Abstract
Background
Although Vietnam has taken great efforts to reduce child mortality in recent years, a large number of children still die at early age. Only a few studies have been conducted to identify at-risk groups in order to provide baseline information for effective interventions.
Objective
The study estimated the overall trends in infant mortality rate (IMR) and under-five mortality rate (U5MR) during 1986–2011 and identified demographic and socioeconomic determinants of child mortality.
Design
Data from the Vietnam Multiple Indicator Cluster Surveys (MICSs) in 2000 (MICS2), 2006 (MICS3) and 2011 (MICS4) were analysed. The IMR and U5MR were calculated using the indirect method developed by William Brass. Unadjusted and adjusted odds ratios were estimated to assess the association between child death and demographic and socioeconomic variables. Region-stratified stepwise logistic regression was conducted to test the sensitivity of the results.
Results
The IMR and U5MR significantly decreased for both male and female children between 1986 and 2010. Male children had higher IMR and U5MR compared with females in all 3 years. Women who were living in the Northern Midlands and Mountain areas were more likely to experience child deaths compared with women who were living in the Red River Delta. Women who were from minor ethnic groups, had low education, living in urban areas, and had multiple children were more likely to have experienced child deaths.
Conclusion
Baby boys require more healthcare attention during the first year of their life. Comprehensive strategies are necessary for tackling child mortality problems in Vietnam. This study shows that child mortality is not just a problem of poverty but involves many other factors. Further studies are needed to investigate pathways underlying associations between demographic and socioeconomic conditions and childhood mortality.
Keywords: infant mortality, under-five mortality, MICS, Vietnam, survey analysis, mortality trends
Introduction
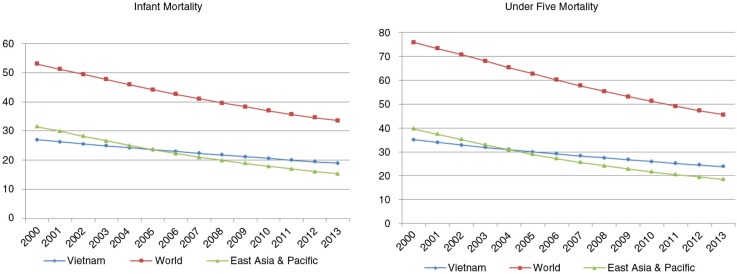
The under-five mortality rate (U5MR) and the infant mortality rate (IMR) have both fallen significantly in developing countries since the declaration of Millennium Development Goals (MDGs) in 2000. However, infant health remains a serious public health problem in Vietnam (1). In an effort to achieve MDG4 to reduce the child mortality, Vietnam reduced U5MR from 58 per 1,000 live births in 1990 to 24 per 1,000 in 2009 (2). In spite of this, since 2005, the IMR and U5MR in Vietnam have been higher than the average for countries in the East Asian and Pacific region. Currently, a large number of children in Vietnam still die before they reach their fifth birthday (see Fig. 1).1,2
Fig. 1.
Trends in IMR and U5MR in Vietnam, regions and the world.
In order to achieve significant reductions in childhood mortality in Vietnam, it is important to identify the vulnerable groups who have social characteristics strongly associated with childhood mortality so that appropriate action can be taken. However, to date, there have been limited epidemiological studies on this subject. Nga et al. identified the causes of neonatal death in Quang Ninh province and analysed this distribution by age at death, birth weight, and place of delivery from a clinical perspective (3). Pham et al. investigated the patterns of child mortality by gender (4). They found that the mortality rate for boys was much higher than for girls and that this was associated with parents’ educational levels, in particular those of the father. Knowles et al. performed a situational analysis of health inequity in Vietnam focussing on maternal and child mortality and showed that being an ethnic minority was the most important risk factor for high infant mortality (5). Hoa et al. examined the trends in neonatal, infant, and U5MR in a northern district of Vietnam between 1970 and 2000 and analysed socioeconomic differences in child survival over time (6). They identified dramatic reductions in IMR and U5MR during that period but not in the neonatal mortality rate (NMR). They also showed that U5MR and NMR were not associated with households’ economic situation although there was some association with mothers’ education and ethnicity. Swenson et al. investigated the factors influencing infant mortality with a specific focus on community characteristics and found that the most significant predictor of infant mortality was living area (7).
Likewise, previous studies in Vietnam were mostly based in specific regions, thus limiting the generalisability of their results. Others are outdated (3–7). Findings from previous studies have not been sufficient to identify the most vulnerable groups, or specify the types of interventions needed. This study aims to address the evidence gap in relation to taking action to reduce childhood mortality in Vietnam by 1) investigating overall trends in IMR and U5MR (1986–2011) by demographic and socioeconomic factors and 2) identifying the demographic and socioeconomic determinants of the early childhood deaths.
Methods
Data collection
Data from the Vietnam Multiple Indicator Cluster Surveys (MICSs) in 2000 (MICS2), 2006 (MICS3), and 2011 (MICS4) were used in this study. The Vietnam General Statistics Office has conducted the MICS every 5 years as a part of the global MICS programme. The United Nations Children's Fund (UNICEF) provided technical and financial support for all MICSs.
A stratified two-stage cluster sampling was designed to select eligible respondents. Six ecological regions were used as main strata. The primary sampling unit (PSU), a cluster for the survey, was defined on the basis of enumeration areas (EAs) and about 33 households out of 100 were selected in each EA acquiring a sampling probability of one-third. In each survey, there are three structured questionnaires, which are for households, 15–49 year-old women, and under-five year-old children. All the variables used for this study were derived from the women's datasets.
