Abstract
Patients from racial and ethnic minorities experience higher mortality after cardiac surgery compared to white patients, both during the early postoperative phase as well as long term. A number of factors likely explain poor outcomes in black and minority patients, which include differences in biology, comorbid health conditions, socioeconomic background, and quality of hospital care. Recent evidence suggests that a major factor underlying excess mortality in these groups is due to their over-representation in low-quality hospitals, where all patients regardless of race have worse outcomes. In this review, we examine the factors underlying racial disparities in outcomes after cardiac surgery, with a primary focus on the role of hospital quality.
Keywords: Racial disparity, Health disparities, Coronary artery bypass grafting, CABG, Hospital quality, Hospital outcomes, Quality improvement
Introduction
Over 400,000 cardiac surgeries are performed each year in the USA [1]. Pioneered more than 50 years ago, cardiac surgery, which includes coronary artery bypass graft (CABG) surgery and valve surgery, has been the cornerstone of treatment of ischemic and valvular heart disease [2]. Despite the decline in surgical volumes in recent years [3], cardiac surgery remains one of the most common operating room procedures in the USA [4].
Reducing mortality after cardiac surgery has been a major focus of regional as well as national quality improvement programs over the past two decades [5]. Refinement in operative techniques, greater use of arterial conduits, emphasis on pharmacotherapy at the time of discharge as well as the widespread participation in the Society of Thoracic Surgeons national quality improvement registry have led to more than 50 % reduction in cardiac surgical mortality—from 3.9 % in 1990 to 1.9 % in 2009 [6, 7]. Although significant progress in improving cardiac surgical outcomes has been achieved, racial and ethnic differences in outcomes following cardiac surgery have persisted [8, 9•]. Factors underlying racial differences in cardiac surgical outcomes may include biology and genetics, higher prevalence of comorbidities, socioeconomic and environmental factors, quality of care, and the complex interrelationship of these factors [10, 11]. Recent studies have shown that poor outcomes in blacks are in large part due to over-representation of black and minority patients in lower-quality hospitals. In this article, we review existing evidence regarding factors underlying racial disparities in outcomes of cardiac surgery, with a primary focus on the role of hospital quality. Given the relative paucity of literature on disparities in other ethnic groups (e.g., Hispanics), we will primarily focus this article on disparities between black and white patients.
Overview of Racial Disparities in Outcomes After Cardiac Surgery
A number of studies have showed that mortality and morbidity after cardiac surgery is significantly higher in black patients compared to white patients [12, 13]. In patients undergoing CABG, risk of early mortality is 1.5 times higher in blacks, and this difference in mortality is further magnified over long term [8, 9•] In a recent paper that used Medicare data 2007–2008, Rangrass et al. [14••] found that the risk of 30-day mortality after CABG in black Medicare beneficiaries was 35 % higher compared to whites. In another study of >30,000 patients from the Veterans Administration, Rumsfeld et al. [15] found that black race was associated with higher mortality (OR 1.52, 95 % CI 1.10 to 2.11, p=0.01) in patients with low surgical risk. This was due to a higher incidence of postoperative complications in black patients [15]. Furthermore, racial differences in clinical outcomes following cardiac surgery also persist long term. Using Medicare data, Konety et al. [9•] found that the risk of 3-month and 1-year mortality in black patients was 11 and 25 % higher compared to white patients. Differences in mortality difference were further magnified at 5 years, when risk-adjusted mortality in black patients was nearly twice that among white patients [16]. Similar differences in outcomes by race have also been reported in valve surgery and cardiac transplantation [17].
Proposed Mechanisms of Racial Differences in Outcomes
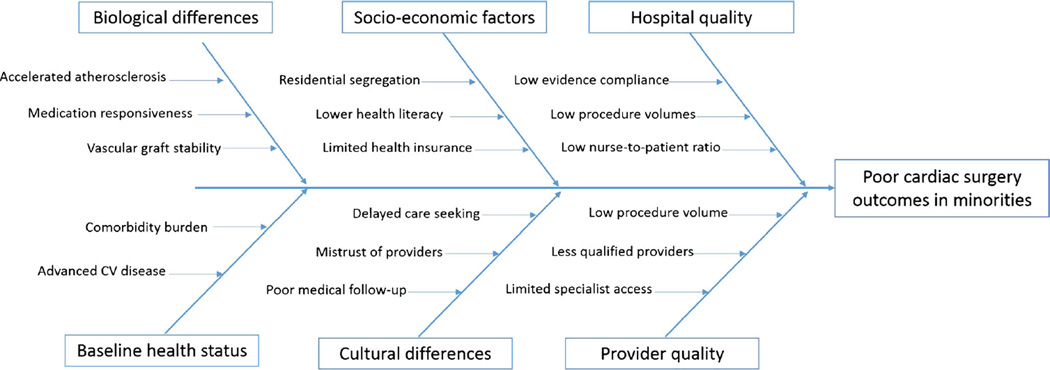
Although a number of studies have described racial differences in surgical outcomes, fewer studies have explained the mechanism of survival differences by race. The relationship between race and outcomes is likely to be multifaceted and includes biological and genetic differences, health status and comorbidities, and differences in social and physical environments (Fig. 1). However, a growing body of literature suggests that over-representation of black and minority patients at lower-quality hospitals may be a significant driver of racial differences in outcomes.
