Abstract
Team-based models of care are an important way to meet the complex medical and psychosocial needs of the homebound. As part of a quality improvement project to address patient, program, and system needs, we restructured a portion of our large, physician-led academic home-based primary care practice into a team-based model. With support from an office-based nurse practitioner, a dedicated social worker, and a dedicated administrative assistant, physicians were able to care for a larger number of patients. Hospitalizations, readmissions, and patient satisfaction remained the same while physician panel size increased and physician satisfaction improved. Our Team Approach is an innovative way to improve interdisciplinary, team-based care though practice restructuring and serves as an example of how other practices can approach the complex task of caring for the homebound.
Keywords: multidisciplinary care, team based care, nurse practitioner, homebound
INTRODUCTION
As the population ages and the prevalence of individuals living with multiple chronic conditions continues to grow, the number of chronically ill elders who are homebound will grow as well 1. Compared to their non-homebound counterparts, the homebound have a disproportionately high disease and symptom burden, significant functional limitations, and higher mortality 2-4. Homebound individuals often require more complex care that addresses not only medical needs related to their chronic illnesses, but also psychosocial needs that arise in part due to their isolation from traditional social supports and services 3,5.
Innovative care delivery models attempt to meet the complex needs of the homebound and demonstration projects such as Independence at Home promote models of care that maintain or improve the quality of care while reducing healthcare costs 6,7. Strong primary care with a focus on care coordination is an important way to improve the quality of care for patients with complex chronic illness while at the same time limiting the costs of their care 8. For the most complex patients, this is often best accomplished using a team-based model of care 8-10.
Providing care for individuals with multiple medical and psychosocial needs is challenging and may increase physician burden and contribute to burnout 11. Burnout is common among primary care physicians 12 and may be related to increased productivity expectations as well as a growing amount of administrative and patient care work that happens outside of the patient encounter itself 13,14. While there is no simple cure for primary care physician burnout, research suggests that well-functioning, team-based models of care may help to improve physician job satisfaction and decreased physician burnout 9,15 and may be particularly helpful in care of complex populations such as the homebound.
The Mount Sinai Visiting Doctors (MSVD) is the nation’s largest academic home-based primary care program and serves approximately 1000 homebound patients annually in Manhattan 16. Since its inception, physicians have coordinated nearly all aspects of patient care. In order to meet the growing demand for the program’s services, we sought to pilot a new team-based model of care that increased our capacity to care for patients while also improving patient access to immediate telephonic care. Our goal was to more efficiently utilize all members of the care team by distributing responsibilities amongst the team.
Our pilot, referred to as the “Team Approach,” was designed to improve clinical outcomes, remain cost-effective, and be acceptable to both patients and physicians. The structure and development of the Team Approach to home-based primary care are described below and a comparison of the Team Approach and usual care hospitalization rates and patient and physician satisfaction are presented.
METHODS
Intervention Setting
Described in detail elsewhere 16,17, the Mount Sinai Visiting Doctors program was founded in 1995 and employs an interdisciplinary team to provide primary care for patients in their homes. To be enrolled in the program, patients must meet the Medicare definition of homebound: able to leave home only with great difficulty and for absences that are infrequent or of short duration 18. Newly enrolled MSVD patients are 75% female and nearly 70% are over the age of 80. Thirty six percent are white, 32% are Hispanic, and 22% are black. Forty three percent have Medicaid and 32% live alone. Ninety one percent require assistance with at least one activity of daily living (ADL) and 99% require assistance with at least one instrumental activity of daily living (IADL). Chronic disease is highly prevalent with 49% of patients carrying a diagnosis of dementia, 26% with depression, 18% with chronic lung disease, and 13% with cancer. Forty three percent have severe symptom burden 19.
Demand for the MSVD program services exceeds the capacity of the program to see patients and there is generally a wait time of weeks to months for newly referred patients. The MSVD team includes physicians, nurse practitioners, registered nurses, social workers, and administrative assistants. The program is supported by the Icahn School of Medicine at Mount Sinai and is a site for medical student, resident, and fellow education. Additional support for MSVD comes from the Mount Sinai Hospital as well as from philanthropy.