Estimation of IMR and U5MR in Vietnam 1986–2010
To estimate IMR (the number of children dying at less than 1 year of age per 1,000 live births that year) and U5MR (the number of children dying at less than 5 years of age per 1,000 live births that year), the indirect method developed by William Brass in late 1960s (8) and modified by Coale and Trussel later (9) was used here. This method has been widely used in previous studies and provides consistent results with the direct method (10). A brief explanation is as follows:
To begin with, an average parity per woman P(i) and the proportion of dead children D(i) in each age group of women were estimated from the number of children ever born, the number of surviving children, and the number of women belonging to each age group. A multiplier K(i) was estimated for each age group of women [Eq(1)].
| 1 |
Then, the probabilities of dying (q(x)) and the probabilities of surviving (l(x)) were determined as q(x) = K(i)D(i). The reference times were obtained using the model as below [Eq(2)].
| 2 |
The t(i) values were then subtracted from the period of survey to produce the reference date. The a(i), b(i), c(i), e(i), f(i), and g(i) are constant coefficients and were taken from the North model life table (11), which was chosen because mortality patterns of the Vietnamese population are most similar to the North model life family, the one with low child and elderly mortality level (12, 13). Finally, the q(x) values from each group were transformed into 1 q 0 (infant mortality) and 5 q 0 (under-five mortality) for each reference point.
To identify trends of IMR and U5MR, each mortality rate was regressed on reference periods. Because the quadratic term was not significant in the curvature model, the final model was linear. The same procedures were applied to examine the trends in IMR and U5MR across the six regions, urban and rural living areas and maternal educational levels.
Determinants associated with having a child death
Analyses were performed with MICS4 (2011) data because it provided the most recent data and the largest sample size.
The outcome variable is a child death experience reported by mothers. This was derived from answers to a question to the mother about whether she had ever given birth to a child who was born alive but later died.
Demographic and socioeconomic factors available in the MICS women's dataset that had been shown to be associated with child mortality in previous studies were the independent variables (14–17). The region was divided into six categories: Red River Delta; Northern Midlands and Mountain areas; Northern Central area and Central Coastal area; Central Highlands; South East and Mekong River Delta. Mothers’ ages were grouped into three categories; 15–24, 25–34, and 35–49 years. Living area was assessed by asking whether respondents were living in either urban or rural areas. The mothers’ educational level variable comprised three categories: ‘primary of less’ for respondents who reported that their highest level of education was grade five, ‘secondary’ for respondents who reported that their highest level of education was between grade six and twelve, and ‘tertiary’ for respondents who reported that they finished professional school, college or university and above. The household wealth index was used as a proxy for economic status. Wealth scores were derived by Principal Component Analysis using information collected on each household's ownership of consumer goods and amenities in related to household wealth. The scores were divided into quintiles from the poorest to the wealthiest. Mothers’ ethnicity was classified as one of the two groups: Kinh, which is the main ethnic group accounting for about 84% of Vietnamese people, and non-Kinh. Marital status was grouped into two categories: ‘married’ meaning ‘living with a spouse’ and ‘not married’ which included ‘never married’ and ‘widowed/divorced/separated’. It was assumed that the number of times a woman had given birth could be a confounder and therefore the number of children ever born to a mother was also included as a continuous independent variable.
The unit of analysis in this study was the mother. Univariable and multivariable logistic regressions were performed producing unadjusted and adjusted odds ratios (ORs) for each independent variable. We also performed region-stratified, multivariable stepwise logistic regression as a sensitivity analysis. Here, mothers’ education levels were dichotomised as lower level (finished junior high school or less) and higher level (finished senior high school or above). All analyses were carried out using R statistical software (18).
Results
Estimates of IMR and U5MR in Vietnam during 1986–2010
Weighted and non-weighted numbers of women and children ever born, alive, and dead are shown in Table 1. The age distribution of women in this study was roughly consistent with the population pyramid except that the number of women aged 40–44 in MICS3 was larger than the age groups 30–34 and 25–30 years. The number of children ever born and dead was the lowest for women aged 15–19 and 20–24 years. The average number of children ever born decreased consistently across the three time points.
Table 1.