Fig. 1.
Root cause analysis of higher mortality in black and other minority patients after cardiac surgery
Biologic and Genetic Factors
Genetic differences between whites, blacks, and other ethnic minorities may be associated with 1) accelerated atherosclerotic disease progression in the African-American and Mexican-American populations [18–20], 2) differential pharmacological response to preventive therapy [18, 21, 22], and 3) vascular receptor profile differences which may be of particular importance in graft stability in post-bypass surgical patient [23]. However, genetic differences by race explain only a small proportion of the variation in cardiac surgical outcomes [24, 25]. Moreover, overemphasis on genetic differences between blacks and whites may detract from the importance of inequalities in care that account for a substantial proportion of racial differences in surgical outcomes [26, 27].
Health Status and Comorbidities
In a previous study of patients undergoing cardiac surgery, black patients were found to have a higher prevalence of diabetes (40 vs. 29 %), heart failure (26 vs. 18 %), and chronic renal disease (18 vs. 10 %), compared to white patients suggesting that patient-level differences in comorbidities may explain survival differences between blacks and whites [14••]. Although most studies have adjusted for patient-level differences, confounding by unmeasured disease severity cannot be entirely excluded. However, given that comorbidities account for <5 % of racial differences in survival [14••], it appears unlikely that racial differences in survival are entirely explained by unmeasured disease severity and comorbidities.
Socioeconomic and Cultural Factors
Socioeconomic status is an important determinant of overall health and can impact health outcomes in a number of important ways. It is a measure of financial well-being as well as overall educational status. On a direct level, it influences the ability to afford high-quality healthcare. Indirectly, socioeconomic status also influences behavior towards risk factors (e.g., smoking), seeking medical treatment, as well as periprocedural care [28, 29].
It is well known that African-American and Hispanic patients are more likely to be uninsured or underinsured [30], have less education, and lower income [31, 32]. In a study examining Medicare beneficiaries ≥65 years, Popescu et al. [33] demonstrated lower access to highly ranked hospitals among socially disadvantaged and ethnic minorities. Sociocultural differences and racial sensitization also affects rapport and trust between patients and physicians [34]. Black and white patient populations perceive health issues differently and have differing knowledge, attitude, beliefs, and practices [35]. This may contribute to the lower frequency of accepting medical advice, including recommendations for peri- or post-surgical care, which may contribute to outcome differences [36, 37].
The Role of Hospital and Provider Quality
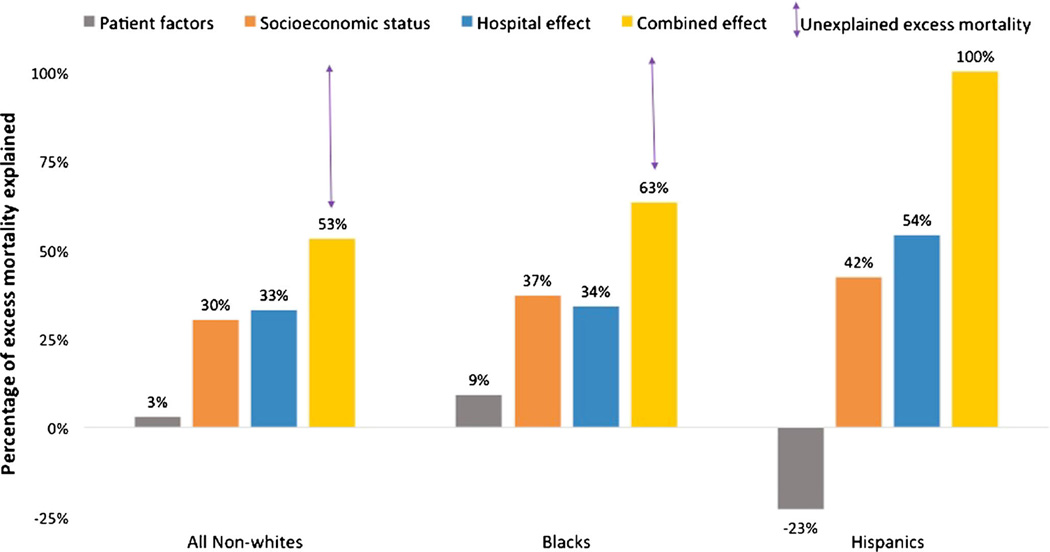
A number of studies have demonstrated that poor outcomes in racial and ethnic minorities may be largely due to the fact that blacks and other minority patients disproportionately seek care at poor-quality hospitals, which consistently underperform on several key measures of hospital quality. In the Rangrass study [14••], differences in the admitting hospital accounted for 34 % of the outcome differences between black and white patients and 54 % of the differences in outcomes between Hispanic and white patients. Socioeconomic status further explained more than 30 % of the disparities in clinical outcomes. In contrast, patient-level risk factors explained only 3 % of the mortality difference between black and white patients. Nevertheless, a significant proportion of the difference in outcomes remained unexplained, suggesting that other factors may be playing an important role (Fig. 2). In another study of Medicare beneficiaries, black patients undergoing several key cardiac surgical procedures (including CABG, aortic valve replacement, and aortic aneurysm repair) had a 20 % higher mortality compared to white patients, most of which was attributable to lower hospital quality [38]. Notably, the hospitals that disproportionately serve black and minority patients have lower surgical volumes and excess surgical mortality regardless of the patient’s race [39, 40]. In the Rangrass study [14••], hospitals with >18 % nonwhite CABG patients had 30 % excess CABG mortality in nonwhite patients and a 19 % higher CABG mortality in white patients, when compared to hospitals with <2 % nonwhite patients. These data suggest that worse outcomes in black and minority patients may be largely due to the fact that they predominantly seek care in poor-quality hospitals.