A full time physician in the program carries a panel of 90-100 patients. There were 7.8 FTE physicians at the time of this pilot. Physicians bill Medicare, Medicaid, or commercial insurance with fee-for-service charges using home visit codes. Home visits occur during the morning through mid-afternoon and physicians provide extensive telephonic care coordination during the remainder of the day. Physicians visit patients on average every 6 to 10 weeks but can make more frequent home visits or urgent home visits when needed. On a rotating schedule, physicians are assigned to perform urgent visits for patients with acute clinical changes. Physicians coordinate all aspects of care including follow up of imaging studies and laboratory work, coordination of equipment and supply orders, placement of specialty referrals, and supervision of nursing care and social services provided by community-based agencies. All information from patient visits and phone calls is documented in the electronic medical record (EMR).
The two nurse practitioners at MSVD fill a flexible role in the practice that includes direct patient care in the form of urgent visits, quality and performance improvement activities, support as needed during registered nurse triage, and oversight of care transitions for MSVD patients. In addition to screening and triaging referrals to the program, the two registered nurses at MSVD triage incoming clinical calls and page physicians with any urgent clinical issues. They then assist physicians in facilitating urgent community nursing services and arranging for emergency room evaluation when needed. Non-urgent clinical messages and other non-clinical messages are routed to the physicians via the EMR and are addressed when physicians return to the office after visits.
Physicians place referrals as needed to MSVD social workers to help address specific issues such as home care services, financial issues, caregiver and patient coping, and concerns for abuse or neglect. Approximately one-third of patients in the practice are actively followed by social work at a given time. There is approximately one full time social worker for every two physician FTE 20.
Administrative assistants answer all calls and route calls to physicians and registered nurses as needed. Administrative assistants are each assigned roles to meet other practice needs: scheduling and confirming physician appointments, scheduling specialty appointments, scheduling labs and imaging studies, coordinating transportation for patients as needed, ordering all necessary patient supplies and DME. There is approximately one administrative assistant for every two physician FTE.
Intervention Description
In order to meet growing demand for MSVD’s services, the program leadership conducted informal discussions with all staff members to explore ways to expand the program’s capacity while trying to better meet the needs of the patient and the program’s interdisciplinary team. The following issues were identified: First, registered nurses only contacted physicians with the most urgent clinical patient issues while physicians were on visits in the community. In general, patients and families had to wait until the end of the day to have their clinical needs addressed; this sometimes delayed needed care. Second, social worker involvement was largely reactive in nature and relied on physician referrals, which often delayed social work interventions or limited the social worker’s interventions to crisis management. Third, physicians faced large volumes of telephone calls from patients, caregivers, nursing agencies, vendor companies, and pharmacies upon the physician’s return to the office after seeing patients each day. This work was time consuming and could perhaps be better handled by other members of the interdisciplinary team.
With these needs in mind and using existing team-based models of care as a guide 10,21, we restructured a portion of our practice to implement and evaluate a Team Approach to care that would address these patient, program, and system concerns (Figure 1.) Mount Sinai has long been supportive of the clinical and educational missions of MSVD and heavily subsidizes the program’s cost. Additional grant funding was obtained to enact the staffing changes required for this pilot. All Team Approach team members volunteered to take part in the pilot and participation in the pilot did not affect their salary or compensation. When the pilot began, patients whose physicians chose to take part in the pilot were assigned to the Team Approach. During the pilot, all new referrals to the practice were randomly assigned to Team Approach or usual care based on physician availability.
Figure 1. Practice Needs and Team Approach Intervention at the Mount Sinai Visiting Doctors Program.
