Abstract
Background:
Diabetes is the fifth leading cause of death in the world. Hence, we investigated the factors affecting disease control among diabetic patients referred to Imam Reza Hospital (central hospital in the Northwest of Iran).
Materials and Methods:
One hundred and eight diabetic patients were evaluated. Patient's main medications including insulin, metformin, glibenclamide, and glytazon were registered and the levels of fasting blood sugar (FBS), glucose 2 h postprandial (pp), and hemoglobin A1c (HbA1c) were measured. All risk factors were evaluated by using a questionnaire completed by the patients.
Results:
The average of HbA1c, FBS, and glucose 2 h pp was 7.33%, 159 mg/dl, and 233.03 mg/dl, respectively. In patients whose disease was controlled, the family history of the disease, the type of medication, and the visits to family physician had a significant association with disease control. The average mean of HbA1c among patients with controlled and uncontrolled disease was 5.93% and 8.63 % respectively.
Conclusion:
Less stress, education, and weekly exercise had an essential role in controlling the disease in diabetic patients from the Northwest of Iran and noncompliance with the prescribed diet by the physician and lack of timely medicine intake were the main reasons for uncontrolled disease.
Keywords: Control, diabetes, effective factors, hemoglobin A1c, treatment
INTRODUCTION
Diabetes is the fifth leading cause of death globally and causes 6.8% of death in all age categories.[1] The spread of diabetes has an increasing trend due to aging, changes in life style, diet, and lack of exercises. It is anticipated that the number of diabetic patients will increase to 300 million patients by the year 2025.[2] This disease is the reason for lower limb amputation, and incidence of blindness or loss of vision.[3,4] According to World Health Organization reports, just 37% of diabetic patients have controlled disease.[5] One of the main factors in diabetes is the geographical factor and according to the last claim by world diabetes federation half of the population in Persian Gulf countries are disposed to diabetes.[6] Several other factors which can affect the spread of this disease are genetic elements, behavioral, weather, and environmental factors.[7] People with high risk of developing disease are described as over 30 years old, hereditary, obesity, body mass index (BMI) ≥25 kg/m2, lack of physical activity, giving birth to a child weighing more than 4 kg, high blood pressure ≥140/90 mmHg, high density lipoprotein <35 mg/dL, and triglycerides >250 mg/dL.[8] Diet and drug regimen is the most important factors for controlling the disease and <50% of patients in developing countries are receiving enough drugs.[9] The main goal in the treatment strategies is controlling blood glucose, which will improve life quality of the patients.[10] Several studies have established the relationship between hemoglobin A1c (HbA1c) level and life quality of patients and every 1% reduction will improve 5% of life quality of the patients.[11] In this study, we aim to investigate the role of different factors on control of diabetes in diabetic patients in the Northwest of Iran.
MATERIALS AND METHODS
Sampling
One hundred and eight diabetic patients who were referred to central diabetes center in Imam Reza Hospital (Tabriz, East Azarbaijan province, Iran) were selected voluntarily. All patients participated voluntarily in the study and confirmed their participation by written consent. Inclusion criteria were patients with approved diabetes who were referred to Imam Reza Hospital, and all of these patients were included in the study. This study was confirmed by the ethical committee of Tabriz University of Medical Sciences.
Tools
The study was done during the period of 8 months, and a questionnaire was utilized to collect data such as height, weight, age, diet and life style, and patients’ BMI was calculated. The questionnaire was developed after interviewing with experts and validated by Cronbach's alpha in SPSS version 21 (IBM SPSS Statistics, New York, USA). The level of HbA1c, fasting blood sugar (FBS) and glucose 2 h postprandial were measured by a BS-800 machine (Mindray, Shenzhen, China) and kit components were from Pishtaz Teb (Pishtaz Teb, Tehran, Iran) and glucose and FBS kits were obtained from Pars Iran Azmoon (Pars Iran Azmoon, Tehran, Iran). HbA1c values below 6.7% were considered controlled diabetes and those above this level were considered uncontrolled diabetes (as provided by the manufacturer). Patients’ drugs included insulin, metformin HCl, glibenclamide, and glitazone. Overall effects of treatment were concluded from the outcome of each controlled factor.
Statistical analysis
SPSS version 21 was used for statistical analysis. Cronbach's alpha was applied for the validation of Questionnaire. A P-value below 0.05 was considered statistically significant.