Number of women and children ever born, alive and dead in each age group in Vietnam, 2001, 2006, and 2011
| Survey | Age group | FP(i) | CEB(i) | CA(i) | CD(i) | wFP(i) | wCEB(i) | wCA(i) | wCD(i) |
|---|---|---|---|---|---|---|---|---|---|
| MICS2 | 15–19 | 1,900 | 71 | 68 | 3 | ||||
| 20–24 | 1,398 | 823 | 788 | 35 | |||||
| 25–30 | 1,341 | 2,143 | 2,062 | 81 | |||||
| 30–34 | 1,337 | 3,156 | 3,008 | 148 | |||||
| 35–39 | 1,313 | 4,016 | 3,765 | 251 | |||||
| 40–44 | 1,181 | 4,195 | 3,889 | 306 | |||||
| 45–49 | 782 | 3,166 | 2,899 | 267 | |||||
| MICS3 | 15–19 | 1,839 | 59 | 59 | 0 | 1768.3 | 48.3 | 48.3 | 0.0 |
| 20–24 | 1,391 | 761 | 752 | 9 | 1358.7 | 692.8 | 685.7 | 7.1 | |
| 25–30 | 1,195 | 1,671 | 1,631 | 40 | 1168.0 | 1497.0 | 1465.4 | 31.6 | |
| 30–34 | 1,218 | 2,556 | 2,474 | 82 | 1207.4 | 2409.5 | 2333.0 | 76.5 | |
| 35–39 | 1,273 | 3,182 | 3,056 | 126 | 1306.0 | 3162.2 | 3041.4 | 120.8 | |
| 40–44 | 1,345 | 4,064 | 3,879 | 185 | 1385.1 | 3981.4 | 3803.9 | 177.5 | |
| 45–49 | 1,210 | 4,154 | 3,846 | 308 | 1276.4 | 4214.6 | 3899.3 | 315.3 | |
| MICS4 | 15–19 | 1,760 | 88 | 87 | 1 | 1697.6 | 82.0 | 80.6 | 1.5 |
| 20–24 | 1,632 | 805 | 792 | 13 | 1609.1 | 818.6 | 806.4 | 12.2 | |
| 25–30 | 1,790 | 2,222 | 2,177 | 45 | 1810.4 | 2213.4 | 2175.1 | 38.3 | |
| 30–34 | 1,738 | 3,197 | 3,147 | 50 | 1810.6 | 3308.5 | 3258.1 | 50.4 | |
| 35–39 | 1,642 | 3,629 | 3,509 | 120 | 1661.6 | 3655.9 | 3529.0 | 127.0 | |
| 40–44 | 1,653 | 4,134 | 3,931 | 203 | 1620.8 | 3962.8 | 3781.5 | 181.3 | |
| 45–49 | 1,448 | 4,052 | 3,801 | 251 | 1452.9 | 4033.5 | 3796.6 | 236.8 |
FP(i): Female population; CEB(i): Children ever born; CA(i): Children alive; CD(i): Children dead; wFP(i): weighted Female population; CEB(i): weighted Children ever born; CA(i): weighted Children alive; CD(i): weighted Children dead.
Trends of IMR and U5MR in Vietnam during 1986–2010
Table 2 provides estimates of IMR and U5MR based on the data from Table 1.
Table 2.
IMR and U5MR in Vietnam, 2001, 2006, and 2011
| Survey | Age group (years) | X | Weight | qx | Time Ref | Ref.P | IMR | U5MR |
|---|---|---|---|---|---|---|---|---|
| MICS2 | 15–19 | 1 | 0 | 0.0529 | 0.7150 | 1999.7 | 0.0529 | 0.0794 |
| 20–24 | 2 | 0.2 | 0.0478 | 1.7687 | 1998.6 | 0.0415 | 0.0594 | |
| 25–30 | 3 | 1.2 | 0.0391 | 3.4962 | 1996.9 | 0.0324 | 0.0434 | |
| 30–34 | 5 | 1.2 | 0.0483 | 5.6867 | 1994.7 | 0.0351 | 0.0483 | |
| 35–39 | 10 | 1.2 | 0.0651 | 8.1895 | 1992.2 | 0.0402 | 0.0572 | |
| 40–44 | 15 | 0.8 | 0.0750 | 10.9471 | 1989.5 | 0.0423 | 0.0609 | |
| 45–49 | 20 | 0.4 | 0.0861 | 13.9964 | 1986.4 | 0.0434 | 0.0628 | |
| MICS3 | 15–19 | 1 | 0 | 0.0000 | 0.6008 | 2006.1 | ||
| 20–24 | 2 | 0.2 | 0.0115 | 1.7222 | 2005.0 | 0.0110 | 0.0126 | |
| 25–30 | 3 | 1.2 | 0.0215 | 3.6153 | 2003.1 | 0.0192 | 0.0232 | |
| 30–34 | 5 | 1.2 | 0.0322 | 6.0184 | 2000.7 | 0.0256 | 0.0322 | |
| 35–39 | 10 | 1.2 | 0.0392 | 8.7503 | 1998.0 | 0.0277 | 0.0352 | |
| 40–44 | 15 | 0.8 | 0.0451 | 11.6746 | 1995.0 | 0.0290 | 0.0373 | |
| 45–49 | 20 | 0.4 | 0.0752 | 14.7279 | 1992.0 | 0.0388 | 0.0548 | |
| MICS4 | 15–19 | 1 | 0 | 0.0218 | 0.7951 | 2010.2 | 0.0218 | 0.0268 |
| 20–24 | 2 | 0.2 | 0.0163 | 1.9584 | 2009.0 | 0.0154 | 0.0182 | |
| 25–30 | 3 | 1.2 | 0.0176 | 3.8103 | 2007.2 | 0.0159 | 0.0188 | |
| 30–34 | 5 | 1.2 | 0.0155 | 6.1077 | 2004.9 | 0.0133 | 0.0155 | |
| 35–39 | 10 | 1.2 | 0.0358 | 8.6964 | 2002.3 | 0.0256 | 0.0322 | |
| 40–44 | 15 | 0.8 | 0.0465 | 11.4933 | 1999.5 | 0.0296 | 0.0385 | |
| 45–49 | 20 | 0.4 | 0.0593 | 14.5037 | 1996.5 | 0.0322 | 0.0432 |
qx: probability of children mortality at x years old in specific age group of women; Reference period (Ref.P): year where the mortality rates are applied; Time reference (Time Ref) is the distance between time of conduction survey and reference period.