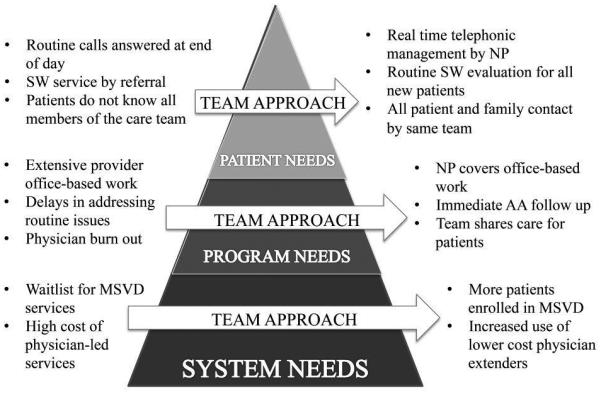
*NP= nurse practitioner, SW= social worker, AA= administrative assistant
Table 1 compares the differences in staffing and personnel cost between the Team Approach and usual care. The new team consisted of two full-time physicians, one full-time nurse practitioner, one full-time social worker, and one full-time administrative assistant. In the second year of the pilot one full time physician decreased his hours and an additional part-time physician was added to the team to maintain 2 FTEs in the Team Approach. These team members worked only with Team Approach patients. The two RNs in the practice continued to jointly serve both Team Approach and usual care patients. Importantly, the Team Approach had an increased ratio for NP to MD FTE as compared to usual care: there was one NP for every 2 MDs in the Team Approach and there was 1 NP for approximately every 6 MDs in usual care. The ratio of SW, AA, and RN to MDs remained approximately the same between the Team Approach and usual care.
Table 1.
Comparison of Staffing and Personnel Cost Between Team Approach and Usual Care at the Mount Sinai Visiting Doctors Program
| Position | Team Approach | Usual Care | |||
|---|---|---|---|---|---|
| Salary ($)/ FTE* |
FTE | Cost ($) | FTE | Cost ($) | |
| Medical Doctor |
140,000 | 2 | 280,000 | 5.8 | 812,000 |
| Nurse Practitioner |
100,000 | 1 | 100,000 | 1 | 100,000 |
| Administrative Assistant |
40,000 | 1 | 40,000 | 3 | 120,000 |
| Social Worker | 52,000 | 1 | 52,000 | 2.6 | 135,200 |
| Registered Nurse |
75,000 | 0.5 | 37,500 | 1.5 | 112,500 |
| Total Annual Personnel Cost ($) |
509,500 | 1,279,700 | |||
| Number of Patients Cared For** |
260 | 522 | |||
| Personnel Cost per Patient Cared For ($) |
1,960 | 2,452 | |||
FTE= full time equivalent
based on panel size per Medical Doctor FTE: Team Approach 130 patients, usual care 90 patients
While physicians continued to visit patients at home and bill for their services, the nurse practitioner was primarily office-based. She continually reviewed each Team Approach physician’s EMR messages and addressed urgent clinical issues from the office within minutes. She also initiated real-time management of non-urgent clinical and non-clinical issues such as medication refills, durable medical equipment orders, communication with community nurses, and coordination with other providers. In addition, the nurse practitioner was available to follow patients admitted to inpatient care facilities and conduct select follow-up, urgent, and post-discharge visits. These visit days were arranged to coincide with days when physicians were in the office and available to address their own calls.
The social worker performed a psychosocial intake on all new Team Approach patients upon enrollment and proactively addressed any psychosocial issues. If new issues arose, the social worker continued to respond to all referrals for social work services. Rather than be assigned to a particular task for the whole practice, the administrative assistant addressed all needed administrative needs for Team Approach patients such as scheduling specialty appointments, labs, and radiology, coordinating transportation for patients as needed, and ordering all necessary patient supplies and durable medical equipment. Because she was more familiar with the patients and their needs, she could more assertively follow-up on pending orders.
Day-to-day communication among team members occurred via the EMR and informal office conversations. In addition, weekly team meetings with all team members were initiated to discuss newly enrolled patients and complex cases. Although no formal unified patient care plan was created, each discipline led discussions about the logistical, psychosocial, and medical domains of the most complex patients’ care. During these meetings the team also discussed the implementation of the Team Approach and used an iterative process to make needed adjustments to the team members’ responsibilities and work flows.