Fig. 2.
Relative contribution of patient factors, socioeconomic status, and hospital effect in excess 30-day mortality after coronary artery bypass grafting in Black and Hispanic Medicare beneficiaries. Bars represent the proportion of excess mortality that was explained after adjustment for the specified covariate (Representation of numerical data derived from study by Rangrass et al. [14••])
Konety et al. [9•] studied a cohort 591,139 black and white patients, 65 years and older, who underwent CABG between 1997 and 2000 at 1091 hospitals. After adjustment of patient characteristics, CABG mortality was 8, 11, and 25 % higher in black patients at 30 days, 90 days, and 1 year, respectively, compared to whites. Black patients were more likely to undergo CABG at hospitals with lower CABG volume and higher in-hospital mortality. After adjustment for hospital-level effects, differences in 30-day and 90-day outcomes between black and white patients disappeared. However, 1-year mortality remained significantly higher in black patients.
So why do black patients preferentially seek care at poor-quality hospitals? Although empirical data are limited, a number of factors may influence patients’ choice of specific hospitals and physicians.
Before the 1960s, segregation of health care by race was legal, and some states had separate hospitals for black and white patients as well as separate systems for training black physicians [41]. Although these practices are no longer sanctioned, old patient referral patterns may prevail, effectively limiting access to high-quality hospitals for blacks. Prior research suggests that residential segregation is an important factor in racial health disparities and may create differential access to high-quality hospitals. In a study using the Medicare database for the years 2000–2005, Vaughan-Sarrazin et al. [42•] examined the impact of racial heterogeneity at a community and hospital level on access to high-quality hospitals. They found that the likelihood of admission to a high-mortality hospital for treatment of acute myocardial infarction (AMI) was 35 % higher for blacks than that for whites in areas with high residential segregation, i.e., neighborhoods with an unevenly distributed large black population, but not significantly different in areas with low segregation, i.e., where the proportion of black and white patients were closer to the average and were distributed evenly across neighborhoods. These data might suggest that poor-quality hospitals are located in areas with high residential segregation and therefore more likely to be accessed by black patients. While that may be partly true, other studies have shown that even when black patients live in close proximity to a high-quality hospital, they are more likely to bypass such a hospital in preference for a higher mortality hospital that may be at a farther distance [43]. Dimick et al. [44••] found similar results for patients undergoing CABG. While black patients were twice as likely to reside within 5 miles of a high-quality hospital (45 vs. 26 %), they were 25 % more likely than whites to receive care at a high-mortality, low-quality hospital, which was located further away from a high-quality hospital. For areas with high residential segregation blacks were 48 % more likely than whites to undergo CABG at low-quality hospitals. This may reflect differences in referral patterns for different racial groups. Culture and patient preferences may also intensify choice of hospitals, especially in segregated areas. It is likely that cultural concordance is an important factor for black patients and may play an important role in determining choice of hospitals [45, 46].
Second, physician referral patterns may also impact hospital and physician selection. Black patients are more likely to be treated by black physicians [47, 48] who, in turn, are more likely to practice in hospitals with a tradition of caring for black patients [49, 50]. Whether this pattern is by choice or due to limited access is unclear. The primary care physician treating black patients also report difficulties in referring patient to high-quality specialist providers and secure non-emergent patient admissions [50]. Black patients also are more likely to undergo cardiac surgery by surgeons with poorer reported outcomes or risk-adjusted operative mortality [51, 52]. Black patients are also likely to receive poorer periprocedural care, with 80 % of black patients receiving their primary care from approximately one fourth of the physicians, who were also more likely to be less qualified and had lower access to necessary technology [50].
