Abstract
Background
Despite significant achievements in health indicators during previous decades, Vietnam lags behind other developing countries in reducing common early childhood illnesses, such as diarrhea and respiratory infections. To date, there has been little research into factors that contribute to the prevalence and treatment of childhood morbidity in Vietnam.
Objective
This study examines the determinants of diarrhea and ‘illness with a cough’ and treatments for each of the conditions among young children in Vietnam, and describes trends over time.
Design
Data from the Vietnam Multiple Indicator Cluster Surveys in 2000, 2006, and 2011 were used. Multivariable logistic regressions were undertaken to investigate factors associated with these childhood illnesses and proper treatment patterns.
Results
Between 2000 and 2011, the prevalence of diarrhea among children under the age of five declined from 11 to 7%, while having illness with a cough increased to 40% in 2011 after falling from 69 to 28% between 2000 and 2006. During the same period, the prevalence of oral rehydration therapy (ORT) for treating diarrhea increased from 13 to 46%, whereas the rate of seeking formal treatment for illnesses with a cough fell from 24 to 7%. Multivariable models indicated that children who were older than 2 years (odds ration [OR]: 0.44, 95% confidence interval [CI]: 0.37–0.53, p<0.001), male (OR: 1.21, 95% CI: 0.64–2.37, p<0.05), living in rural areas (OR: 1.28, 95% CI: 1.00–1.64, p<0.05), or of Kinh ethnicity (OR: 0.70, 95% CI: 0.56–0.87, p<0.01) were more likely to suffer from diarrhea. Ethnic differences and higher household wealth were factors significantly associated with having illness with a cough. In particular, the effect of level of wealth on illness with a cough varied in each wave. Mothers with higher levels of education had higher odds of seeking ORT compared with mothers with the lowest level of education. Seeking formal treatment for children who have illness with a cough was associated with being in a household in the richest wealth quintile (OR: 0.56, 95% CI: 0.34–0.91, p<0.05).
Conclusions
This study demonstrates the importance of identifying different risk factors for these two illnesses and also factors associated with healthcare-seeking behaviors in order to reduce the burden of childhood morbidity in Vietnam. Policies aimed at tackling childhood morbidities should include comprehensive strategies that impact on socioeconomic and environmental factors.
Keywords: cough, diarrhea, MICS, oral hydration therapy, prevalence, under-five children, Vietnam
Introduction
Epidemiological evidence suggests that diarrhea and respiratory infections are main causes of morbidity and mortality in children under the age of five, accounting for more than two-fifths of all deaths worldwide (1). Diarrheal disease is the third leading cause of infant and child mortality in developing countries and represents 11% of all deaths in children under the age of five (2). One major reason for the poor outcomes of diarrhea episodes is the mismanagement of cases during acute situations. The use of rehydration therapy for watery diarrhea in children is directly related to survival (3). When a child is suffering from moderate dehydration, oral rehydration solution (ORS) may be enough while intravenous infusion of rehydration solution is needed in more severe cases (4).
Oral rehydration therapy (ORT) has significantly contributed to the reduction of childhood deaths from diarrhea (5) being operationally simple, effective, and inexpensive (6). However, despite its salient benefits, the use of ORT for diarrhea in developing countries has been neglected for various reasons. Many misconceive the seriousness of diarrhea in children and overlook the benefits of ORT treatment believing that every child normally experiences diarrhea and that they will recover without treatment (7). Some parents do not use ORT for reasons of affordability and accessibility (7). These barriers to the use of ORT impact differently on population subgroups making it difficult to correctly identify the most vulnerable.
Manna et al.'s study of the determinants of healthcare-seeking behavior for diarrheal illness among children under the age of five in India found that the formal education of primary caregivers was associated with care seeking outside the home (8). Another study by Ali et al. (9) observed that misperception of diarrhea in rural Bangladesh was the most common barrier to the use of ORT among severe cases and that difficulties in administering ORS were also common. In one of the few studies of ORT implementation in the Vietnamese context, Kaljee et al. investigated the preferences for healthcare providers regarding diarrhea treatment in Nha Trang. Using both qualitative and quantitative analysis, they showed that more than half of the respondents self-treated with medication purchased from a pharmacy or medications stored at home during the initial stages of diarrhea. Only less than a quarter utilized public healthcare providers during the initial stage of illness (10).
Childhood pneumonia is another major cause of childhood mortality. Each year, more than two million children die of acute respiratory infections, mostly pneumonia (11). Rapid recognition and treatment with effective medicine is critical because fatality when untreated is extremely high (12). In addition, the infection can be mistaken for malaria because the symptoms are similar (13). For these reasons, it is very important to obtain accurate diagnosis and deliver treatment quickly by an appropriate healthcare provider once the initial symptoms are apparent.