Because of increased support from the nurse practitioner, social worker, and administrative assistant, we projected that physicians would be able to increase their panel size by 40% as compared to a usual care physician and therefore manage an active panel of approximately 130-150 patients. When a physician was out of the office, he or she was covered by the other Team Approach physician or the nurse practitioner. When possible, urgent visits and hospital discharge visits were performed by Team Approach physicians or the nurse practitioner.
Outcomes and Analysis
The Team Approach was implemented in August of 2009 and evaluation of the Team Approach occurred from January 2010 until December 2011. During this time, all patients who were newly referred to the program were assigned to the next available physician regardless of Team Approach or usual care affiliation.
We used the EMR to obtain basic demographic information about all patients enrolled in MSVD in 2010 and 2011 and used chi square tests to compare the characteristics of Team Approach patients to those receiving usual care patients.
We obtained information about hospital admissions and readmissions at Mount Sinai Hospital for all MSVD patients from the EMR. We described the characteristics of hospital admissions and 30 day readmissions for both Team Approach and usual care patients in 2010 and 2011. We calculated how many days patients were active in the program in both 2010 and 2011 and then calculated the number and rates of admissions and 30 day readmissions. We used chi square and Wilcoxon rank sum tests to compare the differences between Team Approach and usual care patients. We performed all analysis using SAS version 9.2 (SAS Institute, Inc., Cary, NC.)
We evaluated initial patient satisfaction using an annual patient survey administered by the Survey Center at Mount Sinai Hospital distributed in April of 2010. In addition to standard questions related to patient satisfaction with the program in general, questions specifically addressed satisfaction with, identification with, and availability of team members involved in the Team Approach. We used a chi square test to compare differences in satisfaction between Team Approach and usual care.
In order to evaluate physician satisfaction, we developed and administered an anonymous online survey to all MSVD physicians in January of 2011. Physicians indicated if they were involved with the Team Approach and then responded to questions about job satisfaction. Most responses were on a five-point Likert scale and trends in physician satisfaction are reported.
We used average 2010 staff salaries to calculate personnel costs for the Team Approach and usual care. We then calculated the personnel cost per patient cared for based on a MD panel size for 130 in the Team Approach and 90 in usual care.
RESULTS
During the two-year study period the Team Approach served 347 patients and usual care approach served 1074 patients. Each Team Approach physician carried a panel of approximately 130 patients. During the same time period, usual care physicians continued to carry a panel of about 90 patients. Approximately 50% of urgent visits for Team Approach patients were performed by Team Approach providers. All Team Approach patients had visits following hospital discharge and 100% of hospital discharge visits were performed by Team Approach providers.
Table 2 describes select demographic characteristics for Team Approach patients and usual care patients and reports p-values assessing differences between the groups. There were no statistically significant differences in age, gender, ethnicity, and Medicaid status between the two groups.
Table 2.
Characteristics of Mount Sinai Visiting Doctors Patients
| Characteristic | Team (n=347) | Usual Care (n=1074) |
p-value |
|---|---|---|---|
| Age (years) | 81.4 | 80.2 | 0.2 |
| Female | 77.8% | 74.9% | 0.3 |
| Medicaid | 35.7% | 40.2% | 0.1 |
| Ethnicity | |||
| White | 37.8% | 40.8% | 0.3 |
| Black | 29.7% | 23.2% | |
| Latino | 26.5% | 31.9% | |
| Other | 6.1% | 4.0% |
Table 3 presents data about hospitalization and 30 day readmissions at Mount Sinai Hospital for Team Approach and usual care patients during the 2 year study period. On average, 32.6% of Team Approach patients and 29.4% of usual care patients were hospitalized during 2010 and 2011 (p= 0.28). There were no statistically significant differences between mean hospitalizations per patient (0.59 and 0.57, p=0.82) and annual hospital admission rate (0.73 and 0.82, p=0.39) between Team Approach and usual care patients. Similarly, there were no statistically significant differences between percentage of patients with readmissions (22.1% and 20.6%, p=0.73) or percentage of hospitalizations that resulted in readmission (9.7% and 9.1%, p=0.73) between Team Approach and usual care patients.
Table 3.