Finally, hospitals that predominantly serve black and minority appear to be resource poor and therefore limited in engaging quality improvement efforts. For example, Jha et al. [53] demonstrated that hospitals caring for the majority of black patients had higher AMI mortality and significantly lower nursing to patient ratios compared to other hospitals. Popescu et al. [43] demonstrated that black Medicare enrollees are more likely to be admitted to safety net hospitals, which typically serve large numbers of uninsured or underinsured patients. Lack of resources may compromise a hospitals’ ability to engage in quality improvement efforts.
Reducing Disparities in Outcomes
Three decades of research have consistently demonstrated racial differences in cardiac surgery outcomes, but dedicated investigations into amelioration of these disparities have been lacking [54–57]. Consequently, these disparities have persisted over time [58, 14••]. The task of improving disparities in outcomes is an uphill but important one. Reducing racial disparities will require a multifaceted approach. In order to ensure that clinical outcomes are not dependent on the color of one’s skin, we need to ensure that all patients have access to the same high-quality care and that healthcare is consistent and standardized across hospitals.
First, efforts at eliminating poverty, improving literacy, and improving employment opportunities, with goal of broad social upliftment of disadvantaged social minorities, need to be at the heart of this change [54]. Second, it is essential to ensure that interaction of patients with the healthcare system is easy and seamless that removes barriers from accessing high-quality care. Culturally sensitive and locally appropriate community level interventions like the use of care navigators/coordinators are promising [59]. Efforts at improving earlier detection before disease becomes advanced, improvement in perioperative care with focus on managing risk factors and comorbidities, and avoiding complications could also have a significant impact on outcomes in this group [60]. Improvement in patient-provider communication and close provider follow-up could also help improve issues related to provider mistrust [34].
Concentrating quality improvement efforts at hospitals where a majority of racial minorities seek care could have a major impact on reducing racial disparities in healthcare especially given the concentration of black and minority patients at relatively fewer hospitals. This would require a concerted effort at understanding the specific organizational (e.g., surgeons, physicians, nurses), cultural (e.g., problem solving, innovation), and leadership (e.g., senior management) issues that may be related to poor performance at such hospitals. Developing a better understanding of the specific issues faced by such hospitals would be the key to designing targeted quality improvement programs at such hospitals. In the 1990s, the Northern New England Cardiovascular Disease Study Group used a combination of data feedback, continuous quality improvement, and cross-visit by surgeons, anesthesiologists, and nurses within a consortium of hospitals which led to a dramatic 20 % improvement in CABG mortality [61]. Similar exchange between high-mortality hospitals that disproportionately serve racial and ethnic minorities with nearby lower-mortality hospitals could stimulate quality improvement through an observation of their processes. In a recently study, Siegel et al. [62] describe a consortium of 10 high-volume hospitals serving a largely minority populations which underwent a systematic process of quality improvement, consisting of evidence-based order sets for AMI care, training and implementation of interdisciplinary care teams for overseeing patient outcomes, regular reporting and quarterly internal assessment of hospital quality measures, and external regulatory group performing intermittent site visits. In 2 years, between 2005 and 2007, these measures were associated with significant improvement in compliance with evidence-based AMI care among racial minorities in 7 out of 10 hospitals and the complete elimination of racial differences in three.
It is important to note that the provision of hospital care to ethnic minorities in the USA is highly concentrated, meaning that large gains in racial disparities may be made by targeting improvements to a relatively small number of hospitals. Jha et al. [53] demonstrated that more than 40 % of elderly black Medicare beneficiaries hospitalized during 2004 were concentrated in just 5 % of the nearly 4500 hospitals in the USA. The Centers for Medicare and Medicaid services (CMS) recently initiated hospital incentives for good outcomes under the pay-for-performance (P4P) program [63, 64]. Although some improvement has been noted in outpatient care for Blacks and Hispanics [65], it is unclear if the implementation of P4P has led to improvement in overall measures of hospital quality and a reduction in racial disparities, for which further research is warranted [66].
Another avenue for quality improvement in surgical care for minorities would include selective regionalization of high-risk procedures, like cardiac surgery, which could improve patient outcomes by ensuring that patients undergo cardiac surgery by high-volume surgeons at high-volume centers [67, 68]. However, such an approach could have unintended consequences by worsening geographic access and choice [69], and therefore more empirical data are needed.