There are few studies on determinants of the prevalence or treatment of respiratory illnesses with cough symptoms in children. Hatt et al. explored the interaction between parental education and economic status on the prevalence of respiratory illness (14). They found that maternal education was more protective of the disease for children in wealthy families than for children in poor families, while father's education was also protective but operated independently of economic status. Basu et al. also emphasized the importance of maternal education. They showed that lack of maternal education is a significant correlate of cough episodes in children and that even primary education completion is protective of child health (15). However, to the best of our knowledge, apart from one qualitative study (10), little if any research has been published on healthcare-seeking behaviors for treating respiratory illnesses with cough symptoms in children in Vietnam.
Because of the seriousness of diarrhea and respiratory infections in children in developing countries such as Vietnam, research is needed to investigate the determinants of occurrence of those illnesses and also barriers to seeking treatment for these conditions. Given the major social and economic transitions that Vietnam has experienced in recent years, it is important to consider how patterns of illness and treatment are changing over time. This epidemiological study of children in Vietnam has two main objectives. The first is to identify the determinants of diarrhea and ‘illness with a cough’ and assess change in the determinants over time. The second objective is to identify factors that determine whether treatment is sought for these two conditions and assess change in these factors over time.
Methods
Data source
Data were derived from the three rounds of Multiple Indicator Cluster Survey (MICS) in Vietnam, performed in 2000 (wave 2), 2006 (wave 3), and 2011 (wave 4), respectively. The MICS was initially designed by UNICEF and then conducted by the General Statistics Office in collaboration with the Ministry of Health (MOH) and the Ministry of Labor, Invalids and Social Affairs (MOLISA). The surveys are intended to provide internationally comparable and statistically rigorous nationally representative data to fill gaps in evidence on issues related to the health status, development, and living standards of Vietnamese women and children.
The sample for MICS in Vietnam was based on probability, using the urban and rural areas within each of six regions as the main sampling strata. Sampling was undertaken in two stages. Within each stratum, a pre-determined number of enumeration areas were chosen using the probability proportional to the size. After household lists were updated within the selected enumeration areas, systematic samples of 20 household were drawn in each sample enumeration.
The MICS is a repeated cross-sectional survey, which targets different respondents each year. Three waves of data collection (2nd, 3rd, and 4th wave) in 2000, 2006, and 2011 are currently available. The MICS datasets and results have been published on the UNICEF website (mics.unicef.org). There are three separate datasets in each wave, which are for households, women aged 15–29 years, and children under the age of five. Data used in this analysis were drawn from the dataset for children. More detailed information on MICS can be found elsewhere (16–18).
Dependent variables
There are four binary dependent variables, two measuring recent illnesses and two measuring treatment for those who reported the illnesses. The illness variables are diarrhea and illness with a cough. They were derived from answers to questions about whether a child aged 5 years or less had experienced either diarrhea or an illness with a cough during the 2 weeks prior to the interview. Response options were yes versus no.
The treatment measures refer to ORT for recent diarrhea and formal treatment for recent illness with a cough. The ORT variable was derived from answers to a question, which asked mothers about treatment given to children during a recent episode of diarrhea. This question had five possible responses, which were used to derive a binary variable: fluid from ORS packet or pre-packaged ORS fluid versus other kinds of water. The binary treatment variable for recent illness with a cough was derived from responses to a question, which asked about the treatment mothers sought. This variable was coded: seeking formal healthcare such as public or private hospital, health center, or doctor versus seeking relative/friend, shop, traditional healer, or none.
Independent variables
Demographic and socioeconomic factors available in the MICS dataset, which were known, from previous studies, to have association with the dependent variables, were chosen as the independent variables. Child's age, in years, was transformed into a binary variable using the mean age of the study population as the cutoff point. Breastfeeding was dichotomized as yes (ever breastfed) versus no (never breastfed). The mother's education variable comprised five categories: ‘less than primary’, for respondents who had never been to school or did not finish grade 5; ‘lower secondary’, for respondents who attained their highest level of education between grades 6 and 9; ‘upper secondary’, for respondents who attained their highest level of education between grades 10 and 12; and ‘tertiary’, for respondents who finished professional school, college, or university and above.
Ethnicity was classified into two groups: Kinh, which is the ethnic majority in Vietnam, accounting for about 86% of the population, and non-Kinh (18). A household wealth index was used as a proxy variable for economic status. This was constructed based on the information on household's ownership of consumer goods and amenities related to dwelling characteristics, water, and sanitation. Household wealth scores were derived by principal component analysis, and the scores were divided into quintiles from the poorest to the wealthiest. A time variable (wave) was included as a proxy for survey year.
