Abstract
Background
Use of waterpipe tobacco smoking (WTS) is now prevalent among U.S. adolescents. However, the more clinically relevant questions are whether users exhibit sustained patterns of use and whether use is increasing over time relative to other tobacco products. We aimed to examine factors associated with sustained WTS among U.S. adolescents and to compare prevalence trends between WTS and other tobacco products.
Methods
The Monitoring the Future (MTF) project began assessing WTS among 12th grade students in 2010. In 2014, we conducted multivariable regression analyses to examine correlates of sustained WTS, which we defined as use at least 6 times in the past 12 months. We used trend analysis to compare use of WTS and other types of tobacco.
Results
Of the 8737 participants queried from 2010-2013, 18.8% (1639) reported past-year WTS, while 7.2% (627) reported sustained use. Sustained WTS was inversely associated with female sex (vs. males, OR=0.78, 95% CI=0.63, 0.96), African-American race (vs. Caucasians, OR=0.26, 95% CI=0.14, 0.48), and increased number of parents in the home (P<0.001). Sustained WTS was positively associated with increased school-level parental education (P<.002), lower grades (P=.005), truancy (P<.001), lower religiosity (P<.001), evenings out per week (P<.001), and dating (P<.03). Visual inspection and non-overlapping confidence intervals suggest that both past-year and sustained WTS are significantly increasing relative to cigarette use but not small cigar use.
Conclusions
Given the prevalence of sustained WTS and indications of its increase over time, it should be included in efforts related to tobacco surveillance and intervention.
Keywords: hookah, waterpipe, tobacco, smoking, youth
Introduction
Smoking tobacco with a waterpipe (also known as a hookah or narghile) is an emerging trend.1–3 Many smokers perceive the potential harm from waterpipe tobacco smoking (WTS) to be low.4–6 Compared with a single cigarette, however, one waterpipe session— which typically occurs over approximately 45-60 minutes7,8—can expose the user to substantially greater amounts of key toxicants, including tar, nicotine, carbon monoxide, and polycyclic aromatic hydrocarbons.7,9–12 These findings are consistent with preliminary reports that associate WTS with cancer, cardiovascular disease, decreased pulmonary function, and nicotine dependence.13,14
Past research suggests that, among U.S. college students, the prevalence of WTS is about 20%-40% ever and 5-15% in the past 30 days.1,15–18 Studies of high school students report lifetime WTS prevalence rates of as much as 15-17% by the senior year of high school.15,17,19,20 A recent study of high school seniors found an 18% WTS prevalence rate and identified certain key socio-demographic and lifestyle correlates associated with past-year WTS, including sex, race, parental education level, and use of other substances.21
However, sustained WTS has been less frequently examined. Concern about adverse health effects and addiction have often been minimized due to the assumption that use is generally intermittent or experimental.22 While some users report more frequent use, suggesting an extension beyond experimentation,23,24 it is not clear to what extent sustained use is exhibited in nationally-representative samples. Heavier users are potentially exposed to a greater volume of toxicants and are more likely to report being dependent on WTS and more resistant to quitting.25,26
Another important unanswered question is whether use over time is changing relative to other forms of tobacco use. While some indications are that use may be increasing,3,20 many organizations are resistant to invest in long-term surveillance. For example, the 2015 Youth Risk Behavior Surveillance Survey for U.S. high school students asks about smokeless tobacco, cigars, and electronic cigarettes, but it does not assess WTS.27
Monitoring the Future (MTF), which uses a weighted multistage random sampling procedure to ensure that results are nationally representative, began assessing WTS among 12th grade students in 2010.28 Data are currently available through 2013. We first aimed to leverage this source of data to assess sustained WTS, including determination of independent associations between various socio-demographic and lifestyle factors and sustained WTS. Second, we aimed to compare prevalence trends for WTS with prevalence trends for other tobacco products during the study period.
Methods
Participants and Procedures
A detailed description of the University of Michigan's MTF study is available elsewhere.29 In brief, MTF uses a multi-stage sampling procedure to obtain nationally representative samples of students attending public and private schools in the 48 contiguous states. Sample weights are assigned to each student to account for differential probabilities of selection. The present study examines data from 12th graders only, because WTS was not asked of 8th and 10th graders. We combined data from 2010-2013 to include all available data (N=8737). Students completed self-administered, machine-readable questionnaires during a normal class period. Response rates averaged 83%.29 Absence on the day of data collection was the primary reason that students were missed; it is estimated that less than 1% of students declined to complete the questionnaire.29 The study received approval from the University of Michigan IRB (HUM00063656).
Measures
The WTS question in the MTF survey reads: “During the last 12 months, on how many occasions (if any) have you smoked tobacco using a hookah (water pipe)?” with response categories 0, 1-2, 3-5, 6-9, 10-19, 20-39, 40+. For this study, the main outcome variable of sustained use was defined as use on at least 6 occasions in the last 12 months. This cutoff was selected a priori for two reasons. First, use at least every other month seems to indicate a sustained pattern beyond isolated or experimental use which might be due to a particular event such as Spring Break or a holiday party.1,16,30 Second, because available data indicate that a single WTS session delivers the tar of about 40 cigarettes,31–33 use on six occasions over the past year would indicate tar inhalation approximating 12 packs of cigarettes—at least 1 per month on average—which represents concerning and sustained exposure. We assessed cigarette use by asking, “How frequently have you smoked cigarettes during the past 30 days?” with a responses ranging from “not at all” to “two packs or more per day.” Current (past 30-day) cigarette use was defined as no if “not at all” was selected and as yes if any other choice was selected. Small cigar use was assessed with an item similar to WTS (past-year use) and was categorized the same as cigarette use (“not in the past year” versus all others).
