Abstract
Persons with disabilities use more health care services due to ill health and face higher health care expenses and burden. This study explored the incidence of catastrophic health expenditures of households with persons with disabilities compared to that of those without such persons. We used the Korean Health Panel (KHP) dataset for the years 2010 and 2011. The final sample was 5,610 households; 800 (14.3%) of these were households with a person with a disability and 4,810 (85.7%) were households without such a person. Households with a person with a disability faced higher catastrophic health expenditures, spending about 1.2 to 1.4 times more of their annual living expenditures for out-of-pocket medical expenses, compared to households without persons with disabilities. Households having low economic status and members with chronic disease were more likely to face catastrophic health expenditures, while those receiving public assistance were less likely. Exemption or reduction of out-of-pocket payments in the National Health Insurance and additional financial support are needed so that the people with disabilities can use medical services without suffering financial crisis.
Keywords: Disability, Household, Catastrophic Health Expenditure
Graphical Abstract
INTRODUCTION
The National Health Insurance (NHI) program in Korea is an essential social security net covering the entire population. Healthcare providers are reimbursed by a regulated fee for service and out-of-pocket (OOP) rates for each medical service (range 20–40%). On average, OOP payments financed 37% of health expenditures in Korea, compared with 20% of those across OECD countries in 2011 (1). High OOP payment is a barrier to use of medical services, resulting in limited financial protections and healthcare inequities (2). Although health insurance systems and financial risk pooling mechanisms have evolved in Korea, there is still reliance on OOP healthcare financing; the incidence of catastrophic payments is much higher in Korea than other high-income countries (3).
Along with medical aid programs for people below the poverty line, the Korean government has expanded benefit coverage along with reducing OOP payment for disadvantaged groups in order to alleviate the financial burdens of high health expenditures. For example, registered patients with rare and difficult-to-treat diseases or cancers pay only 10% of the total medical expenses as OOP payments. Despite these government efforts, many disadvantaged groups are not considered target populations for benefit enhancement. In particular, people with disability or chronic illness who have more healthcare needs but are above the poverty line are exposed to the risks of not receiving necessary medical services without regard for their ability to pay. High healthcare expenditure and low capacity to pay for catastrophic health expenditures can produce impoverishment.
Catastrophic health expenditure is a construct to measure the burden of OOP payment relative to financial resources. It is defined as “when a household’s total out-of-pocket health payments equal or exceed 40% of household’s capacity to pay or non-subsistence spending” (4). Catastrophic health expenditure has been used to evaluate the equity of healthcare payments at the national level (3,5) and to address the catastrophic impact of OOP payments on lives at the individual and household levels (6,7,8,9,10,11). Increasingly, research finds that people with disabilities face significantly higher total healthcare expenditures, OOP spending, and burden compared to those without disabilities (7,11,12,13,14,15,16).
Even though people with disabilities may not always need consistent healthcare in the long term, they are at risk of developing secondary conditions, which co-occur with other chronic conditions (17) and occupational injury incidence (18), and thus use more health services (15). Because physical or mental disability contributes to job loss or reduced earnings (19), low family income as well as high healthcare needs due to disability also cause high medical expenditure burdens. Even relatively small expenses can be catastrophic to poor households and catastrophic healthcare expenditures can lead to impoverishment (10,20). Both OOP expenses and household characteristics, such as economic and insurance status, were related to the incidence of catastrophic health expenditures for households with special-needs children (14,20), households with chronically ill members (21,22), and people with mental health problems (19).
Even with universal social insurance, Korea also faces relatively high OOP payments for healthcare as a percentage of household consumption (3,5). Some studies suggested that Korean households with poor or chronically ill members are particularly vulnerable (21,23,24). The Korean government faces critical challenges to enhance benefit coverage and equity in financial protection. At this point in time, it is important to determine how much of a burden regarding OOP payments and how much risk of impoverishment due to high healthcare payments households with disabled members face. Moreover, previous research mostly included disability as one factor associated with catastrophic health expenditures rather than focusing on households with members with disabilities (8,9,10,11). Therefore, we estimated the incidence of catastrophic healthcare expenditures among households with members who are disabled compared to those without members who are disabled. Additionally, we identified factors associated with catastrophic healthcare in entire sample. This will be helpful to promote the Korean government’s actions to protect them against the financial burden of healthcare.
MATERIALS AND METHODS
Study design
We used the Korean Health Panel (KHP) dataset, which was collected by the Korean Institution for Health and Social Affairs and the Korean National Health Insurance Corporation. The KHP is a nationwide representative survey with a stratified, multistage probability sampling design providing scientific data on health service use, expenditure, and health behaviors at individual and household levels. The KHP questionnaires consisted of household components and household member components and were surveyed by both interview and diary method to supplement memory. Since the first survey started in 2008 with a sample of 7,866 households and 24,616 household members, integrated data for the given year were released from 2008 to 2011.Two-year household-level data from the 2010–2011 KHP were combined to improve estimate precision. That is, we used the 2010 KHP for health expenditure and household characteristic variables and the 2011 data for living expenditure information, because the KHP measured health expenditures from a given year and living expenditures and income made in the previous year. In 2010, 17,885 individuals from 5,956 households and in 2011, 17,035 individuals from 5,741 households responded. After merging the data, 5,637 households responded. A total of 27 households with deaths within the year were excluded. The final sample was 5,610 households; 800 (14.3%) were households with members with disabilities and 4,810 (85.7%) were households without members with disabilities.
