo G. S., Yusuf H., Montero M., Touyz R. M. Novel nox homologues in the vasculature: focusing on Nox4 and Nox5. Clinical Science. 2011;120(4):131–141. doi: 10.1042/cs20100384. [DOI] [PubMed] [Google Scholar]
- 110.Roe N. D., He E. Y., Wu Z., Ren J. Folic acid reverses nitric oxide synthase uncoupling and prevents cardiac dysfunction in insulin resistance: role of Ca2+/calmodulin-activated protein kinase II. Free Radical Biology and Medicine. 2013;65:234–243. doi: 10.1016/j.freeradbiomed.2013.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gordeeva A. V., Zvyagilskaya R. A., Labas Y. A. Cross-talk between reactive oxygen species and calcium in living cells. Biochemistry. 2003;68(10):1077–1080. doi: 10.1023/a:1026398310003. [DOI] [PubMed] [Google Scholar]
- 112.Thompson M. D., Mei Y., Weisbrod R. M., et al. Glutathione adducts on sarcoplasmic/endoplasmic reticulum Ca2+ ATPase Cys-674 regulate endothelial cell calcium stores and angiogenic function as well as promote ischemic blood flow recovery. The Journal of Biological Chemistry. 2014;289(29):19907–19916. doi: 10.1074/jbc.m114.554451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.An B., Chen Y., Li B., Qin G., Tian S. Ca2+-CaM regulating viability of Candida guilliermondii under oxidative stress by acting on detergent resistant membrane proteins. Journal of Proteomics. 2014;109:38–49. doi: 10.1016/j.jprot.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 114.Chaube R., Hess D. T., Wang Y.-J., et al. Regulation of the skeletal muscle ryanodine receptor/Ca2+-release channel RyR1 by S-palmitoylation. The Journal of Biological Chemistry. 2014;289(12):8612–8619. doi: 10.1074/jbc.m114.548925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bogeski I., Niemeyer B. A. Redox regulation of ion channels. Antioxidants and Redox Signaling. 2014;21(6):859–862. doi: 10.1089/ars.2014.6019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kaplan P., Babusikova E., Lehotsky J., Dobrota D. Free radical-induced protein modification and inhibition of Ca2+-ATPase of cardiac sarcoplasmic reticulum. Molecular and Cellular Biochemistry. 2003;248(1-2):41–47. doi: 10.1023/a:1024145212616. [DOI] [PubMed] [Google Scholar]
- 117.Lushington G. H., Zaidi A., Michaelis M. L. Theoretically predicted structures of plasma membrane Ca2+-ATPase and their susceptibilities to oxidation. Journal of Molecular Graphics and Modelling. 2005;24(3):175–185. doi: 10.1016/j.jmgm.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 118.Nishida M., Ishikawa T., Saiki S., et al. Voltage-dependent N-type Ca2+ channels in endothelial cells contribute to oxidative stress-related endothelial dysfunction induced by angiotensin II in mice. Biochemical and Biophysical Research Communications. 2013;434(2):210–216. doi: 10.1016/j.bbrc.2013.03.040. [DOI] [PubMed] [Google Scholar]
- 119.Morciano G., Giorgi C., Bonora M., et al. Molecular identity of the mitochondrial permeability transition pore and its role in ischemia-reperfusion injury. Journal of Molecular and Cellular Cardiology. 2015;78:142–153. doi: 10.1016/j.yjmcc.2014.08.015. [DOI] [PubMed] [Google Scholar]
- 120.Rao V. K., Carlson E. A., Yan S. S. Mitochondrial permeability transition pore is a potential drug target for neurodegeneration. Biochimica et Biophysica Acta (BBA)—Molecular Basis of Disease. 2014;1842(8):1267–1272. doi: 10.1016/j.bbadis.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Basañez G., Soane L., Hardwick J. M. A new view of the lethal apoptotic pore. PLoS Biology. 2012;10(9) doi: 10.1371/journal.pbio.1001399.e1001399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Liu Y., Chen X. J. Adenine nucleotide translocase, mitochondrial stress, and degenerative cell death. Oxidative Medicine and Cellular Longevity. 2013;2013:10. doi: 10.1155/2013/146860.146860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.McCommis K. S., Baines C. P. The role of VDAC in cell death: friend or foe? Biochimica et Biophysica Acta. 2012;1818(6):1444–1450. doi: 10.1016/j.bbamem.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Halestrap A. P., Doran E., Gillespie J. P., O'Toole A. Mitochondria and cell death. Biochemical Society Transactions. 2000;28(2):170–177. doi: 10.1042/bst0280170. [DOI] [PubMed] [Google Scholar]