Socio-demographic variables of interest included sex, race/ethnicity, number of parents in the home, parental education level, school socioeconomic status (SES), population density, and region of the U.S.
Race and ethnicity were assessed per MTF protocol. The item asked “How do you describe yourself?” and allowed participants to choose as many as they wished from 9 different options. These responses were subsequently collapsed into four mutually-exclusive categories: Caucasian, African-American, Hispanic, or Other. Details on categories and coding are provided in Table 1. Those who did not select any check-boxes were considered missing. Parental education, also assessed using MTF protocol, was based on an 11-point scale created from an average of the mother and father's data and divided into quintiles. To determine school SES, the average parental education level for each school was collapsed into quartiles. Population density was based on United States Census Metropolitan Statistical Areas (MSAs).
Table 1. Associations between Participant Characteristics and Waterpipe Tobacco Smoking.
| Characteristics | All | Any WTS (a) | Sustained WTS (a) | Adjusted Odds Ratio (95% Confidence Interval) (c) | P (d) | ||
|---|---|---|---|---|---|---|---|
| N = 8737 | 1639 / 8737 = 18.8% | 627 / 8737 = 7.2% | |||||
| Column % | Row % | P (b) | Row % | P (b) | |||
| Socio-demographic Characteristics | |||||||
| Sex | .01 | <.001 | |||||
| Male | 49.6 | 20.1 | 8.5 | 1 | |||
| Female | 50.4 | 17.4 | 5.8 | 0.78 (0.63, 0.96) | |||
| Race/Ethnicity (d) | <.001 | <.001 | |||||
| Caucasian | 59.3 | 20.4 | 7.6 | 1 | |||
| African-American | 11.7 | 7.1 | 2.4 | 0.26 (0.14, 0.48) | |||
| Hispanic | 16.1 | 20.3 | 8.2 | 1.00 (0.66, 1.49) | |||
| Other | 13.0 | 19.3 | 7.9 | 1.06 (0.78, 1.44) | |||
| Number of Parents | .82 | .02 | <.001 | ||||
| 0 | 6.2 | 18.3 | 10.0 | 1 | |||
| 1 | 28.2 | 19.3 | 8.3 | 0.69 (0.42, 1.14) | |||
| 2 | 65.6 | 18.5 | 6.4 | 0.46 (0.30, 0.73) | |||
| Parents Education Level Index (e) | .62 | .61 | .44 | ||||
| 1 (Low) | 10.1 | 18.5 | 5.8 | 1 | |||
| 2 | 21.6 | 17.7 | 7.5 | 1.25 (0.72, 2.18) | |||
| 3 | 28.9 | 19.9 | 7.6 | 1.41 (0.80, 2.47) | |||
| 4 | 26.2 | 18.5 | 6.8 | 1.32 (0.74, 2.36) | |||
| 5 (High) | 13.2 | 19.9 | 7.2 | 1.44 (0.79, 2.64) | |||
| School SES (rank) | <.001 | .03 | .002 | ||||
| 1 (Low) | 28.3 | 15.2 | 5.6 | 1 | |||
| 2 | 23.2 | 16.2 | 5.9 | 1.30 (0.83, 2.04) | |||
| 3 | 24.4 | 21.8 | 9.0 | 1.69 (1.08, 2.65) | |||
| 4 (High) | 24.2 | 22.0 | 8.2 | 1.60 (1.06, 2.42) | |||
| Population density | <.001 | <.001 | |||||
| Large MSA | 30.9 | 21.4 | 7.6 | 1 | |||
| Non-MSA | 49.1 | 20.5 | 8.4 | 1.06 (0.78, 1.45) | |||
| Other MSA | 20.0 | 10.6 | 3.7 | 0.48 (0.32, 0.72) | |||
| US Region | <.001 | <.001 | |||||
| Northeast | 17.8 | 17.9 | 5.3 | 1 | |||
| North Central | 23.6 | 19.2 | 7.6 | 0.68 (0.42, 1.11) | |||
| South | 35.6 | 14.6 | 4.9 | 1.39 (0.92, 2.08) | |||
| West | 23.1 | 25.1 | 11.5 | 2.28 (1.41, 3.70) | |||
|
| |||||||
| Educational Characteristics | |||||||
| Grades | <.001 | <.001 | .005 | ||||
| A | 36.2 | 15.3 | 5.3 | 1 | |||
| B | 47.9 | 19.4 | 7.2 | 1.20 (0.91, 1.57) | |||
| C or below | 16.0 | 24.4 | 11.1 | 1.54 (1.10, 2.15) | |||
| Days cut school in the past month | <.001 | <.001 | <.001 | ||||
| Not at all | 69.0 | 13.9 | 4.9 | 1 | |||
| 1 or 2 times | 20.8 | 26.9 | 9.7 | 1.76 (1.37, 2.26) | |||
| 3 or more times | 10.3 | 37.1 | 17.6 | 2.48 (1.79, 3.43) | |||
| Plans to graduate from college | .046 | .006 | 0.66 | ||||
| Definitely won't | 7.8 | 17.8 | 8.7 | 1 | |||
| Probably won't | 9.3 | 21.1 | 9.1 | 1.04 (0.62, 1.72) | |||
| Probably will | 23.5 | 20.8 | 8.0 | 0.97 (0.65, 1.46) | |||
| Definitely will | 59.5 | 17.7 | 6.2 | 0.94 (0.64, 1.38) | |||
|
| |||||||
| Employment Characteristics | |||||||
| Hours per week in a job | <.001 | .001 | .63 | ||||
| None | 38.6 | 14.4 | 5.7 | 1 | |||
| 1-15 hrs | 32.5 | 20.1 | 7.2 | 0.93 (0.62, 1.40) | |||
| 16-30+ hrs | 28.9 | 23.4 | 9.1 | 1.04 (0.67, 1.63) | |||
| Weekly income from paid work | <.001 | <.001 | .09 | ||||
| None | 43.8 | 14.8 | 5.4 | 1 | |||
| $1-75 | 22.8 | 20.1 | 7.2 | 1.20 (0.82, 1.77) | |||
| $75+ | 33.4 | 23.4 | 9.6 | 1.46 (0.93, 2.27) | |||
|
| |||||||
| Other Characteristics | |||||||
| Religiosity | <.001 | <.001 | <.001 | ||||
| Not important | 19.3 | 23.9 | 9.6 | 1 | |||
| A little important | 20.6 | 20.6 | 6.7 | 0.70 (0.52, 0.95) | |||
| Pretty important | 22.4 | 18.1 | 6.9 | 0.83 (0.61, 1.13) | |||
| Very important | 24.5 | 10.8 | 3.7 | 0.50 (0.35, 0.71) | |||