Households with disabled members
We classified households as having one or more disabled members if the respondent answered that at least one family member was registered in a national disability registry system according to the Korean Disability Act. The Korean Ministry of Health and Welfare has administered a national disability registry system since 1988 in order to establish a welfare delivery system for disabled persons. This system classified persons into one of 15 disability types and six grades of severity from 1 (very severe) to 6 (mild). If people diagnosed with a disability voluntarily apply for disability registration, they are registered into the system after passing the disability grade examination. As of December 2012, there were 2.5 million registered persons with disabilities; this value represents approximately 5.0% of the Korean population.
Because we had only household-level data on healthcare expenditures, we had to allocate one value to each household characteristic variable. In the case of households with two or more members with a disability, information on the first household member with a disability was used for analysis.
Catastrophic health expenditure
Health expenditures are defined as catastrophic when OOP spending on healthcare exceeds a given threshold of a household’s capacity to pay (3,5). Since there was no consensus on the threshold proportion of household expenditures, which varied from 5% to 40%, we used various threshold levels (10%, 20%, 30%, and 40%). A household’s capacity to pay was measured by the total consumption expenditure of the household after basic subsistence needs have been met; that is, the average household yearly non-food expenditure. According to Xu et al. (5), consumption expenditure is a more accurate reflection of purchasing power compared to income reported in household surveys in many countries. The amount after monthly food expenditure was deducted from monthly living expenditure was used to calculate yearly expenditure. OOP healthcare expenditures were measured by the sum of OOP payments that any household members made for emergencies, inpatient and outpatient services, and prescription drugs in a given year. Indirect medical costs, such as payment for transportation or care, were not included.
Explanatory variables
We included variables for the household characteristics and the demographic and disability characteristics of members using KHI data as explanatory variables. Household characteristics included number of household members; household income quintiles; receiving public assistance (yes, no); having a member over 65 years (yes, no); household head over 65 years (yes, no); Household head's employment status (working, not working); and having a member with chronic disease including neoplasm, hypertension, cerebrovascular disease, diabetes, and arthritis (yes, no). Equivalent household income was obtained by dividing household income by the square root of the number of household members in order to adjust for differences in family size. Total sample was divided into five groups of equivalent household income distribution (called quintiles).
Disability characteristics of members included type and severity of disability. We combined the 15 disability types of the Korean National Disability Registry into four types: mobility (physical and brain impairments), sensory (visual and auditory impairments), mental (mental retardation, developmental disability, and mental illness), and chronic conditions including renal function impairment. Severity of disability, which was graded from 1 (very severe) to 6 (very mild), was reclassified as severe (Grades 1 and 2) and moderate (Grades 3 to 6, not registered).
Methodology
We examined differences in sample characteristics and healthcare expenditures between households with members with disabilities compared to those without members with disabilities with chi-square and t-tests respectively. We used descriptive analysis to capture the occurrence of catastrophic health expenditures and multiple logistic regression models to identify determinants of catastrophic healthcare expenditures. Because there is a difference only in link function between probit and logit, we chose logit modeling, which is more common in the literature on catastrophic health expenditures. Adjusted odds ratios (OR) were presented with 95% confidence intervals (CI). For analysis, we used PASW Statistics for Windows, Version 18.0 (IBM Corporation, NY, USA).
Ethics statement
This study was exempted from the institutional review board at the Seoul National University Hospital because it analyzed secondary data already released to the public (IRB No. 1501-284-901).
RESULTS
Sample characteristics
As shown in Table 1, there was a significant difference in characteristics between the households with and without members with disabilities. Lower income groups (the first and second quintiles) of the five income quintiles comprised 61.2% of households with members with disabilities, compared with 36.7% of households without such members. The proportion of households with members with disabilities increased as household income quintiles decreased, which is the reverse of households without members with disabilities. Receiving public assistance was related to the presence of a family member with disabilities. The proportion of households having a member with chronic disease including neoplasm, hypertension, cerebrovascular disease, diabetes, and arthritis were higher in households with members with disabilities than in households without such a person. The characteristics of heads of household were also associated with the presence of a household member with disabilities. Households with members with disabilities were more likely to have heads of households aged 65 or more and not working which means lower economic capability.