Statistical analysis
Descriptive statistics were conducted to describe patterns of illness and treatment by the independent variables in each separate survey wave (2000, 2006, and 2011). Using a combined dataset covering all three survey waves, separate sets of multivariable logistic regressions were performed for each of the four dependent variables. Odds ratios (OR) and 95% confidence intervals (CIs) are reported. Initially, four separate models with only main effects were examined. Additional analyses were performed including interaction terms (time multiplied by each predictor variable) to assess change in associations between independent and dependent variables across the survey waves. Each interaction term was tested separately, and only those that were significant at p≤0.05 were included in the final model. All analyses were performed using STATA 12.0 software.
Ethical consideration
This study is based on secondary data from the MICS with all identifying information that has been removed. The survey obtained informed consent from the mothers before conducting survey questionnaires. All information in the original dataset was collected confidentially (16–18).
Results
Derivation of study sample
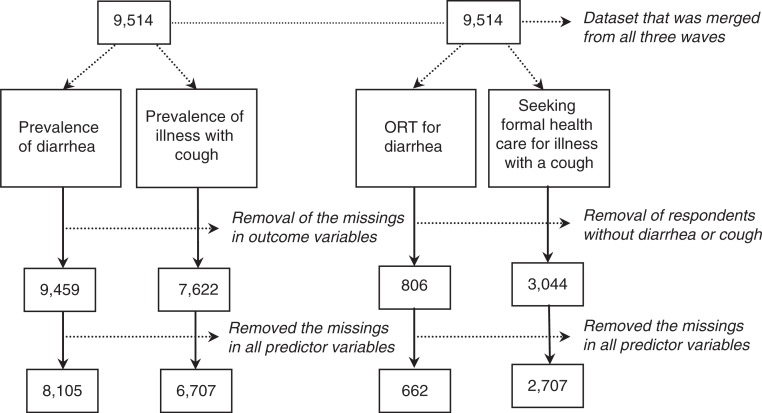
Figure 1 shows the derivation of the four study samples used in the regressions. The initial study population (N=9,514) was combined from three waves of MICS including complete data on the relevant dependent and independent variables.
Fig. 1.
Derivation of study samples for logistic regression analysis using combined MICS data, 2000, 2006, and 2011.
Patterns of illness, treatment by survey years
Tables 1 and 2 show the prevalence of four dependent variables by demographic and socioeconomic characteristics. Diarrhea was much less common than illness with a cough (11% vs. 69% in 2000, 8% vs. 28% in 2006, and 7% vs. 40% in 2011). Prevalence of diarrhea decreased continuously from 11% in 2000 to 7% in 2011, whereas the prevalence of an illness with a cough rebounded to 40% in 2011 after declining from 69% in 2000 to 28% in 2006. There was a consistent pattern in the prevalence of diarrhea across the three waves. For example, children who were older, were male, had ever been breastfed, had mothers with higher levels of education lived in urban areas, or were of Kinh ethnicity had lower prevalence of diarrhea than their counterparts in all 3 years (2000, 2006, and 2011). However, illness with a cough was less consistent across the survey waves (Table 1).
Table 1.
Distribution of diarrhea and illness with cough in children under-five in Vietnam by demographic and socioeconomic characteristics, 2000, 2006, and 2011
| Diarrhea | Illness with cough | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | ||||||||
|
|
|
|
|
|
|
||||||||
| Variables | Category | N | % | N | % | N | % | N | % | N | % | N | % |
| Average | 2,471 | 11 | 2,251 | 8 | 3,383 | 7 | 1,072 | 69 | 2,251 | 28 | 3,384 | 40 | |
| Child's age | <2 years | 1,371 | 13 | 1,325 | 10 | 2,058 | 9 | 627 | 70 | 1,325 | 29 | 2,059 | 39 |
| ≥2 years | 1,100 | 7 | 926 | 5 | 1,325 | 4 | 445 | 68 | 926 | 26 | 1,325 | 40 | |
| Child's gender | Female | 1,209 | 9 | 1,105 | 7 | 1,652 | 7 | 531 | 71 | 1,105 | 27 | 1,653 | 38 |
| Male | 1,262 | 12 | 1,146 | 9 | 1,731 | 7 | 541 | 67 | 1,146 | 28 | 1,731 | 41 | |
| Breastfeeding | No | 46 | 9 | 38 | 3 | 76 | 7 | 22 | 68 | 38 | 24 | 76 | 45 |