| Excluded (g) | 13.2 | 24.8 | 11.3 | 0.70 (0.43, 1.13) | |||
| Evenings out per week | <.001 | <.001 | <.001 | ||||
| Less than one | 12.2 | 7.8 | 2.0 | 1 | |||
| One | 15.2 | 11.4 | 4.0 | 1.88 (0.98, 3.62) | |||
| Two | 26.0 | 15.8 | 5.0 | 2.18 (1.14, 4.19) | |||
| Three | 23.0 | 22.0 | 8.3 | 3.32 (1.75, 6.27) | |||
| Four or five | 15.4 | 26.8 | 10.9 | 4.64 (2.32, 9.28) | |||
| Six or seven | 8.2 | 34.7 | 17.6 | 7.15 (3.37, 15.17) | |||
| Dating | <.001 | <.001 | .03 | ||||
| Never | 32.0 | 11.7 | 4.5 | 1 | |||
| Once a month or less | 17.8 | 19.8 | 7.3 | 1.48 (1.04, 2.10) | |||
| 2 or 3 times a month | 15.7 | 20.6 | 7.1 | 1.26 (0.87, 1.82) | |||
| Once a week | 14.7 | 20.6 | 7.7 | 1.33 (0.89, 1.97) | |||
| 2 or 3 times a week | 13.7 | 25.4 | 10.2 | 1.61 (1.12, 2.30) | |||
| Over 3 times a week | 6.1 | 29.3 | 13.3 | 1.54 (0.96, 2.46) | |||
Abbreviations: WTS = Waterpipe Tobacco Smoking.
Sustained WTS was defined as use ≥ 6 times in the past 12 months.
Rao-Scott chi-square test adjusts for complex survey design.
Adjusted odds ratios are for sustained WTS and were computed using logistic regression.
Test for trend was computed only for ordered categorical variables.34
Items assessing race and ethnicity asked “How do you describe yourself?” and allowed participants to choose more than one from the following options: (1) Black or African American; (2) Mexican American or Chicano; (3) Cuban American; (4) Puerto Rican; (5) Other Hispanic or Latino; (6) Asian American; (7) White (Caucasian); (8) American Indian or Alaska Native; and (9) Native Hawaiian or Other Pacific Islander. These responses were subsequently collapsed into four mutually-exclusive categories. Participants marking only (7) were classified as Caucasian, those selecting only (1) were classified as African American, those selecting only (2), (3), (4), or (5) or any combination of these were categorized as Hispanic; and those who selected other categories or multiple categories were defined as Other. Those who did not select check-boxes were considered missing.
Based on an 11-point scale created from an average of the mother and father's data, divided into quintiles. Those with missing data were excluded from analysis.
California respondents excluded.
Lifestyle characteristics assessed included students' educational behaviors and aspirations, employment, religiosity and social activity, all of which have been shown to have preliminary associations with WTS.17,18,21,34 For grade point average, students responded to the item “Which of the following best describes your average grade so far in high school?” We collapsed data into three categories: A (90-100), B (80-89), or C or below. We assessed truancy by asking “During the LAST FOUR WEEKS, how many whole days of school have you missed because you skipped or ‘cut’?” To assess educational plans, we asked “How likely is it that you will graduate from college (four-year program) after high school?” followed by a 4-point Likert scale. Students also self-reported the number of hours per week in a job and their average weekly income from paid work. We assessed religiosity by asking students “How important is religion in your life?” followed by a 4-point Likert scale. Students were also asked “During a typical week, on how many evenings do you go out for fun and recreation?” and “On the average, how often do you go out with a date (or your spouse, if you are married)?” Response choices for all measures are noted in the tables.
Statistical Analysis
We used descriptive statistics to examine respondent characteristics and to determine the prevalence of past-year and sustained WTS. Because all covariates were categorical, we used 2-way chi-square tests to assess bivariable associations between covariates and WTS outcomes. To assess multivariable associations, we used logistic regression analyses for the primary outcome variable of sustained WTS. We used an established method for assessing overall linear trend for ordered categorical independent variables.35 All analyses were adjusted to account for the complex sample design, including clustering of individuals within schools and integrating survey weights. Because only 2.9% of those in the sample had any missing covariate data, we used list-wise deletion instead of imputation for multivariable analyses. Because there was no effect of year in diagnostic bivariable and multivariable logistic regression analyses, we grouped all years together for all primary analyses.