Health Policy
Key health policy reforms have been undertaken by several states to improve the quality of health services available to the socially disadvantaged classes [70]. First, several states, like Alabama, Texas, and New York, have implemented loan repayment schemes for medical professionals providing services in medically underserved areas in order to improve the doctor-to-patient ratios in these communities. Second, scholarship programs have been established to bolster the training of physicians from socially disadvantaged backgrounds in order to generate a workforce adept at dealing with challenges unique to these communities. Third, several programs have been initiated for the sensitization of the medical community regarding racial differences in healthcare practices and cultural competency. These initiatives are promising but the actual impact of these measures on reducing healthcare disparities remains to be studied.
Conclusion
Although significant improvement in cardiac surgical outcomes has occurred in recent years, racial disparities in outcomes have largely remained unchanged. A major determinant of higher mortality in blacks and ethnic minorities undergoing cardiac surgery is their over-representation at low-quality hospitals. Concentrating quality improvement efforts at hospitals that disproportionately serve racial and ethnic minorities could go a long way in reducing racial disparities in cardiac surgical outcomes.
Abbreviations
- CABG
Coronary artery bypass graft
- AMI
Acute myocardial infarction
- CMS
Centers for Medicare & Medicaid Services
- P4P
Pay-for-performance
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest Rohan Khera, Mary Vaughan-Sarrazin, Gary E. Rosenthal, and Saket Girotra declare that they have no conflict of interest.
Contributor Information
Rohan Khera, Email: rohan-khera@uiowa.edu, Department of Internal Medicine, University of Iowa Hospitals & Clinics, 200 Hawkins Drive, E325 GH, Iowa City, IA 52242, USA.
Mary Vaughan-Sarrazin, Department of Internal Medicine, University of Iowa Hospitals & Clinics, 200 Hawkins Drive, E325 GH, Iowa City, IA 52242, USA; Center for Comprehensive Access and Delivery Research and Evaluation, Iowa City Veterans Affairs Medical Center, Iowa City, IA, USA; Institute of Clinical and Translational Science (ICTS), University of Iowa Carver College of Medicine, Iowa City, IA, USA.
Gary E. Rosenthal, Institute of Clinical and Translational Science (ICTS), University of Iowa Carver College of Medicine, Iowa City, IA, USA Division of General Internal Medicine, Department of Internal Medicine, University of Iowa Carver College of Medicine, Iowa City, IA, USA.
Saket Girotra, Institute of Clinical and Translational Science (ICTS), University of Iowa Carver College of Medicine, Iowa City, IA, USA; Division of Cardiovascular Medicine, Department of Internal Medicine, University of Iowa Carver College of Medicine, Iowa City, IA, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Centers for Disease Control and Prevention. FastStats - Inpatient surgery. [accessed October 4, 2014]; http://www.cdc.gov/nchs/fastats/inpatient-surgery.htm.
- 2.Mehta NJ, Khan IA. Cardiology’s 10 greatest discoveries of the 20th century. Texas Heart Inst J Texas Heart Inst St Luke’s Episcopal Hosp Texas Child Hosp. 2002;29(3):164–171. [PMC free article] [PubMed] [Google Scholar]
- 3.Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA: J Am Med Assoc. 2011;305(17):1769–1776. doi: 10.1001/jama.2011.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elixhauser A, Andrews RM. Profile of inpatient operating room procedures in US hospitals in 2007. Arch Surg. 2010;145(12):1201–1208. doi: 10.1001/archsurg.2010.269. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson TB., Jr Mortality in coronary artery bypass grafting: what’s next? Circulation. 2012;125(20):2409–2411. doi: 10.1161/CIRCULATIONAHA.112.106856. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson TB, Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL Committee STSND. A decade of change–risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990–1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Soc Thorac Surg Ann Thorac Surg. 2002;73(2):480–489. doi: 10.1016/s0003-4975(01)03339-2. discussion 9–90. [DOI] [PubMed] [Google Scholar]
- 7.ElBardissi AW, Aranki SF, Sheng S, O’Brien SM, Greenberg CC, Gammie JS. Trends in isolated coronary artery bypass grafting: an analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg. 2012;143(2):273–281. doi: 10.1016/j.jtcvs.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 8.Becker ER, Rahimi A. Disparities in race/ethnicity and gender in in-hospital mortality rates for coronary artery bypass surgery patients. J Natl Med Assoc. 2006;98(11):1729–1739. [PMC free article] [PubMed] [Google Scholar]
- 9. Konety SH, Vaughan Sarrazin MS, Rosenthal GE. Patient and hospital differences underlying racial variation in outcomes after coronary artery bypass graft surgery. Circulation. 2005;111(10):1210–1216. doi: 10.1161/01.CIR.0000157728.49918.9F. This study found that black patients undergoing CABG have higher mortality at both early (30-day) and late (90-day and 1-year) follow-up, compared to white patients.