- 125.Ghibelli L., Diederich M. Multistep and multitask Bax activation. Mitochondrion. 2010;10(6):604–613. doi: 10.1016/j.mito.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 126.Gouspillou G., Sgarioto N., Kapchinsky S., et al. Increased sensitivity to mitochondrial permeability transition and myonuclear translocation of endonuclease G in atrophied muscle of physically active older humans. The FASEB Journal. 2014;28(4):1621–1633. doi: 10.1096/fj.13-242750. [DOI] [PubMed] [Google Scholar]
- 127.Halestrap A. P., Clarke S. J., Javadov S. A. Mitochondrial permeability transition pore opening during myocardial reperfusion—a target for cardioprotection. Cardiovascular Research. 2004;61(3):372–385. doi: 10.1016/s0008-6363(03)00533-9. [DOI] [PubMed] [Google Scholar]
- 128.Halestrap A. P. What is the mitochondrial permeability transition pore? Journal of Molecular and Cellular Cardiology. 2009;46(6):821–831. doi: 10.1016/j.yjmcc.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 129.McStay G. P., Clarke S. J., Halestrap A. P. Role of critical thiol groups on the matrix surface of the adenine nucleotide translocase in the mechanism of the mitochondrial permeability transition pore. Biochemical Journal. 2002;367(2):541–548. doi: 10.1042/BJ20011672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Sánchez G., Fernández C., Montecinos L., Domenech R. J., Donoso P. Preconditioning tachycardia decreases the activity of the mitochondrial permeability transition pore in the dog heart. Biochemical and Biophysical Research Communications. 2011;410(4):916–921. doi: 10.1016/j.bbrc.2011.06.095. [DOI] [PubMed] [Google Scholar]
- 131.Brinkkoetter P.-T., Song H., Lösel R., et al. Hypothermic injury: the mitochondrial calcium, ATP and ROS love-hate triangle out of balance. Cellular Physiology and Biochemistry. 2008;22(1–4):195–204. doi: 10.1159/000149797. [DOI] [PubMed] [Google Scholar]
- 132.Voronina S., Okeke E., Parker T., Tepikin A. How to win ATP and influence Ca2+ signaling. Cell Calcium. 2014;55(3):131–138. doi: 10.1016/j.ceca.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 133.Deng Y., Ren X., Yang L., Lin Y., Wu X. A JNK-dependent pathway is required for TNFα-induced apoptosis. Cell. 2003;115(1):61–70. doi: 10.1016/s0092-8674(03)00757-8. [DOI] [PubMed] [Google Scholar]
- 134.Maryanovich M., Gross A. A ROS rheostat for cell fate regulation. Trends in Cell Biology. 2013;23(3):129–134. doi: 10.1016/j.tcb.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 135.Wagner S., Rokita A. G., Anderson M. E., Maier L. S. Redox regulation of sodium and calcium handling. Antioxidants and Redox Signaling. 2013;18(9):1063–1077. doi: 10.1089/ars.2012.4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Thompson J. W., Narayanan S. V., Perez-Pinzon M. A. Redox signaling pathways involved in neuronal ischemic preconditioning. Current Neuropharmacology. 2012;10(4):354–369. doi: 10.2174/1570159x11209040354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Eisenberg-Lerner A., Kimchi A. PKD is a kinase of Vps34 that mediates ROS-induced autophagy downstream of DAPk. Cell Death and Differentiation. 2012;19(5):788–797. doi: 10.1038/cdd.2011.