| Yes | 2,425 | 11 | 2,213 | 8 | 3,307 | 7 | 1,050 | 69 | 2,213 | 28 | 3,308 | 39 | |
| Mother's education | <Primary | 818 | 13 | 380 | 9 | 670 | 8 | 365 | 70 | 380 | 22 | 671 | 42 |
| Lower secondary | 1,239 | 11 | 347 | 11 | 1,379 | 7 | 556 | 70 | 347 | 26 | 1,379 | 40 | |
| Upper secondary | 351 | 7 | 847 | 8 | 660 | 7 | 125 | 64 | 847 | 31 | 660 | 37 | |
| Tertiary | 63 | 3 | 677 | 6 | 674 | 6 | 26 | 62 | 677 | 28 | 674 | 38 | |
| Area | Urban | 495 | 7 | 332 | 4 | 1,373 | 6 | 199 | 62 | 332 | 27 | 1,373 | 39 |
| Rural | 1,976 | 11 | 1,919 | 9 | 2,010 | 8 | 873 | 70 | 1,919 | 28 | 2,011 | 40 | |
| Ethnicity | Non-Kinh | 400 | 14 | 746 | 12 | 481 | 11 | 154 | 65 | 746 | 24 | 481 | 39 |
| Kinh | 2,071 | 10 | 1,505 | 6 | 2,902 | 6 | 918 | 70 | 1,505 | 30 | 2,903 | 40 | |
| Wealth quintiles | Poorest | 642 | 14 | 757 | 10 | 667 | 9 | 300 | 67 | 757 | 23 | 667 | 44 |
| Second | 606 | 13 | 468 | 5 | 571 | 7 | 278 | 73 | 468 | 32 | 572 | 42 | |
| Middle | 444 | 7 | 431 | 7 | 639 | 7 | 208 | 67 | 431 | 29 | 639 | 38 | |
| Fourth | 407 | 9 | 365 | 9 | 733 | 6 | 150 | 70 | 365 | 33 | 733 | 39 | |
| Richest | 372 | 12 | 230 | 3 | 773 | 6 | 136 | 65 | 230 | 23 | 773 | 35 | |
Table 2.
Distribution of ORT and formal treatment for cough in children under-five in Vietnam by demographic and socioeconomic characteristics, 2000, 2006, and 2011
| ORT | Formal treatment for illness with cough | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| 2001 | 2006 | 2011 | 2001 | 2006 | 2011 | ||||||||
|
|
|
|
|
|
|
||||||||
| Variables | Category | N | % | N | % | N | % | N | % | N | % | N | % |
| Average | 263 | 13 | 174 | 22 | 225 | 46 | 742 | 24 | 625 | 24 | 1,340 | 7 | |
| Child's age | <2 years | 185 | 15 | 131 | 24 | 179 | 46 | 438 | 24 | 383 | 25 | 804 | 7 |
| ≥2 years | 78 | 9 | 43 | 16 | 46 | 46 | 304 | 24 | 242 | 21 | 536 | 7 | |
| Child's gender | Female | 110 | 12 | 78 | 18 | 108 | 38 | 366 | 24 | 300 | 21 | 633 | 6 |
| Male | 153 | 14 | 96 | 26 | 117 | 53 | 376 | 24 | 325 | 26 | 707 | 8 | |
| Mother's education | <Primary | 104 | 9 | 33 | 6 | 51 | 25 | 254 | 23 | 82 | 27 | 285 | 7 |
| Lower secondary | 133 | 17 | 37 | 27 | 94 | 51 | 389 | 26 | 91 | 23 | 555 | 8 | |
| Upper secondary | 23 | 13 | 65 | 25 | 42 | 52 | 80 | 19 | 263 | 19 | 244 | 6 | |
| Tertiary | 3 | 0 | 39 | 28 | 38 | 53 | 19 | 16 | 189 | 29 | 256 | 6 | |
| Area | Urban | 37 | 19 | 13 | 31 | 74 | 47 | 124 | 19 | 89 | 17 | 539 | 5 |
| Rural | 226 | 12 | 161 | 22 | 151 | 45 | 618 | 25 | 536 | 25 | 801 | 8 | |
| Ethnicity | Non-Kinh | 56 | 14 | 84 | 15 | 51 | 43 | 102 | 25 | 179 | 27 | 188 | 5 |
| Kinh | 207 | 13 | 90 | 29 | 174 | 47 | 640 | 24 | 446 | 22 | 1,152 | 7 | |
| Wealth quintiles | Poorest | 93 | 9 | 76 | 18 | 56 | 32 | 204 | 29 | 175 | 26 | 294 | 8 |
| Second | 63 | 11 | 35 | 20 | 41 | 41 | 204 | 24 | 149 | 23 | 243 | 7 | |
| Middle | 45 | 20 | 29 | 28 | 42 | 60 | 140 | 21 | 125 | 29 | 246 | 7 | |
| Fourth | 36 | 17 | 26 | 27 | 44 | 52 | 105 | 22 | 122 | 20 | 283 | 9 | |
| Richest | 26 | 15 | 8 | 38 | 42 | 48 | 89 | 19 | 54 | 13 | 274 | 4 | |
The prevalence of ORT for diarrhea increased from 13% in 2000 to 22% in 2006, and 46% in 2011, while the proportion seeking formal treatment for illness with a cough decreased during the same period. In particular, there was a clear decline between 2006 and 2011. Prevalence patterns for both ORT utilization and formal treatment for illness with a cough varied across the three time points (Table 2).