Table 1. Characteristics of subjects.
| Characteristics | Households with members with disabilities | Households without members with disabilities | χ2 | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Total (n = 5,610) | 800 | 14.3 | 4,810 | 85.7 | |
| Number of household members | |||||
| 1 person | 613 | 12.7 | 94 | 11.8 | 130.880* |
| 2 persons | 1206 | 25.1 | 328 | 41.0 | |
| 3 persons | 907 | 18.9 | 155 | 19.4 | |
| 4 persons | 1566 | 32.6 | 125 | 15.6 | |
| ≥ 5 persons | 518 | 10.8 | 98 | 12.3 | |
| Household income quintiles | |||||
| Q1 (poorest) | 282 | 35.3 | 847 | 17.6 | 194.405* |
| Q2 | 207 | 25.9 | 920 | 19.1 | |
| Q3 | 122 | 15.3 | 983 | 20.4 | |
| Q4 | 101 | 12.6 | 1,023 | 21.3 | |
| Q5 (richest) | 88 | 11.0 | 1,035 | 21.5 | |
| Public assistance | |||||
| Yes | 146 | 18.3 | 190 | 4.0 | 249.106* |
| No | 654 | 81.8 | 4,620 | 96.0 | |
| Having a member over 65 years | |||||
| Yes | 519 | 64.9 | 1,582 | 32.9 | 299.562* |
| No | 281 | 35.1 | 3,228 | 67.1 | |
| Household head's age, yr | |||||
| < 65 | 398 | 49.8 | 3,597 | 74.8 | 209.647* |
| ≥ 65 | 402 | 50.3 | 1,213 | 25.2 | |
| Household head's employment status | |||||
| Working | 429 | 53.6 | 3,765 | 78.3 | 220.861* |
| Not working | 371 | 46.4 | 1,045 | 21.7 | |
| Having a member with neoplasm | |||||
| Yes | 91 | 11.4 | 384 | 8.0 | 10.181† |
| No | 709 | 88.6 | 4,426 | 92.0 | |
| Having a member with hypertension | |||||
| Yes | 461 | 57.6 | 1,651 | 34.3 | 158.643* |
| No | 339 | 42.4 | 3,159 | 65.7 | |
| Having a member with cerebrovascular disease | |||||
| Yes | 140 | 17.5 | 171 | 3.6 | 254.727* |
| No | 660 | 82.5 | 4,639 | 96.4 | |
| Having a member with diabetes | |||||
| Yes | 202 | 25.3 | 684 | 14.2 | 62.745* |
| No | 598 | 74.8 | 4,126 | 85.8 | |
| Having a member with arthritis | |||||
| Yes | 348 | 43.5 | 1,078 | 22.4 | 160.906* |
| No | 452 | 56.5 | 3,732 | 77.6 | |
*P < 0.001, † P < 0.01.
Of households with one or more members with disabilities, 9.5% had two or more members with a disability (Table 2). We noted that information of the first household member with a disability was used for analysis in the case of households with two or more members with a disability. The majority of people with disabilities had mobility disabilities, followed by sensory disabilities, mental disabilities, and chronic conditions; most had moderate disabilities. They were more likely to be heads of households, not working, and receive medical aid.
Table 2. Characteristics of household with members with disabilities*.
| Characteristics | No. of households | % |
|---|---|---|
| Type of disability | ||
| Mobility | 553 | 69.1 |
| Sensory | 160 | 20.0 |
| Mental | 64 | 8.0 |
| Chronic condition | 23 | 2.9 |
| Severity of disability | ||
| Severe | 177 | 22.1 |
| Moderate | 575 | 71.9 |
| Not registered | 48 | 6.0 |
| Relationship with the head of the household | ||
| Self | 488 | 61.0 |
| Spouse | 162 | 20.3 |
| Child | 81 | 10.1 |
| Others | 69 | 8.6 |
| Over 65 years | ||
| No | 401 | 50.1 |
| Yes | 399 | 49.9 |
| Employment status | ||
| Working | 285 | 35.6 |
| Not working | 496 | 62.0 |
| NA | 19 | 2.4 |
| Medical security | ||
| National health insurance | 606 | 75.8 |
| Medical aid | 173 | 21.6 |
| Others | 21 | 2.6 |
*In the case of households with two or more members with a disability, information of the first household member with a disability was used for analysis. NA, not applicable.
Out-of-pocket healthcare expenditure
Households with disabled members reported annual OOP healthcare expenditures of 1,465.10 USD, which was 1.29 times higher than households without disabled members. Table 3 presents means for four basic components of healthcare expenditures by service types: emergency, inpatient, and outpatient services, and prescription drugs. Households with members with disabilities spend more for inpatient services and prescription drugs than those without members with disabilities. Conversely, expenditures for outpatient services were higher in households without members with disabilities. The financial burden of OOP spending as a proportion of living costs except food was 1.77 times greater for households with members with disabilities compared with those without such members.