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kruk J. S., Vasefi M. S., Heikkila J. J., Beazely M. A. Reactive oxygen species are required for 5-HT-induced transactivation of neuronal platelet-derived growth factor and TrkB receptors, but not for ERK1/2 activation. PLoS ONE. 2013;8(9) doi: 10.1371/journal.pone.0077027.e77027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sag C. M., Wolff H. A., Neumann K., et al. Ionizing radiation regulates cardiac Ca handling via increased ROS and activated CaMKII. Basic Research in Cardiology. 2013;108(6, article 385) doi: 10.1007/s00395-013-0385-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ramirez-Correa G. A., Cortassa S., Stanley B., Gao W. D., Murphy A. M. Calcium sensitivity, force frequency relationship and cardiac troponin I: critical role of PKA and PKC phosphorylation sites. Journal of Molecular and Cellular Cardiology. 2010;48(5):943–953. doi: 10.1016/j.yjmcc.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Taylor S. S., Zhang P., Steichen J. M., Keshwani M. M., Kornev A. P. PKA: Lessons learned after twenty years. Biochimica et Biophysica Acta—Proteins and Proteomics. 2013;1834(7):1271–1278. doi: 10.1016/j.bbapap.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Brennan J. P., Bardswell S. C., Burgoyne J. R., et al. Oxidant-induced activation of type I protein kinase A is mediated by RI subunit interprotein disulfide bond formation. The Journal of Biological Chemistry. 2006;281(31):21827–21836. doi: 10.1074/jbc.m603952200. [DOI] [PubMed] [Google Scholar]
- 143.Papa S., Rasmo D. D., Technikova-Dobrova Z., et al. Respiratory chain complex I, a main regulatory target of the cAMP/PKA pathway is defective in different human diseases. FEBS Letters. 2012;586(5):568–577. doi: 10.1016/j.febslet.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 144.Papa S., De Rasmo D. Complex I deficiencies in neurological disorders. Trends in Molecular Medicine. 2013;19(1):61–69. doi: 10.1016/j.molmed.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 145.do Carmo A., Balça-Silva J., Matias D., Lopes M. C. PKC signaling in glioblastoma. Cancer Biology and Therapy. 2013;14(4):287–294. doi: 10.4161/cbt.23615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lee I.-T., Yang C.-M. Inflammatory signalings involved in airway and pulmonary diseases. Mediators of Inflammation. 2013;2013:12. doi: 10.1155/2013/791231.791231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Nitti M., Pronzato M. A., Marinari U. M., Domenicotti C. PKC signaling in oxidative hepatic damage. Molecular Aspects of Medicine. 2008;29(1-2):36–42. doi: 10.1016/j.mam.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 148.Mochly-Rosen D., Das K., Grimes K. V. Protein kinase C, an elusive therapeutic target? Nature Reviews Drug Discovery. 2012;11(12):937–957. doi: 10.1038/nrd3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Welman A., Griffiths J. R., Whetton A. D., Dive C. Protein kinase C delta is phosphorylated on five novel Ser/Thr sites following inducible overexpression in human colorectal cancer cells. Protein Science. 2007;16(12):2711–2715. doi: 10.1110/ps.072874607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Aicart-Ramos C., Sánchez-Ruiloba L., Gómez-Parrizas M., Zaragoza C., Iglesias T., Rodríguez-Crespo I. Protein kinase D activity controls endothelial nitric oxide synthesis. Journal of Cell Science. 2014;127(part 15):3360–3372. doi: 10.1242/jcs.148601. [DOI] [PubMed] [Google Scholar]