Factors associated with illness and treatment
Table 3 shows the results of the multivariable logistic regressions for each of the four dependent variables conducted on the dataset comprising multiple waves of the MICS (2000, 2006, and 2011). The odds of diarrhea and illness with a cough were lower in waves 3 and 4 compared to wave 2, holding all other variables constant. Children aged two or above (OR=0.44, CI =0.37–0.53) and of Kinh ethnicity (OR=0.70, CI=0.56–0.87) demonstrated lower odds of suffering from diarrhea compared with their counterparts. Male children and those living in rural areas had significantly higher odds of having recent diarrhea, compared to children who were female and living in urban areas.
Table 3.
Multivariable regression results for the determinants of illnesses and proper treatments in children under-five in Vietnam, 2000, 2006, and 2011
| Diarrhea | Illness with cough | ORT | Seeking formal healthcare for illness with cough | ||
|---|---|---|---|---|---|
| Variables | Categories | OR(CI) | OR(CI) | OR(CI) | OR(CI) |
| Wave† | Wave 2 | Ref. | Ref. | Ref. | Ref. |
| Wave 3 | **0.70 (0.55–0.88) | ***0.21 (0.17–0.26) | 1.78 (0.97–3.26) | 0.98 (0.72–1.34) | |
| Wave 4 | ***0.67 (0.55–0.81) | ***0.43 (0.33–0.57) | ***5.26 (3.25–8.52) | ***0.26 (0.19–0.34) | |
| Child's age | <2 years | Ref. | Ref. | Ref. | Ref. |
| ≥2 years | ***0.44 (0.37–0.53) | 0.97 (0.87–1.08) | 0.84 (0.52–1.35) | 0.95 (0.76–1.18) | |
| Child's gender | Female | Ref. | Ref. | Ref. | |
| Male | *1.21 (0.64–2.37) | 1.05 (0.95–1.16) | *1.61 (1.09–2.38) | 1.12 (0.90–1.39) | |
| Mother's education | <Primary | Ref. | Ref. | Ref. | Ref. |
| Lower secondary | 1.02 (0.83–1.26) | 0.99 (0.86–1.15) | ***2.71 (1.56–4.71) | 1.17 (0.88–1.55) | |
| Upper secondary | 0.90 (0.69–1.17) | 1.02 (0.86–1.21) | *2.26 (1.17–4.39) | 0.85 (0.58–1.23) | |
| Tertiary | 0.77 (0.56–1.06) | 1.02 (0.85–1.24) | *2.32 (1.09–4.96) | 1.33 (0.89–1.90) | |
| Area | Urban | Ref. | Ref. | Ref. | Ref. |
| Rural | *1.28 (1.00–1.64) | 0.97 (0.85–1.12) | 0.87 (0.50–1.51) | 1.32 (0.95–1.83) | |
| Ethnicity | Non-Kinh | Ref. | Ref. | Ref. | Ref. |
| Kinh | **0.70 (0.56–0.87) | **1.29 (1.10–1.51) | 0.71 (0.42–1.20) | 1.07 (0.78–1.46) | |
| Wealth quintiles | Poorest | Ref. | Ref. | Ref. | Ref. |
| Second | 0.87 (0.69–1.11) | *1.91 (1.17–3.11) | 1.29 (0.72–2.32) | 0.81 (0.60–1.11) | |
| Middle | 0.85 (0.65–1.11) | 1.42 (0.85–2.37) | *2.24 (1.22–4.12) | 0.87 (0.62–1.23) | |
| Fourth | 0.85 (0.64–1.13) | *1.97 (1.12–3.45) | 1.88 (0.97–3.63) | 0.83 (0.58–1.20) | |
| Richest | 0.80 (0.56–1.14) | 1.11 (0.62–2.00) | 1.45 (0.63–3.34) | *0.56 (0.34–0.91) | |
| Breastfeeding | No | Ref. | Ref. | ||
| Yes | 1.23 (1.03–1.42) | 0.90 (0.63–1.29) | |||
| Wave×wealth index | Wave×second | *0.78 (0.64–0.96) | |||
| Wave×middle | *0.81 (0.66–1.00) | ||||
| Wave×fourth | *0.73 (0.58–0.91) | ||||
| Wave×richest | 0.82 (0.66–1.03) |
Wave 2, year 2000; wave 3, year 2006; wave 4, year 2011
p<0.05
p<0.01
p<0.001.
However, Kinh children had higher odds of experiencing illness with a cough than non-Kinh children (OR =1.29, CI=1.10–1.51). There was negative interaction between wealth and survey year (wave), suggesting that the impact of wealth status on illness with a cough decreased in each subsequent wave.