Table 3. Average out-of-pocket healthcare expenditures and non-food consumption.
| Spending type | Expenditures (USD*) | Ratio‡ | t-test | ||||
|---|---|---|---|---|---|---|---|
| Households with disabled members | Households without disabled members | ||||||
| Mean | SD | Portion† | Mean | SD | |||
| Total OOP spending (A) | 1,465.1 | 1,995.1 | 0.54 | 1,136.7 | 1,647.7 | 1.29 | 4.413§ |
| Emergency | 22.3 | 172.1 | 0.07 | 16.6 | 109.8 | 1.35 | 0.914 |
| Inpatient | 552.3 | 1,349.10 | 0.51 | 276.7 | 1,034.00 | 2.00 | 5.515§ |
| Outpatient | 630.8 | 952.9 | 0.22 | 669.1 | 1,095.40 | 0.94 | -0.930 |
| Prescription drugs | 269.3 | 355.8 | 0.50 | 180.9 | 228.4 | 1.49 | 6.672§ |
| Non-food consumption (B) | 11,969.1 | 10,007.8 | 16,852.4 | 11,759.3 | 0.71 | -12.446§ | |
| OOP spending share in non-food consumption (A)/(B) | 0.20 | 0.34 | 0.11 | 0.28 | 1.77 | 6.632§ | |
*Calculated at the exchange rate of 1,102.3 Korean won (KRW) to the United States dollars (USD) as on February 16, 2015. †Mean value of OOP expenditures of members with disabilities divided by those of total household members in a household with members with disabilities. ‡mean OOP expenditures of households with members with disabilities divided by those of households without members with disabilities. §P < 0.001. OOP, out-of-pocket.
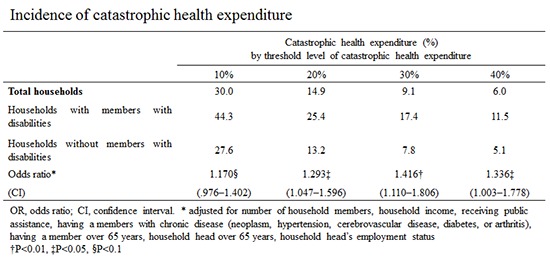
Catastrophic health expenditures
Table 4 presents the incidence of catastrophic health expenditures for households with and without members with disabilities and by disability characteristics. Households with members with disabilities spent a higher ratio of annual living expenditures on OOP expenses compared to households without members with disabilities. The occurrence of catastrophic health expenditure in the households without disabled members was 27.6%, 13.2%, 7.8%, and 5.1% with the threshold at 10%, 20%, 30% and 40% respectively. Meanwhile, those with one or more members with disabilities spent 44.3%, 25.4%, 17.4%, and 11.5%.
Table 4. Incidence of catastrophic health expenditure.
| Households and disabilities | Catastrophic health expenditure (%) by threshold level of catastrophic health expenditure | ||||
|---|---|---|---|---|---|
| 10% | 20% | 30% | 40% | ||
| Total households | 30.0 | 14.9 | 9.1 | 6.0 | |
| Without members with disabilities | 27.6 | 13.2 | 7.8 | 5.1 | |
| With members with disabilities | 44.3 | 25.4 | 17.4 | 11.5 | |
| χ2 | 90.223* | 80.703* | 76.543* | 49.399* | |
| Type of disability | |||||
| Mobility | 47.4 | 26.6 | 17.9 | 11.4 | |
| Sensory | 37.5 | 23.1 | 16.3 | 11.9 | |
| Mental | 28.1 | 14.1 | 9.4 | 9.4 | |
| Chronic condition | 60.9 | 43.5 | 34.8 | 17.4 | |
| χ2 | 14.469† | 9.159‡ | 7.956‡ | 1.097 | |
| Severity of disability | |||||
| Severe | 44.1 | 27.7 | 18.6 | 13.0 | |
| Moderate | 44.3 | 24.7 | 17.0 | 11.1 | |
| χ2 | 0.003 | 0.640 | 0.255 | 0.499 | |
*P < 0.001, † P < 0.01, ‡ P < 0.05.
Disability type of members with disabilities was associated with catastrophic healthcare expenditures. Households with members with physical disabilities or chronic conditions were more likely to experience catastrophic healthcare expenditures than those with members with visual or auditory impairment and mental illness. However, with the threshold of 40%, there was no significant difference in incidence of catastrophic health expenditure by disability type. On the other hand, severity of disability did not make a difference of catastrophic health expenditures.
Table 5 presents the results from the logistic regression analysis conducted to identify the impact of having one or more member with a disability on incidence of catastrophic healthcare expenditures in entire households, after adjusting for other explanatory variables. We included control variables of number of household members, household income, receiving public assistance, having a member over 65 years, household head over 65 years, household head’s employment status, and having household members with chronic diseases (neoplasm, hypertension, cerebrovascular disease, diabetes, or arthritis). The model goodness-of-fit based on the Hosmer-Lemeshow test was satisfactory with all threshold levels (10%, 20%, 30%, and 40%).