- 151.Olala L. O., Shapiro B. A., Merchen T. C., Wynn J. J., Bollag W. B. Protein kinase C and Src family kinases mediate angiotensin II-induced protein kinase D activation and acute aldosterone production. Molecular and Cellular Endocrinology. 2014;392(1-2):173–181. doi: 10.1016/j.mce.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Li G., Wang Y. Protein kinase D: a new player among the signaling proteins that regulate functions in the nervous system. Neuroscience Bulletin. 2014;30(3):497–504. doi: 10.1007/s12264-013-1403-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Olayioye M. A., Barisic S., Hausser A. Multi-level control of actin dynamics by protein kinase D. Cellular Signalling. 2013;25(9):1739–1747. doi: 10.1016/j.cellsig.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 154.Wang Q. J. PKD at the crossroads of DAG and PKC signaling. Trends in Pharmacological Sciences. 2006;27(6):317–323. doi: 10.1016/j.tips.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 155.Cowell C. F., Döppler H., Yan I. K., Hausser A., Umazawa Y., Storz P. Mitochondrial diacylglycerol initiates protein-kinase-D1-mediated ROS signaling. Journal of Cell Science. 2009;122(7):919–928. doi: 10.1242/jcs.041061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Storz P., Toker A. Protein kinase D mediates a stress-induced NF-κB activation and survival pathway. The EMBO Journal. 2003;22(1):109–120. doi: 10.1093/emboj/cdg009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Storz P., Döppler H., Toker A. Activation loop phosphorylation controls protein kinase D-dependent activation of nuclear factor κB. Molecular Pharmacology. 2004;66(4):870–879. doi: 10.1124/mol.104.000687. [DOI] [PubMed] [Google Scholar]
- 158.Sag C. M., Wagner S., Maier L. S. Role of oxidants on calcium and sodium movement in healthy and diseased cardiac myocytes. Free Radical Biology and Medicine. 2013;63:338–349. doi: 10.1016/j.freeradbiomed.2013.05.035. [DOI] [PubMed] [Google Scholar]
- 159.Dietrich S., Uppalapati R., Seiwert T. Y., Ma P. C. Role of c-MET in upper aerodigestive malignancies—from biology to novel therapies. Journal of Environmental Pathology, Toxicology and Oncology. 2005;24(3):149–162. doi: 10.1615/jenvpathtoxoncol.v24.i3.20. [DOI] [PubMed] [Google Scholar]
- 160.Calise J., Powell S. R. The ubiquitin proteasome system and myocardial ischemia. The American Journal of Physiology—Heart and Circulatory Physiology. 2013;304(3):H337–H349. doi: 10.1152/ajpheart.00604.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Voutsadakis I. A. The ubiquitin-proteasome system and signal transduction pathways regulating Epithelial Mesenchymal transition of cancer. Journal of Biomedical Science. 2012;19(1, article 67) doi: 10.1186/1423-0127-19-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Isasa M., Zuin A., Crosas B. Integration of multiple ubiquitin signals in proteasome regulation. Methods in Molecular Biology. 2012;910:337–370. doi: 10.1007/978-1-61779-965-5_15. [DOI] [PubMed] [Google Scholar]
- 163.Kim M., Otsubo R., Morikawa H., et al. Bacterial effectors and their functions in the ubiquitin-proteasome system: insight from the modes of substrate recognition. Cells. 2014;3(3):848–864. doi: 10.3390/cells3030848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Powell S. R., Herrmann J., Lerman A., Patterson C., Wang X. The ubiquitin-proteasome system and cardiovascular disease. Progress in Molecular Biology and Translational Science. 2012;109:295–346. doi: 10.1016/B978-0-12-397863-9.00009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Reyskens K. M. S. E., Essop M. F. HIV protease inhibitors and onset of cardiovascular diseases: a central role for oxidative stress and dysregulation of the ubiquitin-proteasome system. Biochimica et Biophysica Acta (BBA)—Molecular Basis of Disease. 2014;1842(2):256–268. doi: 10.1016/j.bbadis.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 166.Segref A., Kevei É., Pokrzywa W., et al. Pathogenesis of human mitochondrial diseases is modulated by reduced activity of the ubiquitin/proteasome system. Cell Metabolism. 2014;19(4):642–652. doi: 10.1016/j.cmet.2014.01.016. [DOI] [PubMed] [Google Scholar]