- 10.Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667–669. doi: 10.1111/j.1525-1497.2006.0512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Project Hope) 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 12.Kaul P, Lytle BL, Spertus JA, DeLong ER, Peterson ED. Influence of racial disparities in procedure use on functional status outcomes among patients with coronary artery disease. Circulation. 2005;111(10):1284–1290. doi: 10.1161/01.CIR.0000157731.66268.E1. [DOI] [PubMed] [Google Scholar]
- 13.Holmes JS, Arispe IE, Moy E. Heart disease and prevention: race and age differences in heart disease prevention, treatment, and mortality. Med Care. 2005;43(3 Suppl):I33–I41. [PubMed] [Google Scholar]
- 14. Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg. 2014;149(3):223–227. doi: 10.1001/jamasurg.2013.4041. This study found that 34% of the excess CABG mortality in black Medicare beneficiaries was attributable to care at a low-quality hospital.
- 15.Rumsfeld JS, Plomondon ME, Peterson ED, Shlipak MG, Maynard C, Grunwald GK, et al. The impact of ethnicity on outcomes following coronary artery bypass graft surgery in the Veterans Health Administration. J Am Coll Cardiol. 2002;40(10):1786–1793. doi: 10.1016/s0735-1097(02)02485-3. [DOI] [PubMed] [Google Scholar]
- 16.Gray RJ, Nessim S, Khan SS, Denton T, Matloff JM. Adverse 5-year outcome after coronary artery bypass surgery in blacks. Arch Intern Med. 1996;156(7):769–773. [PubMed] [Google Scholar]
- 17.Flattery MP, Baker KM. Evidence for racial disparity in cardiac transplantation survival rates. J Cult Divers. 2004;11(1):25–30. [PubMed] [Google Scholar]
- 18.Stewart D, Johnson W, Saunders E. Hypertension in black Americans as a special population: why so special? Current Cardiol Rep. 2006;8(6):405–410. doi: 10.1007/s11886-006-0097-8. [DOI] [PubMed] [Google Scholar]
- 19.Horikawa Y, Oda N, Cox NJ, Li X, Orho-Melander M, Hara M, et al. Genetic variation in the gene encoding calpain-10 is associated with type 2 diabetes mellitus. Nat Genet. 2000;26(2):163–175. doi: 10.1038/79876. [DOI] [PubMed] [Google Scholar]
- 20.Ito K, Bick AG, Flannick J, Friedman DJ, Genovese G, Parfenov MG, et al. Increased burden of cardiovascular disease in carriers of APOL1 genetic variants. Circ Res. 2014;114(5):845–850. doi: 10.1161/CIRCRESAHA.114.302347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krauss RM, Mangravite LM, Smith JD, Medina MW, Wang D, Guo X, et al. Variation in the 3-hydroxyl-3-methylglutaryl coenzyme a reductase gene is associated with racial differences in low-density lipoprotein cholesterol response to simvastatin treatment. Circulation. 2008;117(12):1537–1544. doi: 10.1161/CIRCULATIONAHA.107.708388. [DOI] [PubMed] [Google Scholar]
- 22.Burroughs VJ, Maxey RW, Levy RA. Racial and ethnic differences in response to medicines: towards individualized pharmaceutical treatment. J Natl Med Assoc. 2002;94(10 Suppl):1–26. [PMC free article] [PubMed] [Google Scholar]
- 23.Ergul A, Tackett RL, Puett D. Distribution of endothelin receptors in saphenous veins of African Americans: implications of racial differences. J Cardiovasc Pharmacol. 1999;34(3):327–332. doi: 10.1097/00005344-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Royal CD, Dunston GM. Changing the paradigm from ‘race’ to human genome variation. Nat Genet. 2004;36(11 Suppl):S5–S7. doi: 10.1038/ng1454. [DOI] [PubMed] [Google Scholar]
- 25.Bamshad M, Wooding S, Salisbury BA, Stephens JC. Deconstructing the relationship between genetics and race. Nat Rev Genet. 2004;5(8):598–609. doi: 10.1038/nrg1401. [DOI] [PubMed] [Google Scholar]
- 26.Pearce N, Foliaki S, Sporle A, Cunningham C. Genetics, race, ethnicity, and health. BMJ. 2004;328(7447):1070–1072. doi: 10.1136/bmj.328.7447.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Braun L. Race, ethnicity, and health: can genetics explain disparities? Perspect Biol Med. 2002;45(2):159–174. doi: 10.1353/pbm.2002.0023. [DOI] [PubMed] [Google Scholar]