Mothers’ education level was significantly associated with seeking ORT. Children whose mothers attained lower secondary education and above had more than double the odds of receiving ORT during an episode of diarrhea, compared with children with mothers who attained primary or lower education. Children who were male (OR=1.61, CI=1.09–2.38) or who were from households in the middle wealth quintile (OR=2.24, CI=1.22–4.12) were more likely to receive ORT than children who were female or from households in the poorest wealth quintile. There were no significant interactions between any of the independent variables and survey year (wave) suggesting that the effects were similar in each wave. Seeking treatment through formal healthcare services was significantly associated only with household wealth. The odds ratio for the wealthiest compared with the poorest quintile was 0.56 (CI: 0.34–0.91).
Discussion
This study on the determinants of diarrhea and illness with a cough and their respective treatments among young children in recent years in Vietnam has a few key findings.
First, we found an undesirable trend in seeking formal healthcare services for treating illness with a cough. Not only was the use of formal healthcare for illness with a cough low, but this decreased over time. Children's cough symptoms can be easily overlooked unless production of thick sputum or persistent over a long time (20, 21). Such misconceptions can put children at risk because mothers often think that formal treatment is not necessary. Nevertheless, if there are reliable, available, and affordable primary healthcare facilities, mothers may seek treatment. Yet, many Vietnamese increasingly mistrust public primary healthcare facilities mainly because the quality of public services in the community has fallen since the legalization of private medical practice in 1989. On the other hand, private healthcare is expensive. This may explain Vietnamese mothers’ reluctance to seek healthcare for illnesses that they do not perceive as being serious (21).
A second finding is that being of Kinh ethnicity was negatively associated with having recent diarrhea, but positively associated with illnesses with a cough. This may be explained by environmental factors. The occurrence of diarrhea is heavily dependent on hygiene and environmental factors such as unsafe water, polluted soil, and bad hygiene (22). Ethnic minorities in Vietnam, which account for only about 15% of the population, mainly reside in remote and mountainous areas where hygiene-related infrastructure and environmental conditions are often poor (23). Although environmental factors were already included in part through the wealth index, which measured household amenities related to sanitation, unclean environments outside the household can also promote infection which leads to diarrhea in children. The positive association between Kinh ethnicity and illness with a cough may be explained by the fact that people of Kinh ethnicity are more likely to live in more developed urban areas in which there is exposure to air pollution, which can lead to respiratory problems in children (24).
Household wealth effects over time are also noteworthy. Specifically, the protective effect of wealth for illness with a cough was higher in successive waves, consistent with previous studies that have demonstrated a negative relationship between poverty and respiratory diseases. Crowded living environments, non-immunization, and ignorance of preventive measures, all of which are common among poorer people, may have also been influential (25). As the gap between the rich and the poor widened in Vietnam during the study period, higher economic status may have been protective for illness with cough.
Another finding is that mothers’ education levels were significantly associated with seeking ORT, but not with seeking formal treatment for an illness with a cough. A plausible reason for this can be found in research conducted by Ali et al. in Bangladesh, who claimed that a main reason for not using ORT was because of the misconception that ORT can stop the diarrhea (9). The mothers with incorrect information about the benefits of ORT were half as likely to use ORT compared with mothers who understood correctly that ORG is not a cure for diarrhea but helps replace lost salt and water. On the other hand, one of the reasons why mothers do not seek formal healthcare services for illness with a cough is because of distrust of public services and non-affordability of private services.
An unexpected result was the significant negative association between household wealth and seeking formal healthcare for illness with a cough. Children from households in the richest wealth quintile were less likely to seek formal healthcare for illness with cough, compared to children in the poorest quintile, but they were more likely to use ORT for diarrhea. There are some studies that support a negative association between wealth and formal healthcare-seeking for illness with cough. For example, Taffa and Chepngeno (21) revealed that household income was significantly associated with healthcare-seeking behaviors only up to a certain threshold. For those children above the threshold, other factors, such as proper understanding of the disease, were important determinants. There are some possible underlying mechanisms that may be operating here. Those who are richer are more likely to be more highly educated (26–28). In Vietnam, many people choose self-treatment during the initial stage unless the symptoms were perceived as being too severe (10). For example, 40–60% of individuals initially depend on self-treatment using western or traditional medicines, and about 27.3% stock various medicines, including antibiotics, for self-medication (29). Wealthier mothers who are better educated may try to control cough symptoms by using high-quality self-medication at home. It is also possible that cough symptoms in children from wealthier households may be less serious during early stages of the disease process because of good nutritional environments. On the other hand, commercial ORS can be up to seven times more costly than homemade ORS (30). Given that children may have diarrhea for as many as 60 days a year, and diarrhea tends to spread easily among siblings in the same family, commercial ORS can be very costly for poorer families. This is therefore one reason why we might expect that children from rich households would be more likely to be treated with ORT.