Hospitalization and 30 Day Readmission in 2010 and 2011 at the Mount Sinai Visiting Doctors Program
| Variable | Team (n=347) | Usual Care (n=1074) |
P-value* | |
|---|---|---|---|---|
| Hospitalizations, total | 205 | 614 | ||
| Mean per Patient (range) |
0.6 (0-6) | 0.6 (0-24) | 0.8 | |
| Mean Person Days of Observation (range) |
462.6 (6-730) |
423.3 (1-730) |
||
| Annual Hospital Admission Rate per Patient |
0.7 | 0.8 | 0.4 | |
| Patients with Any Hospital Stay, n (%) |
113(32.6%) | 316 (29.4%) | 0.3 | |
| 30 Day Readmissions, total | 32 | 127 | ||
| Patients with Any Readmission, n (%) |
25 (7.2%) | 65 (6.1%) | ||
| Hospitalized Patients with Readmission, % |
22.1 | 20.6 | 0.7 | |
| % Hospitalizations Resulting in Readmission |
9.7% | 9.1% | 0.7 | |
P value based on chi square tests and Wilcoxon rank sum tests
837 personalized surveys were mailed to MVSD patients to be completed by patients or by caregivers if patients were unable. A total of 330 responses were received (39% response rate.) Team Approach patients completed 59 of these surveys and usual care patients completed 263 surveys (team approach status could not be determined for 8 respondents). In general, all MSVD patients were highly satisfied with their care regardless of their Team Approach status. 63% of Team Approach patients and 67% of usual care patients rated their overall quality of care a 10 on a scale from 0 to 10 (where 0 is the worst and 10 is the best). Both Team Approach and usual care patients reported seeing their provider as often as necessary (95% Team Approach and 96% usual care) and found nurses helpful (100% Team Approach and 99% usual care) and social workers helpful (85% Team Approach and 80% usual care.) None of these differences were statistically significant.
Likewise, there were no statistically significant differences between patient perceptions of team roles and functioning. The majority of patients felt there was a team of providers and staff who care for them (75% Team Approach and 66% usual care) and felt confident in the recommendations made by nursing staff (100% Team Approach and 99% usual care.) Nearly all patients felt that they were able to speak to a doctor if they needed to do so (98% Team Approach and 99% usual care.)
Physician survey responses were obtained for the three Team Approach physicians and eleven usual care physicians, representing a 100% response rate among MSVD physicians. All Team Approach physicians strongly agreed that they were adequately meeting patient’s needs while only two of eleven usual care physicians strongly agreed with this statement. No Team Approach physicians reported feeling emotionally drained from work while four of eleven usual care physicians reported feeling emotionally drained. Two of three Team Approach physicians strongly agreed that their workload was manageable while only three of eleven usual care physicians agreed.
Table 1 presents the personnel cost comparison between Team Approach and usual care. While annual personnel costs were higher for the Team Approach, Team Approach providers cared for a larger number of patients. As a result, personnel cost per patient cared for was 20% less in the Team Approach than the usual care model ($1,960 and $2,452 respectively.)
DISCUSSION
Our study demonstrates the feasibility, acceptability, and comparability of care of home-based primary care services delivered by a structured team-based model of care that includes physicians, a nurse practitioner, a social worker, and an administrative assistant. The Team Approach succeeded in instituting real-time office-based management of patient issues by a nurse practitioner and increased physician capacity to provide direct patient care, while creating a stronger interdisciplinary team. This occurred without negatively impacting clinical outcomes, patient satisfaction, or physician satisfaction.
During the implementation of the Team Approach, we made several minor adjustments to our original plan. Though we initially set a goal of between 260 and 300 patients for the Team Approach, we found that 260 patients was the most feasible panel size. While we had anticipated that the greatest challenge would be for the physicians due to their increased panel size in the Team Approach, we observed that it was instead the workload for non-physician staffing that determined panel size. We expected that the nurse practitioner would help most with straightforward cases, freeing physicians up to address complex patient care situations when they returned to the office. However, the nurse practitioner instead took an enhanced role in the management of the most complex patients on the Team Approach physician panels. She often arranged for proactive home visits to address poorly controlled chronic health problems. Because of the large volume of office-based work, the nurse practitioner had to limit the number of urgent, follow-up, and hospital visits performed and visited patients only one day a week. Similarly, the social worker did a portion of initial intake visits via phone instead of with a home visit due to the demands of an increased caseload.