We compared trends over time (2010-2013) by visual inspection. However, we also used linear regression to calculate slope estimates and 95% confidence intervals for each tobacco type over the four years. We then examined overlap between the 95% confidence intervals of these slope estimates for each WTS trend (any 12-month use and 12-month sustained use) and each other tobacco use trend (30-day cigarette use and 12-month cigar or small cigar use).36–38 We performed statistical analyses with SAS version 9.3,39 and two-tailed P values <.05 were considered significant.
Results
The 8737 respondents were 50.4% female, 59.3% Caucasian, 11.7% African-American, and 16.1% Hispanic. About two-thirds (65.6%) of the sample reported having two parents in the home. While about one-third of respondents originated from the southern U.S. (35.6%), other U.S. regions were roughly equally represented (Table 1).
Weighted results demonstrated WTS prevalence of 18.8% over the past 12 months. About one in 14 (7.2%) of participants reported 6 or more WTS sessions in the past 12 months, indicating sustained use. Thus, 38% of past-year WTS users were sustained users. The complete distribution of this variable is in Table 2. About one-fifth (20.7%) of respondents reported smoking small cigars (also called “cigarillos” or “blunts”) in the past 12 months, and 17.8% reported smoking cigarettes in the past 30 days. Both small cigar use (in the past 12 months) and cigarette use (in the past 30 days) were significantly associated with WTS use in the past 12 months (Figure 1). However, among past-year WTS users, 53.8% were not current users of cigarettes and about 38.1% had not used little cigars in the past year (Figure 1).
Table 2. Frequency of Waterpipe Tobacco Smoking by Study Year.
| Year | Number of Times Smoked Waterpipe Tobacco in the Past Year | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| 0 | 1-2 | 3-5 | 6-9 | 10-19 | 20-39 | 40+ | |
| 2010 | 82.9% | 6.5% | 4.1% | 2.3% | 1.8% | 1.2% | 1.2% |
| 2011 | 81.5% | 8.2% | 4.4% | 1.4% | 2.1% | 0.8% | 1.7% |
| 2012 | 81.7% | 6.9% | 4.0% | 2.7% | 1.8% | 0.8% | 2.2% |
| 2013 | 78.6% | 7.3% | 5.0% | 2.8% | 2.5% | 2.1% | 1.7% |
Figure 1. Prevalence of little cigar and cigarette smoking among those who had and had not smoked tobacco from a waterpipe.
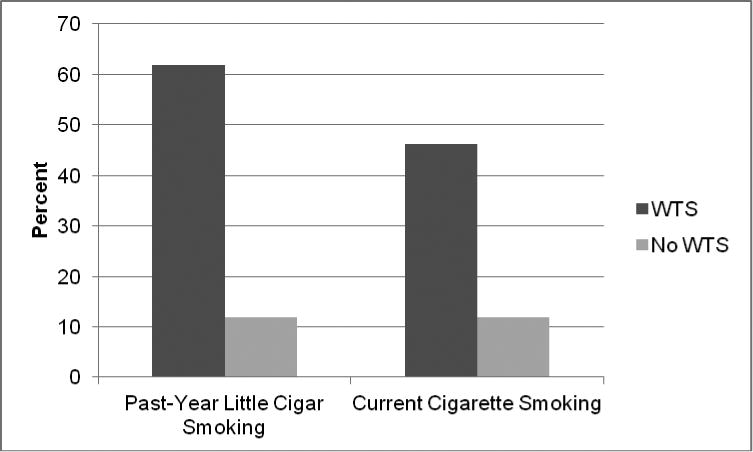
WTS indicates Waterpipe Tobacco Smoking. Dark vertical bars indicate the percentage of WTS users who also engaged in past-year little cigar smoking and past 30-day cigarette smoking, respectively. Light vertical bars indicate the percentage of non-WTS users who engaged in past-year little cigar smoking and past 30-day cigarette smoking. Monitoring the Future does not assess use of cigarettes in the past 12 months. Both comparisons were significant at the P<.001 level using X2 analyses.
Sustained WTS was higher among males than females (8.5% vs. 5.8%, P<.001). Additionally, while between 7.5% and 8.2% of Caucasians, Hispanics, and those who identified as “Other” race/ethnicity reported sustained WTS, only 2.4% of African-Americans reported this behavior (P<.001). Sustained WTS was highest in the West (11.5%) followed by the North Central, Northeast, and South (7.6%, 5.3%, and 4.9%, respectively). Other bivariable associations are presented in Table 1.
In the multivarable model that controlled for all covariates (Table 1), compared to males, females had a reduced odds of sustained WTS (OR=0.78, 95% CI=0.63, 0.96). Compared with Caucasian students, African-American students had lower odds of sustained WTS (OR=0.26, 95% CI=0.14, 0.48). Although participant's parents' educational level was not significantly associated with sustained WTS (P=.44) at the individual level, school level parent education was positively associated with sustained WTS (P=.002). Students with a greater number of parents in the house had a reduced odds of sustained WTS (P<.001). Compared with those who lived in a large MSA, those in other MSAs (the most rural areas) had lower odds of sustained WTS (OR=0.48, 95% CI=0.32, 0.72). Finally, compared with those in the Southern U.S., those in the Western U.S. had higher odds of sustained WTS (OR=2.28, 95% CI=1.41, 3.70). Multiple lifestyle factors, including lower grades (P=.005), increased truancy (P<.001), lower religiosity (P<.001), more evenings out per week (P<.001), and more dating (P=.03) were also independently associated with sustained WTS.