RESULTS
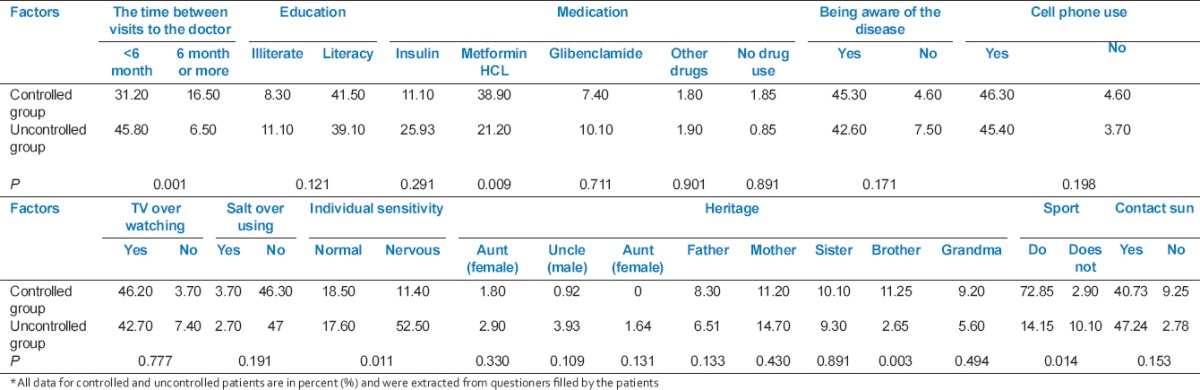
From the investigated population, 46 (42.5%) were men and 62 (57.5%) were women. Overall 52 (48.15%) patients had controlled disease of which 22 (20%) were men and 30 (28%) were women and 56 (51.85%) patients had uncontrolled disease of which 24 (22.23%) were men and 32 (29.77%) were women. The age of patients ranged from 15 to 80 (average: 55.8 years) and had diabetes for more than a year. The mean duration of diabetes was 12.7 years. All laboratory analyses for controlled and uncontrolled patients are presented in Table 1. Cronbach's alpha reliability index was 82%. The time between visits to the doctor, medication, hereditary (brother), and sport had a significant relationship with the controlled group [Table 2]. At the time of visiting the doctor, patients who were examined by the doctor every 6 months or more had a significant difference in control of disease, but patients who were examined in <6 months had no significant difference. About 30% of insulin users had controlled disease, but 65% of the patients who consumed metformin had controlled disease. 65.5% of the patients who had average of 2 h exercise during the week had controlled disease. By hereditary, 67% of patients with the history of diabetes in one of their siblings had controlled disease. All other factors had no difference between the controlled and uncontrolled groups [Table 2]. Moreover, the sleep duration of the patients was between 3 h and 10 h and just 4 patients had sleep disorder.
Table 1.
Laboratory indexes of controlled and uncontrolled groups with their ranges
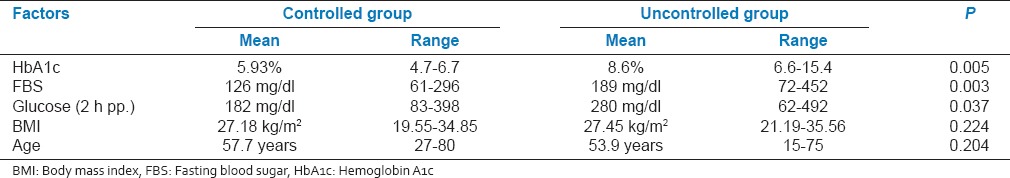
Table 2.