- 28.Jones RG, Trivedi AN, Ayanian JZ. Factors influencing the effectiveness of interventions to reduce racial and ethnic disparities in health care. Soc Sci Med. 2010;70(3):337–341. doi: 10.1016/j.socscimed.2009.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fredericks S, Lo J, Ibrahim S, Leung J. An examination of the difference in performance of self-care behaviours between white and non-white patients following CABG surgery: a secondary analysis. Can J Cardiovasc Nurs=J Can Soins Infirmiers Cardio-Vasculaires. 2010;20(4):21–29. [PubMed] [Google Scholar]
- 30.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Review: MCRR. 2000;57(Suppl 1):108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 31.Hines PM, Boyd-Franklin N. African American families. Ethn Fam Ther. 2005;3:87–100. [Google Scholar]
- 32.DeNavas-Walt C. Income, Poverty, and Health Insurance Coverage in the United States (2005) DIANE Publishing. 2010 [Google Scholar]
- 33.Popescu I, Nallamothu BK, Vaughan-Sarrazin MS, Cram P. Racial differences in admissions to high-quality hospitals for coronary heart disease. Arch Intern Med. 2010;170(14):1209–1215. doi: 10.1001/archinternmed.2010.227. [DOI] [PubMed] [Google Scholar]
- 34.Gordon HS, Pugach O, Berbaum ML, Ford ME. Examining patients’ trust in physicians and the VA healthcare system in a prospective cohort followed for six-months after an exacerbation of heart failure. Patient Educ Couns. 2014 doi: 10.1016/j.pec.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 35.Kressin NR, Clark JA, Whittle J, East M, Peterson ED, Chang BH, et al. Racial differences in health-related beliefs, attitudes, and experiences of VA cardiac patients: scale development and application. Med Care. 2002;40(1 Suppl):I72–I85. doi: 10.1097/00005650-200201001-00009. [DOI] [PubMed] [Google Scholar]
- 36.Yeung M, Kerrigan J, Sodhi S, Huang PH, Novak E, Maniar H, et al. Racial differences in rates of aortic valve replacement in patients with severe aortic stenosis. Am J Cardiol. 2013;112(7):991–995. doi: 10.1016/j.amjcard.2013.05.030. [DOI] [PubMed] [Google Scholar]
- 37.Gordon HS, Paterniti DA, Wray NP. Race and patient refusal of invasive cardiac procedures. J Gen Intern Med. 2004;19(9):962–966. doi: 10.1111/j.1525-1497.2004.30131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lucas FL, Stukel TA, Morris AM, Siewers AE, Birkmeyer JD. Race and surgical mortality in the United States. Ann Surg. 2006;243(2):281–286. doi: 10.1097/01.sla.0000197560.92456.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries: 1989–2000. Med Care. 2005;43(4):320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- 40.Liu JH, Zingmond DS, McGory ML, SooHoo NF, Ettner SL, Brook RH, et al. Disparities in the utilization of high-volume hospitals for complex surgery. JAMA: J Am Med Assoc. 2006;296(16):1973–1980. doi: 10.1001/jama.296.16.1973. [DOI] [PubMed] [Google Scholar]
- 41.Smith DB. Addressing racial inequities in health care: civil rights monitoring and report cards. J Health Polit Policy Law. 1998;23(1):75–105. doi: 10.1215/03616878-23-1-75. [DOI] [PubMed] [Google Scholar]
- 42. Sarrazin MV, Campbell M, Rosenthal GE. Racial differences in hospital use after acute myocardial infarction: does residential segregation play a role? Health Aff (Project Hope) 2009;28(2):w368–w378. doi: 10.1377/hlthaff.28.2.w368. This study found that in areas with higher residential segregation among racial groups, black patients were more likely to receive care for acute myocardial infarction at low-quality hospitals.
- 43.Popescu I, Cram P, Vaughan-Sarrazin MS. Differences in admitting hospital characteristics for black and white Medicare beneficiaries with acute myocardial infarction. Circulation. 2011;123(23):2710–2716. doi: 10.1161/CIRCULATIONAHA.110.973628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dimick J, Ruhter J, Sarrazin MV, Birkmeyer JD. Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Project Hope) 2013;32(6):1046–1053. doi: 10.1377/hlthaff.2011.1365. This study found that black patients were more likely to reside closer to a high quality hospital with low CABG mortality, but were more likely to undergo CABG at a farther high-mortality, low-quality hospital.