Visual inspection of point estimates over time suggests that sustained and past-year WTS are increasing while past-year small cigar use and past 30-days cigarette use are decreasing (Figure 2). Linear regression coefficients over the time period 2010-2013 were 0.08 for any past-year WTS (95% CI = -0.01, 0.17), 0.14 for sustained past-year WTS (95% CI = -0.0003, 0.27), -0.048 for past-year small cigar use (95% CI = -0.12, 0.03) and -0.070 for past 30-day cigarette smoking (95% CI = -0.12, -0.02). Therefore, confidence intervals did not overlap between past-year WTS (-0.01, 0.17) and cigarette smoking (-0.12, -0.02). Additionally, confidence intervals did not overlap between sustained WTS (-0.0003, 0.27) and cigarette smoking (-0.12, -0.02). However, both WTS outcomes did overlap with the small cigar outcome.
Figure 2. Trends in tobacco use from 2010-2013.
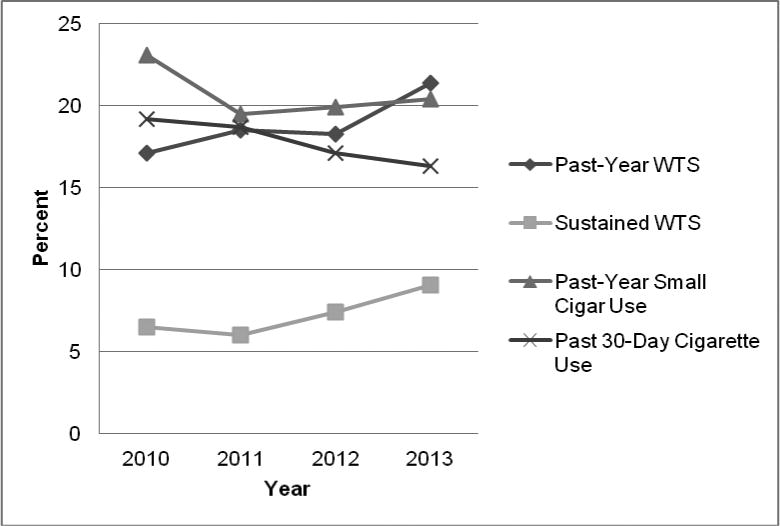
WTS indicates Waterpipe Tobacco Smoking. Sustained WTS indicates use 6 or more times in the past 12 months.
Discussion
Over the period 2010-2013, nearly one out of every five (18.8%) U.S. 12th graders used a waterpipe to smoke tobacco in the past-year, and 38% of those individuals did so at least 6 times in the past year. These findings are consistent with other studies of U.S. adolescents but lower than studies of adolescents from the Eastern Mediterranean Region, where WTS is more endemic.3,17 One common theme of prior WTS data has been that ever use tends to be substantially higher than frequent use, suggesting a high level of experimentation but a lower level of sustained use.18,40,41 However, these findings suggest that over a third of past-year users exhibit a more sustained pattern equating to a high toxicant load. For example, because one WTS session, which can last up to 45-60 minutes,7,8 is associated with about 40 times the tar inhaled from a single cigarette,31–33 the current findings suggest that over 7% of U.S. high school seniors has inhaled the tar of 240 cigarettes, or 12 packs of cigarettes, in the past year from waterpipes. Therefore, WTS is common enough among U.S. youth to be included in future surveillance and prevention efforts. These findings also raise concern regarding dependence, because heavier users may be more likely to be dependent.26
As indicated in Figure 1, there is substantial overlap between WTS and other forms of inhaled tobacco use in this population. However, the amount of disjunction between the behaviors is also noteworthy. For example, of past-year WTS users, over half were not current users of cigarettes. This suggests that there is a large population of WTS-only smokers who represent an important target for prevention programming.
Although parental educational level was not significantly associated with WTS at the individual level, the average school-level educational attainment was significantly associated with sustained WTS, which was more prevalent in schools with higher proportions of more highly educated parents. While there are possible explanations for this phenomenon—such as possible increased availability of these products in wealthier neighborhoods—it deserves future study.
This study also found that sustained WTS was less prevalent among African-Americans but roughly comparable among other racial and ethnic groups. Because African-Americans are known to have higher prevalence of cigar and small cigar use,28 it is possible that their lower rate of WTS is due to a substitution effect. However, this issue may be valuable to explore in future qualitative work. Another issue worth considering is the meaning of the term Caucasian, which generally includes those of Middle Eastern ethnicity, who may be particularly at risk.42 Thus, it is possible that this subgroup may at least somewhat influence the association between Caucasian race and WTS.
Sustained WTS was generally associated with the western U.S. in fully-adjusted models (OR=2.28, 95% CI=1.41, 3.70). However, there was also relative consistency of prevalence throughout the U.S.—while sustained use was 11.5% in the West, it was still between 4.9% and 7.6% in the other regions. Thus, while ultimately there may be some benefit to focusing on the Western region, sustained use prevalence rates are relatively consistent across geography.