- 167.Warnatsch A., Bergann T., Krüger E. Oxidation matters: the ubiquitin proteasome system connects innate immune mechanisms with MHC class I antigen presentation. Molecular Immunology. 2013;55(2):106–109. doi: 10.1016/j.molimm.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 168.Kwak Y.-D., Wang B., Li J. J., et al. Upregulation of the E3 ligase NEDD4-1 by oxidative stress degrades IGF-1 receptor protein in neurodegeneration. The Journal of Neuroscience. 2012;32(32):10971–10981. doi: 10.1523/jneurosci.1836-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Obin M., Shang F., Gong X., Handelman G., Blumberg J., Taylor A. Redox regulation of ubiquitin-conjugating enzymes: mechanistic insights using the thiol-specific oxidant diamide. The FASEB Journal. 1998;12(7):561–569. doi: 10.1096/fasebj.12.7.561. [DOI] [PubMed] [Google Scholar]
- 170.Jahngen-Hodge J., Obin M. S., Gong X., et al. Regulation of ubiquitin-conjugating enzymes by glutathione following oxidative stress. The Journal of Biological Chemistry. 1997;272(45):28218–28226. doi: 10.1074/jbc.272.45.28218. [DOI] [PubMed] [Google Scholar]
- 171.Kumar A., Wu H., Collier-Hyams L. S., et al. Commensal bacteria modulate cullin-dependent signaling via generation of reactive oxygen species. The EMBO Journal. 2007;26(21):4457–4466. doi: 10.1038/sj.emboj.7601867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Tian H., Zhang B., Di J., et al. Keap1: one stone kills three birds Nrf2, IKKβ and Bcl-2/Bcl-xL. Cancer Letters. 2012;325(1):26–34. doi: 10.1016/j.canlet.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 173.Nordgren K. K. S., Wallace K. B. Keap1 redox-dependent regulation of doxorubicin-induced oxidative stress response in cardiac myoblasts. Toxicology and Applied Pharmacology. 2014;274(1):107–116. doi: 10.1016/j.taap.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 174.Kanzaki H., Shinohara F., Kajiya M., Kodama T. The Keap1/Nrf2 protein axis plays a role in osteoclast differentiation by regulating intracellular reactive oxygen species signaling. The Journal of Biological Chemistry. 2013;288(32):23009–23020. doi: 10.1074/jbc.m113.478545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Reinheckel T., Ullrich O., Sitte N., Grune T. Differential impairment of 20S and 26S proteasome activities in human hematopoietic K562 cells during oxidative stress. Archives of Biochemistry and Biophysics. 2000;377(1):65–68. doi: 10.1006/abbi.2000.1717. [DOI] [PubMed] [Google Scholar]
- 176.Shang F., Taylor A. Ubiquitin-proteasome pathway and cellular responses to oxidative stress. Free Radical Biology and Medicine. 2011;51(1):5–16. doi: 10.1016/j.freeradbiomed.2011.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sickmann A., Reinders J., Wagner Y., et al. The proteome of Saccharomyces cerevisiae mitochondria. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(23):13207–13212. doi: 10.1073/pnas.2135385100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Jeon H. B., Choi E. S., Yoon J. H., et al. A proteomics approach to identify the ubiquitinated proteins in mouse heart. Biochemical and Biophysical Research Communications. 2007;357(3):731–736. doi: 10.1016/j.bbrc.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 179.Peng J., Schwartz D., Elias J. E., et al. A proteomics approach to understanding protein ubiquitination. Nature Biotechnology. 2003;21(8):921–926. doi: 10.1038/nbt849. [DOI] [PubMed] [Google Scholar]