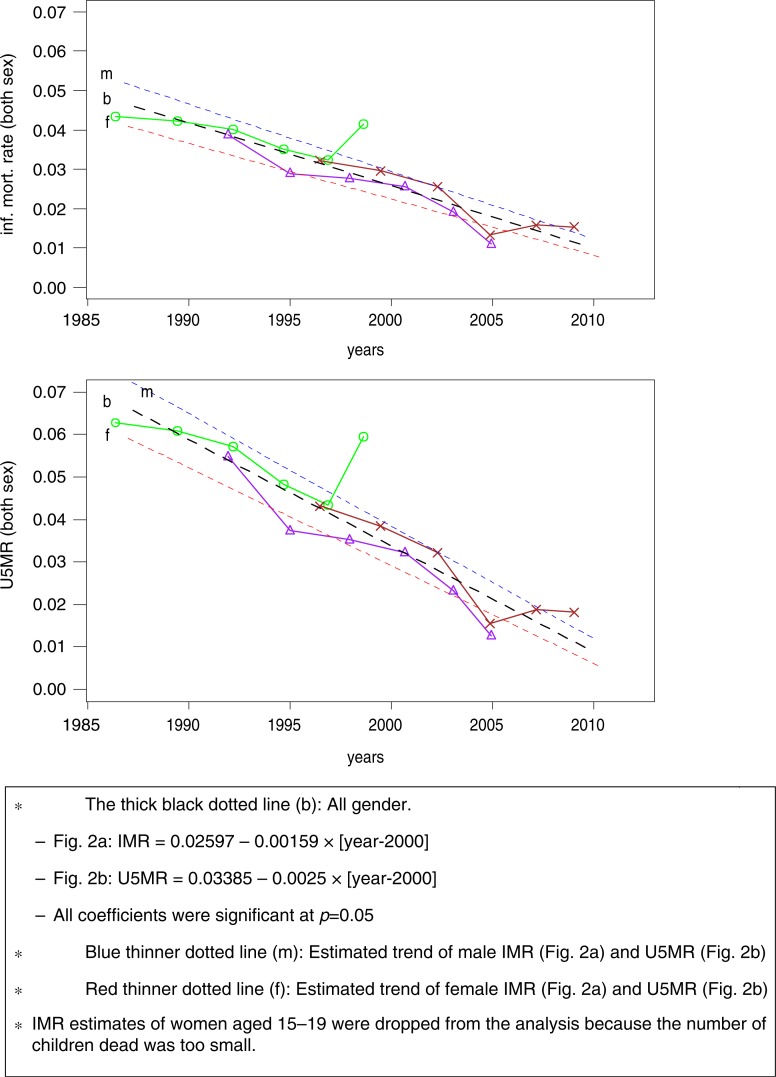
The results of linear regressions are shown in Fig. 2a and b. Regression lines for IMR and U5MR indicate that the number of dead children under age 1 and 5 per 1,000 decreased respectively by 1.6 and 2.5 on average per year. This declining trend occurred among both male and female children. The IMR and U5MR for male children were consistently higher than those for female children between 1986 and 2010.
Fig. 2.
Estimated trends in (a) IMR and (b) U5MR from 1986 to 2010 in Vietnam derived from MICS2 (green line with marked ○), MICS3 (purple line with marked Δ), and MICS4 (brown line with marked ×).
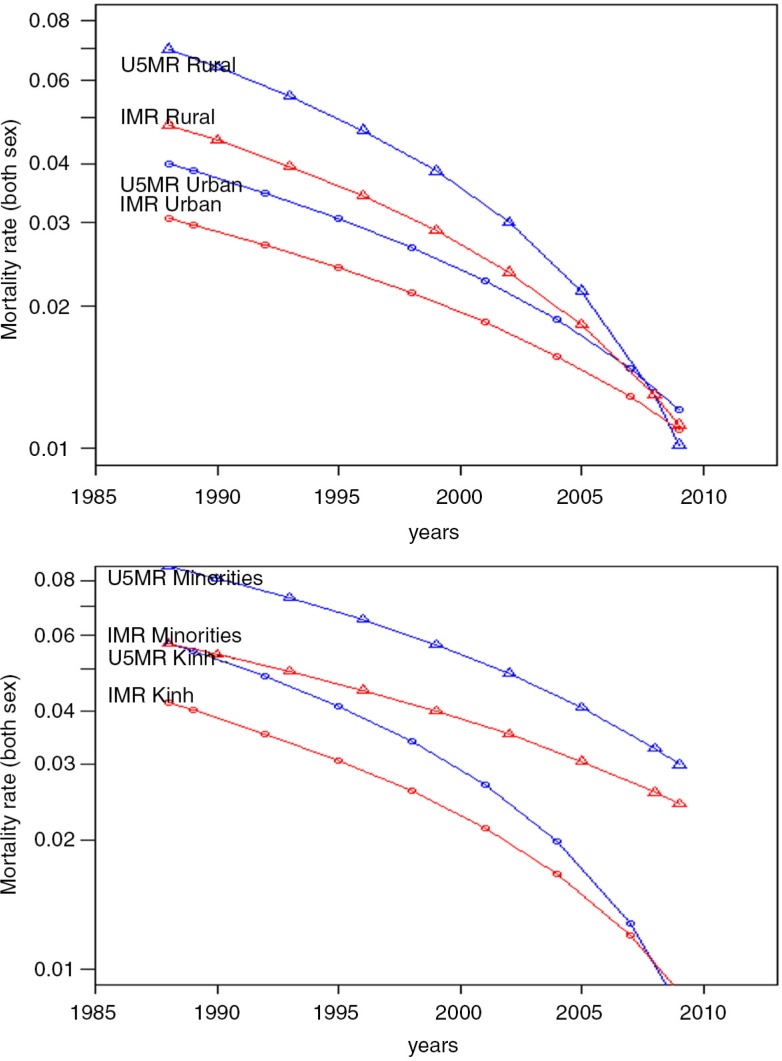
3 presents estimates of the IMR and U5MR in 2000 and regression coefficients by region, living area and mothers’ educational level. Overall, the IMR and U5MR decreased. The large gap in the IMR and U5MR between urban and rural areas (IMR: 0.03 versus 0.05, U5MR: 0.04 versus 0.07) in 1987 narrowed to zero around 2010 (Fig. 3a). However, this was not the case for the gap between the minor and major ethnic groups. Although the IMR and U5MR decreased for both ethnic groups during the same period, the reduction in the Kinh ethnic group was larger, leading to a wider gap between two groups around 2010 (Fig. 3b).