Sustained WTS was associated with poorer academic achievement, including lower grades and truancy. Other risk-taking behaviors—including other forms of tobacco use—have been associated with these factors.43–45 However, this is interesting in juxtaposition with the findings noted above that use was more prevalent in higher SES areas, which is not often the case for cigarette smoking. Therefore, WTS may represent a hybrid behavior for which some traditional associations apply while others do not. This may make intervention challenging.
Sustained WTS was more common among those with more active social and occupational lives, such as those spending more evenings out per week and dating. This is consistent with the perception of WTS as a highly social behavior, which has been described in both quantitative and qualitative studies.6,46–49
Over the period 2010-2013, as indicated visually in Figure 2, both past-year and sustained WTS prevalence seem to be trending upward. Because the WTS confidence intervals do not overlap with the confidence intervals for cigarette smoking, these data suggest that both WTS outcomes may be increasing relative to cigarette smoking. Additionally, visual inspection of these trends suggests that the rise in sustained WTS seems to be larger than the rise in overall WTS prevalence. While this is concerning because it may indicate transitions from occasional users to more frequent users over time, longitudinal analyses assessing the same individuals over time will be needed to confirm possible trends such as these.
Policy changes have driven much of the decrease in cigarette smoking over the past two decades.50,51 However, it has been noted that most extant policies do not adequately address WTS.8,52 Thus, one interpretation of possible increases in WTS compared with cigarette smoking is that policy measures aimed at reducing cigarette prevalence may have unintended consequences of a subsequent migration to WTS.53 Policy makers should consider these findings while modifying existing clean indoor legislation and other tobacco regulations. For example, while the newly-implemented Affordable Care Act allows insurers to charge cigarette smokers up to 50% higher premiums,54 this may not affect WT users.
Limitations
The MTF survey relied on self-report of waterpipe use without biochemical verification. Additionally, it is a necessary limitation of the data that at present MTF does not assess 30-day or lifetime WTS. It should also be noted that the definition of “sustained” used in this study was based on report of WTS 6 times in the preceding year, and not on lack of interruption of WTS. Finer-grained data will be needed for more detailed pattern analysis. Additionally, our time-trend analyses sought to compare linear trends and did not model changes using higher-order (i.e., quadratic or cubic) terms. When more data points are available, more complex modeling approaches may be useful. Finally, because of the breadth of the MTF instrument it was not able to accommodate in-depth assessments specific to WTS such as attitudes, normative beliefs, and expectancies.
Conclusions
This 4-year study of a nationally-representative sample of U.S. 12th graders demonstrates a substantial prevalence of WTS in terms of use at least 6 times in the past year, and that both past-12-month and sustained WTS seem to be increasing in comparison with cigarette smoking. These findings suggest that WTS should be included with other forms of tobacco in efforts related to surveillance and intervention. This study was also valuable in that it revealed important bivariable and multivariable relationships between sustained WTS and important socio-demographic and lifestyle factors which may help target interventions. However, analyses also revealed a relative consistency of WTS across multiple demographic factors. Thus, optimal intervention is likely to be challenging, because it will need to reach a large cohort of varied individuals.
Acknowledgments
We acknowledge our funding sources. The Monitoring the Future study is conducted at the University of Michigan and is supported by the National Institute on Drug Abuse (R01-DA001411). Dr. Primack and Dr. Sidani are supported by a grant from the National Cancer Institute (R01-CA140150).
Footnotes
Financial disclosure: The authors have no financial disclosures to report.
Conflict of Interest Statement: The Monitoring the Future study is conducted at the University of Michigan and is supported by the National Institute on Drug Abuse (R01-DA001411). Dr. Primack and Dr. Sidani are supported by a grant from the National Cancer Institute (R01-CA140150). These funding agencies had no role in study design; collection, analysis and interpretation of the data; writing the report; or the decision to submit the report for publication.
References
- 1.Primack BA, Shensa A, Kim KH, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36(1-2):1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martinasek MP, McDermott RJ, Martini L. Waterpipe (hookah) tobacco smoking among youth. Curr Probl Pediatr Adolesc Health Care. 2011;41:34–57. doi: 10.1016/j.cppeds.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Barnett TE, Shensa A, Kim KH, Cook RL, Nuzzo E, Primack BA. The predictive utility of attitudes toward hookah tobacco smoking on current use and use among a sample of college students. Am J Health Behav. 2013;37(4):433–439. doi: 10.5993/AJHB.37.4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nuzzo E, Shensa A, Kim KH, et al. Associations between hookah tobacco smoking knowledge and hookah smoking behavior among US college students. Health Educ Res. 2013;28(1):92–100. doi: 10.1093/her/cys095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakkash RT, Khalil J, Afifi RA. The rise in narghile (shisha, hookah) waterpipe tobacco smoking: A qualitative study of perceptions of smokers and non smokers. BMC Public Health. 2011;11:315. doi: 10.1186/1471-2458-11-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jacob P, Abu Raddaha AH, Dempsey D, et al. Comparison of nicotine and carcinogen exposure with water pipe and cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2013;22(5):765–772. doi: 10.1158/1055-9965.EPI-12-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffiths MA, Harmon TR, Gilly MC. Hubble Bubble Trouble: The Need for Education About and Regulation of Hookah Smoking. J Public Policy Mark. 2011;30(1):119–132. doi: 10.1509/jppm.30.1.119. [DOI] [Google Scholar]