These modifications underscore the importance of assessing needs and capacity of non-physician members of the team as well as the importance of regular meetings to address program needs and make changes as needed. We also found that these meetings provided an opportunity for team members to express their own frustrations and get support from the team, which may have contributed to improved physician satisfaction among Team Approach physicians.
While we hypothesized that the increased care coordination and easy accessibility of immediate office-based, telephonic management would lower rates of hospitalization and 30-day readmission, there was no difference in hospitalization or readmission rates for Team Approach patients as compared to the usual care patients. This lack of association may be due to unmeasured clinical differences between the Team Approach and usual care patients. Alternatively, the potential benefits of care coordination and telephone management by the Team Approach may not have been realized because the Team Approach providers and staff were caring for significantly more patients. While most MSVD patients are hospitalized at Mount Sinai Hospital, the fact that only hospitalizations at Mount Sinai Hospital are recorded also may have impacted our ability to detect differences between the groups.
We are encouraged that there was no decrease in satisfaction for team approach patients despite the fact that Team Approach physicians cared for a larger patient panel. These findings are consistent with other research suggesting that well-functioning teams improve patient satisfaction 9,10. Importantly, the Team Approach nurse practitioner, social worker, and administrative assistant managed many patient issues that were traditionally addressed only by the physician. Such team restructuring allows non-clinical staff to assume more responsibility for patient care issues that do not require a physician-level intervention and represents an approach to primary care 22 that is equally, and possibly more, satisfactory to patients.
Physician survey data suggests that Team Approach physicians were more satisfied and felt more able to meet patient needs while maintaining their own emotional health. Team Approach physicians chose to participate in this pilot and this may have impacted the high levels of satisfaction reported. Yet as compared to usual care, the Team Approach has more in common with other high-functioning primary care practices where physicians are highly satisfied: sharing care among non-physician team members, limiting physician responsibility for tasks not requiring physician-level intervention, improving team communication, formalizing work flows, and clarifying team member roles 23. Future program evaluation should assess non-physician team member satisfaction with the Team Approach, which was not formally assessed in this pilot.
As with any pilot program, it is essential to consider the program’s cost effectiveness as compared to usual care. In addition to the decreased personnel cost per patient cared for by the Team Approach, additional revenue generated by the Team Approach should also be considered. Because of patient panel sizes, the Team Approach increased each physician’s capacity to see patients by 40% and the revenue generated by this volume of additional visits could potentially offset the costs of the nurse practitioner’s salary. For example, the Team Approach employed an additional 0.3 FTE nurse practitioner at an additional cost of approximately $30,000 per year per MD FTE (Table 1). If a typical patient is seen 6 times per year and Medicare’s reimbursement for a home visit is approximately $130, each additional patient generates $780 per year. The Team Approach allowed each full time physician to follow another 30 patients per year, which resulted in an estimated $46,000 in additional revenue. This more than covers the additional $30,000 in salary costs for the nurse practitioner. In addition, revenue from the nurse practitioner’s own visits would further offset the cost of her salary.
Future work should prospectively track clinical revenue and provider costs. When we retrospectively reviewed productivity information, we found that issues such as incomplete tracking of nurse practitioner productivity, multiple part time physicians with limited and fluctuating clinical responsibilities, and intermittent physician leaves of absence limited our ability to accurately compare program costs for the Team Approach and usual care at MSVD.