Table 3.
Estimated IMR and U5MR in 2000 and the slopes by region, living area, and education of mother in Vietnam, 1986–2000
| IMR at 2000 | IMR slope | U5MR at 2000 | U5MR slope | |
|---|---|---|---|---|
| Region | ||||
| Red River Delta | 0.0253 | −0.0009 | 0.0332 | −0.0014 |
| Northern Midlands and Mountain areas | 0.0298 | −0.0012 | 0.0400 | −0.0020 |
| Northern Central area and Central Coastal area | 0.0275 | −0.0018 | 0.0365 | −0.0029 |
| Central Highlands | 0.0275 | −0.0017 | 0.0365 | −0.0028 |
| South East | 0.0180 | −0.0010 | 0.0220 | −0.0014 |
| Mekong River Delta | 0.0256 | −0.0023 | 0.0341 | −0.0037 |
| Living area | ||||
| Urban | 0.0194 | −0. 0009 | 0.0240 | −0.0013 |
| Rural | 0.0271 | −0.0018 | 0.0357 | −0.0028 |
| Mother's education | ||||
| Primary | 0.0347 | −0.0022 | 0.0476 | −0.0038 |
| Secondary | 0.0296 | −0.0018 | 0.0396 | −0.0030 |
| Tertiary | 0.0205 | −0.0014 | 0.0258 | −0.0020 |
Fig. 3.
Trends in IMR (red line) and U5MR (blue line) (a) in urban areas (○) and rural areas (Δ) from 1986 to 2010 in Vietnam and (b) in Kinh group (○) and Ethnic Minorities (Δ) from 1986 to 2010 in Vietnam.
Determinants of child mortality
The total number of women aged 15–49 in MICS4 was 12,115, of which 8,179 women had ever given birth to a child. Table 4 presents an overview of child deaths by maternal demographic and socioeconomic characteristics.
Table 4.
Distribution of child deaths by demographic and socioeconomic characteristics in Vietnam, 2011
| Categories | N | Child death (%) |
|---|---|---|
| Region | ||
| Red River Delta | 1,239 | 54 (4) |
| Northern Midlands and Mountain areas | 1,503 | 142 (9) |
| Northern Central area and Central Coastal area | 1,273 | 96 (8) |
| Central Highlands | 1,467 | 117 (8) |
| South East | 1,335 | 57 (4) |
| Mekong River Delta | 1,362 | 86 (6) |
| Mother's age (years) | ||
| 15–24 | 702 | 13 (2) |
| 25–34 | 2,765 | 76 (3) |
| 35–49 | 4,712 | 463 (10) |
| Living area | ||
| Urban | 3,439 | 182 (5) |
| Rural | 4,740 | 370 (8) |
| Mother's education | ||
| Primary or lower | 2,181 | 221 (10) |
| Secondary | 4,817 | 304 (6) |
| Tertiary | 1,181 | 27 (2) |
| Wealth index quintiles | ||
| Poorest | 1,630 | 182 (11) |
| Second | 1,393 | 123 (9) |
| Middle | 1,529 | 95 (6) |
| Fourth | 1,729 | 82 (5) |
| Richest | 1,898 | 69 (4) |
| Ethnicity | ||
| Kinh | 6,860 | 380 (6) |
| Non-Kinh | 1,319 | 172 (13) |
| Marital status | ||
| Currently married | 7,430 | 498 (7) |
| Not married | 749 | 54 (7) |
| Total | 8,179 | 552 (7) |
Overall, the percentage of women who had experienced a child death was less than 10% in most of the categories. However, there were some gradients across categories within variables. For example, of the women who were older, had lower educational levels and lower wealth, higher proportions experienced child mortality.
Table 5 shows the association between child deaths and maternal demographic and socioeconomic factors. With the exception of marital status, all the variables showed a significant association with child death in the unadjusted regression, but this attenuated in the adjusted regression.
Table 5.