Table 5. Factors associated with incidence of catastrophic health expenditures.
| Variables | Catastrophic health expenditure (%) by threshold level of catastrophic health expenditure | |||||||
|---|---|---|---|---|---|---|---|---|
| 10% | 20% | 30% | 40% | |||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Having one or more member with a disability (y = 1) | 1.170§ | (0.976-1.402) | 1.293‡ | (1.047-1.596) | 1.416† | (1.110-1.806) | 1.336‡ | (1.003-1.778) |
| Number of household members (ref: 1 person) | ||||||||
| 2 persons | 1.618* | (1.313-1.993) | 1.566* | (1.233-1.990) | 1.537† | (1.164-2.031) | 1.614† | (1.160-2.247) |
| 3 persons | 1.215 | (0.951-1.553) | 1.016 | (0.747-1.383) | 0.944 | (0.644-1.382) | 0.947 | (0.592-1.515) |
| 4 persons | 1.032 | (0.802-1.328) | 0.866 | (0.621-1.208) | 0.804 | (0.524-1.232) | 0.906 | (0.538-1.524) |
| 5 persons | 1.410‡ | (1.060-1.875) | 0.875 | (0.589-1.300) | 0.893 | (0.538-1.483) | 0.967 | (0.516-1.812) |
| Household income quintiles (ref: Q5) | ||||||||
| Q1 (poorest) | 3.604* | (2.822-4.604) | 4.123* | (2.954-5.753) | 5.867* | (3.632-9.478) | 5.555* | (3.137-9.837) |
| Q2 | 2.384* | (1.914-2.970) | 2.531* | (1.836-3.490) | 3.700* | (2.308-5.931) | 2.900* | (1.639-5.132) |
| Q3 | 1.594* | (1.276-1.990) | 1.678† | (1.201-2.346) | 2.146† | (1.304-3.531) | 1.845‡ | (1.008-3.376) |
| Q4 | 1.099 | (0.871-1.386) | 1.093 | (0.760-1.572) | 1.467 | (0.858-2.508) | 1.466 | (0.774-2.778) |
| Receiving public assistance (y = 1) | 0.327* | (0.247-0.434) | 0.247* | (0.171-0.358) | 0.286* | (0.185-0.441) | 0.252* | (0.146-0.436) |
| Having a member over 65 years(y = 1) | 1.095 | (0.869-1.380) | 1.128 | (0.829-1.535) | 0.877 | (0.578-1.328) | 0.852 | (0.503-1.443) |
| Household head aged over 65 years (y = 1) | 1.380† | (1.086-1.755) | 1.345§ | (0.994-1.818) | 1.875† | (1.259-2.794) | 2.088† | (1.260-3.460) |
| Household head's employment status (working = 1) | 0.741* | (0.630-0.872) | 0.611* | (0.506-0.738) | 0.658* | (0.526-0.824) | 0.632† | (0.485-0.825) |
| Having a member with neoplasm (y=1) | 2.006* | (1.620-2.484) | 2.379* | (1.865-3.036) | 2.135* | (1.601-2.846) | 2.306* | (1.669-3.187) |
| Having a member with hypertension (y=1) | 1.407* | (1.217-1.627) | 1.338† | (1.114-1.609) | 1.323‡ | (1.056-1.657) | 1.256§ | (0.959-1.646) |
| Having a member with cerebrovascular disease (y=1) | 1.946* | (1.493-2.537) | 1.487† | (1.117-1.979) | 1.338§ | (0.965-1.855) | 1.384§ | (0.953-2.010) |
| Having a member with diabetes (y=1) | 1.636* | (1.381-1.938) | 1.413† | (1.160-1.722) | 1.413† | (1.122-1.779) | 1.392‡ | (1.063-1.823) |
| Having a member with arthritis (y=1) | 1.602* | (1.377-1.863) | 1.543* | (1.288-1.849) | 1.526* | (1.230-1.894) | 1.362‡ | (1.054-1.760) |
| Likelihood ratio test | 1098.022* | 876.195* | 665.516* | 467.729* | ||||
| Hosmer-Lemeshow goodness-of-fit test | 10.343 | 5.473 | 6.225 | 4.499 | ||||
| Nagelkerke R2 | 0.252 | 0.254 | 0.245 | 0.219 | ||||
*P < 0.001, † P < 0.01, ‡ P < 0.05, § P < 0.1. OR, odds ratio; CI, confidence interval; ref, reference; y, yes.
The result indicates about 1.2 to 1.4 times greater likelihood at different threshold levels in households with members with disabilities compared to those without, even controlling for key variables that are known to influence catastrophic health expenditure. Household size, household income, receiving public assistance, household head’s age and employment status, and having a member with chronic diseases were statistically significant. Number of household members had a negative association with catastrophic health expenditures at the all threshold levels. Households with two persons were more likely to experience financial burden due to medical expenses than single households. Low household income was a high-risk factor for experiencing catastrophic healthcare expenditures at the all threshold levels. Compared with households in the top 20% of the household income quintiles (Q5), those in the lowest (Q1) household income quintiles were about four to five times as likely to experience catastrophic healthcare expenditures. Households whose heads were over 65 or not working were more likely to incur catastrophic health expenses. The presence of a member with chronic disease in a household increased the odds of catastrophic health expenditures by 1.3 to 2.4 times at different thresholds and by different chronic diseases.