Evaluated factors in diabetic controlled and uncontrolled groups
DISCUSSION
The main index in controlling diabetes is the measurement of glycosylated hemoglobin and in this study, we observed 27 mg/dl increase in FBS for every 1% change in the HbA1c. It has been demonstrated that there is a relationship between A1c and FBS of the population of the study.[12] HbA1c is an index for the blood glucose for past 2-3 months and is a better index for evaluating control of diabetes in the patients. Its normal range in a normal human being is between 4.5 and 6.7%.[13] In this study, the average of HbA1c in controlled patients was 5.93% and in uncontrolled patients was 8.63% and HbA1c range above 6.7% was considered as uncontrolled patients. In our studied population, 52% of the patients had uncontrolled disease. A similar study from South Africa reported an average of 11.2% HbA1c in their patients[14] wherein loss of therapeutic facilities was the major reason for the high rate in uncontrolled patients. However, in our study, noncompliance with the diet prescribed by the physician and lack of timely medicine intake were the main reasons for uncontrolled disease. Previous studies have reported 53% and 84.3% of the patients with uncontrolled disease,[14,15] which was attributed, respectively, to nondiet factors and high stress.[15] In this study, 9 patients had the history of hospitalization, among which 4 of them were admitted because of diabetic foot ulcers, 3 of them because of renal transplantation, and two of them because of hyperglycemia. A similar rate of hospitalization because of hyperglycemia is previously reported. However, the average HbA1c in this study was 7.66% and 56% of patients had uncontrolled disease.[16]
In this study, 37.03% of the patients used insulin and 79.6% used metformin tablet for treatment. In tablet consumers, 61% took single tablets, 33% took two types of drugs and 3% took three types of drugs, but in a similar study, 84% of the patients used oral medications for treatment, among which 68% used single type, 27% used two types and 4% used three types of drugs for treatment. However, in their study, metformin was the main type of oral medication.[16] Both in this study and previous study, 65% of the controlled patients used metformin for oral medication. Interestingly, we did not find any relationship between aging and control of the disease (P = 0.204). However, aging is associated with physiological and psychological changes and reduces abilities and life quality of the patients.[1] But our finding indicates that patients with young age had less knowledge about the disease and did not care about controlling their disease and hence there was no significant difference between aging and control of the disease. The BMI calculated in our study was 27.31kg/m2, which was less similar to previous reports.[17] This result indicates that in our study because of daily exercise by the patients, they had relatively favorable weight and were taller which led to less BMI than the previous report.[17] In our study, there was a significant relationship between education and control of the disease but Millar et al. could not find any significant relationship between education and control of the disease.[17] Our educated patients had enough knowledge on how to control their disease; they had experience of googling about diet and controlling their disease. In this study, 81.48% of the patients had a history of the disease in one of their close relatives, which was higher than similar studies with a report of 58% family history of the disease.[18] Most of the family history in our study was in sons and brothers.
In this study, 72% of the patients who visited doctor twice or less during a year had controlled disease, but 60% of the patients who visited doctor every 3 months or less had uncontrolled disease, which can be due to higher stress and anxiety (P = 0.011). These results can indicate the role of stress in controlling the disease, which was previously suggested by others.[19] Voluntarily participation and random selection of the patients in this study can explain the role of visiting a doctor on developing uncontrolled disease and we can conclude the importance of less stress consequent to interactions with doctors and family members in control of the disease. In addition, sport has a crucial role for controlling the disease. Several studies indicated that sports could increase body sensitivity to insulin and reduce FBS and control of the diabetes.[20,21] However, most of the patients conventionally are reducing their sport and exercises after disease[22] but in our study, 65% of the patients engaged themselves in a 2 h of exercise per week had controlled disease. We have to consider the destruction of red blood cells as one of the reasons for lower HbA1c measurement, which can lead to missing identification and control of the disease in diabetic patients.
CONCLUSION