Unadjusted and adjusted logistic regression for child deaths in Vietnam, 2011
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
|
|
|
|||
| OR | CI | OR | CI | |
| Region | ||||
| Red River Delta | ||||
| Northern Midlands and Mountain areas | 2.29a | 1.66–3.16 | 1.58a | 1.08–2.32 |
| North Central area and Central Coastal area | 1.79a | 1.27–2.52 | 1.17 | 0.81–1.69 |
| Central Highlands | 1.90a | 1.36–2.65 | 0.81 | 0.55–1.17 |
| South East | 0.98b | 0.67–1.43 | 0.99 | 0.66–1.49 |
| Mekong River Delta | 1.48a | 1.04–2.10 | 1.30 | 0.88–1.92 |
| Mother's age (years) | ||||
| 15–24 | ||||
| 25–34 | 1.50 | 0.83–2.71 | 0.89 | 0.49–1.64 |
| 35–49 | 5.78a | 3.31–10.08 | 1.66 | 0.92–2.98 |
| Number of children | 2.44a | 2.28–2.61 | 2.36a | 2.17–2.56 |
| Living area | ||||
| Urban | ||||
| Rural | 1.52a | 1.26–1.82 | 0.78b | 0.61–0.98 |
| Mother's education | ||||
| Primary or lower | ||||
| Secondary | 0.60a | 0.50–0.72 | 1.52a | 1.18–1.95 |
| Tertiary | 0.21a | 0.14–0.31 | 1.05 | 0.64–1.72 |
| Wealth index | ||||
| Poorest | ||||
| Second | 0.77b | 0.60–0.97 | 1.12 | 0.82–1.51 |
| Middle | 0.52a | 0.40–0.68 | 0.95 | 0.68–1.34 |
| Fourth | 0.39a | 0.30–0.52 | 0.86 | 0.60–1.25 |
| Richest | 0.30a | 0.22–0.40 | 0.74 | 0.49–1.14 |
| Ethnicity | ||||
| Kinh | ||||
| Non-Kinh | 2.56a | 2.11–3.09 | 1.57a | 1.15–2.14 |
| Marital status | ||||
| Currently married | ||||
| Not married | 1.08 | 0.81–1.45 | 0.92 | 0.75–1.13 |
p<0.01
p<0.05.
In multivariable logistic regression, mothers from the Northern Midlands and Mountain areas were more likely to experience child deaths compared with those from the Red River Delta (OR: 1.58, 95% confidence interval [CI] = 1.08–2.32). The number of children ever born to a mother was also significantly associated with the likelihood of a child death. However, the odds of experiencing a child death reduced from 2.44 (95% CI = 2.28–2.61) in the unadjusted regression to 2.36 (95% CI = 2.17–2.56) in the adjusted regression.
Table 6.
Results of region-stratified stepwise logistic regression for child deaths in Vietnam in 2011
| Red River Delta | Northern Midlands and Mountain areas | North Central area and Central Coastal area | Central Highlands | South East | Mekong River Delta | |
|---|---|---|---|---|---|---|
| (Intercept) | 0.0011a | 0.0099a | 0.0054a | 0.0062a | 0.0022a | 0.0067a |
| No children ever born | 4.08a | 3.08a | 2.46a | 1.99a | 2.43a | 2.43a |
| Low education (mothers) | 0.58c | 2.03d | 2.64c | |||
| Minority ethnic | 11.03b | 4.17a | 1.54d | |||
| Rural resident | 0.61c | 0.59c |
p<0.001
p<0.01
p<0.05
p<0.1.
Women who were living in rural areas were more likely to have experienced a child death compared with those living in urban areas (OR: 1.52, 95% CI = 1.26–1.82) in the univariable analysis. However, this association was reversed when adjusting for covariates (OR: 0.78, 95%CI=0.61–0.98). The relationship between mothers’ education level and child death in the univariable regression also reversed when covariates were added. In the multivariable analysis, women who completed secondary school were more likely to experience a child death compared with those who attained primary or lower education (OR: 1.52, 95%CI: 1.18–1.95). In the multivariable analysis, the odds of experiencing a child death was higher for women in minor ethnic groups compared with Kinh women (OR: 1.57, 95%CI: 1.15–2.14).
The direction of the coefficients for the predictor variables across the six regions in the sensitivity analyses remained the same as the main analyses except for education (Table 6). Although low education was associated with higher odds of experiencing a child death in the Central Highlands and South East, it was associated with lower odds of a child death in the Northern Midlands and Mountain areas.
Discussion
The present study estimated the IMR and U5MR and their trends in Vietnam over the period 1986–2010 and investigated demographic and socioeconomic factors associated with child mortality. There are some noteworthy findings.
First, boys showed higher IMRs and U5MRs compared with girls in all years. This is consistent with the research by Hoa et al. who analysed socioeconomic differences in child survival during 1970–2000 (6). They found that boys had higher mortality risks than girls because boys are more vulnerable during their neonatal period, particularly in the case of preterm birth. According to Ingemarsson, preterm baby boys have double risks of dying during their first year compared to baby girls (19). Our finding suggests that antenatal and neonatal care have to be strengthened to improve child mortality and in particular for baby boys.
Second, the falling rates for both IMR and U5MR were much higher in rural areas. This can be explained by the recent reductions in rural poverty rates in Vietnam. For example, the poverty rate in rural areas fell substantially from 66.4% in 1993 to 18.7% in 2008 (20). Although the poverty rate in urban areas also declined during the same period, urban poverty is a relatively recent phenomenon with many urban poor living in recently urbanised peripheral districts in cities. These people are mostly low-income migrants who also suffer from various social problems. As a result, there have been limited opportunities for further reductions of child mortality in urban areas since 2008 (20).