DISCUSSION
This study revealed that households with members with disabilities had higher healthcare expenditures than those without members with disabilities. In general, people with disabilities use more healthcare services and make more payments for medical services due to disabling and secondary conditions than the general population (12,17,25,26). In particular, expenditures for total healthcare and inpatient service were greater for households with members with disabilities than those for their counterparts, while costs for outpatient services were the opposite. Lack of physical and psychosocial access to medical services would prevent people with disabilities from outpatient visits whenever they were needed, resulting in hospitalization due to their worsening conditions. Their vulnerable health status and lack of early treatment may require more resource-intensive services and therefore more spending for medical services (12). This finding suggests that preventive approaches for people with disability are crucial to reduce medical costs at both the individual and social level as well as to promote their health.
We also found that a considerable proportion of families with one or more members with disabilities face the catastrophic financial burden of medical expenses. Almost half of households with members with disabilities (44.3%) reported spending more than 10% of their living expenditures for healthcare. Conservatively, one in ten households with members with disabilities paid 40% more. Families with members with disabilities spent about 1.2 to 1.4 times more on annual living expenditures for OOP spending compared to households without members with disabilities. Having one or more member with disabilities was a statistically significant risk factor of catastrophic health expenditure, even after controlling for various variables known to be associated with it in previous research. This is consistent with previous studies that demonstrated that having members with disabilities in the household increases risk of catastrophe (7,8,11). It was also the same for children with disabilities (14,20) and for persons with mental health problems (19). Factoring in that people with disabilities underutilize medical services due to limited access or economic reasons (27,28), the disparity between households with and without members with disabilities resulting from financial considerations would actually be greater. Higher financial burdens measured relative to their capacity to pay results from not only OOP healthcare expenses but also lower household incomes in families with members with disabilities. High healthcare expenditure and low capacity to pay can lead to impoverishment. On the other hand, families with members with disabilities can choose to underutilize healthcare services or reduce consumption of other items for family members with or without disabilities owing to economic burden (29). Consequentially, spending excessive OOP health expenditure may provoke households with members with disabilities to reduce quality of life for all household members.
Differences in incidence of catastrophic health expenditures were also found in type but not severity of disability. There was a tendency that people with chronic conditions or mobility disabilities were more likely to be at risk of catastrophic health expenditure than those with sensory or mental disabilities. They were not statistically significant, after adjusting for variables such as household income or chronic disease (not shown). A previous study showed a similar pattern that elderly households with people with sensory or mental disabilities reported lower occurrence rate of catastrophic health expenditure than those with physical disabilities with a10% threshold (31). However, because we had a relatively small frequency of each type of disability who experienced catastrophic health expenditure with higher levels of threshold, careful interpretation is required. The existing study results on severity of disability are not consistent (15,31). Palmer and colleagues (15) reported that disability degree was strongly related to the use and economic burdens of healthcare; that is, people who require assistance eating or toileting experienced high healthcare costs. In addition, persistently disabled working age adults had higher total expenditures and proportion of family income spent as OOP expenses than the temporarily disabled who were more likely to employed, less likely to be poor, and more likely to be privately insured (26). On the other hand, Roh (31) reported households with elderly with severe disability in Korea, compared to those with moderate disability, did not have higher prevalence of catastrophic health expenditure like our results, but higher likelihood to remain exposed to catastrophic health expenditure at high threshold levels. One explanation of this finding is that because the incidence of catastrophic health expenditure showed different patterns by both type and severity among our sample, it offset the effects. For example, people with severe disability had slightly higher financial burden of medical expenses than those with moderate disability among the physically disabled with threshold at 10%, while it did the opposite among people with sensory, mental, or chronic conditions. The results of additional analysis by both type and severity also indicated that people with moderate rather than severe disabilities had more individual and household medical expenditures among those with physical, visual, mental disabilities, or chronic conditions (not shown). This was similar to a study on healthcare costs of people with physical disabilities (32). People with severe mobility problems cannot receive medical services without help when they need to visit hospitals. However, we cannot identify the reasons for medical expenditure by disability characteristics. Further study is required with large samples by disability type subgroups.
The result of multiple logistic analyses showed that household income and socioeconomic status was an important determinant of catastrophic expenses. The bottom 20% quintile faced about four to six times greater risk of catastrophic health expenditure compared to the top 20% at all threshold levels. Having household heads who were over 65 years or did not participate in economic activity also was associated with financial burden. Catastrophic health expenditures for families in low economic statuses, in turn, may cause reduced use of medical services and higher health vulnerability. Having a household member with chronic diseases was a factor differentiating the incidence of catastrophic health expenditures. This is similar to previous studies (10,22,30). In particular, households having a member with neoplasm had a higher risk of incurring catastrophic health expenditure than with other chronic disease. A previous study reported that in the early stage after cancer diagnosis, medical costs were high and catastrophic health expenditures were likely to occur (21). Our findings suggested that households with members with disabilities and with a chronic condition could be the priority target of support for OOP spending.