- 9.Cobb CO, Shihadeh A, Weaver MF, Eissenberg TE. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2011;13(2):78–87. doi: 10.1093/ntr/ntq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maziak W, Rastam S, Shihadeh A, et al. Nicotine exposure in daily waterpipe smokers and its relation to puff topography. Addict Behav. 2011;36:397–399. doi: 10.1016/j.addbeh.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alzoubi KH, Khabour OF, Azab M, et al. CO exposure and puff topography are associated with Lebanese waterpipe dependence scale score. Nicotine Tob Res. 2013;15(10):1782–1786. doi: 10.1093/ntr/ntt049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sepetdjian E, Shihadeh A, Saliba NA, Monzer B. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food Chem Toxicol. 2008;46:1582–1590. doi: 10.1016/j.fct.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 13.Raad D, Gaddam S, Schunemann HJ, et al. Effects of waterpipe tobacco smoking on lung function: A systematic review and meta-analysis. Chest. 2011;139(4):764–774. doi: 10.1378/chest.10-0991. [DOI] [PubMed] [Google Scholar]
- 14.Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: A systematic review. Int J Epidemiol. 2010;39(3):834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 15.Sutfin EL, McCoy TP, Reboussin BA, Wagoner KG, Spangler J, Wolfson M. Prevalence and correlates of waterpipe tobacco use among college students in North Carolina. Drug Alcohol Depend. 2011;115(1-2):131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grant A, Morrison R, Dockrell MJ. The prevalence of waterpipe (shisha, narghile, hookah) use among adults in Great Britain, and factors associated with waterpipe use: Data from cross-sectional online surveys in 2012 and 2013. Nicotine Tob Res. 2014:1–8. doi: 10.1093/ntr/ntu015. [DOI] [PubMed] [Google Scholar]
- 17.Primack BA, Walsh M, Bryce C, Eissenberg TE. Water-pipe tobacco smoking among middle and high school students in Arizona. Pediatrics. 2009;123(2):e282–288. doi: 10.1542/peds.2008-1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Primack BA, Sidani JE, Agarwal AA, Shadel WG, Donny EC, Eissenberg TE. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med. 2008;36(1):81–86. doi: 10.1007/s12160-008-9047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnett TE, Curbow BA, Weitz JR, Johnson TM, Smith-Simone SY. Water pipe tobacco smoking among middle and high school students. Am J Public Health. 2009;99(11):2014–2019. doi: 10.2105/AJPH.2008.151225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smith JR, Edland SD, Novotny TE, et al. Brief: Increasing hookah use in California. Am J Public Health. 2011;101(10):1876–1879. doi: 10.2105/AJPH.2011.300196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Palamar JJ, Zhou S, Sherman S, Weitzman M. Hookah use among US high school seniors. Pediatrics. 2014 doi: 10.1542/peds.2014-0538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Griffiths MA, Ford EW. Hookah smoking: behaviors and beliefs among young consumers in the United States. Soc Work Public Health. 2014;29(1):17–26. doi: 10.1080/19371918.2011.619443. [DOI] [PubMed] [Google Scholar]
- 23.Fielder RL, Carey KB, Carey MP. Prevalence, frequency, and initiation of hookah tobacco smoking among first-year female college students: A one-year longitudinal study. Addict Behav. 2012;26(4):221–224. doi: 10.1016/j.addbeh.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: predictors and characteristics among current hookah users. Tob Induc Dis. 2009;5(1):16. doi: 10.1186/1617-9625-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asfar T, Ward KD, Eissenberg TE, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5:19. doi: 10.1186/1471-2458-5-19. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC553967. Accessed March 10, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maziak W, Ward KD, Eissenberg TE. Factors related to frequency of narghile (waterpipe) use: the first insights on tobacco dependence in narghile users. Drug Alcohol Depend. 2004;76(1):101–106. doi: 10.1016/j.drugalcdep.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. 2015 National Youth Risk Behavior Survey. [Accessed March 10, 2015];2014:1–22. http://www.cdc.gov/healthyyouth/yrbs/pdf/questionnaire/2015_hs_questionnaire.pdf. [Google Scholar]
- 28.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Ann Arbor, MI: 2014. [Accessed March 10, 2015]. Demographic Subgroup Trends among Adolescents in the Use of Various Licit and Illicit Drugs, 1975-2013. http://monitoringthefuture.org/pubs/occpapers/mtf-occ81.pdf. [Google Scholar]
- 29.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE, Miech RA. Ann Arbor, MI: 2014. [Accessed March 10, 2015]. Monitoring the Future National Survey Results on Drug Use, 1975-2013: Volume I, Secondary School Students. http://www.monitoringthefuture.org/pubs/monographs/mtf-vol1_. [Google Scholar]
- 30.Dugas E, Michele TM, Low NCP, Cournoyer D, O'Loughlin J. Water-pipe smoking among North American youths. Pediatrics. 2010;125(6):1184–1189. doi: 10.1542/peds.2009-2335. [DOI] [PubMed] [Google Scholar]
- 31.Katurji M, Daher N, Sheheitli H, Saleh R, Shihadeh A. Direct measurement of toxicants inhaled by water pipe users in the natural environment using a real-time in situ sampling technique. Inhal Toxicol. 2010;22(13):1101–1109. doi: 10.3109/08958378.2010.524265. [DOI] [PubMed] [Google Scholar]
- 32.Cobb C, Ward KD, Maziak W, Shihadeh A, Eissenberg TE. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34(3):275–285. doi: 10.5993/AJHB.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. Geneva, Switzerland: World Health Organization; 2005. [Accessed March 10, 2015]. TobReg Advisory Note: Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators. http://www.who.int/tobacco/global_interaction/tobreg/waterpipe/en/ [Google Scholar]
- 34.Primack BA, Shensa A, Kim K, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res. 2013;15(1):29–35. doi: 10.1093/ntr/nts076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sribney W. A comparison of different test for trend. [Accessed March 10, 2015];Stata Resour Support. 1996 http://www.stata.com/support/faqs/statistics/test-for-trend.