The third intriguing finding is that although the mortality rate decreased significantly in both ethnic groups, the trend in the ethnic minorities was less favourable than the Kinh ethnic group, as seen in Fig. 3b. It is well recognised in Vietnam that ethnic minorities usually lack physical and social assets, and reside in remote areas with limited access to various governmental subsidy programmes and welfare benefits (21, 22). Another possible reason for the slow reduction in child mortality among ethnic minorities has to do with traditional practices including home deliveries, rituals surrounding birth and negative perceptions of healthcare personnel (23). Language barriers can also be a problem, discouraging ethnic minorities from seeking formal healthcare services. As such, slower progress in reducing child mortality rates for ethnic minorities in Vietnam is not only due to poverty but to other social factors.
The results of the analysis, which was intended to identify the determinants of child deaths, also provide a few notable findings. First, compared with women living in the Red River Delta, women in the Northern Midlands and Mountain areas had higher odds of experiencing a child death. The Northern Midlands and Mountain areas have a relatively hot and humid subtropical climate throughout the year. About six to ten hurricanes and tropical depressions causing floods occur annually in those areas. These conditions directly threaten lives, especially the vulnerable, including young children in the region. In addition, mountainous or half-mountainous geographical features may hamper access to healthcare services. Poor and harsh climatic conditions and low accessibility to healthcare services may therefore help explain the higher odds of child mortality in the region.
Unlike some previous studies, those living in rural areas had lower odds of experiencing a child death (22). A plausible explanation for this can be found in emergence of urban poverty, as already mentioned. A mini-crisis in early 2008 in Vietnam had a negative impact on the poor, who were mainly living in marginalised urban areas. In addition, they also suffer from various non-income-related aspects of poverty, such as the hazards of pollution, risks to personal safety, and harsh work and housing conditions (20). These are possible reasons why women living in rural areas were less likely to experience a child death compared with women in urban areas.
A final finding is the positive association between maternal education and child death, which also differs from the results of previous studies (17, 24). However, the region-stratified sensitivity analyses provided different outcomes. The relationship between maternal education and a child death was statistically significant only in the two regions (Northern Midlands and Mountain areas and Central Highlands). However, the association was negative for women only in the North Central area and Central Coastal area. Though we tried adding the independent variables stepwise, starting with education in the Northern Midlands and Mountain areas dataset, the direction of the coefficient changed from positive to negative when we added the number of children (results not shown). This suggests that mothers with higher education tended to have a fewer children. That is, the number of children acted as a confounding factor, which accords with the results of a study by Adebowale et al. (22). We suggest that the reasons for the higher likelihood of child death among mothers with higher education in the Northern Midlands and Mountain areas should be explored in future studies.
Strengths and limitations
To our knowledge, this is the first study of its kind to investigate recent child mortality trends in Vietnam using the indirect method. Unlike previous studies, we controlled for the effect of the number of children. Yet, this study has also some limitations to consider.
Although there is evidence that occupation, religion, and living environment of mothers are risk factors for child deaths (25, 26), these variables were not available in our dataset. Additionally, experiencing child mortality is likely to be associated with community-level factors such as public sanitation facilities, birth delivery practices, and perceptions about traditional medicines (27). Additional analysis using multilevel techniques may provide further insights into child mortality in Vietnam. We also acknowledge that the survey may have underestimated child deaths because of the sensitivity of the topic for mothers. However, we are unable to assert whether and to what extent this may have occurred.
Conclusions
This study provides evidence and guidance for future policy to address childhood mortality in Vietnam. Interventions should focus on the most vulnerable groups such as the newly emerging urban poor and also ethnic minorities. These policies should not only involve socioeconomic improvements but should also include interventions for cultural and behavioural change. There is a need for further studies to investigate pathways underlying the associations between demographic and socioeconomic conditions and childhood mortality in Vietnam.
Acknowledgements
This paper was written as part of a collaborative project on health system strengthening in Vietnam, which is being implemented by the Hanoi School of Public Health, the Hanoi Medical University, Hanoi, Vietnam; the University of Medicine and Pharmacy of Ho Chi Minh City, Vietnam; and JW LEE Center for Global Medicine, Seoul National University College of Medicine, Seoul, Korea. We express our deep appreciation for Jennifer Stewart Williams from Umeå University for her great effort in supporting our writing process. We also thank Viet Nguyen from Harvard Medical School for editing the English content of this paper.
This paper is part of the Special Issue: Millennium Development Goals in Vietnam: the Progress and Social Determinants. More papers from this issue can be found at www.globalhealthaction.net
Footnotes
Authors' contributions
All listed authors have contributed significantly to the manuscript and approved the final version for publication. HYL and DVD analysed and interpreted data and drafted the manuscript. SC, TTHO, and TGK critically revised the manuscript.
Conflict of interest and funding
No conflict of interests was declared in this study.