- 45.Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 46.Johnson RL, Saha S, Arbelaez JJ, Beach MC, Cooper LA. Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. J Gen Intern Med. 2004;19(2):101–110. doi: 10.1111/j.1525-1497.2004.30262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Aff (Project Hope) 2000;19(4):76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- 48.Komaromy M, Grumbach K, Drake M, Vranizan K, Lurie N, Keane D, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996;334(20):1305–1310. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 49.Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. [PubMed] [Google Scholar]
- 50.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 51.Mukamel DB, Weimer DL, Buchmueller TC, Ladd H, Mushlin AI. Changes in racial disparities in access to coronary artery bypass grafting surgery between the late 1990s and early 2000s. Med Care. 2007;45(7):664–671. doi: 10.1097/MLR.0b013e3180325b81. [DOI] [PubMed] [Google Scholar]
- 52.Mukamel DB, Weimer DL, Mushlin AI. Referrals to high-quality cardiac surgeons: patients’ race and characteristics of their physicians. Health Serv Res. 2006;41(4 Pt 1):1276–1295. doi: 10.1111/j.1475-6773.2006.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167(11):1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 54.Chan PS. The gap in current disparities research: a lesson from the community. Circ Cardiovasc Qual Outcome. 2014 doi: 10.1161/CIRCOUTCOMES.114.001234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jha AK, Zaslavsky AM. Quality reporting that addresses disparities in health care. JAMA: J Am Med Assoc. 2014;312(3):225–226. doi: 10.1001/jama.2014.7204. [DOI] [PubMed] [Google Scholar]
- 56.Wimmer NJ, Spertus JA, Kennedy KF, Anderson HV, Curtis JP, Weintraub WS, et al. Clinical prediction model suitable for assessing hospital quality for patients undergoing carotid endarterectomy. J Am Heart Assoc. 2014;3(3):e000728. doi: 10.1161/JAHA.113.000728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lurie N. Health disparities—less talk, more action. N Engl J Med. 2005;353(7):727–729. doi: 10.1056/NEJMe058143. [DOI] [PubMed] [Google Scholar]
- 58.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 59.Fouad M, Wynn T, Martin M, Partridge E. Patient navigation pilot project: results from the Community Health Advisors in Action Program (CHAAP) Ethn Dis. 2010;20(2):155–161. [PubMed] [Google Scholar]
- 60.Esnaola NF, Hall BL, Hosokawa PW, Ayanian JZ, Henderson WG, Khuri SF, et al. Race and surgical outcomes: it is not all black and white. Ann Surg. 2008;248(4):647–655. doi: 10.1097/SLA.0b013e31818a159a. [DOI] [PubMed] [Google Scholar]
- 61.O’Connor GT, Plume SK, Olmstead EM, Morton JR, Maloney CT, Nugent WC, et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. North N Engl Cardiovasc Dis Study Group JAMA: J Am Med Assoc. 1996;275(11):841–846. [PubMed] [Google Scholar]
- 62.Siegel B, Sears V, Bretsch JK, Wilson M, Jones KC, Mead H, et al. A quality improvement framework for equity in cardiovascular care: results of a national collaborative. J Healthcare Qual: Off Publ Ntnl Assoc Healthcare Qual. 2012;34(2):32–42. doi: 10.1111/j.1945-1474.2011.00196.x. quiz –3. [DOI] [PubMed] [Google Scholar]
- 63.Epstein AM. Paying for performance in the United States and abroad. N Engl J Med. 2006;355(4):406–408. doi: 10.1056/NEJMe068131. [DOI] [PubMed] [Google Scholar]
- 64.Stulberg J. The physician quality reporting initiative–a gateway to pay for performance: what every health care professional should know. Qual Manag Health Care. 2008;17(1):2–8. doi: 10.1097/01.QMH.0000308632.74355.93. [DOI] [PubMed] [Google Scholar]
- 65.Bhalla R, Schechter CB, Strelnick AH, Deb N, Meissner P, Currie BP. Pay for performance improves quality across demographic groups. Qual Manag Health Care. 2013;22(3):199–209. doi: 10.1097/QMH.0b013e31829a6b4f. [DOI] [PubMed] [Google Scholar]
- 66.Ryan A, Sutton M, Doran T. Does winning a pay-for-performance bonus improve subsequent quality performance? Evidence from the Hospital Quality Incentive Demonstration. Health Serv Res. 2014;49(2):568–587. doi: 10.1111/1475-6773.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nallamothu BK, Saint S, Ramsey SD, Hofer TP, Vijan S, Eagle KA. The role of hospital volume in coronary artery bypass grafting: is more always better? J Am Coll Cardiol. 2001;38(7):1923–1930. doi: 10.1016/s0735-1097(01)01647-3. [DOI] [PubMed] [Google Scholar]
- 68.Grumbach K, Anderson GM, Luft HS, Roos LL, Brook R. Regionalization of cardiac surgery in the United States and Canada. Geographic access, choice, and outcomes. JAMA: J Am Med Assoc. 1995;274(16):1282–1288. [PubMed] [Google Scholar]
- 69.Mirvis DM, Graney MJ. Impact of race and age on the effects of regionalization of cardiac procedures in the Department of Veterans Affairs Health Care System. Am J Cardiol. 1998;81(8):982–987. doi: 10.1016/s0002-9149(98)00076-9. [DOI] [PubMed] [Google Scholar]
- 70.National Conference of State Legislatures. [Accessed November 15 2014];Health Disparities: State Laws. 2014 http://www.ncsl.org/research/health/health-disparities-laws.aspx. [Google Scholar]