Although this is the first study of its kind, there are some limitations. First, as mentioned before, ORT is effective only on watery diarrhea because it does not stop diarrhea. ORT prevents dehydration during a diarrhea episode. Therefore, we suggest that future questionnaires should include questions about the type or duration of diarrhea to more accurately measure proper treatment. Second, childhood diarrhea and illness with a cough are likely to be associated with community-level factors such as accessibility to clean water or air, sanitation facilities, and hygiene practices (31). Future research exploring the effects of contextual factors using multi-level modeling could help to further explain the associations described here. Finally, there are possibly many other determinants that are not available in this dataset.
Conclusions
The findings of this study indicate the importance of raising awareness of childhood illnesses, such as diarrhea and illness with a cough, in Vietnam, and developing interventions that target at-risk groups, such as those who are from ethnic minorities, who have less wealth, and whose mothers have limited schooling. However, it is important that campaigns convey accurate messages and do not mislead. For example, aggressive marketing campaigns on ORT can wrongly convince people that ORT is effective on all kinds or diarrhea, and they promote unnecessary use of expensive commercial treatments. Qualitative research may also help to improve understanding of these and other issues. Future policies aimed at tackling childhood morbidity should include comprehensive strategies that impact on socioeconomic and environmental factors.
Authors' contributions
All listed authors have contributed significantly to the manuscript and approved the final version for publication. HYL designed the concept, analyzed and interpreted data, and drafted the manuscript. NVH drafted the manuscript, gave critical comments, and edited the manuscript. SGC gave critical comments, revised the manuscript, and completed editing.
Conflict of interest and funding
The authors declare there are no conflicts of interest.
Acknowledgement
This paper was written as part of a collaborative project on health system strengthening in Vietnam, which is being implemented by the Hanoi School of Public Health, the Hanoi Medical University, Hanoi, Vietnam; the University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam; and JW LEE Center for Global Medicine, Seoul National University College of Medicine, Seoul, Korea. We express our deep appreciation for Jennifer Stewart Williams from Umeå University for her great effort in supporting our writing process. We also thank Viet Nguyen from Harvard Medical School for editing the English content of this paper.
This paper is part of the Special Issue: Millennium Development Goals in Vietnam: the Progress and Social Determinants. More papers from this issue can be found at www.globalhealthaction.net
References
- 1.Bryce J, Boschi-Pinto C, Shibuya K, Black RE, the WHO Child Health Epidemiology Reference Group WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.Vaahtera M, Kulmala T, Maleta K, Cullinan T, Salin ML, Ashorn P. Epidemiology and predictors of infant morbidity in rural Malawi. Paediatr Perinat Epidemiol. 2000;14:363–71. doi: 10.1046/j.1365-3016.2000.00308.x. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Diarrhoeal disease. 2009. Fact sheet. WHO. (Available at: http://www.who.int/mediacentre/factsheets/fs330/en/)
- 5.Ahmed FU, Ekhlasur Rahman M, Dewan S. Outcome of children rehydrated in a hospital ORT corner in Bangladesh: a follow-up study. J Diarrhoeal Dis Res. 1999;17:17–21. [PubMed] [Google Scholar]
- 6.Patwari A. Cost effective strategy for promotion of appropriate case management of diarrheal diseases – establishment of DTUs. Indian J Pediatr. 1991;58:783–7. doi: 10.1007/BF02825435. [DOI] [PubMed] [Google Scholar]
- 7.Charyeva Z, Cannon M, Oguntunde O, Garba AM, Sambisa W, Bassi AP, et al. Reducing the burden of diarrhea among children under five years old: lessons learned from oral rehydration therapy corner program implementation in Northern Nigeria. J Health Popul Nutr. 2015;34:4. doi: 10.1186/s41043-015-0005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manna B, Nasrin D, Kanungo S, Roy S, Ramamurthy T, Kotloff KL, et al. Determinants of health care seeking for diarrheal illness in young children in urban slums of Kolkata, India. Am J Trop Med Hyg. 2013;89(1 Suppl):56–61. doi: 10.4269/ajtmh.12-0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali M, Atkinson D, Underwood P. Determinants of use rate of oral rehydration therapy for management of childhood diarrhoea in rural Bangladesh. J Health Popul Nutr. 2000;18:103–8. [PubMed] [Google Scholar]