The Team Approach succeeded in meeting MSVD’s goals to serve more patients, improve our program’s ability to provide immediate telephonic care, and improve job satisfaction and reduced burden for physicians. As a result, MSVD has disseminated the Team Approach to the rest of our practice in various ways. It was quickly evident that having the administrative assistant work with an individual physicians rather than perform one task for the whole practice improved efficiency and facilitated coverage; in 2011 this administrative assistant-physician pairing system was adopted for the whole practice. Following the pilot, a second similarly structured team was created and MSVD is currently in the process of securing funding to transition our entire practice into physician, nurse practitioner, social worker, and administrative assistant teams. In addition, we are developing an alternative model for caring for our most complex patients whereby a nurse practitioner co-manages a subset of each physician’s high-need patients; this model is directly based on lessons we learned while implementing the Team Approach. While interdisciplinary care has long been the standard of care at MSVD, we are among those who believe that in order to meet population need, primary care must move towards a thoughtfully designed, team-based model of care 22,24.
While we analyzed outcomes related to several key aspects of the pilot, there are limitations to our evaluation. As mentioned previously, we did not collect data on hospitalizations outside of Mount Sinai, satisfaction for non-physician staffing, and individual provider productivity and billing information. In addition, further information about the day-to-day activities of non-physician team members and an assessment of the relationships among team members would further elucidate the essential differences between the Team Approach and usual care. Finally, the Team Approach may not be generalizable to other practice settings where other patient needs, financial constraints, and delivery system structures may dictate different standards of care for the homebound or those with complex chronic illness.
However, we believe that our approach to the design and implementation of the Team Approach is useful to others seeking ways to bring team-based care to their practice. In particular, others should consider the needs of the patient, program, and system in the design of interventions in order to get maximal impact from program changes. For example, if the MSVD nurse practitioner carried her own panel of patients, MSVD’s capacity to care for patients would have increased to similar levels as those that we achieved with the Team Approach. However, this would not have addressed other important needs like improving patient access to immediate care, proactive SW involvement, and redistributing physician administrative workload. While these needs are more difficult to measure than panel size or productivity goals, they must be addressed in order to provide sustainable, high quality primary care.
A team-based model of home-based primary care is the best way to meet complex biomedical and psychosocial needs of the homebound. While adequate program funding remains the most significant impediment to delivery of such care, health care reforms such as Independence at Home and Accountable Care Organizations may shift funding away from a fee-for-service billing system and provide new opportunities for routine incorporation of team-based care for the homebound 6. The Team Approach provides an important example of how such team-based care benefits patients, programs, and the system as a whole.
Footnotes
The development of the Team Approach at MSVD has been made possible by the generous donations of the following foundations: The Fan Fox and Leslie R. Samuels Foundation, The Radio Drama Network, and the Y.C. Ho/Helen and Michael Chiang Foundation.
REFERENCES
- 1.A Profile of Older Americans: 2011. U.S. Department of Health and Human Services; 2011. Accessed at http://www.aoa.gov/aoaroot/aging_statistics/Profile/2011/docs/2011profile.pdf. [Google Scholar]
- 2.Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358–62. doi: 10.1111/j.1532-5415.2010.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kellogg FR, Brickner PW. Long-term home health care for the impoverished frail homebound aged: a twenty-seven-year experience. J Am Geriatr Soc. 2000;48:1002–11. doi: 10.1111/j.1532-5415.2000.tb06902.x. [DOI] [PubMed] [Google Scholar]