References
- 1.Malqvist M, Nga NT, Eriksson L, Wallin L, Hoa DP, Persson LA. Ethnic inequity in neonatal survival: a case-referent study in northern Vietnam. Acta Paediatr. 2011;100:340–6. doi: 10.1111/j.1651-2227.2010.02065.x. [DOI] [PubMed] [Google Scholar]
- 2.General Statistics Office. 2009 census final results. Hanoi: GSO Vietnam; 2010. [Google Scholar]
- 3.Nga NT, Hoa DT, Malqvist M, Persson LA, Ewald U. Causes of neonatal death: results from NeoKIP community-based trial in Quang Ninh province, Vietnam. Acta Paediatr. 2012;101:368–73. doi: 10.1111/j.1651-2227.2011.02513.x. [DOI] [PubMed] [Google Scholar]
- 4.Pham TL, Kooreman P, Koning RH, Wiersma D. Gender patterns in Vietnam's child mortality. J Popul Econ. 2013;26:303–22. [Google Scholar]
- 5.Knowles JC, Bales S, Vu ML, Le QC, Tran TMO, Duong HL. Ha Long City, Vietnam: UNICEF Vietnam; 2009. Health equity in Viet Nam: a situational analysis focused on maternal and child mortality. Background paper prepared for UNICEF Consultancy on ‘Equity in Access to Quality Healthcare for Women and Children’. April 8–10. [Google Scholar]
- 6.Hoa DP, Nga NT, Malqvist M, Persson LA. Persistent neonatal mortality despite improved under-five survival: a retrospective cohort study in northern Vietnam. Acta Paediatr. 2008;97:166–70. doi: 10.1111/j.1651-2227.2007.00604.x. [DOI] [PubMed] [Google Scholar]
- 7.Swenson IE, Nguyen MT, Pham BS, Vu QN, Vu DM. Factors influencing infant mortality in Vietnam. J Biosoc Sci. 1993;25:285–302. [PubMed] [Google Scholar]
- 8.Brass W, Coale A. Methods of analysis and estimation. In: Brass W, Princeton University, Office of Population Research, editor. The demography of tropical Africa. Princeton, NJ: Princeton University Press; 1968. pp. 88–139. [Google Scholar]
- 9.Coale AJ, Trussell J. Annex I: estimating the time to which Brass estimates apply. Popul Bull UN. 1977;10:87–9. [PubMed] [Google Scholar]
- 10.Udjo EO. Levels and trends in infant and child mortality among some Kanuri of north-east Nigeria. J Trop Pediatr. 1987;33:43–7. doi: 10.1093/tropej/33.1.43. [DOI] [PubMed] [Google Scholar]
- 11.United Nations, Department of International Economic and Social Affairs. Step-by-step guide to the estimation of child mortality. New York: United Nations; 1990. [Google Scholar]
- 12.General Statistical Office. Population projection result for the whole country, geographic regions and 61 provinces/cities, Vietnam, 1999–2024. Hanoi: General Statistical Office; 2001. [Google Scholar]
- 13.General Statistical Office. Population projections for Vietnam, 2009–2049. Hanoi: General Statistical Office; 2011. [Google Scholar]
- 14.Hobcraft JN, McDonald JW, Rutstein SO. Demographic determinants of infant and early child mortality: a comparative analysis. Popul Stud. 1985;39:363–85. [Google Scholar]
- 15.Yassin KM. Indices and sociodemographic determinants of childhood mortality in rural Upper Egypt. Soc Sci Med. 2000;51:185–97. doi: 10.1016/s0277-9536(99)00459-1. [DOI] [PubMed] [Google Scholar]
- 16.Wheatley L. Factors affecting child mortaltiy [Honors Theses] University of Tennessee at Chattanooga, Chattanooga, TN; 2015. [Google Scholar]
- 17.Cleland JG, Van Ginneken JK. Maternal education and child survival in developing countries: the search for pathways of influence. Soc Sci Med. 1988;27:1357–68. doi: 10.1016/0277-9536(88)90201-8. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team. A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 19.Ingemarsson I. Gender aspects of preterm birth. BJOG. 2003;110(Suppl 20):34–8. doi: 10.1016/s1470-0328(03)00022-3. [DOI] [PubMed] [Google Scholar]
- 20.Vietnam Academy of Social Sciences. Poverty reduction in Vietnam: achievements and challenges. Hanoi: Thegioi Publisher; 2011. [Google Scholar]
- 21.World Bank. Country social analysis ethnicity and development in Vietnam: summary report. Washington, DC: World Bank; 2009. [Google Scholar]
- 22.Adebowale AS, Yusuf BO, Fagbamigbe AF. Survival probability and predictors for woman experience childhood death in Nigeria: ‘analysis of North-South differentials’. BMC Public Health. 2012;12:430. doi: 10.1186/1471-2458-12-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goland E, Hoa DT, Malqvist M. Inequity in maternal health care utilization in Vietnam. Int J Equity Health. 2012;11:24. doi: 10.1186/1475-9276-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bicego GT, Boerma JT. Maternal education and child survival: a comparative study of survey data from 17 countries. Soc Sci Med. 1993;36:1207–27. doi: 10.1016/0277-9536(93)90241-u. [DOI] [PubMed] [Google Scholar]
- 25.Kayode GA, Ansah E, Agyepong IA, Amoakoh-Coleman M, Grobbee DE, Klipstein-Grobusch K. Individual and community determinants of neonatal mortality in Ghana: a multilevel analysis. BMC Pregnancy Childbirth. 2014;14:165. doi: 10.1186/1471-2393-14-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adedini SA, Odimegwu C, Imasiku EN, Ononokpono DN, Ibisomi L. Regional variations in infant and child mortality in Nigeria: a multilevel analysis. J Biosoc Sci. 2015;47:165–87. doi: 10.1017/S0021932013000734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Boadi KO, Kuitunen M. J Health Popul Dev Countries. 2005. Childhood diarrheal morbidity in the Accra metropolitan area Ghana: socio-economic environmental and behavioral risk determinants. 1–13. [Google Scholar]