The findings of this study indicates that less stress, education, and weekly exercise had a significant role in controlling disease progression in diabetic patients from the Northwest of Iran and noncompliance with the prescribed diet by the physician and lack of timely medicine intake were the main reasons for uncontrolled disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We thank all staff of Imam Reza Hospital, Tabriz, Iran for their collaboration in sample collection. We also thank Central Laboratory of IRH for their collaboration and participation. This study was funded by Drug Applied Research Center, Tabriz University of Medical Sciences. All diabetic patients voluntarily completed questionnaire and gave sample for blood analysis and all procedures performed in our study were in accordance with the ethical standards of the Ethical Committee of Tabriz University of Medical Sciences on behalf of Ministry of Health of Iran and were according to the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
REFERENCES
- 1.Miksch A, Hermann K, Rölz A, Joos S, Szecsenyi J, Ose D, et al. Additional impact of concomitant hypertension and osteoarthritis on quality of life among patients with type 2 diabetes in primary care in Germany — A cross-sectional survey. Health Qual Life Outcomes. 2009;7:19. doi: 10.1186/1477-7525-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rafraf M, Bazyun B, Sarabchian M, Safaeiyan A. Effect of vitamin E supplementation on metabolic status and serum lipoprotein (a) level in type 2 diabetics. Zanjan Univ Med Sci J. 2014;22:84–94. [Google Scholar]
- 3.Bell DS. Combination therapy for type 2 diabetes. Am Fam Physician. 2001;64:1812–1814. [PubMed] [Google Scholar]
- 4.Eid M, Mafauzy M, Faridah A. Glycaemic control of type 2 diabetic patients on follow up at hospital Universiti Sains Malaysia. Malays J Med Sci. 2003;10:40–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 6.Diabetes Atlas. 5th ed. Brussels: International Diabetes Federation; 2011. Diabetes Atlas. Available from: http://www.idf.org/diabetesatlas . [Google Scholar]
- 7.Kamal Alanani NM, Alsulaimani AA. Epidemiological pattern of newly diagnosed children with type 1 diabetes mellitus, Taif, Saudi Arabia. ScientificWorldJournal 2013. 2013 doi: 10.1155/2013/421569. 421569. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Mahdavi AR, Etemad K, Haider M, Alavinia SM. The effect of seeing a family physician on the level of glycosylated hemoglobin (HbA1c) in type 2 diabetes mellitus patients. J Diabetes Metab Disord. 2013;12:2. doi: 10.1186/2251-6581-12-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsanasab H, Pudeh BM, Alizadeh A, Abediankenari S. Evaluation of correlation between HbA1c with the risk factors of lipid profile in patients with type 2 diabetes. J Mazandaran Univ Med Sci. 2013;22:153–6. [Google Scholar]
- 10.Kooshyar H, Shoorvazi M, Dalir Z, Hosseini M. Health literacy and its relationship with medical adherence and health-related quality of life in diabetic community-residing elderly. J Mazandaran Univ Med Sci. 2014;23:134–43. [Google Scholar]
- 11.Côté I, Grégoire JP, Moisan J, Chabot I. Quality of life in hypertension: The SF-12 compared to the SF-36. Can J Clin Pharmacol. 2004;11:e232–8. [PubMed] [Google Scholar]
- 12.Goldstein DE, Walker B, Rawlings SS, Hess RL, England JD, Peth SB, et al. Hemoglobin A1c levels in children and adolescents with diabetes mellitus. Diabetes Care. 1980;3:503–7. doi: 10.2337/diacare.3.4.503. [DOI] [PubMed] [Google Scholar]
- 13.Gillery P, Hue G, Bordas-Fonfrède M, Chapelle JP, Drouin P, Lévy-Marchal C, et al. Hemoglobin A1C determination and hemoglobinopathies: Problems and strategies. Ann Biol Clin (Paris) 2000;58:425–9. [PubMed] [Google Scholar]
- 14.Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE. NGSP Steering Committee. The national glycohemoglobin standardization program: A five-year progress report. Clin Chem. 2001;47:1985–92. [PubMed] [Google Scholar]
- 15.Rotchford AP, Rotchford KM. Diabetes in rural South Africa - an assessment of care and complications. S Afr Med J. 2002;92:536–41. [PubMed] [Google Scholar]
- 16.Burgmann K, Fatio S, Jordi B, Rutishauser J. Medical care of type 2 diabetes mellitus in light of international and national recommendations: A retrospective analysis. Swiss Med Wkly. 2013;143:w13871. doi: 10.4414/smw.2013.13871. [DOI] [PubMed] [Google Scholar]
- 17.Millar A, Cauch-Dudek K, Shah BR. The impact of diabetes education on blood glucose self-monitoring among older adults. J Eval Clin Pract. 2010;16:790–3. doi: 10.1111/j.1365-2753.2009.01195.x. [DOI] [PubMed] [Google Scholar]
- 18.Trief PM, Wade MJ, Britton KD, Weinstock RS. A prospective analysis of marital relationship factors and quality of life in diabetes. Diabetes Care. 2002;25:1154–8. doi: 10.2337/diacare.25.7.1154. [DOI] [PubMed] [Google Scholar]
- 19.Surwit RS, van Tilburg MA, Zucker N, McCaskill CC, Parekh P, Feinglos MN, et al. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25:30–4. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- 20.Zisser H, Gong P, Kelley CM, Seidman JS, Riddell MC. Exercise and diabetes. Int J Clin Pract Suppl. 2011;65:71–5. doi: 10.1111/j.1742-1241.2010.02581.x. [DOI] [PubMed] [Google Scholar]
- 21.Santhanakrishnan I, Lakshminarayanan S, Kar SS. Factors affecting compliance to management of diabetes in Urban Health Center of a tertiary care teaching hospital of south India. J Nat Sci Biol Med. 2014;5:365–8. doi: 10.4103/0976-9668.136186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aylin K, Arzu D, Sabri S, Handan TE, Ridvan A. The effect of combined resistance and home-based walking exercise in type 2 diabetes patients. Int J Diabetes Dev Ctries. 2009;29:159–65. doi: 10.4103/0973-3930.57347. [DOI] [PMC free article] [PubMed] [Google Scholar]