Meanwhile, public assistance played a crucial role in reducing the economic burdens of healthcare experienced. Exemption or reduction of OOP payment by medical aid reduced the economic burden of medical spending, which is a finding consistent with previous research (21,26). Relatively more households with members with disabilities known in this sample (18.3%) were receiving economic benefits from public assistance than those without members with disabilities (4%). However, because Korean medical aid is targeting only people below the poverty line or with specific conditions, many people with disabilities are exposed to risk of excessive medical expenses, resulting in low quality of life and impoverishment. Of course, the Korean National Health Insurance system is required for a reduction in co-payments and expansion of benefit coverage to achieve universal health coverage. Economically marginalized households with great health needs need additional financial support to use medical services without suffering financial hardship.
This study has several limitations. First, the incidence of catastrophic healthcare expenditure depends on the definition or measurement of the capacity to pay and medical expenditures. The former can be measured with household income, consumption expenditure, and consumption expenditure minus real or expected food expenditure. The latter differs from formal medical costs expended in health care institutions, such as charges for emergencies, inpatient and outpatient care and prescription drugs, to informal ones including over-the-counter drug and health supplements (33). Because the study results may differ according to data source researcher use, careful consideration is needed to compare the incidence of catastrophic health expenditure between studies. Second, recall bias may prevent capture of the complete healthcare expenditure of each household because the KHP survey collected data by self-report. While other data sources used for research on catastrophic health expenditure in Korea have the same limitations, we used the KHP dataset in that it used complementary diary methods to reduce recall bias and provided comprehensive information as a dataset specialized in health service use and expenditure.
We proved the financial burden of medical services for households with members with disabilities compared with those without members with disabilities using representative household survey data. We found that household with members with disabilities are more likely to face catastrophic health expenditures. By developing policies to reduce OOP payments and protect households with members with disabilities from catastrophic health expenditures, health disparities as well as differences in health service use between people with and without disabilities would be reduced.
Although Korea has national health insurance and a medical aid program for the poor, the Korean government faces high OOP payments and numbers of households with catastrophic health expenditures. Catastrophic financial burdens of health expenditures are an especially critical issue to households with members with disabilities because people with disabilities have higher healthcare use and expenses but lower economic status. Our findings suggest that one strategy to reduce OOP expenditure is to increase financial support for households with members with disabilities in order to protect them from catastrophic burdens of medical spending and impoverishment. This study can be used to ensure better access to health services and a higher degree of financial protection for low-income disability groups against the economic impact of illness.
Footnotes
Funding: This study was supported by Seoul National University Bundang Hospital Research Fund (grant No. 13-2014-009).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design: Lee JE, Shin HI, Do YK. Analysis and interpretation of data: Lee JE, Shin HI, Yang EJ. Writing or revision of the manuscript: Lee JE, Shin HY. Manuscript approval: all authors.
References
- 1.Organization for Economic Cooperation and Development. Health at a glance 2013: OECD indicators. [accessed on 26 May 2015]. Available at http://dx.doi.org/10.1787/health_glance-2013-en.
- 2.Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24:63–71. doi: 10.1093/heapol/czn037. [DOI] [PubMed] [Google Scholar]
- 3.van Doorslaer E, O’Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, Harbianto D, Herrin AN, Huq MN, Ibragimova S, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16:1159–1184. doi: 10.1002/hec.1209. [DOI] [PubMed] [Google Scholar]
- 4.Xu K. Distribution of health payments and catastrophic expenditures methodology: discussion paper number 2-2005. [accessed on 26 May 2015]. Available at http://apps.who.int/iris/bitstream/10665/69030/1/EIP_HSF_DP_05.2.pdf.