- 4.Qiu WQ, Dean M, Liu T, et al. Physical and mental health of homebound older adults: an overlooked population. J Am Geriatr Soc. 2010;58:2423–8. doi: 10.1111/j.1532-5415.2010.03161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ornstein K, Smith K, Boal J. Understanding and Improving the Burden and Unmet Needs of Informal Caregivers of Homebound Patients Enrolled in a Home-Based Primary Care Program. Journal of Applied Gerontology. 2009;28:482–503. doi: 10.1177/0733464808329828. [DOI] [PubMed] [Google Scholar]
- 6.DeCherrie LV, Soriano T, Hayashi J. Home-based primary care: a needed primary-care model for vulnerable populations. The Mount Sinai journal of medicine, New York. 2012;79:425–32. doi: 10.1002/msj.21321. [DOI] [PubMed] [Google Scholar]
- 7.Independence at Home Demonstration Fact Sheet August 2012. Centers for Medicare and Medicaid Services; 2012. Accessed September 2, 2012, at http://www.innovations.cms.gov/Files/fact-sheet/IAHfactsheet.pdf. [Google Scholar]
- 8.Boult C, Green AF, Boult LB, et al. Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's "retooling for an aging America" report. J Am Geriatr Soc. 2009;57:2328–37. doi: 10.1111/j.1532-5415.2009.02571.x. [DOI] [PubMed] [Google Scholar]
- 9.Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA : the journal of the American Medical Association. 2004;291:1246–51. doi: 10.1001/jama.291.10.1246. [DOI] [PubMed] [Google Scholar]
- 10.Litaker D, Mion L, Planavsky L, et al. Physician - nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients' perception of care. Journal of interprofessional care. 2003;17:223–37. doi: 10.1080/1356182031000122852. [DOI] [PubMed] [Google Scholar]
- 11.Adams WL, McIlvain HE, Lacy NL, et al. Primary care for elderly people: why do doctors find it so hard? The Gerontologist. 2002;42:835–42. doi: 10.1093/geront/42.6.835. [DOI] [PubMed] [Google Scholar]
- 12.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of internal medicine. 2012;172:1377–85. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 13.Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA : the journal of the American Medical Association. 2011;305:2009–10. doi: 10.1001/jama.2011.652. [DOI] [PubMed] [Google Scholar]
- 14.Farber J, Siu A, Bloom P. How much time do physicians spend providing care outside of office visits? Annals of internal medicine. 2007;147:693–8. doi: 10.7326/0003-4819-147-10-200711200-00005. [DOI] [PubMed] [Google Scholar]
- 15.Harris MF, Proudfoot JG, Jayasinghe UW, et al. Job satisfaction of staff and the team environment in Australian general practice. The Medical journal of Australia. 2007;186:570–3. doi: 10.5694/j.1326-5377.2007.tb01055.x. [DOI] [PubMed] [Google Scholar]
- 16.Smith KL, Ornstein K, Soriano T, et al. A multidisciplinary program for delivering primary care to the underserved urban homebound: looking back, moving forward. J Am Geriatr Soc. 2006;54:1283–9. doi: 10.1111/j.1532-5415.2006.00835.x. [DOI] [PubMed] [Google Scholar]
- 17.Ornstein K, Hernandez CR, DeCherrie LV, et al. The Mount Sinai (New York) Visiting Doctors Program: meeting the needs of the urban homebound population. Care management journals : Journal of case management ; The journal of long term home health care. 2011;12:159–63. doi: 10.1891/1521-0987.12.4.159. [DOI] [PubMed] [Google Scholar]
- 18.Medicare and Home Health Care 2013 Accessed June 26, 2013, at http://www.medicare.gov/publications/pubs/pdf/10969.pdf. [Google Scholar]
- 19.Wajnberg A, Ornstein K, Zhang M, et al. Symptom burden in chronically ill homebound individuals. J Am Geriatr Soc. 2013;61:126–31. doi: 10.1111/jgs.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reckrey JM, Gettenberg G, Ross H, et al. The critical role of social workers in home-based primary care. Social work in health care. 2014;53:330–43. doi: 10.1080/00981389.2014.884041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boyd CM, Boult C, Shadmi E, et al. Guided care for multimorbid older adults. The Gerontologist. 2007;47:697–704. doi: 10.1093/geront/47.5.697. [DOI] [PubMed] [Google Scholar]
- 22.Margolius D, Bodenheimer T. Transforming primary care: from past practice to the practice of the future. Health Aff (Millwood) 2010;29:779–84. doi: 10.1377/hlthaff.2010.0045. [DOI] [PubMed] [Google Scholar]
- 23.Sinsky CA, Willard-Grace R, Schutzbank AM, et al. In search of joy in practice: a report of 23 high-functioning primary care practices. Annals of family medicine. 2013;11:272–8. doi: 10.1370/afm.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saba GW, Villela TJ, Chen E, et al. The myth of the lone physician: toward a collaborative alternative. Annals of family medicine. 2012;10:169–73. doi: 10.1370/afm.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]