- 10.Kaljee LM, Thiem VD, von Seidlein L, Genberg BL, Canh DG, Tho le H, et al. Healthcare use for diarrhoea and dysentery in actual and hypothetical cases, Nha Trang, Viet Nam. J Health Popul Nutr. 2004;22:139–49. [PubMed] [Google Scholar]
- 11.Mulholland K. Magnitude of the problem of childhood pneumonia. Lancet. 1999;354:590–2. doi: 10.1016/S0140-6736(98)10238-6. [DOI] [PubMed] [Google Scholar]
- 12.Reyes H, Perez-Cuevas R, Salmeron J, Tome P, Guiscafre H, Gutierrez G. Infant mortality due to acute respiratory infections: the influence of primary care processes. Health Policy Plan. 1997;12:214–23. doi: 10.1093/heapol/12.3.214. [DOI] [PubMed] [Google Scholar]
- 13.Kallander K, Nsungwa-Sabiiti J, Balyeku A, Pariyo G, Tomson G, Peterson S. Home and community management of acute respiratory infections in children in eight Ugandan districts. Ann Trop Paediatr. 2005;25:283–91. doi: 10.1179/146532805X72430. [DOI] [PubMed] [Google Scholar]
- 14.Hatt LE, Waters HR. Determinants of child morbidity in Latin America: a pooled analysis of interactions between parental education and economic status. Soc Sci Med. 2006;62:375–86. doi: 10.1016/j.socscimed.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Basu AM, Stephenson R. Low levels of maternal education and the proximate determinants of childhood mortality: a little learning is not a dangerous thing. Soc Sci Med. 2005;60:2011–23. doi: 10.1016/j.socscimed.2004.08.057. [DOI] [PubMed] [Google Scholar]
- 16.General Statistics Office (GSO) Final Report. Hanoi, Vietnam: GSO; 2000. Viet Nam multiple indicator cluster survey 2000. [Google Scholar]
- 17.General Statistics Office (GSO) Final Report. Hanoi, Vietnam: GSO; 2006. Viet Nam multiple indicator cluster survey 2006. [Google Scholar]
- 18.General Statistics Office (GSO) Final Report. Hanoi, Vietnam: GSO; 2011. Viet Nam multiple indicator cluster survey 2011. [Google Scholar]
- 19.General Statistical Office. , Vietnam: Statistical Publishing House; 2009. The 2009 Vietnam population and housing census: completed results. [Google Scholar]
- 20.Webair HH, Ghouth ASB. ‘This diarrhoea is not a disease …’ local illness concepts and their effects on mothers health seeking behaviour: a qualitative study, Shuhair, Yemen. BMC Public Health. 2014;14:581. doi: 10.1186/1471-2458-14-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health. 2005;10:240–5. doi: 10.1111/j.1365-3156.2004.01381.x. [DOI] [PubMed] [Google Scholar]
- 22.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis. 2005;5:42–52. doi: 10.1016/S1473-3099(04)01253-8. [DOI] [PubMed] [Google Scholar]
- 23.Baulch B, Haughton D, Haughton J, Chuyen TTK. 2002. Ethnic minority development in Vietnam: a socioeconomic perspective. World Bank Policy Research Working Paper (2836) [Google Scholar]
- 24.Lin CA, Martins MA, Farhat SC, Pope CA, 3rd, Conceicao GM, Anastácio VM. et al. Air pollution and respiratory illness of children in Sao Paulo, Brazil. Paediatr Perinat Epidemiol. 1999;13:475–88. doi: 10.1046/j.1365-3016.1999.00210.x. [DOI] [PubMed] [Google Scholar]
- 25.Tupasi TE, Velmonte MA, Sanvictores MEG, Abraham L, De Leon LE, Tan SA, et al. Determinants of morbidity and mortality due to acute respiratory infections: implications for intervention. J Infect Dis. 1988;157:615–23. doi: 10.1093/infdis/157.4.615. [DOI] [PubMed] [Google Scholar]
- 26.Chatman S. Berkeley, CA: Center for Studies in Higher Education, University of California at Berkeley; 2011. Wealth, cost, and the undergraduate student experience at large public research universities. [Google Scholar]
- 27.Hemelt SW, Dave EM. The impact of tuition increases on enrollment at public colleges and universities. Educ Eval Policy Anal. 2011;33:435–57. [Google Scholar]
- 28.United States Government Accountability Office. Washington, DC: USGAO; 2014. Higher education: state funding trends and policies on affordability. [Google Scholar]
- 29.Okumura J, Wakai S, Umenai T. Drug utilisation and self- medication in rural communities in Vietnam. Soc Sci Med. 2002;54:1875–86. doi: 10.1016/s0277-9536(01)00155-1. [DOI] [PubMed] [Google Scholar]
- 30.Islam MR, Greenough WB, III, Rahaman MM, Choudhury AA, Sack DA. Labon-gur (common salt and brown sugar) oral rehydration solution in the treatment of diarrhoea in adults. J Trop Med Hyg. 1980;83:41–5. [PubMed] [Google Scholar]
- 31.Boadi KO, Kuitunen M. Childhood diarrheal morbidity in the Accra metropolitan area Ghana: socio-economic environmental and behavioral risk determinants. J Health Popul Developing Countries. 2005;7:1–13. [Google Scholar]