- 36.Schenker N, Gentleman J. On judging the significance of differences by examining the overlap between confidence intervals. Am Stat. 2001;55(3):182–186. http://www.jstor.org/stable/2685796. Accessed March 10, 2015. [Google Scholar]
- 37.Cumming G, Finch S. Inference by eye: confidence intervals and how to read pictures of data. Am Psychol. 2005;60(2):170–180. doi: 10.1037/0003-066X.60.2.170. http://www.ncbi.nlm.nih.gov/pubmed/15740449. Accessed March 10, 2015. [DOI] [PubMed] [Google Scholar]
- 38.Cumming G. Inference by eye: reading the overlap of independent confidence intervals. Stat Med. 2009;28(2):205–220. doi: 10.1002/sim.3471. http://www.ncbi.nlm.nih.gov/pubmed/18991332. Accessed March 10, 2015. [DOI] [PubMed] [Google Scholar]
- 39.SAS. SAS Statisical Software. 2009 [Google Scholar]
- 40.Grekin ER, Ayna DD. Waterpipe smoking among college students in the United States: A review of the literature. J Am Coll Heal. 2012;60(3):244–249. doi: 10.1080/07448481.2011.589419. [DOI] [PubMed] [Google Scholar]
- 41.Akl EA, Gunukula SK, Aleem S, et al. The prevalence of waterpipe tobacco smoking among the general and specific populations: A systematic review. BMC Public Health. 2011;11:244. doi: 10.1186/1471-2458-11-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Primack BA, Mah J, Shensa A, Rosen D, Yonas MA, Fine MJ. Associations between race, ethnicity, religion, and waterpipe tobacco smoking. J Ethn Subst Abuse. 2014;13(1):58–71. doi: 10.1080/15332640.2013.850462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wechsler H, Davenport AE, Dowdall GW, Grossman SJ, Zanakos SI. Binge drinking, tobacco, and illicit drug use and involvement in college athletics. A survey of students at 140 American colleges. J Am Coll Heal. 1997;45(5):195–200. doi: 10.1080/07448481.1997.9936884. [DOI] [PubMed] [Google Scholar]
- 44.Ames GM, Cunradi CB, Moore RS. Alcohol, tobacco, and drug use among young adults prior to entering the military. Prev Sci. 2002;3(2):135–144. doi: 10.1023/a:1015435401380. http://www.ncbi.nlm.nih.gov/pubmed/12088138. Accessed March 10, 2015. [DOI] [PubMed] [Google Scholar]
- 45.Chassin L, Presson CC, Sherman SJ. Adolescent cigarette smoking: a commentary and issues for pediatric psychology. J Pediatr Psychol. 2005;30(4):299–303. doi: 10.1093/jpepsy/jsi025. http://www.ncbi.nlm.nih.gov/pubmed/15863427. Accessed March 10, 2015. [DOI] [PubMed] [Google Scholar]
- 46.Carroll MV, Shensa A, Primack BA. A comparison of cigarette- and hookah-related videos on YouTube. Tob Control. 2013;22(5):319–323. doi: 10.1136/tobaccocontrol-2011-050253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Afifi RA, Khalil J, Fouad F, et al. Social norms and attitudes linked to waterpipe use in the Eastern Mediterranean Region. Soc Sci Med. 2013;98:125–134. doi: 10.1016/j.socscimed.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 48.Maziak W, Fouad FM, Asfar T, et al. Prevalence and characteristics of narghile smoking among university students in Syria. Int J Tuberc Lung Dis. 2004;8(7):882–889. http://www.ncbi.nlm.nih.gov/pubmed/15260281. Accessed March 10, 2015. [PubMed] [Google Scholar]
- 49.Primack BA, Rice KR, Shensa A, et al. U.S. hookah tobacco smoking establishments advertised on the Internet. Am J Prev Med. 2012;42(2):150–156. doi: 10.1016/j.amepre.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Levy DT, Ross H, Zaloshnja E, Shuperka R, Rusta M. The role of tobacco control policies in reducing smoking and deaths caused by smoking in an Eastern European nation: results from the Albania SimSmoke simulation model. Cent Eur J Public Health. 2008;16(4):189–198. doi: 10.21101/cejph.a3486. http://www.ncbi.nlm.nih.gov/pubmed/19256288. Accessed March 10, 2015. [DOI] [PubMed] [Google Scholar]
- 51.Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98(8):1443–1450. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Primack BA, Hopkins M, Hallett C, et al. US health policy related to hookah tobacco smoking. Am J Public Health. 2012;102(9):e47–e51. doi: 10.2105/AJPH.2012.300838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jawad M, McEwen A, McNeill A, Shahab L. The importance of addressing waterpipe tobacco smoking: Research and policy responses. Addiction. 2013:1887–1888. doi: 10.1093/ntr/ntt103.5. [DOI] [PubMed] [Google Scholar]
- 54.Tozzi J. How Much More Will Smokers Pay for Obamacare? [Accessed March 10, 2015];Bloom Businessweek. 2013 http://www.businessweek.com/articles/2013-12-03/how-much-more-will-smokers-pay-for-obamacare.