- 5.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 6.Gotsadze G, Zoidze A, Rukhadze N. Household catastrophic health expenditure: evidence from Georgia and its policy implications. BMC Health Serv Res. 2009;9:69. doi: 10.1186/1472-6963-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kronenberg C, Barros PP. Catastrophic healthcare expenditure - drivers and protection: the Portuguese case. Health Policy. 2014;115:44–51. doi: 10.1016/j.healthpol.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Amaya Lara JL, Ruiz Gómez F. Determining factors of catastrophic health spending in Bogota, Colombia. Int J Health Care Finance Econ. 2011;11:83–100. doi: 10.1007/s10754-011-9089-3. [DOI] [PubMed] [Google Scholar]
- 9.Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage. Health Aff (Millwood) 2009;28:w467–78. doi: 10.1377/hlthaff.28.3.w467. [DOI] [PubMed] [Google Scholar]
- 10.Su TT, Kouyaté B, Flessa S. Catastrophic household expenditure for health care in a low-income society: a study from Nouna District, Burkina Faso. Bull World Health Organ. 2006;84:21–27. doi: 10.2471/blt.05.023739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yardim MS, Cilingiroglu N, Yardim N. Catastrophic health expenditure and impoverishment in Turkey. Health Policy. 2010;94:26–33. doi: 10.1016/j.healthpol.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Anderson WL, Wiener JM, Finkelstein EA, Armour BS. Estimates of national health care expenditures associated with disability. J Disabil Policy Stud. 2011;21:230–240. [Google Scholar]
- 13.Mitra S, Findley PA, Sambamoorthi U. Health care expenditures of living with a disability: total expenditures, out-of-pocket expenses, and burden, 1996 to 2004. Arch Phys Med Rehabil. 2009;90:1532–1540. doi: 10.1016/j.apmr.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114:79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- 15.Palmer M, Nguyen T, Neeman T, Berry H, Hull T, Harley D. Health care utilization, cost burden and coping strategies by disability status: an analysis of the Viet Nam National Health Survey. Int J Health Plann Manage. 2011;26:e151–68. doi: 10.1002/hpm.1052. [DOI] [PubMed] [Google Scholar]
- 16.Wyszewianski L. Families with catastrophic health care expenditures. Health Serv Res. 1986;21:617–634. [PMC free article] [PubMed] [Google Scholar]
- 17.Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004;94:443–445. doi: 10.2105/ajph.94.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi J, Wheeler KK, Lu B, Bishai DM, Stallones L, Xiang H. Medical expenditures associated with nonfatal occupational injuries among U.S. workers reporting persistent disabilities. Disabil Health J. 2015;8:397–406. doi: 10.1016/j.dhjo.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Zuvekas SH, Selden TM. Mental health and family out-of-pocket expenditure burdens. Med Care Res Rev. 2010;67:194–212. doi: 10.1177/1077558709345499. [DOI] [PubMed] [Google Scholar]
- 20.Lukemeyer A, Meyers MK, Smeeding T. Expensive children in poor families: out-of-pocket expenditures for the care of disabled and chronically ill children in welfare families. J Marriage Fam. 2000;62:399–415. [Google Scholar]
- 21.Choi JW, Cho KH, Choi Y, Han KT, Kwon JA, Park EC. Changes in economic status of households associated with catastrophic health expenditures for cancer in South Korea. Asian Pac J Cancer Prev. 2014;15:2713–2717. doi: 10.7314/apjcp.2014.15.6.2713. [DOI] [PubMed] [Google Scholar]
- 22.Rahman MM, Gilmour S, Saito E, Sultana P, Shibuya K. Health-related financial catastrophe, inequality and chronic illness in Bangladesh. PLoS One. 2013;8:e56873. doi: 10.1371/journal.pone.0056873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim Y, Yang B. Relationship between catastrophic health expenditures and household incomes and expenditure patterns in South Korea. Health Policy. 2011;100:239–246. doi: 10.1016/j.healthpol.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Ruger JP, Kim HJ. Out-of-pocket healthcare spending by the poor and chronically ill in the Republic of Korea. Am J Public Health. 2007;97:804–811. doi: 10.2105/AJPH.2005.080184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan L, Beaver S, Maclehose RF, Jha A, Maciejewski M, Doctor JN. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil. 2002;83:1196–1201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 26.Pumkam C, Probst JC, Bennett KJ, Hardin J, Xirasagar S. Health care expenditures among working-age adults with physical disabilities: variations by disability spans. Disabil Health J. 2013;6:287–296. doi: 10.1016/j.dhjo.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Iezzoni LI, Killeen MB, O’Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Serv Res. 2006;41:1258–1275. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JE, Kim HR, Shin HI. Accessibility of medical services for persons with disabilities: comparison with the general population in Korea. Disabil Rehabil. 2014;36:1728–1734. doi: 10.3109/09638288.2013.867368. [DOI] [PubMed] [Google Scholar]
- 29.Altman BM, Cooper PF, Cunningham PJ. The case of disability in the family: impact on health care utilization and expenditures for nondisabled members. Milbank Q. 1999;77:39–75. doi: 10.1111/1468-0009.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee TJ, Lee HJ, Kim Y. Analysis of catastrophic health expenditures using 1st wave Korea health panel data. Korean J Health Econ Policy. 2012;18:95–111. [Google Scholar]
- 31.Roh SH. The longitudinal study on the factors of catastrophic health expenditure among disabled elderly households. Korean J Soc Welf. 2012;64:51–77. [Google Scholar]
- 32.Lee JY, Kim BK, Eun SJ, Kim Y, Kim YI. Healthcare expenditures of disabled households in Seoul, Korea. J Rehabil Res. 2009;13:199–223. [Google Scholar]
- 33.Jung YI, Lee HJ, Lee TJ, Kim H. Measures of household catastrophic health expenditure: systematic review and implications. Korean J Health Econ Policy. 2013;19:1–27. [Google Scholar]


